Abstract
Tilia americana and Annona diversifolia are plants widely distributed in Mexico and sold in markets for their medicinal properties on the central nervous system (CNS) including possible neuroprotection. Pharmacological studies have corroborated CNS activities due to flavonoid constituents, but evidence of their neuroprotector effects are lacking. This study was conducted to test aqueous and organic extracts of these two plants for neuroprotective effects in a novel experimental model of intestinal ischemia in situ. T. americana and A. diversifolia aqueous and organic extracts were administrated to guinea pigs at an oral dose of 100 and 300 mg/kg for 15 days. Twenty four hours after the last administration, the animals were anesthetized and intestinal ischemia in situ was induced by clamping for 80 min selected branches of the superior mesenteric artery. Ischemic segments placed in an in vitro organ bath were stimulated electrically (0.3 Hz frequency, 3.0 ms duration, 14 V intensity) and chemically (ACh; 1 × 10−9 to 1×10−5 M). Neuroprotection was considered present when the depressed contractile response of the ischemic tissue to electrical stimulation was normalized in the treated animals. Results showed that pretreatment with the T. americana hexane and aqueous extracts, but not with those from A. diversifolia, significantly improved responses of the ischemic tissue. These results suggest that T. americana possesses neuroprotective effects against neuronal damage induced by ischemia, and that flavonoids as well as non-polar constituents are involved. Our study supports the use of this plant in folk medicine and suggests its possible effectiveness for stroke prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke or cerebrovascular accident is a medical emergency and one of the leading causes of the death and disability worldwide. It consists of a critical reduction in blood flow caused by a sudden obstruction of an artery in an area of the brain [1]. Its pathophysiology is complex and it involves excitotoxicity mechanisms, inflammatory pathways, oxidative damage, ionic imbalances, apoptosis, angiogenesis, but also neuroprotection [2]. A large number of neuroprotective agents have been reported to be highly effective in reducing ischemic lesion in animal brains by interrupting this cascade, but none reduce mortality and/or attenuate disability in stroke patients [3, 4]. The only drug approved in the United States by the Food and Drug Administration (FDA) for treatment of acute ischemic stroke is the recombinant tissue plasminogen activator (rtPA), a thrombolytic agent. Its use, however, is limited by its narrow therapeutic window [2]. The search for agents offering a therapeutic alternative for the management of acute ischemic stroke, whatever their origin or mechanism of action should therefore be continued.
In Mexico as in the rest of the world, medicinal plants are popularly considered as an alternative for the treatment of central nervous diseases [5]. Unfortunately, only a small percentage of medicinal plants with neuroprotective properties have been investigated in experimental models of global or focal ischemia in search of evidence of this CNS activity. This is the case of Ginkgo biloba extract EGb 761 [6], Camellia sinensis infusion (Green Tea [7]), an ethanolic extract of Crataegus oxyacantha [8], the organic extracts from Allium cepa, Artemisia absinthium [9, 10], Ocimum basilicum [11], Mimusops elengi [12] and those from olive leaf enriched in oleuropein [13]. Moreover, the neuroprotective effects of Vitis amurensis and Ilex latifolia have been investigated in in vitro studies on the glutamate-induced excitotoxicity in rat cortical neurons in culture [14, 15].
Annona diversifolia Saff. (Annonaceae) (A. diversifolia) is a tree indigenous to Mexico commonly known as “ilama”, “ilama zapote”, “ilamazapotl” and “zapote de vieja” [16]. Previous pharmacological studies have reported its anxiolytic, antinociceptive and anticonvulsant activities attributed to a non-polar active metabolite identified as palmitone [17–20]. On the other hand, the Tilia genus belongs to Tiliaceae family, which consists of 24 species, mainly distributed in Europe and Asia, and a few in North America [21]. In Mexico, Tilia americana var. mexicana (Schltdl.) Hardin (T. americana), is a medicinal species distributed from Northern Chihuahua to Southern Oaxaca commonly known as linden flower and leaf, “tilia”, or “tilo de hoja” [22]. Throughout the world, Tilia species have been used in traditional medicine for their tranquilizing properties. Infusions of the inflorescences are widely used in Latin America as sedatives and tranquilizers [23, 24], as well as anti-inflammatory agents and in arthritic pain [25, 26]. Previous studies have shown the CNS activities of T. americana and the presence of active metabolites such as glycosides of quercetin and kaempherol and a terpenoid-like beta-sitosterol [27–30].
These two plants are widely distributed in Mexico and are sold in local markets for their purported medicinal CNS properties including a possible neuroprotector effect; they are prepared as aqueous or organic extracts. Although it is well known that these two species have CNS activity and contain active metabolites such as flavonoids and terpenoids, there is no evidence that they are capable of eliciting neuroprotection against ischemia. The present study was therefore designed to investigate the possible neuroprotective effect of A. diversifolia and T. americana aqueous and organic extracts on the neuronal damage induced by intestinal ischemia in situ in guinea pig ileum subjected to chemical and electrical stimulation in a previously described novel model [31, 32].
Materials and Methods
Animals
Adult male guinea pigs, weighing 600–900 g and obtained from our breeding facilities were used. Animals were housed one per cage in a temperature-controlled room (22 ± 2 °C) with an automatically timed cycle of 12 h light/dark (lights on 08:00–20:00 hours). Food (Purina Chow, St. Louis, MO, USA) and water were available ad libitum. Twenty-four hours before experiments, food was withheld and free access to water was maintained. Surgery and experiments were performed between 07:00 and 14:00 hours. This study was carried out under the provisions of the Declaration of Helsinki, and adhered to the National Health Ministry guidelines for the use of laboratory animals, as well as by the Official Mexican Norm for animal care and management (NOM-062-ZOO-1999) [33]. It was approved by the corresponding local ethics committees and registered as projects Nos. 022-2012 (Facultad de Medicina, UNAM) and NC093280 (Instituto Nacional de Psiquiatría).
Plant Material
Annona diversifolia Saff. (Annonaceae) (A. diversifolia) leaves were collected in Tejupilco, Guerrero in September 2010, and a voucher specimen of the plant (AN9702) was deposited at the “Herbarium of useful plants Efraim Hernandez X” of the Autonomous University of Chapingo, State of Mexico. Tilia americana var. mexicana (Schltdl.) Hardin (Tiliaceae) (T. americana) inflorescences were collected in Tenango de Doria, Hidalgo in June 2007 and a voucher specimen of the plant (IMSS M-15070) was deposited at the Instituto Mexicano del Seguro Social in Mexico City.
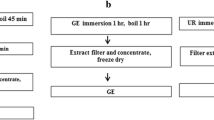
Preparation of the Extracts
The aqueous extract of A. diversifolia was obtained by using 50 g of dried and powdered leaves in a process of infusion in 500 ml of boiling water. The extract was separated from residues by gravity filtration; samples were then frozen in liquid nitrogen and later lyophilized during 12 h using a Heto FD3 Lab lyophilizer to yield 1.11 g (2.22 %). In the case of the organic extracts of A. diversifolia, the dried and powdered leaves (1.5 kg) were exhaustively extracted with hexane (28 L × 3) and ethanol (28 L × 3) through maceration at room temperature (22 °C) and subsequent evaporation in vacuum to give 42 g (2.8 %) and 89 g (5.9 %) of semisolid and syrupy hexane and ethanol crude extracts, respectively.
Preliminary phytochemical studies of this species have demonstrated the presence of palmitone (16-hentriacontanone), oleic acid, stearic acid and palmitic acid [18, 34], as well as acetogenins such as laherradurin and cherimolin-2 [35] in the hexane extract; whereas the alkaloid liriodenine was identified in the methanol extract [36].
In the case of the aqueous extract of T. Americana, the air-dried powdered inflorescences (24 g) were extracted by infusion in boiling water (500 ml) for 1 h. The resulting extract was separated from its residue by gravity filtration; samples were frozen in liquid nitrogen and freeze-dried for 12 h in the lyophilizer mentioned above. The final crude aqueous extract consisted of 1.3 g of a yellow powder or 5.3 % from dry weight. For the preparation of the organic extracts of T. americana, the air-dried powdered ground leaves (1.86 kg) were successively extracted with hexane (4 L × 3), and methanol (4 L × 3) by maceration at room temperature (22 °C). The solvents were separated from the residues by gravity filtration and then evaporated in vacuum. The final crude extracts were obtained in percentage from dry weight (% d.w.) as follows: 25.8 g of a yellow greasy hexane extract (1.38 % d.w.), and 134.4 g of a dark brown syrupy methanol extract (7.2 % d.w.).
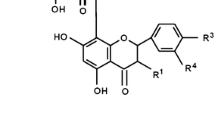
In phytochemical studies from this species have been identified beta-sitosterol in the hexane crude extracts [27]; whereas glycosides of quercetin and kaempherol have been characterized in the methanol crude extract, such as kaempferol-3,7-O-dirhamnoside (kaempferitrin), quercetin-3-O-glucoside (isoquercitrin), kaempferol-3-O-glucoside (astragalin), kaempferol-3-O-rhamnoside, kaempferol-3-O-(6-p-coumaroyl)-glucoside (tiliroside), quercetin-3,7-O-dirhamnoside, quercetin-3-pentoside and quercetin-malonylhexoside [24, 29, 37].
Reagents and Drugs
Potassium chloride (KCl), calcium chloride (CaCl2), sodium chloride (NaCl), magnesium chloride (MgCl2), barium chloride (BaCl2), sodium bicarbonate (NaHCO3), sodium phosphate monobasic monohydrate (NaH2PO4 · H2O), dextrose, were purchased from J. T. Baker. Tween® 80, xylazine hydrochloride, acetylcholine chloride (ACh) and choline chloride were purchased from Sigma Aldrich Mexico and ketamine was purchased from Revetmex®. Vehicle consisted of 0.5 % Tween®80 in saline solution (s.s., 0.9 % NaCl), the Krebs–bicarbonate with glucose (K–B) solution contained (mM): NaCl 118, KCl, 4.7; CaCl2 2.5, MgCl2 1.2, NaH2PO4, 1.2; NaHCO3, 25; dextrose, 11, and choline chloride, 0.3 [31, 32, 38].
Intestinal Ischemia In Situ
As previously was described by Rodriguez et al. [31] and Santiago-Mejia et al. [32], guinea pigs were anaesthetized with an intramuscular injection of a mixture of ketamine (Anesket™, 100 mg/kg) and xylazine (20 mg/kg). Through a 1.5 cm laparotomy the distal part of the ileum was exposed without considering the 10 cm of the tissue nearest to the cecum. The blood supply to a selected portion of the ileum (15 cm) was interrupted by clamping the corresponding ileal branches of the superior mesenteric artery (SMA). The intestine was returned to the abdominal cavity, which was then closed with silk suture. Animals were kept under anesthesia for the rest of experiment. After 80 min of ischemia, the ischemic portion was removed and placed in a Petri dish with K–B solution maintained at 37 °C and bubbled with 95 % O2/5 % CO2. Six ischemic ileum segments 1.5 cm in length were cut and placed in a 20 ml organ bath containing K–B solution at 37 °C and gassed with 95 % O2/5 % CO2. All segments were run simultaneously. The upper end of the ileum was attached to a Grass FT-03C force displacement transducer connected to a Grass 7B polygraph to record isometric contractions. The resting tension was fixed at 1 g. Preparations were allowed to equilibrate for 60 min under continuous superfusion (10 ml/min) of warm K–B solution, and then stimulated with ACh (1 × 10−5 M) to ascertain their viability. The mechanical ileum responses were analyzed with a computerized data acquisition system (PolyView System, version 2.5, Grass instruments).
Electrical and Chemical Stimulation
Preparations were electrically stimulated through two silver electrodes that were positioned parallel to the segments. The anode was placed intraluminally. Maximal contractions of the segments were elicited by transmural nerve stimulation using rectangular current pulses (0.3 Hz of frequency, 3.0 ms of duration and 14 V intensity) delivered by a Grass S88 stimulator and a Med-Lab Stimu-Splitter II. Voltage was progressively increased from 1 to 14 V and superfusion was not interrupted during electrical stimulation. In all the cases, when a maximal contractile effect was obtained, the preparations were washed with 30–60 ml of warm K–B and were chemically stimulated. Chemical stimulations for each tissue, consisted of ACh from 1 × 10−9 to 1 × 10−5 M; KCl, 32 mM; and BaCl2 10 mM [31, 32]. When a maximal contractile effect with each concentration of drug was obtained, the preparations were washed with 30–60 ml of warm K–B solution. Concentrations are expressed as final drug concentrations actually in contact with preparations.
Experimental Design
Sham Tissue
Segments of ileum obtained from animals with laparatomy but without the occlusion of SMA. Animals included in this group received vehicle at an oral way for 15 days.
Ischemic Tissue
Segments of ileum obtained from animals with intestinal ischemia by SMA occlusion.
Treated Tissue
Segments of ileum obtained from animals with intestinal ischemia pretreated with the T. americana and A. diversifolia aqueous and organic extracts at an oral dose of 100 and 300 mg/kg for 15 days. One animal was used for each extract and each dose. The ischemia in situ was performed 24 h after the last administration of each extract.
Verapamil Tissue
Segments of ileum obtained from animals with intestinal ischemia pretreated with 0.3 mg/kg of verapamil (a calcium channel blocker), as positive control of neuroprotection, administered intravenously 15 min before ischemia.
Statistical Analysis
Data are expressed as the mean ± SEM with six replicates. Contractile responses were expressed as grams of tension or as the area under the curve (AUC) in units of area (ua). This parameter was calculated from the concentration–response curves to ACh (1 × 10−9 to 1 × 10−5 M). Significant differences between the contractile response in the ischemic and sham groups were determined by Student’s t test. Significant differences among contractile response of the ischemic segments exposed to electrical and chemical stimulation and other treatment groups were determined using one-way ANOVA followed by Dunnett’s test. Statistical analysis and graphics were performed using the Graph-Pad Prism (version 5.0) software. At least 6 repetitions were performed for each treatment. Significance was considered present at a P < 0.05.
Results
As observed in a typical recording (Fig. 1), the maximal contractile response in the sham guinea pig ileum was 2.55 ± 0.11 g after electrical (14 V, 0.3 Hz, 3.0 ms, 5 min) stimulation and 4.72 ± 0.09 g after chemical (ACh, 1 × 10−5 M) stimulation. These responses were significantly (P < 0.05) diminished by 75 % (0.63 ± 0.16 g) and 62 % (1.81 ± 0.25 g), respectively, in the ischemic guinea pig ileum (Fig. 1a, b). Oral administration of vehicle (0.5 % Tween 80 in s.s.) during 15 days before intestinal ischemia did not modify the contractile response after electrical stimulation of the ischemic tissue without vehicle (0.75 ± 0.12 g) (Fig. 2a, b).
Contractile response induced by electrical field stimulation (14 V, 0.3 Hz, 3.0 ms) in ischemic tissue from animals pretreated with hexane (HEX), methanol (MeOH) or aqueous (AQUO) extracts of T. americana (a) or hexane (HEX), ethanol (EtOH) and aqueous (AQUO) extracts of A. diversifolia (b). Verapamil is a positive control. Contractions are expressed in grams of tension. *P < 0.05 versus sham group, Student's t test. # P < 0.05 versus ischemic group, one way ANOVA followed by Dunnett's test. Each bar represents the mean ± SEM of 6 repetitions
Response of Tissues to Electrical Stimulation
Pretreatment with verapamil (positive neuroprotector) significantly increased responses to electrical stimulation by 84 ± 12 % (1.38 ± 0.09 g) in comparison to the ischemic tissue receiving vehicle (Fig. 2a, b). Pretreatment with the hexane or aqueous extracts of T. americana at 100 mg/kg did not change the reactivity of ischemic tissues to electrical stimulation (Fig. 2a), but 300 mg/kg of these extracts did significantly increase reactivity by 95.5 ± 22.2 and 88.8 ± 39 % (1.47 ± 0.17 and 1.42 ± 0.29 g), respectively, resembling the response obtained with verapamil (Fig. 2a). The methanol extract did not influence contractile responses of the ischemic tissue at the dosages tested (Fig. 2a). In no case did the active treatments completely restored responses to the levels observed in of the sham group (Fig. 2a). None of the extracts of A. diversifolia at the doses tested influenced ischemic tissue reactivity (Fig. 2b).
Response of Tissues to Chemical Stimulation
After chemical stimulation with ACh (1 × 10−5 M), the maximal contractile response of the ischemic tissues from animals pretreated with 100 mg/kg of T. americana hexane or aqueous extracts significantly increased by 132 ± 14.90 % (3.02 ± 0.19 g) or 85.89 ± 24.60 % (2.42 ± 0.32 g), respectively; whereas an increase of 142.30 ± 23.89 % (3.15 ± 0.31 g) or 92.30 ± 27.01 % (2.50 ± 0.35 g), correspondingly, was observed at 300 mg/kg (Fig. 3a). These responses were equivalent to that obtained with verapamil (116.60 ± 28.40 %, 2.82 ± 0.37 g) (Fig. 3a). The AUC of concentration–response curves to ACh in the ischemic tissues receiving vehicle was significantly increased by verapamil or the hexane and aqueous extracts of T. americana (Table 1). No differences were seen when the verapamil response was compared to those observed with the extracts (Table 1). The increased contractile responses did not reach the maximal response observed in sham tissues (Table 1). As in the case of responses to electrical stimulation, reactivity to ACh was not modified by extracts of A. diversifolia (Table 1; Fig. 3b).
Concentration-response curves to ACh in the ischemic tissues from animals pretreated with hexane (HEX), methanol (MeOH) or aqueous (AQUO) extracts of T. americana (a); hexane (HEX), ethanol (EtOH) and aqueous (AQUO) extracts of A. diversifolia (b). Verapamil group is a positive control. Contractions are expressed as grams of tension. Each point represents the mean ± SEM of 6 repetitions
Responses to chemical stimulation with KCl (32 mM), in ischemic tissues were significantly increased by pretreatment with 0.3 mg/kg of verapamil, both doses of the hexane extract or 100 mg/kg of the aqueous extract of T. americana (Table 1). Responses to BaCl2 (10 mM) were not different in tissues from the sham and ischemic animals. Moreover, pretreatment with T. americana or A. diversifolia extracts did not modify the reactivity of these tissues, except in those obtained from animals pretreated with 300 mg/kg of the methanol extract of T. americana, which showed a significant decrease (Table 1).
Discussion
The ischemic model used in this study constitutes a pharmacological tool in which neuronal damage to myenteric neurons is related to a reduction in the contractile response after electrical and chemical stimulation in the guinea pig ileum [31, 32, 38]. The reduced response in ischemic tissues can be prevented with pretreatment with certain agents, such as antioxidants or calcium channels blockers, as verapamil, considered as neuroprotective drugs [39]. In the present study, pretreatment with hexane or aqueous extracts of the T. americana inflorescences, but not those obtained from A. diversifolia, prevented the dysfunctional response (reduced contractile activity) of the ischemic tissue in a significant manner. It is known that electrical stimulation of the ileum preparations induces the release of various neurotransmitters from functional synapses, mainly ACh [40, 41]. The ACh-induced contraction is produced by an increase in the frequency of the action potentials and the depolarization of the smooth muscle cells, which results in smooth muscle contraction [42]. A diminution of the electrically induced contraction in ischemic tissues might be due to reduction of either neurotransmitter release, or the ability of smooth muscle to contract in response to the released neurotransmitters such as ACh. To confirm neuronal damage in this model, the contractile response induced chemically with KCl was also investigated. The KCl-induced contraction is due to depolarization of the cells caused by the increase of K+, which leads to the opening of L-type Ca2+ voltage-dependent channels, increased intracellular Ca2+ concentration and contraction [43]. The KCl-stimulated ischemic tissue showed a reduced contractile response that was prevented with hexane and aqueous extracts of T. americana, as was also observed in the chemical stimulation with ACh. A partial prevention of the neuronal damage observed in the presence of T. americana hexane and aqueous extracts suggest that non-polar and polar constituents are involved in its effect. On the other hand, the integrity of smooth muscle cells was examined in the BaCl2 experiments, since it is known that this agent enters the intracellular space and stimulates smooth muscle directly [44]. Results of these experiments discard a role of smooth muscle damage in the reduced contractile response to electrical stimulation after ischemia. The reduction in reactivity to BaCl2 observed by pretreatment with 300 mg/kg of the methanol extract of T. americana may be attributed to a toxic effect, since an LD50 of 375 mg/kg, i.p. has been reported for this material in mice [27, 28].
The precise mechanism of action and metabolites involved in the effect of the T. americana extracts are unknown; several constituents might be acting at the same time through several pathways. It is known that in ischemia reactive oxygen species are generated; drugs acting as scavengers of these species inhibit apoptosis or excitatory neurotransmitters thus reducing neuronal damage [39]. Furthermore, treatments with extracts that contain high concentrations of flavonoids minimize neuronal damage induced by ischemia [14, 45]. Previous studies with T. americana have reported abundant presence of beta-sitosterol (0.06 % yield from hexane extract) and some fatty acids [27], as well as of flavonoids of quercetin (16.84 ± 2.80 mg/g) and kaempherol (2.20 ± 0.18 mg/g) such as kaempheritrin, isoquercitrin, rutin, astragalin, quercitrin and tiliroside [24, 27–30, 37]. The presence of these metabolites could explain reports on the neuroprotective effect of polar extracts of medicinal plants, attributed to the presence of quercetin, kaempherol, myricetin and catechin [6, 8, 37, 46, 47]. Individual administration of epicatechin and hesperidin has shown protection against neuronal damage [48], while narigenin and quercetin inhibited the inflammatory process that is known to lead to neuronal injury [48–50]. It is possible that these active metabolites of T. americana are involved in the protection observed in the present experiments. It should be interesting to in the future to explore their individual effects and mechanisms of action by using this novel model of ischemia.
In conclusion, these results give evidences that non-polar and polar extracts of T. americana but not from A. diversifolia, prevented neuronal damage induced by ischemia in situ. Our study reinforces the use of T. americana in folk medicine and suggests its utility for stroke prevention. However, additional studies in an in vivo model of cerebral ischemia should be carried out to confirm the neuroprotective activity of T. americana var. mexicana.
References
Hossmann KA (2006) Pathophysiology and therapy of experimental stroke. Cell Mol Neurobiol 26:1057–1083
Sahota P (2011) Investigational therapies for ischemic stroke: neuroprotection and neurorecovery. Neurother 8:434–451
De Keyser J, Sulter G, Luiten PG (1999) Clinical trials with neuroprotective drugs in acute ischaemic stroke: are we doing the right thing? Trends Neurosci 22:535–540
Cheng YD, Al-Khoury L, Zivin JA (2004) Neuroprotection for ischemic stroke: two decades of success and failure. NeuroRx 1:36–45
Gomes NG, Campos MG, Órfao JM, Ribeiro CA (2009) Plants with neurobiological activity as potential targets for drug discovery. Prog Neuropsychopharmacol Biol Psychiatry 33:1372–1389
Paganelli RA, Benetoli A, Milani H (2006) Sustained neuroprotection and facilitation of behavioral recovery by the Ginkgo biloba, EGb 761, after transient forebrain ischemia in rats. Behav Brain Res 174:70–77
Abdeen SM, Mathew TC, Path FRS, Dashti HM, Asfar S (2011) Protective effects of green tea on intestinal ischemia-repersufión injury. Nutrition 27:598–603
Elango C, Devaraj SN (2010) Immunomodulatory effect of Hawthorn extract in an experimental stroke model. J Neuroinflammation 30:97
Shri R, Bora KS (2008) Neuroprotective effect of methanolic extracts of Allium cepa on ischemia and reperfusión-induced cerebral injury. Fitoterapia 79:86–96
Bora KS, Sharma A (2010) Neuroprotective effect of Artemisia absinthium L. on focal ischemia and reperfusion-induced cerebral injury. J Ethnopharmacol 129:403–409
Bora KS, Arora S, Shri R (2011) Role of Ocimum basilicum L. in prevention of ischemia and reperfusión-induced cerebral damage, and motor dysfuntions in mice brain. J Ethnopharmacol 137:1360–1365
Nagakannan P, Shivasharan BD, Thippeswamy BS, Veerapur VP, Bansal P (2012) Protective effect of hydroalcoholic extract of Mimusops elengi Linn. flowers against middle cerebral artery occlusion induced brain injury in rats. J Ethnopharmacol 140:247–254
Rabiei Z, Bigdeli MR, Rasoulian B, Ghassempour A, Mirzajani F (2012) The neuroprotection effect of pretreatment with olive leaf extract on brain lipidomics in rat stroke model. Phytomedicine 19:940–946
Kim JY, Jeong HY, Lee HK, Kim S, Hwang BY, Bae K, Seong YH (2012) Neuroprotection of the leaf and stem of Vitis amurensis and their active compounds against ischemic brain damage in rats and excitotoxic in cultured neurons. Phytomedicine 19:150–159
Kim JY, Lee HK, Hwang BY, Kim S, Yoo JK, Seong YH (2012) Neuroprotection of Ilex latifolia and caffeoylquinic acid derivatives against excitotoxic and hypoxic damage of cultured rat cortical neurons. Arch Pharm Res 35:1115–1122
Ruiz SE, Morett A (1997) Las Anonas en el México Prehispánico. Memorias Congreso Internacional de Anonáceas, Chapingo, México
González-Trujano ME, Tapia E, Lopez-Meraz L, Navarrete A, Reyes-Ramirez A, Martínez A (2006) Anticonvulsant effect of Annona diversifolia Saff. and palmitone on penicillin-induced convulsive activity: a behavioral and EEG study in rats. Epilepsia 47:1810–1817
Carballo AI, Martínez AL, González-Trujano ME, Pellicer F, Ventura-Martínez R, Díaz-Reval MI, López-Muñoz FJA (2010) Antinociceptive activity of Annona diversifolia Saff. leaf extracts and palmitone as bioactive compound. Pharmacol Biochem Behav 95:6–12
González-Trujano ME, López-Meraz L, Reyes-Ramírez A, Aguillón M, Martínez A (2009) Effect of repeated administration of Annona diversifolia Saff. (Ilama) extracts and palmitone on rat amygdala kindling. Epilepsy Behav 16:590–595
Cano-Europa E, González-Trujano ME, Reyes-Ramírez A, Hernández-García A, Blas-Valdivia V, Ortiz-Butrón R (2010) Palmitone prevents pentylenetetrazole-caused neuronal damage in the CA3 hippocampal region of prepubertal rats. Neurosci Lett 470:111–114
Hardin JW (1990) Variation patterns and recognition of Tilia americana. s, 1. Syst Bot 15:33–48
Martínez M (1979) Catálogo de nombres vulgares y científicos de plantas mexicanas. Fondo de Cultura Económica, México
Coleta M, Campos MG, Cotrim MD, Cunha AP (2001) Comparative evaluation of Melissa officinalis L., Tilia europea L., Passiflora edulis Sims. and Hypericum perforatum L. in the elevated plus maze anxiety test. Pharmacopsychiatry 34:520–521
Pérez-Ortega G, Guevara-Fefer P, Chávez M, Herrera J, Martínez A, Martínez AL, González-Trujano ME (2008) Sedative and anxiolytic efficacy of Tilia americana var. mexicana inflorescences used traditionally by communities of State of Michoacan, Mexico. J Ethnopharmacol 116:461–468
Martínez M (1969) Las plantas medicinales de México, 5th edn. Andrés Ediciones Botas, México
Estrada EL (1985) Maximino Martínez (1888–1964). Jardín botánico de plantas medicinales “Maximino Martínez” Universidad Autónoma Chapingo, Chapingo, México
Aguirre-Hernández E, Rosas-Acevedo H, Soto-Hernández M, Martínez AL, Moreno J, González-Trujano ME (2007) Bioactivity-guided isolation of β-Sitosterol and some fatty acids as active compounds in the anxiolytic and sedative effects of Tilia americana var. mexicana. Planta Med 73:1148–1155
Aguirre-Hernández E, Martínez AL, Gonzalez-Trujano ME, Moreno J, Vibrans H, Soto-Hernández M (2007) Pharmacological evaluation of the anxiolytic and sedative effects of Tilia americana L. var. mexicana in mice. J Ethnopharmacol 109:140–145
Herrera-Ruiz M, Román-Ramos R, Zamilpa A, Tortoriello J, Jiménez-Ferrer JE (2008) Flavonoids from Tilia americana with anxiolytic activity in plus-maze test. J Ethnopharmacol 118:312–317
Martínez AL, González-Trujano ME, Aguirre-Hernández E, Moreno J, Soto-Hernández M, López-Muñoz FJ (2009) Antinociceptive activity of Tilia americana var. mexicana inflorescences and quercetin in the formalin test and in arthritic pain model in rats. Neuropharmacol 56:564–571
Rodriguez R, Ventura-Martínez R, Santiago-Mejia J, Avila-Costa MR, Fortoul TI (2006) Altered responsiveness of the guinea-pig isolated ileum to smooth muscle stimulants and to electrical stimulation after in situ ischemia. Br J Pharmacol 147:371–378
Santiago-Mejia J, Ventura-Martinez R, Gomez C, Parra-Gamez L, Gonzalez-Rios J, Rodriguez R (2007) Polyviewed expression of the altered contractility of the guinea-pig ileum alters ischemia in situ and superfusion in vitro. J Physiol Pharmacol 58:275–285
NOM-062-ZOO-1999 (1999) Secretaría de Salud Norma Oficial Mexicana, México
González-Trujano ME, Navarrete A, Reyes B, Cedillo-Portugal E, Hong E (2001) Anticonvulsant properties and bio-guided isolation of palmitone from leaves of Annona diversifolia. Planta Med 67:136–141
Schlie-Guzmán MA, García-Carrancá A, González-Esquinca AR (2009) In vitro and in vivo antiproliferative activity of laherradurin and cherimolin-2 of Annona diversifolia Saff. Phytother Res 23:1128–1133
De la Cruz Chacón I, González-Esquinca AR (2012) Liriodenine alkaloid in Annona diversifolia during early development. Nat Prod Res 26:42–49
Aguirre-Hernández E, González-Trujano ME, Martínez AL, Moreno J, Kite G, Terrazas T, Soto-Hernández M (2010) HPLC/MS analysis and anxiolytic-like effects of quercetin and kaempferol flavonoids from Tilia americana var. mexicana. J Ethnopharmacol 127:91–97
Ventura-Martínez R, Santiago-Mejia J, Gomez C, Rodriguez R, Fortoul TI (2008) Acute morphological changes in guinea pig ileum myenteric neurons after ischemia in situ with superfusion in vitro. Pathol Res Pract 204:121–127
Lees KR, Zivin JA, Ashwood T, Davalos A, Davis SM, Diener HC, Grotta J, Lyden P, Shuaib A, Hårdemark HG, Wasiewski WW (2006) Stroke-acute ischemic NXY treatment (SAINT I) trial investigators NXY-059 for acute ischemic stroke. New Engl J Med 354:588–600
Bornstein JC, Costa M, Grider JR (2004) Enteric motor and interneuronal circuits controlling motility. Neurogastroenterol Motil 16:34–38
Gerthoffer W (2005) Signal-transduction pathways that regulate visceral smooth muscle function III. Coupling of muscarinic receptors to signaling kinases and effector proteins in gastrointestinal smooth muscles. Am J Physiol Gastrointest Liver Physiol 288:G849–G853
Reddy H, Watson N, Ford AP, Eglen RM (1995) Characterization of the interaction between muscarinic M2 receptors and β–adrenoceptor subtypes in guinea-pig isolated ileum. Br J Pharmacol 114:49–56
Karaki H, Ozaki H, Hori M, Mitsui-Saito M, Amano KI, Harada KI, Miyamoto S, Nakazawa H, Won KJ, Sato K (1997) Calcium movements, distribution, and functions in smooth muscle. Pharmacol Rev 49:157–215
Hansen TR, Dineen DX, Petrak R (1984) Mechanism of action of barium ion on aortic smooth muscle. Am J Physiol 246:C235–C241
Dajas F, Rivera-Megret F, Blasina F, Arredondo F, Abin-Carriquiry JA, Costa G, Echeverry C, Lafon L, Heizen H, Ferreira M, Morquio A (2003) Neuroprotection by flavonoids. Braz J Med Biol Res 36:1613–1620
Pu F, Mishima K, Irie K, Motohashi K, Tanaka Y, Orito K, Egawa T, Kitamura Y, Egashira N, Iwasaki K, Fujiwara M (2007) Neuroprotective effects of quercetin and rutin on spatial memory impairment in an 8-arm radial task and neuronal death induced by repeat cerebral ischemia in rats. J Pharmacol Sci 104:329–334
Dajas F (2012) Life or death: neuroprotective and anticancer effects of quercetin. J Ethnopharmacol 143:383–396
Akhlaghi M, Bandy B (2009) Mechanisms of flavonoid protection against myocardial ischemia-reperfusion injury. J Mol Cell Cardiol 46:309–317
Jäger AK, Saaby L (2011) Review flavonoids and the CNS. Molecules 16:1471–1485
Chen JC, Ho FM, Lee Chao PD, Chen CP, Jeng KC, Hsu HB, Lee ST, Wu WT, Lin WW (2005) Inhibition of iNOS gene expression by quercetin is mediated by the inhibition of lkappaB kinase, nuclear factor-kappa B and STAT1, and depends on heme oxygenase-1 induction in mouse BV-2 microglia. Eur J Pharmacol 521:9–20
Acknowledgments
This study was supported by Grants from Program to Support Research Projects and Technological Innovation (PAPIIT, IN201713), National Council of Science and Technology (CONACYT, 80811) and National Institute of Psychiatry (INP-NC093280). PhD. G.E. Angeles-López thankful a fellowship from General Direction of Academic of Personnel Matters of National University of Mexico (DGAPA-UNAM, 070/2012). We are thankful to Mr. Oscar Ramirez for his technical assistance.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Angeles-López, G.E., González-Trujano, M.E., Déciga-Campos, M. et al. Neuroprotective Evaluation of Tilia americana and Annona diversifolia in the Neuronal Damage Induced by Intestinal Ischemia. Neurochem Res 38, 1632–1640 (2013). https://doi.org/10.1007/s11064-013-1065-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-013-1065-5