Abstract
Parkinson’s disease (PD) is characterized by selective degeneration and loss of dopaminergic neurons in the substantia nigra (SN) of the ventral mid brain leading to dopamine depletion in the striatum. Oxidative stress and mitochondrial damage have been implicated in the death of SN neurons during the evolution of PD. In our previous study on human PD brains, we observed that compared to SN, striatum was significantly protected against oxidative damage and mitochondrial dysfunction. To understand whether brain aging contributes to the vulnerability of midbrain to neurodegeneration in PD compared to striatum, we assessed the status of oxidant and antioxidant markers, glutathione metabolic enzymes, glial fibrillary acidic protein (GFAP) expression and mitochondrial complex I(CI) activity in SN (n = 23) and caudate nucleus (n = 24) during physiological aging in human brains. We observed a significant increase in protein oxidation (P < 0.001), loss of CI activity (P = 0.04) and increased astrocytic proliferation indicated by GFAP expression (P < 0.001) in SN compared to CD with increasing age. These changes were attributed to significant decrease in antioxidant function represented by superoxide dismutase (SOD) (P = 0.03), glutathione (GSH) peroxidase (GPx) (P = 0.02) and GSH reductase (GR) (P = 0.03) and a decreasing trend in total GSH and catalase with increasing age. However, these parameters were relatively unaltered in CD. We propose that SN undergoes extensive oxidative damage, loss of antioxidant and mitochondrial function and increased GFAP expression during physiological aging which might make it more vulnerable to neurotoxic insults thus contributing to selective degeneration during evolution of PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is an age-associated neurodegenerative disease clinically characterized as a movement disorder [1]. The chief pathological hallmark in PD is the gradual loss of dopaminergic neurons in the substantia nigra pars compacta (SNpc) leading to the depletion of dopamine in the striatum which ultimately manifests as motor impairment. Histopathology based staging in human PD brains has shown localized pathology in the brainstem nuclei including the SN that later spreads to the neocortex in the post-motor stage of the disease [2]. Although many anatomical areas are potentially affected, SN is selectively targeted for damage during PD. Research evidences have suggested that the vulnerability of SN dopaminergic neurons to oxidative stress and mitochondrial dysfunction could significantly contribute to neurodegeneration in PD [3–7]. Accordingly, increased oxidative damage [8, 9] and loss of antioxidants such as glutathione (GSH) [10], have been detected in the dopaminergic areas of the PD brain. Further, oxidative and nitrative damage to proteins in SN dopaminergic neurons have been documented in the disease samples from human subjects [11–13] and in the animal models of PD [14–19]. Oxidative and nitrosative stress in PD is directly associated with mitochondrial dysfunction in the SN [20, 21]. Apart from oxidative damage, PD pathology is also associated with neuroinflammation and astrogliosis with upregulation of the glial marker, glial fibrillary acidic protein (GFAP) [22, 23].
In order to investigate whether non-SN brain regions are also affected similar to SN during PD, we recently tested the markers of antioxidant function and oxidative stress in caudate nucleus (CD), putamen (Put) and frontal cortex (FC) in human postmortem PD brain tissues [24]. We observed a relatively lower oxidative damage and mitochondrial dysfunction in the above regions compared to SN and demonstrated that increased GSH level in them might protect against oxidative and mitochondrial damage in PD. Although SN and striatum are part of the nigrostriatal dopaminergic pathway, the selective targeting of SN during PD needs to be explained. Since PD is an age-associated disease, we questioned whether accumulated biochemical differences in SN and striatum during physiological aging might contribute to the selective vulnerability of SN. To address this, we carried out in this study, a comparative evaluation of the status of oxidative damage, antioxidant function, GSH metabolic enzymes, astrogliosis and mitochondrial function with increasing age in human substantia nigra (n = 23; age = 12–80 years) and caudate nucleus (n = 24; age = 4–80 years).
Experimental Procedure
All chemicals used were of analytical grade. Bulk chemicals were obtained from Merck (Whitehouse Station, NJ, USA) and Sisco Research Laboratories Pvt. Ltd. (Mumbai, Maharashtra, India). Nitrocellulose membrane from Millipore (Billerica, MA, USA), mouse monoclonal antibody to glial fibrillary acidic protein (GFAP) (clone GA-5) from Biogenex (San Ramon, CA, U.S.A.), rat polyclonal anti-tubulin antibody from Abcam laboratories (Cambridge, U.K.), horseradish peroxidase conjugated secondary antibodies from Bangalore Genei (Bangalore, Karnataka, India), anti-dinitrophenyl (DNP) and anti-3-nitrotyrosine antibodies and protease inhibitor cocktail from Sigma (Eugene, OR, U.S.A.) were obtained.
Human Tissue Samples and Histology
Human brain samples were sourced from the Human Brain Tissue Repository (HBTR), Department of Neuropathology, National Institute of Mental Health and Neurosciences (NIMHANS), Bangalore, India. The brain tissues were collected with informed consent from the close relatives of the deceased and the Institutional Ethics Committee has approved the study protocol. The brains were from normal subjects who succumbed to road traffic accidents (non-alcoholics, non-diabetics, not on any medication and with no known neurological or psychiatric disorders). Demographic and clinical details of all the subjects were recorded. Within 1 h of death, the body was transferred to a refrigerator maintained at 2–4°C with a recorder and uninterrupted power supply. Following autopsy, the brains were recovered and sliced coronally and kept flat on salt-ice mixture (−15 to −18°C) during dissection and then transferred in plastic zip lock bags into a box to be stored at −80°C in the HBTR. The procedure of dissection took 30–45 min and the brain slices were transferred immediately into the deep freezer. The postmortem interval (PMI) (the elapsed time between death and the freezing of the brain samples following autopsy and dissection) was recorded for each case. The brain areas chosen for the study were anatomically farthest from the site of injury and without distinct edema or abnormal morphology. While the major portion of the tissue was frozen for biochemical studies, a minor portion corresponding to the mirror image bits of the stored tissue were fixed in buffered formalin. These tissues were subjected to routine histological assessment by neuropathologists (SKS and AM) and the samples that maintained tissue integrity were utilized for the study (data not shown). The same procedure of autopsy, tissue handling and other procedures were uniformly maintained for all the samples in this study. Similar tissues from the human brain bank have been earlier utilized extensively as control samples in PD research [24–27] and other studies [28–32].
In the current study, two anatomical areas, substantia nigra (SN) and caudate nucleus (CD) were analyzed from the postmortem brains. Table 1 shows the list of all the brain samples (SN: n = 23; male = 17, female = 6. CD: n = 24; male = 17, female = 7) from which tissues were utilized for the study. The age of the subjects studied ranged from 12 to 80 years for SN samples and 4 to 80 years for CD samples and the PMI ranged from 3 to 22 h. Due to the limitation in the amount of tissue available from each region, all the samples have not been used for all the assays (sample numbers have been indicated for each assay in the legend).
Preparation of Protein Extracts
Brain tissue (~100 mg) was manually homogenized in cold 1× phosphate buffered saline (PBS) containing protease inhibitor cocktail on ice (15 strokes) and sonicated (20 s on ice) in a Sonics-vibra cell sonicator (Sonics and Materials Inc, CT, USA) [30]. The extract was centrifuged (15,000×g, 10 min) to separate the insoluble debris. The supernatant corresponding to the soluble fraction was subjected to protein estimation followed by biochemical assays [24].
SDS PAGE and Western Blot
The brain samples were thawed on ice and homogenized in 1× phosphate buffered saline (PBS) containing protease inhibitor cocktail, homogenized and sonicated on ice (5 s × 5). The extracts were immediately centrifuged at 15,000×g for 10 min to remove insoluble cellular debris and the total protein in the supernatant was estimated. Equal quantities of protein (50 μg) per sample were loaded on 10% SDS PAGE followed by western blot with either anti-GFAP or β-tubulin antibody [24].
Analysis of Oxidative Markers
Estimation of Protein Carbonyls (Oxyblot) and Protein Nitration
Oxyblots were carried out as described earlier [30, 33]. Briefly, brain protein extract (4 mg/ml) was derivatized by dinitrophenyl hydrazine (DNPH) in a 20 μl reaction mixture in the presence of 12% SDS for 20 min at room temperature. The reaction was stopped by neutralization with 2 M Tris in 30% glycerol and 5 μl of the sample was spotted in triplicate on nitrocellulose membrane and probed with anti-DNP antibody. Non-derivatized samples did not show anti-DNP immunoreactivity confirming the specificity of the antibody (data not shown).
To detect protein nitration, protein (10 μg/sample) from different samples were spotted in triplicate onto a nitrocellulose membrane and probed with polyclonal anti-3-nitrotyrosine (3-NT) antibody. Western signals were densitometrically quantified and normalized against the respective anti-tubulin signal.
Estimation of Lipid Peroxidation
Lipid peroxidation was measured by estimation of malondialdehyde (MDA) by thiobarbituric acid reaction method [34]. Tissues were homogenized, sonicated and centrifuged at 16,000g (10 min) at 4°C. 100 μl of the supernatant was added to a mixture containing 0.75 ml of acetic acid (pH 3.5, 20% v/v), 0.1 ml SDS (8%, w/v) and 0.75 ml of thiobarbituric acid (0.8%, w/v) and heated in a boiling water bath for 45 min. The adducts formed were extracted into 1.5 ml of 1-butanol and centrifuged at 2,500 rpm (10 min) and their absorbance was measured at 532 nm. The amount of MDA formed was calculated using the molar extinction coefficient (241 mol/cm).
Assays for Antioxidant Function and GSH Metabolism
Catalase Assay
Catalase activity was assayed by the method described previously [35]. The enzyme activity was expressed as μmol H2O2 consumed/min/mg protein (e = 43.6 mM−1 cm−1). Reaction mixture containing 15 μg protein (sample) was mixed with 900 μl phosphate buffer (0.1 M, pH 7.0) and 50 μl of H2O2 (8.8 mM) and the decrease in absorbance at 240 nm was followed for 5 min.
Superoxide Dismutase Assay
SOD activity was assayed using its inhibitory action on quercetin oxidation based on the method described earlier with minor modifications [36]. The final reaction mixture contained 30 mM Tris HCl (pH 9.1), 0.5 mM EDTA, 50 mM TEMED, 0.05 mM quercetin and 10 μl of brain extract supernatant containing 10 μg of protein. The reaction was monitored at 406 nm for 10 min. One unit of SOD activity was defined as the amount of enzyme (per mg protein) that inhibits quercetin oxidation reaction by 50% of maximal value.
Estimation of Total Glutathione (GSH + GSSG)
Total glutathione estimations were carried out by the 5,5′ dithio-bis-2-nitro benzoic acid recycling method as described earlier [37]. All estimations were conducted in triplicate and total glutathione concentrations were normalized per mg protein.
Glutathione Peroxidase Assay
GPx activity was determined by t-butyl hydroperoxide (tbHP) method [38]. The reaction mixture containing 150 μg protein (sample), 0.1 M phosphate buffer, 0.5 mM EDTA, 100 μl Glutathione reductase (0.24 U), 100 μl GSH (1 mM), 100 μl NADPH (0.15 mM) was incubated at 37°C for 3 min and the reaction was initiated by the addition of 100 μl tbHP (0.12 mM). Change in absorbance at 340 nm was monitored for 5 min spectrophotometrically and the activity was expressed as nmoles of NADPH oxidized/min/mg protein (MEC: 6.22 mM−1 cm−1).
Glutathione Reductase Assay
Solubilized brain protein extract (100 μg) was assayed at 25°C in 0.1 M Tris–HCl (pH 8.1) and 0.2 mM NADPH and the reaction was initiated by the addition of 1 mM GSSG. The enzyme activity was measured by monitoring the oxidation of NADPH, spectrophotometrically at 340 nm, as described earlier [39].
Glutathione-S-Transferase Assay
GST was assayed by the 1-chloro-2,4-dinitro benzene (CDNB) method [40]. To 1 ml reaction mixture containing phosphate buffer (0.1 M, pH 6.5; 0.5 mM EDTA), CDNB (1.5 mM) and 50 μl GSH (1 mM), 30 μg protein (sample) was added and the increase in absorbance at 340 nm was monitored for 5 min. The enzyme activity was expressed as nmoles of S-2,4, dinitrophenyl glutathione formed/min/mg protein (MEC: 9.6 mM−1 cm−1).
Preparation of Mitochondria and Complex I (CI) Assay
Mitochondria from the tissue samples were freshly prepared and subjected to CI assay as previously described [41, 42]. The assay was initiated by addition of aliquots of brain mitochondria to 50 mM potassium phosphate/Tris–HCl, pH 7.4, 500 μM Ethylenediaminetetraacetic acid (EDTA), 1% bovine serum albumin, 200 μM NADH, and 200 μM decylubiquinone with and without 2 μM rotenone in the presence of potassium cyanide (KCN) with 0.002% dichloroindophenol as a secondary electron acceptor. The decrease in the absorbance at 600 nm was recorded as a measure of enzyme reaction rate at 37°C for 10 min, and specific activity was calculated. The results were plotted as relative rotenone sensitive specific activity.
Statistical Analysis
Quantitative data from at least three independent experiments were expressed as mean ± SD followed by analysis of variance (ANOVA) and Pearson’s correlation of linear regression (r value). For all the quantitative data, P < 0.05 was considered to be statistically significant.
Results
Biochemical analysis in PD has demonstrated significant oxidative stress and mitochondrial dysfunction in SN [43–45]. In order to analyze whether increased oxidative stress during physiological aging makes SN selectively vulnerable to PD, we quantitated the level of oxidative damage of proteins in SN (n = 18) compared to CD (n = 21). Accordingly, we observed that protein oxidation (protein carbonylation in tissue extracts determined by oxyblot) was significantly increased in the SN with increasing age while it was unaltered in CD (SN: r = 0.80, P < 0.001; CD: r = 0.19, P = 0.23) (Fig. 1a). On the other hand, protein nitration (determined by total protein 3-NT) showed an increasing trend in SN, although it was not statistically significant with increasing age (r = 0.33, P = 0.11) (Fig. 1b). However, protein 3-NT was relatively unaltered in CD (r = 0.03, P = 0.45) (Fig. 1b).
Analysis of protein oxidation and nitration in postmortem human brains with increasing age. Total protein extract after DNP-derivatization (~10 μg) in SN (n = 18) and CD (n = 21) were spotted on nitrocellulose membrane in triplicate followed by anti-DNP western blot (Oxyblot). Following densitometric analysis, the average for each sample was plotted as mean ± SD followed by regression analysis. The r and P values for each region are shown. a Representative anti-DNP blot of SN and CD tissue extracts with increasing age (arrows indicate the age in years (y) of each sample; flower brackets correspond to the triplicate for each sample) and the quantitative plots of anti-DNP signal (normalized with β-tubulin signal as indicated in Fig. 2b) in SN and CD are shown. Total protein extracts (~100 μg) from SN (n = 18) and CD (n = 21) were spotted on nitrocellulose membrane followed by anti-3NT western blot. Following densitometric analysis, the average for each sample was plotted as mean ± SD followed by regression analysis. The r and P values for each region are shown. b Representative anti-3-NT blot of SN and CD tissue extracts with increasing age (arrows indicate the age in years (y) of each sample; flower brackets correspond to the triplicate for each sample) and the quantitative plots of anti-3-NT signal (normalized with β-tubulin signal as indicated in Fig. 2b) in SN and CD are shown
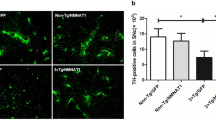
Since oxidative stress in SN dopaminergic neurons contribute to mitochondrial dysfunction in PD via selective inhibition of CI activity [46], we evaluated the CI activity in SN and CD during normal physiological aging. The CI activity was significantly decreased with increasing age in the SN in contrast to CD (SN: r = −0.45, P = 0.04; CD: r = 0.16, P = 0.26) (Fig. 2a) consistent with our earlier study on PD samples wherein striatal tissue displayed relatively unchanged CI activity compared to controls [24]. Similar to mitochondrial damage, neuroinflammation with microglial activation and reactive gliosis are evident during neuronal injury and PD with enhanced GFAP, an astroglial marker in the human mescencephalon [47]. We observed age-dependent increase in GFAP expression in SN but not in CD (SN: r = 0.88, P < 0.001; CD: r = 0.21, P = 0.20) (Fig. 2b). These data indicate a distinct biochemical and physiological distinction between SN and CD that might have direct implications in regional vulnerability during aging and neurodegeneration. We tested whether these regional differences could be due to altered antioxidant function in the nigrostriatal zones.
Quantitative analysis of mitochondrial complex I activity and GFAP in postmortem human SN (n = 18) and CD (n = 21) with increasing age. Mitochondria were prepared from different samples followed by CI assay. The average rotenone-sensitive CI activity for each sample was plotted as mean ± SD followed by regression analysis. The r and P values for each region are shown in a. Total extracts (50 μg) from different samples were spotted on nitrocellulose membrane with increasing age followed by anti-GFAP western blot. b shows a representative SDS PAGE profile of GFAP and β-tubulin in SN and CD (the age in years (y) of each sample is indicated) and dot blot of GFAP (with increasing age) in SN and CD (arrows in the slot blot indicate the age in years (y) of each sample; flower brackets correspond to the triplicate for each sample). Following densitometric analysis, the average for each sample was plotted as mean ± SD followed by regression analysis. The r and P values for each region are shown. Age-dependent alterations in GFAP signal (normalized with the respective β-tubulin signal) in SN and CD are also shown
In the brain samples, the SOD activity in SN was decreased by ~twofold compared to CD in all the samples. In the SN, there was a significant decrease in SOD activity with increasing age while in CD, the activity was relatively unaltered (SN: r = −0.54, P = 0.03; CD: r = −0.33, P = 0.10) (Fig. 3a). Catalase activity showed decreasing trend in the SN compared to CD although it was not statistically significant (SN: r = −0.39, P = 0.07; CD: r = −0.26, P = 0.15) (Fig. 3b). GSH is the most abundant antioxidant in the brain and its depletion is an early marker of oxidative stress in the SN in cases of PD [10, 48]. The total GSH was significantly lower in SN compared to CD which further decreased with increasing age although not to a statistically significant extent. In CD, GSH levels were unaltered with increasing age (SN: r = −0.36, P = 0.12; CD: r = 0.19, P = 0.21) (Fig. 3c). On the other hand, the activity of the antioxidant enzyme thioredoxin reductase was unaltered with increasing age in both SN and CD (Fig. 3d). But, the enzyme activity showed a trend different from the GSH with significantly higher activity in SN compared to CD (Fig. 3d) and this might be a compensatory mechanism for the GSH-mediated antioxidant activity.
Age-associated changes in the antioxidant activities in human postmortem brains. Total extracts from SN and CD samples were utilized for different antioxidant assays and the average for each sample was plotted as mean ± SD followed by regression analysis. The r and P values for each region are shown. a shows the scatter plot of SOD activity with increasing age in SN (n = 14) and CD (n = 19). b shows the comparison of age-dependent catalase activity in SN (n = 18) and CD (n = 21). c shows the comparison of age-dependent total GSH content in SN (n = 18) and CD (n = 14). d shows the quantitative comparison of Thioredoxin reductase activity in SN (n = 12) and CD (n = 18)
Other enzymes related to antioxidant function and GSH metabolism such as glutathione peroxidase (GPx) (SN: r = −0.66, P = 0.02; CD: r = 0.04, P = 0.44) and GSH reductase (GR) (SN: r = −0.62, P = 0.03; CD: r = 0.13, P = 0.30) showed significant decrease in activity in SN with increasing age and this might exacerbate the oxidative damage (Fig. 4a, b). However GPx and GR activities were relatively unaltered in CD with increasing age (Fig. 4a, b). On the other hand, GSH-S-transfease (GST) activity was found unaltered with increasing age both in SN and CD (Fig. 4c).
Analysis of GSH-associated enzymes in postmortem human brains with increasing age. Total extracts from SN and CD samples were utilized for different assays and the average for each sample was plotted as mean ± SD followed by regression analysis. The r and P values for each region are shown. a shows the GPx activity in SN (n = 12) and CD (n = 16) with increasing age. b Shows the GR activity in the SN (n = 12) and CD (n = 19) while c corresponds to the GST activity in SN (n = 12) and CD (n = 17)
Discussion
Although many biochemical studies have analyzed the SN and corpus striatum in the human samples and animal models of PD, studies in these regions during normal physiological aging are limited. The current study has attempted to provide mechanistic explanation that distinguishes SN and CD with increasing age with implications for the vulnerability to neurodegeneration. Our data showed that in the SN, there was significant protein oxidation and nitration with increasing age while it was relatively unchanged in CD (Fig. 1). This was consistent with the previous report [12] which observed twofold higher carbonyls in SN than in striatum and cortex of human brains. In a related study, comparison of lipid peroxidation in different regions of rat brain showed age-dependent increase only in midbrain while it decreased in the striatum [49]. On the other hand, Mizuno and Ohta [50] reported that lipid peroxidation was lower in caudate-putamen nuclei, and SN compared with other areas in adult rats but increased significantly with aging [50].
Ultrastructural and morphological analyses in human brains have demonstrated that during aging, SN dopaminergic neurons undergo apoptosis but this might be mechanistically different from the neuronal death during PD [51]. The selectivity of SN dopaminergic neurons for oxidative damage and degeneration during aging and PD might be due to specific mechanisms. One factor might be the opening of L-type calcium channels that causes continuous calcium influx into the SN neurons, resulting in mitochondrial oxidative stress and susceptibility to toxins. Epidemiological data also links the role of L-type calcium channels to the risk of developing PD [52]. Another contributing factor might be the selective expression of proteins such as D(2) dopamine autoreceptors, GIRK-2 potassium channels etc. and lack of expression of neuroprotective factors [53]. Previously, Waters and colleagues [54] linked alterations in peptide-containing pathways with neurodegeneration emphasizing the sensitivity of the alpha sub-layer of SN neurons in PD while Kish et al. [55] demonstrated that aging produces a specific pattern of striatal dopamine loss with implications for the etiology of idiopathic PD.
Irrespective of the mechanism, the oxidative damage in the SN that contributes to mitochondrial damage and neurodegeneration involves depletion of cellular GSH [56, 57]. While SN neurons during PD show GSH depletion [10], our previous study [24] showed that non-SN regions including CD and putamen in PD brains displayed threefold to fivefold increase in GSH which might protect mitochondria in these anatomical regions against oxidative damage. This could happen either by increased synthesis or leakage of intracellular GSH or by inhibition of extracellular breakdown of GSH. It is plausible that the degeneration of SN neurons might promote compensatory neuroprotective mechanisms by inducing increased GSH synthesis in the non-SN regions [58]. In this regard, regional differences during aging is important as the current study showed significantly lower GSH content in SN compared to CD, which decreased further with increasing age (Fig. 3c). Similarly, mitochondrial CI deficiency specific to SN in post mortem PD brain has been reported [46, 59]. This could be promoted by aging since CI activity was decreased in an age-dependent manner in the SN while it was unaltered in CD (Fig. 2).
Apart from GSH, other antioxidant activities are altered selectively in the SN. The antioxidant enzymes such as SOD, catalase, GPx and GR were found decreased in SN compared to CD (Figs. 3, 4). These deficiencies might exacerbate the oxidative damage induced by GSH depletion and might synergistically make SN vulnerable to neurodegeneration. All brain regions do not follow the same pattern of antioxidant function with increasing age [60]. Accordingly, the SOD and GPx activities did not change in CD while it increased in the mesencephalon; catalase activity decreased in CD. There are divergent reports in literature on the age-dependent alterations in antioxidant function in the brain. Carrillo et al. [61] demonstrated that the activities of Mn-SOD were significantly higher in the old male rats than in young males in SN, striatum and hippocampus but lower in the cerebellum. Further, activities of Cu Zn-SOD, catalase and GPx were relatively unaffected by age. In female rat brains, activities of Mn-SOD and other antioxidant enzymes were unaltered by aging. Benzi et al. [62] suggested the opposite trend and reported that in both SN and CD regions of rat brain, enzyme activity declines steadily with age. In both CD and parietotemporal cortex, the GPx activity increases from 5 to 20 months of age and remains relatively constant thereafter, while in SN, the enzyme activity is practically unmodified during the life span. The activity of GR in caudate-putamen deteriorates after an increase from 5 to 20 months of age. Mizuno and Ohta [50] reported significant reduction in SOD activity in CD and SN in rat brains with aging while the GPx and GR activities were highest in CD-putamen and in SN.
Neuroinflammation, microglial activation and astrocytic proliferation, with GFAP expression have been demonstrated during neuronal injury and PD [63, 64]. Whether microglial activation reflects progressive SN pathology and whether it is dependent on disease duration has to be determined. On the other hand, some reports have questioned whether astrocytic proliferation protects or exacerbates the SN neuron loss [47, 65]. In this regard, age-dependent alterations in GFAP expression might contribute to pathology during PD. Uchida et al. [66] reported that although the number of TH positive neurons in the SN is unaltered with increasing age, the ratio of TH-positive neurons to GFAP-positive glial cells slightly decreased with increasing age. O’Callaghan and Miller [67] reported an elevation in GFAP expression with age throughout the brain with the largest increase observed in corpus striatum. Consistent with some of these reports, we observed selective increase in GFAP expression with increasing age only in the SN but not in CD (Fig. 2b).
Some studies have linked astrocytic proliferation with exposure to toxins and injury in an age and gender dependent manner [68, 69]. Miller et al. [70] reported that the striatal dopamine depletion and GFAP elevation induced by amphetamines in mice was relatively higher in older animals. Based on the data from 6-OHDA administered rats, Gordon et al. [71] observed higher GFAP expression in older animals compared to younger animals indicating that aged astrocytes are more sensitive to gliotrophic factors released by degeneration. Further, there is sustained astrocytic proliferation in aged animals either due to a delay in the clearance of these factors or the inability to terminate GFAP inductions after activation. These data suggest that age-related glial hypersensitivity may independently increase the risk for some degenerative diseases [71].
Gender difference and the role of hormones are linked with the nigrostriatal pathway. This is very pertinent to the nigrostriatal pathology since PD has greater incidence in males compared to females [72]. It has been proposed that gender-specific hormones such as estrogen could significantly affect the function of the nigrostriatal dopaminergic pathway [73]. Estrogen has been linked with neuroprotective function in the brain. Administration of the PD toxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) to male mice resulted in oxidative damage, mitochondrial dysfunction and dopaminergic neurodegeneration in SN, whereas female mice were unaffected [74]. Pre-treatment of female mice with estrogen receptor (ER) antagonist sensitized them to MPTP-mediated toxicity. It was also demonstrated that downregulation of ER decreased the glutaredoxin activity in the midbrain and striatum of female mouse brain, indicating that glutaredoxin expression is regulated through ER signaling and higher glutaredoxin could provide neuroprotection [74]. On the other hand, there are reports in animal models describing either anti-dopaminergic effects or showing no significant effect on the nigrostriatal dopaminergic neurons [75]. Similarly, the role of estrogen in PD patients is controversial with studies showing both pro and anti-dopaminergic effects of estrogen [75]. It was reported that post-menopausal estrogen treatment was associated with a lower risk of PD compared with controls [76]. On the other hand, there are reports of improved dyskinesias or worsened parkinsonism symptoms in women administered with hormone replacement, indicating that estrogen may have an anti-dopaminergic effect [77, 78]. Considering these data, gender-based differences should be considered while investigating the age-dependent effects and toxin induced pathways in the nigrostriatal dopaminergic neurons.
In conclusion, our current study clearly demonstrates age-related alterations in the status of oxidant and antioxidant markers in the SN with implications for mitochondrial dysfunction and astrogial proliferation thus differentiating this region from the CD and explaining the vulnerability of SN to neurodegeneration in PD.
Abbreviations
- PD:
-
Parkinson’s disease
- SN:
-
Substantia nigra
- CI:
-
Mitochondrial complex I
- GSH:
-
Glutathione reduced
- PMI:
-
Postmortem interval
- CD:
-
Caudate nucleus
- 3-NT:
-
3-Nitrotyrosine
- GFAP:
-
Glial fibrillary acidic protein
- SOD:
-
Superoxide dismutase
- GST:
-
Glutathione-s-transferase
- GR:
-
Glutathione reductase
- GPx:
-
Glutathione peroxidase
References
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17:427–442
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Adams JD Jr, Chang ML, Klaidman L (2001) Parkinson’s disease—redox mechanisms. Curr Med Chem 8:809–814
Beal MF (1992) Does impairment of energy metabolism result in excitotoxic neuronal death in neurodegenerative illnesses? Ann Neurol 31:119–130. doi:10.1002/ana.410310202
Jenner P, Dexter DT, Sian J, Schapira AH, Marsden CD (1992) Oxidative stress as a cause of nigral cell death in Parkinson’s disease and incidental Lewy body disease. The Royal Kings and Queens Parkinson’s Disease Research Group. Ann Neurol 32(Suppl):S82–S87
Koiliatsos VE (1998) Parkinson’s disease. In: Burke RE (ed) Cell death and disease of the nervous system. Humana Press, Totowa, pp 459–475
Sayre LM, Smith MA, Perry G (2001) Chemistry and biochemistry of oxidative stress in neurodegenerative disease. Curr Med Chem 8:721–738
Dexter DT, Wells FR, Lees AJ, Agid F, Agid Y, Jenner P, Marsden CD (1989) Increased nigral iron content and alterations in other metal ions occurring in brain in Parkinson’s disease. J Neurochem 52:1830–1836
Sofic E, Paulus W, Jellinger K, Riederer P, Youdim MB (1991) Selective increase of iron in substantia nigra zona compacta of parkinsonian brains. J Neurochem 56:978–982
Bharath S, Hsu M, Kaur D, Rajagopalan S, Andersen JK (2002) Glutathione, iron and Parkinson’s disease. Biochem Pharmacol 64:1037–1048
Alam ZI, Daniel SE, Lees AJ, Marsden DC, Jenner P, Halliwell B (1997) A generalised increase in protein carbonyls in the brain in Parkinson’s but not incidental Lewy body disease. J Neurochem 69:1326–1329
Floor E, Wetzel MG (1998) Increased protein oxidation in human substantia nigra pars compacta in comparison with basal ganglia and prefrontal cortex measured with an improved dinitrophenylhydrazine assay. J Neurochem 70:268–275
Good PF, Hsu A, Werner P, Perl DP, Olanow CW (1998) Protein nitration in Parkinson’s disease. J Neuropathol Exp Neurol 57:338–342
Blanchard-Fillion B, Prou D, Polydoro M, Spielberg D, Tsika E, Wang Z, Hazen SL, Koval M, Przedborski S, Ischiropoulos H (2006) Metabolism of 3-nitrotyrosine induces apoptotic death in dopaminergic cells. J Neurosci 26:6124–6130. doi:10.1523/JNEUROSCI.1038-06.2006
Danielson SR, Andersen JK (2008) Oxidative and nitrative protein modifications in Parkinson’s disease. Free Radic Biol Med 44:1787–1794. doi:10.1016/j.freeradbiomed.2008.03.005
Ferrante RJ, Hantraye P, Brouillet E, Beal MF (1999) Increased nitrotyrosine immunoreactivity in substantia nigra neurons in MPTP treated baboons is blocked by inhibition of neuronal nitric oxide synthase. Brain Res 823:177–182
Hasegawa E, Takeshige K, Oishi T, Murai Y, Minakami S (1990) 1-Methyl-4-phenylpyridinium (MPP+) induces NADH-dependent superoxide formation and enhances NADH-dependent lipid peroxidation in bovine heart submitochondrial particles. Biochem Biophys Res Commun 170:1049–1055
Ischiropoulos H, Beckman JS (2003) Oxidative stress and nitration in neurodegeneration: cause, effect, or association? J Clin Invest 111:163–169
Pennathur S, Jackson-Lewis V, Przedborski S, Heinecke JW (1999) Mass spectrometric quantification of 3-nitrotyrosine, ortho-tyrosine, and o, o′-dityrosine in brain tissue of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-treated mice, a model of oxidative stress in Parkinson’s disease. J Biol Chem 274:34621–34628
Keeney PM, Xie J, Capaldi RA, Bennett JP Jr (2006) Parkinson’s disease brain mitochondrial complex I has oxidatively damaged subunits and is functionally impaired and misassembled. J Neurosci 26:5256–5264. doi:10.1523/JNEUROSCI.0984-06.2006
Schapira AH, Cooper JM, Dexter D, Clark JB, Jenner P, Marsden CD (1990) Mitochondrial complex I deficiency in Parkinson’s disease. J Neurochem 54:823–827
Rogers J, Mastroeni D, Leonard B, Joyce J, Grover A (2007) Neuroinflammation in Alzheimer’s disease and Parkinson’s disease: are microglia pathogenic in either disorder? Int Rev Neurobiol 82:235–246
Werner CJ, Heyny-von Haussen R, Mall G, Wolf S (2008) Proteome analysis of human substantia nigra in Parkinson’s disease. Proteome Sci 6:8
Mythri RB, Venkateshappa C, Harish G, Mahadevan A, Muthane UB, Yasha TC, Srinivas Bharath MM, Shankar SK (2011) Evaluation of markers of oxidative stress, antioxidant function and astrocytic proliferation in the striatum and frontal cortex of Parkinson’s disease brains. Neurochem Res 36:1452–1463. doi:10.1007/s11064-011-0471-9
Karunakaran S, Saeed U, Ramakrishnan S, Koumar RC, Ravindranath V (2007) Constitutive expression and functional characterization of mitochondrial glutaredoxin (Grx2) in mouse and human brain. Brain Res 1185:8–17. doi:10.1016/j.brainres.2007.09.019
Karunakaran S, Saeed U, Mishra M, Valli RK, Joshi SD, Meka DP, Seth P, Ravindranath V (2008) Selective activation of p38 mitogen-activated protein kinase in dopaminergic neurons of substantia nigra leads to nuclear translocation of p53 in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-treated mice. J Neurosci 28:12500–12509. doi:10.1523/jneurosci.4511-08.2008
Alladi PA, Mahadevan A, Yasha TC, Raju TR, Shankar SK, Muthane U (2009) Absence of age-related changes in nigral dopaminergic neurons of Asian Indians: relevance to lower incidence of Parkinson’s disease. Neuroscience 159:236–245. doi:10.1016/j.neuroscience.2008.11.051
Chinta SJ, Kommaddi RP, Turman CM, Strobel HW, Ravindranath V (2005) Constitutive expression and localization of cytochrome P-450 1A1 in rat and human brain: presence of a splice variant form in human brain. J Neurochem 93:724–736. doi:10.1111/j.1471-4159.2005.03061.x
Agarwal V, Kommaddi RP, Valli K, Ryder D, Hyde TM, Kleinman JE, Strobel HW, Ravindranath V (2008) Drug metabolism in human brain: high levels of cytochrome P4503A43 in brain and metabolism of anti-anxiety drug alprazolam to its active metabolite. PLoS One 3:e2337. doi:10.1371/journal.pone.0002337
Chandana R, Mythri RB, Mahadevan A, Shankar SK, Srinivas Bharath MM (2009) Biochemical analysis of protein stability in human brain collected at different post-mortem intervals. Indian J Med Res 129:189–199
Alladi PA, Mahadevan A, Shankar SK, Raju TR, Muthane U (2010) Expression of GDNF receptors GFRalpha1 and RET is preserved in substantia nigra pars compacta of aging Asian Indians. J Chem Neuroanat 40:43–52. doi:10.1016/j.jchemneu.2010.03.007
Alladi PA, Mahadevan A, Vijayalakshmi K, Muthane U, Shankar SK, Raju TR (2010) Ageing enhances alpha-synuclein, ubiquitin and endoplasmic reticular stress protein expression in the nigral neurons of Asian Indians. Neurochem Int 57:530–539. doi:10.1016/j.neuint.2010.06.018
Jagatha B, Mythri RB, Vali S, Bharath MM (2008) Curcumin treatment alleviates the effects of glutathione depletion in vitro and in vivo: therapeutic implications for Parkinson’s disease explained via in silico studies. Free Radic Biol Med 44:907–917. doi:10.1016/j.freeradbiomed.2007.11.011
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126
Bagnyukova TV, Storey KB, Lushchak VI (2003) Induction of oxidative stress in Rana ridibunda during recovery from winter hibernation. J Therm Biol 28:21–28
Tietze F (1969) Enzymic method for quantitative determination of nanogram amounts of total and oxidized glutathione: applications to mammalian blood and other tissues. Anal Biochem 27:502–522
Flohe L, Gunzler WA (1984) Assays of glutathione peroxidase. Methods Enzymol 105:114–121
Carlberg I, Mannervik B (1985) Glutathione reductase. Methods Enzymol 113:484–490
Guthenberg C, Alin P, Mannervik B (1985) Glutathione transferase from rat testis. Methods Enzymol 113:507–510
Mythri RB, Jagatha B, Pradhan N, Andersen J, Bharath MM (2007) Mitochondrial complex I inhibition in Parkinson’s disease: how can curcumin protect mitochondria? Antioxid Redox Signal 9:399–408. doi:10.1089/ars.2007.9.ft-25
Trounce IA, Kim YL, Jun AS, Wallace DC (1996) Assessment of mitochondrial oxidative phosphorylation in patient muscle biopsies, lymphoblasts, and transmitochondrial cell lines. Methods Enzymol 264:484–509
Albers DS, Beal MF (2000) Mitochondrial dysfunction and oxidative stress in aging and neurodegenerative disease. J Neural Transm Suppl 59:133–154
Banerjee R, Starkov AA, Beal MF, Thomas B (2009) Mitochondrial dysfunction in the limelight of Parkinson’s disease pathogenesis. Biochim Biophys Acta 1792:651–663. doi:10.1016/j.bbadis.2008.11.007
Lin MT, Beal MF (2006) Mitochondrial dysfunction and oxidative stress in neurodegenerative diseases. Nature 443:787–795. doi:10.1038/nature05292
Schapira AH, Cooper JM, Dexter D, Jenner P, Clark JB, Marsden CD (1989) Mitochondrial complex I deficiency in Parkinson’s disease. Lancet 1:1269
Damier P, Hirsch EC, Zhang P, Agid Y, Javoy-Agid F (1993) Glutathione peroxidase, glial cells and Parkinson’s disease. Neuroscience 52:1–6
Jenner P (1993) Altered mitochondrial function, iron metabolism and glutathione levels in Parkinson’s disease. Acta Neurol Scand 146(Suppl):6–13
Kolosova NG, Shcheglova TV, Amstislavskaya TG, Loskutova LV (2003) Comparative analysis of LPO products in brain structures of Wistar and OXYS rats of different age. Bull Exp Biol Med 135:593–596
Mizuno Y, Ohta K (1986) Regional distributions of thiobarbituric acid-reactive products, activities of enzymes regulating the metabolism of oxygen free radicals, and some of the related enzymes in adult and aged rat brains. J Neurochem 46:1344–1352
Anglade P, Vyas S, Hirsch EC, Agid Y (1997) Apoptosis in dopaminergic neurons of the human substantia nigra during normal aging. Histol Histopathol 12:603–610
Surmeier DJ, Guzman JN, Sanchez-Padilla J, Goldberg JA (2011) The origins of oxidant stress in Parkinson’s disease and therapeutic strategies. Antioxid Redox Signal 14:1289–1301. doi:10.1089/ars.2010.3521
Double KL, Reyes S, Werry EL, Halliday GM (2010) Selective cell death in neurodegeneration: why are some neurons spared in vulnerable regions? Prog Neurobiol 92:316–329. doi:10.1016/j.pneurobio.2010.06.001
Waters CM, Peck R, Rossor M, Reynolds GP, Hunt SP (1988) Immunocytochemical studies on the basal ganglia and substantia nigra in Parkinson’s disease and Huntington’s chorea. Neuroscience 25:419–438
Kish SJ, Shannak K, Rajput A, Deck JH, Hornykiewicz O (1992) Aging produces a specific pattern of striatal dopamine loss: implications for the etiology of idiopathic Parkinson’s disease. J Neurochem 58:642–648
Riederer BM (1989) Antigen preservation tests for immunocytochemical detection of cytoskeletal proteins: influence of aldehyde fixatives. J Histochem Cytochem 37:675–681
Sofic E, Lange KW, Jellinger K, Riederer P (1992) Reduced and oxidized glutathione in the substantia nigra of patients with Parkinson’s disease. Neurosci Lett 142:128–130
Frade J, Pope S, Schmidt M, Dringen R, Barbosa R, Pocock J, Laranjinha J, Heales S (2008) Glutamate induces release of glutathione from cultured rat astrocytes—a possible neuroprotective mechanism? J Neurochem 105:1144–1152. doi:10.1111/j.1471-4159.2008.05216.x
Mann VM, Cooper JM, Daniel SE, Srai K, Jenner P, Marsden CD, Schapira AH (1994) Complex I, iron, and ferritin in Parkinson’s disease substantia nigra. Ann Neurol 36:876–881. doi:10.1002/ana.410360612
Ciriolo MR, Fiskin K, De Martino A, Corasaniti MT, Nistico G, Rotilio G (1991) Age-related changes in Cu, Zn superoxide dismutase, Se-dependent and -independent glutathione peroxidase and catalase activities in specific areas of rat brain. Mech Ageing Dev 61:287–297
Carrillo MC, Kanai S, Sato Y, Kitani K (1992) Age-related changes in antioxidant enzyme activities are region and organ, as well as sex, selective in the rat. Mech Ageing Dev 65:187–198
Benzi G, Pastoris O, Marzatico F, Villa RF (1989) Cerebral enzyme antioxidant system. Influence of aging and phosphatidylcholine. J Cereb Blood Flow Metab 9:373–380
McGeer PL, Itagaki S, Boyes BE, McGeer EG (1988) Reactive microglia are positive for HLA-DR in the substantia nigra of Parkinson’s and Alzheimer’s disease brains. Neurology 38:1285–1291
Banati RB, Daniel SE, Blunt SB (1998) Glial pathology but absence of apoptotic nigral neurons in long-standing Parkinson’s disease. Mov Disord 13:221–227. doi:10.1002/mds.870130205
Lin LF, Doherty DH, Lile JD, Bektesh S, Collins F (1993) GDNF: a glial cell line-derived neurotrophic factor for midbrain dopaminergic neurons. Science 260:1130–1132
Uchida K, Kihara N, Hashimoto K, Nakayama H, Yamaguchi R, Tateyama S (2003) Age-related histological changes in the canine substantia nigra. J Vet Med Sci 65:179–185
O’Callaghan JP, Miller DB (1991) The concentration of glial fibrillary acidic protein increases with age in the mouse and rat brain. Neurobiol Aging 12:171–174
Castillo-Ruiz MM, Campuzano O, Acarin L, Castellano B, Gonzalez B (2007) Delayed neurodegeneration and early astrogliosis after excitotoxicity to the aged brain. Exp Gerontol 42:343–354. doi:10.1016/j.exger.2006.10.008
Ciesielska A, Joniec I, Kurkowska-Jastrzebska I, Cudna A, Przybylkowski A, Czlonkowska A, Czlonkowski A (2009) The impact of age and gender on the striatal astrocytes activation in murine model of Parkinson’s disease. Inflamm Res 58:747–753. doi:10.1007/s00011-009-0026-6
Miller DB, O’Callaghan JP, Ali SF (2000) Age as a susceptibility factor in the striatal dopaminergic neurotoxicity observed in the mouse following substituted amphetamine exposure. Ann N Y Acad Sci 914:194–207
Gordon MN, Schreier WA, Ou X, Holcomb LA, Morgan DG (1997) Exaggerated astrocyte reactivity after nigrostriatal deafferentation in the aged rat. J Comp Neurol 388:106–119
Dluzen DE, Disshon KA, McDermott JL (1998) Estrogen as a modulator of striatal dopaminergic neurotoxicity. In: Marwah J, Teitelbaum H (eds) Advances in neurodegenerative disorders, vol 1: Parkinson’s disease. Prominent Press, Scottsdale, pp 149–192
Lichtensteiger W (1969) Cyclic variations of catecholamine content in hypothalamic nerve cells during the estrous cycle of the rat, with a concomitant study of the substantia nigra. J Pharmacol Exp Ther 165:204–215
Kenchappa RS, Diwakar L, Annepu J, Ravindranath V (2004) Estrogen and neuroprotection: higher constitutive expression of glutaredoxin in female mice offers protection against MPTP-mediated neurodegeneration. FASEB J 18:1102–1104
Liu B, Dluzen DE (2007) Oestrogen and nigrostriatal dopaminergic neurodegeneration: animal models and clinical reports of Parkinson’s disease. Clin Exp Pharmacol Physiol 34:555–565
Currie LJ, Harrison MB, Trugman JM, Bennett JP, Wooten GF (2004) Postmenopausal estrogen use affects risk for Parkinson disease. Arch Neurol 61:886–888
Bedard P, Langelier P, Villeneuve A (1977) Oestrogens and extrapyramidal system. Lancet 2:1367–1368
Koller WC, Barr A, Biary N (1982) Estrogen treatment of dyskinetic disorders. Neurology 32:547–549
Acknowledgments
This work was financially supported by a research grant from the Indian Council of Medical Research (ICMR IRIS ID No. 2009-07710), India, to MMSB. GH is a senior research fellow of ICMR, India. RM was supported by a senior research fellowship (extended) from Council of Scientific and Industrial Research (CSIR), India. VC gratefully acknowledges the financial support from Sri Siddhartha Medical College, Tumkur, Karnataka, India. We thank all the donors and their relatives for donating human brain tissue samples for this study. Human brain tissues for the study were sourced from Human Brain Tissue Repository for Neurobiological Studies (A National Research Facility), Department of Neuropathology, NIMHANS, Bangalore—560 029.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Venkateshappa, C., Harish, G., Mythri, R.B. et al. Increased Oxidative Damage and Decreased Antioxidant Function in Aging Human Substantia Nigra Compared to Striatum: Implications for Parkinson’s Disease. Neurochem Res 37, 358–369 (2012). https://doi.org/10.1007/s11064-011-0619-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-011-0619-7