Abstract
Lectins are proteins capable of reversible binding to carbohydrates or glycoconjugates. In the central nervous system of mammals, lectins with affinity for mannose/glucose or galactose can modulate cellular communication. ConBr, a lectin isolated from the seeds of Canavalia brasiliensis, previously showed antidepressant effect in the forced swimming test in mice, with involvement of the monoaminergic system. In this study, we investigated the neuroprotective effects of ConBr against quinolinic acid (QA), a well-known NMDA agonist that produces severe neurotoxicity when administered in vivo. ConBr (10 μg/site) administered via intracerebroventricular (i.c.v.) showed a neuroprotective activity against seizures induced by QA (36.8 nmol/site; i.c.v.) when administered 15 min prior to QA, with a percentage of protection around 50%. ConBr was also able to significantly decrease the severity of the seizures but without changes in the latency of the first convulsion or the duration of the seizures. This effect was dependent on the structural integrity of the ConBr protein and its binding capacity to oligosaccharides residues. ConA, a lectin with high similarity to ConBr, did not reverse the QA-induced seizures. Moreover, ConBr was able to protect against hippocampal cell death caused by QA, which was measured by propidium iodide incorporation. QA caused activation of JNK2 and improved the phosphorylation of Ser831 and 845 on the AMPA receptor GluR1 subunit, and both of these effects were counteracted by ConBr. Our data suggest that the lectin ConBr may exert a modulatory action on NMDA receptors, which inhibits its activity in response to QA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glycoproteins are prominent constituents of biological membranes involved in various distinct functions, including ion transport, cell adhesion, molecular recognition and structural support [1, 2]. In the nervous system, the glycan chains covalently attached to asparagine or serine/threonine residues, present in the receptors and neurotransmitter transporters, exhibit a recognized modulatory function on neurotransmission and synaptic plasticity [3].
Glutamate is the principal mediator in the central nervous system (CNS) because approximately 80% of all synapses are glutamatergic. Glutamate acts through two main receptor categories: ionotropic receptors that are cation channels and metabotropic receptors that can modulate intracellular enzymes via G proteins [4]. Ionotropic glutamate receptors (iGluRs) are the prevalent excitatory neurotransmitter receptors in the CNS. They can be classified into three major subfamilies on the basis of pharmacological and electrophysiological profiles: N-methyl-D-aspartate (NMDA), α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA) and kainate (KA) receptors. All of these receptors are macromolecular glycoprotein complexes composed of various subunits exhibiting distinct structures, and glycosylation accounts for 8–24% of the total molecular weight of these receptors [5]. Therefore, members of the iGluR family have between 4 and 12 consensus asparagine (N)-linked glycosylation sites, which are localized at the extracellular N-terminal domain in a region that also contains essential elements for the formation of the ligand-binding groove. Moreover, ligand binding affinity, receptor physiology, susceptibility to allosteric modulation and, in some cases, trafficking may be dependent on the glycosylation state [6].
NMDARs are mainly Ca2+ channels that are gated by glutamate, and these are essential mediators of many forms of synaptic transmission and plasticity. NMDARs are tetramers composed of two NR1 subunits plus two NR2 subunits: NR2A, NR2B, NR2C and NR2D [7, 8]. In CA1 pyramidal cells, NMDARs contain mainly NR2A and/or NR2B subunits, in addition to NR1 [8]. Glycosylation of the NMDA receptors is extensive; for example, considering the molecular weight of 120 kDa for NR1 and 180 kDa for the NR2B subunit, about 20 kDa of this weight consists of sugars for these subunits and about 10 kDa for the other NR2 subunits moieties [9, 10].
Overall, it is evident that glycosylation influences various properties of the glutamate receptors, including the activity of the channel, the binding of ligands and its modulation by lectins.
Lectins are carbohydrate-binding proteins of non-immune origin that display no enzymatic activity toward the recognized sugars. Lectins can be found in all kingdoms of life including viruses, bacteria, plants and animals. Therefore, lectins are a highly diverse group of proteins with diverse biological functions associated with carbohydrate-binding activities [11–13].
Legume lectins are a large group of structurally similar proteins with distinct carbohydrate specificities [11]. The concanavalin A (ConA) lectin, obtained from the seeds of Canavalia ensiformis (Leguminosae Family, Phaseoleae tribe, Diocleinae subtribe), was the first lectin to be isolated [14] and sequenced, and its structure has been determined by three-dimensional X-ray crystallography [15–17]. Therefore, ConA has been extensively studied and characterized with respect to its structure and biological effects on different systems. In the mammalian nervous system, ConA has been used to study neuroplasticity [18–20], to isolate synaptic glutamate receptors [21–23] and to study the biochemical and functional properties of the ionotropic glutamate receptors AMPA [24, 25], Kainato [23, 26–28] and NMDA [26, 29]. In these studies, the consensus was that ConA could potentiate current responses of native and recombinant iGluRs, at least in part by inhibition of receptor desensization.
ConBr, a lectin isolated from the seeds of Canavalia brasiliensis, has had its crystallographic structure defined, shares 99% amino acid sequence identity with ConA and has the same specificity as ConA for glucose/mannose [30].
We demonstrated previously that ConBr (but not ConA) was capable of producing a behavioral modulation predictive of antidedepressive action in mice (assessed by the forced swimming test; TNF) when injected into the lateral ventricle [31]. Additionally, ConBr shares mechanisms of action similar to the classic antidepressants that modulate the serotoninergic, noradrenergic and dopaminergic systems [31]. Despite all of these findings, modulation of the glutamatergic system by ConBr has not yet assessed.
It is well known that excessive glutamate in the synaptic cleft causes neuronal dysfunction and degeneration, and it has been implicated in many pathological processes such as ischemia, traumatic brain injury, seizures and chronic neurodegenerative diseases [4]. The consensus is that the excessive Ca2+ influx via NMDAR is a key event leading to glutamate excitotoxicity [4, 32].
Glutamatergic excitotoxicity has been studied using a variety of in vivo models, including the central administration of quinolinic acid (QA), which has been described as a model of excitotoxicity because it causes over-stimulation of NMDARs [33, 34], causes seizures, stimulates glutamate uptake into synaptic vesicles [35] and increases glutamate release [36].
Taken together, it is evident that the NMDA receptor is a glycoprotein involved in excitotoxicity that could be a potential target for the mannose/glucose-specific lectin, ConBr. Therefore, this study was designed to investigate the possible in vivo interaction between centrally administered ConBr and the neurotoxicity produced by the NMDA agonist, quinolinic acid.
Experimental Procedure
Chemicals
The primary antibodies anti-phospho AMPA Ser845, anti-phospho AMPA Ser831, anti-JNK1/2, anti-ERK1/2 and anti-phospho-ERK1/2 were purchased from Sigma (St. Louis, MO, USA). Anti-β-actin was bought from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Anti-AMPA (total) was purchased from Millipore (Billerica, MA, USA). Anti-AKT and anti-phospho-AKT and anti–phospho-JNK1/2/3 antibodies were purchased from Cell Signaling (Beverly, MA, USA). Acrylamide, bis-acrylamide, β-mercaptoethanol, Hybond™ nitrocellulose, Hyperfilm™ ECL, sodium dodecyl sulfate (SDS), Tris, secondary antibody [anti-rabbit IgG-horse radish peroxidase (HRP)-conjugated] and ECL™ detection reagents were obtained from GE Healthcare Life Sciences (Piscataway, NJ, USA). Quinolinic acid (QA) was purchased from Sigma (St. Louis, MO, USA).
Animals
Male adult Swiss albino mice (30–40 g) were maintained on a 12 h light/12 h dark schedule at 25°C. Mice were housed in plastic cages with food and water available ad libitum. All experiments were designed to minimize animal suffering and to limit the number of animals used, and this study was approved by the local Ethical Committee for Animal Research.
Purification of Lectins
The C. brasiliensis lectin (ConBr) [37] and C. ensiformis lectin (ConA) [14] were isolated by affinity chromatography. Briefly, mature seeds were collected at Ceará state, Northeast Brazil. The seeds were ground into a fine powder in a coffee mill and then defatted with n-hexane. Soluble proteins were extracted at 20°C for 4 h by continuous stirring with 0.9% NaCl (1:10 w/v), followed by centrifugation at 10,000g at 4°C for 20 min. The supernatant was applied to a Sephadex G-50 column (5 × 25 cm), which had been equilibrated with 0.9% NaCl containing 5 mmol l−1 CaCl2 and MnCl2. The column was then washed with equilibration buffer at a flow rate of 45 mL h−1 until the effluent absorbance at 280 nm was below 0.05. The bound lectin was eluted with 0.1 mol l−1 glycine, at pH 2.6, dialyzed extensively with distilled water and lyophilized. The affinity chromatography fraction was further purified using an Äkta chromatographic system and Mono-Q column (5 × 0.5 cm) equilibrated with 20 mmol l−1 Tris–HCl at pH 7.0 and developed with a linear gradient of 20 mmol l−1 Tris–HCl pH 7.0 containing 1.0 mol l−1 NaCl at a flow rate of 1 mL min−1 and a slope of 5% NaCl/min. The lectin preparations, recovered in the unbound fraction, were exhaustively dialyzed with distilled water and freeze-dried. The purity of the lectins was assessed by SDS–PAGE.
Surgical Procedure
Animals were anesthetized with sodium thiopental (60 mg/kg; 10 mL/kg; i.p.). Stereotaxic surgery and infusion techniques were used as previously described by Schmidt et al. [38]. Briefly, in a stereotaxic apparatus, the skin of the skull was removed, and a 27-gauge/7-mm guide cannula was placed 1 mm posterior to the bregma, 1 mm to the right of the midline and 1 mm above the lateral brain ventricle. The guide cannula was implanted 1.5 mm ventral to the superior surface of the skull and fixed with jeweler acrylic cement. The tip of the 30-gauge infusion cannula protruded 1 mm beyond the guide cannula, aiming towards the lateral ventricle. Methylene blue (4 μL) was injected through the cannula to confirm the effectiveness of the infusions. Animals without contrast in the lateral brain ventricle were discarded.
ConBr and QA Infusion
ConBr or ConA was diluted with HEPES–saline buffer without glucose (NaCl 124 mM, KCl 4 mM, MgSO4 1.2 mM, HEPES 25 mM, CaCl2 1 mM, pH 7.4) to a final concentration of 3.3 mg/mL. To determine if ConBr action depends on the protein structural integrity, ConBr was denatured by boiling for 5 min (90°C). In order to block the carbohydrate recognition domain (CRD) on the lectin, ConBr (3.3 mg/mL) was dissolved in Hepes saline buffer containing 0.1 M of its specific sugar (α-methyl-D-mannoside) and maintained for 30 min at 37°C prior to performing the experiments. Animals were pretreated via i.c.v. with ConBr at a concentration of 0.1, 1 or 10 μg/site (volume 3.0 μL) or with vehicle (3.0 μL of HEPES-saline buffer without glucose) 48 h after the cannula implantation. The chemical seizures were induced by QA infusion (4 μL of a 9.2 mM solution; i.c.v.) [38] administered 15 min after the lectin infusion. Mice were observed for 10 min for the occurrence of wild running and clonic, tonic, or tonic–clonic seizures lasting for more than 5 s. Mice not displaying seizures during these 10 min were considered protected.
A quantitative scale [39, 40] was used to evaluate QA-induced seizure severity: 0 = no response; 1 = imobility and excessive grooming plus paroxysmal scratching; 2 = circling and rearing; 3 = wild running; 4 = jumping and falling; 5 = forepaw clonus and tailhypertonus; 6 = generalized tonic–clonic convulsions; and 7 = generalized tonic convulsion and death. The latency and duration of generalized clonic or tonic–clonic convulsions seizures were also determined.
Preparation of Hippocampal Slices
Preparation of hippocampal slices was performed as previously described by Cordova et al. and Molz et al. [41, 42], with adaptations. Briefly, brains were removed and hippocampi dissected (4°C) in cutting buffer (60 mM NaCl, 3 mM KCl, 7 mM MgSO4, 25 mM HEPES, 1.25 mM KH2PO4, 5 mM d-glucose, 110 mM sacarose and 0.5 mM CaCl2, at pH 7.4) that was previously gasified with O2. Hippocampal slices of 400 μm thickness were prepared using a McIlwain Tissue Chopper, and they were individually preincubated for 30 min (300 μL/slice) with Krebs–Ringer buffer (KRB; 120 mM NaCl, 2 mM KCl, 1.2 mM MgSO4, 26 mM NaHCO3, 1.18 mM KH2PO4, 11 mM d-glucose and 1 mM CaCl2) bubbled with 95% O2/5% CO2 up to pH 7.4.
Propidium Iodide (PI) Uptake
Neuronal degeneration was monitored and quantified by densitometric measurement of the cellular uptake of PI (Sigma), a polar compound that only enters dead or dying cells with a damaged cell membrane. Inside the cells, PI binds to nucleic acid and emits a red fluorescence (630 nm) when excited with green light (495 nm). In the present experiments, four hippocampal slices were obtained from each mouse, including the control, ConBr-, quinolinic acid or ConBr plus quinolinic acid-treated mice. The slices were preincubated as described previously, followed by incubation for 30 min at 37°C with PI (7 mg/mL in KRB). Thereafter, the slices were washed with KRB for analysis on a standard inverted microscope (Olympus IX 71) using a rhodamine filter set. Viability analysis was performed in six independent experiments. Therefore, the results represent a mean ± SEM for six experiments performed in quadruplicate. The pictures were taken with an Olympus C5060 camera. The PI uptake was quantified by densitometric analysis with Scion Image software (http://www.scioncorp.com). The area where PI fluorescence (in pixels) was detectable above the background (damaged area of hippocampal slices) was analyzed using the ‘‘density slice’’ option of the Scioncorp software through the division of PI fluorescence by the total area of the slice [43].
Western Blotting
The hippocampi were dissected in the cutting buffer and mechanically homogenized (4°C) in 500 μL of Tris–base 50 mM at pH 7.0, EDTA 1 mM, NaF 100 mM, PMSF 0.1 mM, and Na3VO4 2 mM and then centrifuged (13,000g for 10 min at 4°C) to eliminate cellular debris [44]. The supernatants were individually diluted 1/1 (v/v) with electrophoresis sample buffer for a final concentration of Tris 50 mM (at pH 6.8), EDTA 2 mM, SDS 4%, and glycerol 8%. The protein content was estimated with the method described by Peterson [45], and the concentration was calculated by a pattern curve with bovine serum albumin. Each sample (60 μg of total protein/track) was electrophoresed on 10% SDS–PAGE minigels after addition of 0.2% bromophenol blue and 5% β-mercaptoethanol [41]. The proteins were then transferred to a nitrocellulose membrane using a semidry blotting apparatus (TE 70 SemiPhor™ Unit, GE Healthcare Life Sciences, Piscataway, NJ, USA) (1.2 mA/cm2; 1.5 h), as described by Bjerrum and Heegaard [46], with adaptations [47]. The membranes were blocked (1 h) with 5% skim milk in TBS (10 mM Tris, 150 mM NaCl, at pH 7.5). The GluR1 subunit of the AMPA receptor and ERK1/2 and JNK1/2 total and phosphorylated forms were detected using specific antibodies diluted in TBS-T (10 mM Tris, 150 mM NaCl, 0.1% Tween-20, pH 7.5) containing 2.5% BSA in the dilutions: 1:1,000 (anti-AMPA and anti-phospho AMPA-Ser831 and -Ser845, anti-phospho AKT-serine 473, anti-phospho JNK1/2/3); 1:10,000 (anti-phospho ERK1/2 and anti-total-JNK1/2); and 1:40,000 (anti-total-ERK1/2). Thereafter, the membranes were incubated with anti-rabbit or anti-mouse peroxidase-linked secondary antibody (1:4,000) for 1 h, and the reactions were developed by ECL. All steps of blocking and incubation were followed by three times washing (5 min) of the membranes with TBS-T. The optical density (OD) of the bands was quantified using Scion Image™ (Frederick, MD, USA). The phosphorylation level of each protein was determined as a ratio of OD of the phosphorylated band/OD of the total band. The data are expressed as percentage of the control (considered to be 100%), and the values are presented as mean ± SEM [48].
Statistical Analyses
Data are reported as mean ± SEM. Statistical analyses were performed using a one-way analysis of variance (ANOVA) and applying the Duncan’s test for post-hoc comparison when appropriate, except for evaluation of seizures, whereby the Fisher’s exact test was used. A value of P < 0.05 was considered to be significant.
Results
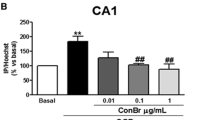
The results depicted in Fig. 1a show that the ConBr (10 μg/site) administrated 15 min before QA infusion provided 54% protection against the incidence of seizures induced by QA. Moreover, in the animals in which ConBr administration did not provide protection against seizures, ConBr caused a statistically significant decrease in the severity of the seizures (Fig. 1b). ConBr treatment had no effect either on latency for seizures or duration of seizures (Table 1). ConBr (1 μg/site) did not exert a protective effect against seizures induced by QA (Fig. 1a, b). In addition, there were no apparent behavioral changes in response to the administration of ConBr alone 1 or 10 μg/site (data not shown).
a Neuroprotective effect of ConBr lectin against seizures induced by quinolinic acid (QA) in mice. b Evaluation of the effect of ConBr against the severity of seizures induced by QA. ConBr (1 or 10 μg/site, i.c.v.) was administered via i.c.v. 15 min prior to QA (4 μL of a 9.2 mM solution; i.c.v.) administration. Mouse behavior was monitored for 10 min. The results represent the percentage of tonic-clonic seizures, **P < 0.01 compared with the control group (vehicle + QA)
Another important question that we addressed was whether or not the ConBr action against seizures induced by QA depended upon the integrity of the tertiary/quaternary protein structure. Figure 2 shows that denaturation of ConBr blocked its effect. In order to investigate if the neuroprotective effect of ConBr was dependent on the carbohydrate-binding domain (CRD), ConBr was incubated with mannose (100 mM) to block its CRD. Figure 2 shows that ConBr previously blocked by mannose lost its protective effects against the incidence of seizures induced by QA.
Evaluation of the neuroprotective effects of ConBr denatured and ConBr-blocked with mannose (100 mM) against seizures induced by QA. ConBr (10 μg/site, i.c.v.) was administered 15 min prior to QA (4 μL of a 9.2 mM solution; i.c.v.) administration. Mouse behavior was monitored for 10 min. The results represent the percentage of tonic-clonic seizures, **P < 0.01 compared with the control group (vehicle + QA)
ConA and ConBr are lectins belonging to the subtribe Diocleinae that share extensive amino acid sequence similarity but exhibit differences in multimeric structures [30]. The results depicted in Fig. 3 show the comparison of the effects of ConA and ConBr on the incidence of seizures induced by QA. Unlike ConBr, ConA (10 μg/site) administrated 15 min prior to QA infusion did not protect against seizures induced by QA.
Comparison of the effects of ConA and ConBr on the incidence of seizures induced by QA. ConBr (10 μg/site, i.c.v.) or ConA (10 μg/site, i.c.v.) were administered 15 min prior to QA (4 μL of a 9.2 mM solution; i.c.v.) administration. Mouse behavior was monitored for 10 min. The results represent the percentage of tonic-clonic seizures, **P < 0.01 compared with the control group (vehicle + QA)
It has been previously demonstrated that QA can produce short-term changes in the phosphorylation systems, probably by a mechanism dependent on NMDA activation after intracerebral administration [49, 50]. Phosphorylation of MAPKs (ERK1/2, p38MAPK and JNK1/2/3) in response to QA was evaluated at 3, 6 and 24 h after treatment (data not shown). Our results showed that QA infusion increased only the phosphorylation of c-Jun N-terminal kinase 2 (JNK2; 54 kDa band) 3 h after its administration, and the treatment with ConBr (10 μg/site) significantly prevented this QA-induced increase in phosphorylation (Fig. 4). In contrast, QA infusion did not alter the phosphorylation of JNK1 in the same conditions (Fig. 4). The total contents of all the kinases were not modified by ConBr treatment or QA infusion.
Modulation of JNK phosphorylation by QA and its inhibition by ConBr. Vehicle or ConBr (10 μg/site, i.c.v.) was administered (i.c.v.) 15 min prior to QA (4 μL of a 9.2 mM solution; i.c.v.) administration. After 3 h, the animals were sacrificed for removal of the hippocampi. The levels of JNK1 and JNK2 phosphorylation were analyzed by western blotting. a A representative western blot of phosphorylated c-Jun N-terminal kinase 1 and 2 (JNK1 and JNK2) and total forms of JNK1 and JNK2. b Quantitative analyses of the levels of JNK1 and JNK2 phosphorylation. c The data are expressed as a percentage of the control (vehicle; considered as 100%). The values are the mean ± SEM of five independent experiments (N = 5). *P < 0.05 QA versus control
Administration of QA through its specific action on the NMDA receptor increases calcium influx, and this process is able to activate various signaling pathways that can culminate in cell death (for a review, see reference 34). In our study, QA infusion increased propidium iodide uptake into hippocampal slices on evaluation at 24 h after its administration, showing labeled dead or dying cells. The pretreatment with ConBr (10 μg/site) significantly prevented QA-induced cell death in the hippocampus (Fig. 5). Interestingly, as depicted in Fig. 6, 24 h after QA infusion, we observed an increased level of serine 831 and 845 phosphorylation on the GluR1 subunit of the AMPA receptor. Moreover, one-way ANOVA revealed that pretreatment with ConBr was able to significantly reverse this effect.
Neuroprotective effect of ConBr against cell death provoked by QA. Cell death was quantified in hippocampal slices 24 h after the infusion of QA (4 μL of a 9.2 mM solution; i.c.v.). The animals received vehicle or ConBr (10 μg/site, i.c.v.) 15 min prior to QA administration. Hippocampal slices were prepared from each treated mouse group (control, ConBr, vehicle plus QA and ConBr plus QA). Propidium iodide (PI) uptake analysis was performed in four hippocampal slices for each treated mouse. Images were analyzed using Scion Image software. The area by the fluorescent propidium iodide (PI) was determined by densitometric analysis. The results represent the mean ± SEM of six experiments performed in quadruplicate. Values are expressed as mean ± SEM. **P < 0.01 ConBr plus QA versus vehicle plus QA, # P < 0.002 vehicle plus QA versus control (vehicle)
Modulation of Serine 831 and 845 phosphorylation on the GluR1 subunit of the AMPA receptor by QA and its inhibition by ConBr. Mice were treated with vehicle or ConBr (10 μg/site, i.c.v.) 15 min prior to QA administration (4 μL of a 9.2 mM solution; i.c.v.). After 24 h, the animals were sacrificed for the removal of the hippocampi. The levels of serine 831 and 845 phosphorylation on the GluR1 subunit of the AMPA receptor were analyzed by western blot. a Representative western blot of phosphorylated serine 831; b quantitative analyses of serine 831 phosphorylation on the GluR1 AMPA receptor; c representative western blot of phosphorylated serine 845; d quantitative analyses of serine 845 phosphorylation on the GluR1 AMPA receptor. The data are expressed as a percentage of the control (vehicle; considered as 100%). The values are the mean ± SEM of seven independent experiments (N = 7). ***P < 0.002 QA versus control or QA + ConBr group
Discussion
The main finding in the present work was the demonstration that ConBr, a mannose/glucose specific lectin, protects against seizures induced by QA in a manner dependent on its native structure and its interaction with oligosaccharide chains, possibly on the NMDA receptors. Likewise, ConBr counteracted QA-dependent JNK2 activation and prevented QA-induced cell death and phosphorylation increases of Ser831 and Ser845 on the GluR1 subunit of AMPA receptors in the hippocampus.
ConA, a lectin with the same carbohydrate affinity and with extensive amino acid sequence similarity to ConBr [30], did not change the percentage, intensity or the duration of seizures. It is important to highlight that ConBr, but not ConA, produced antidepressant-like effects when injected i.c.v. [31]. Moreover, ConBr showed different biological effects than ConA with respect to peripheral biological activities [11], including induction of rat paw edema [51], peritoneal macrophage spreading in the mouse [52], in vivo human lymphocyte stimulation [53], induction of histamine release [54, 55] and NO release [56]. Thus, it is possible that differences in the quaternary conformation of ConBr, as compared with ConA, may be the basis for these divergent phenotypes [30].
ConA has been commonly used as a tool to identify and evaluate the biochemical and eletrophysiological properties of NMDA [22, 29], AMPA [24, 25] and kainate receptors [23, 26–28, 57]. ConA, in the largely majority of these studies, appears to potentiate the activity of AMPA and kainate receptors and, to a less significant degree, of the NMDA receptors [29].
Moreover, in one study, ConA did not alter the binding of MK801, glycine or glutamate in synaptic plasma membranes of the rat hippocampus [58]. Hence, based on our results, it seems clear that ConA and ConBr produce different actions, indicating that the antagonistic effect of ConBr against QA neurotoxicity is more complex than a straightforward carbohydrate interaction, because both lectins are glucose/mannose specific. It is probably the case that ConBr action depends on its structural properties [30] or on a protein–protein interaction between the lectin and its target [28]. Nevertheless, it is obvious that the ConBr interaction with the glycan chain on the cell surface is a fundamental step in order to anchor the lectin on its target because the carbohydrate-binding domain (CRD) blockage with mannose counteracted the neuroprotective effect of ConBr.
Intracerebral injections of QA have been well documented to provoke short-term excitoxicity and seizures by a mechanism mainly dependent on the stimulation of NMDA receptors [33, 34, 59, 60]. Additionally, it has been shown that QA can also stimulate glutamate uptake into synaptic vesicles and increase glutamate release [35, 36].
Our results showed that beside the seizures, QA provoked an elevation of JNK2 phosphorylation in the hippocampus 3 h after its i.c.v. administration. Regarding short term changes in the phosphorylation systems, it was demonstrated that the intrastriatal injection of QA caused hyperphosphorylation of neurofilaments and GFAP in the striatum 30 min after its administration by a mechanism dependent on NMDA activation [50]. Moreover, an intracortical injection of QA increased c-Jun N-terminal kinases (JNKs) and p38MAPK and marginally activated ERK1/2 1 h after administration as evaluated by immunohistochemistry [49]. In addition, QA administration into the rat hippocampus did not show activation of ERK1/2. Conversely, activation of ERK1/2 by 17β-estradiol protected against cell death caused by QA [61]. Therefore, our data demonstrating the short-term modulation of MAPK phosphorylation by QA partially agrees with these studies, as we observed an elevation of hippocampal phosphorylation of 54 kDa JNK isoforms (JNK2/3) 3 h after QA administration without changes to the other MAPKs. In addition, the biochemical effect of QA on the activation of JNK2 was blocked by ConBr. JNKs, a subfamily of MAP kinases, are central mediators of apoptosis and neurodegeneration but also of plasticity and regeneration. Mammalian JNKs are encoded by three distinct genes (jnk1, jnk2, and jnk3), giving rise to at least 10 different splicevariants (isoforms). All variants share an epitope that needs to be dually phosphorylated for JNK activation (phospho-JNK). In the mouse hippocampus, JNK1 is mainly expressed as a 46 kDa band, while JNK2 is mainly expressed as a 54 kDa band. JNK3 is expressed as both isoforms: 46 and 54 kDa [62]. JNK isoforms exhibit various differences concerning the response to stimulus, specificity toward substrates and regulation by upstream kinases [62, 63]. It is interesting to observe that JNK1 (46 kDa) was more active in the basal state. Conversely, in some insults, such as ischemia, the isoforms activated correspond to the 54 kDa band indicating JNK2 and/or JNK3 involved in this process [62–64]. Therefore, our results agree with these possibilities, indicating that QA probably activates JNK isoforms more associated with induction of cell death and degeneration and that ConBr counteracts this effect.
QA provoked significant hippocampal cell death 24 h after its administration, and caused an increase in phosphorylation of Ser831 (approximately 40%) and Ser845 (approximately 20%) on the GluR1 subunit of the AMPA receptor. Cell death may be secondary to the elevation of intracellular Ca2+ by hyperactivation of NMDA receptors. Moreover, it has been demonstrated that a Ca2+-dependent activation of PKA, PKC and CaMKII by QA occurs via NMDA activation [50]. Ser845 can be phosphorylated by PKA, while Ser831 is phosphorylated by PKC and CaMKII, and these phenomena are essential to deliver AMPA receptors to the synapse (for a review, see references [65, 66]). Therefore, it seems possible that i.c.v. administration of QA might cause a sustained activation of NMDA receptors that causes cell death and phosphorylation of the hippocampal AMPA GluR1 subunit. Notably, these effects produced by QA were completely antagonized by ConBr. In spite of all the interesting behavioral and biochemical effects of ConBr, we did not determine if the mechanism of ConBr action was related to the impairment of QA binding to the receptor or stabilization of an inactive conformation of the NMDA receptor, or both. Therefore, future studies using slices and cell culture models that express native NR1, NR2A and NR2B NMDA-receptor subunits will be necessary to address the capacity of ConBr to directly bind to NMDA receptor subunits and determine its ability to block NMDA receptor responses, such as Ca2+ influx.
Taken together, our data suggest that ConBr, a mannose/glucose lectin, may counteract behavioral and biochemical effects of QA, possibly by inhibition of NMDA receptors. Finally, we pose an important question regarding the possibility that cerebral endogenous mannose or galactose-binding lectins [67–71] may be able to cause physiological modulation of the glutamatergic system by direct interaction with ionotropic glutamate receptors such as NMDA.
References
Varki A (1993) Biological roles of oligosaccharides: all of the theories are correct. Glycobiology 3:97–130
Breen KC, Coughlan CM, Hayes FD (1998) The role of glycoproteins in neural development function, and disease. Mol Neurobiol 16:163–220
Matthies H Jr, Kretlow J, Matthies H et al (1999) Glycosylation of proteins during a critical time window is necessary for the maintenance of long-term potentiation in the hippocampal CA1 region. Neuroscience 91:175–183
Lau A, Tymianski M (2010) Glutamate receptors, neurotoxicity and neurodegeneration. Pflugers Arch 460:525–542
Hullebroeck MF, Hampson DR (1992) Characterization of the oligosaccharide side chains on kainate binding proteins and AMPA receptors. Brain Res 590:187–192
Standley S, Baudry M (2000) The role of glycosylation in ionotropic glutamate receptor ligand binding, function, and trafficking. Cell Mol Life Sci 57:1508–1516
Hardingham GE, Bading H (2010) Synaptic versus extrasynaptic NMDA receptor signalling: implications for neurodegenerative disorders. Nat Rev Neurosci 11:682–696
Foster KA, McLaughlin N, Edbauer D et al (2010) Distinct roles of NR2A and NR2B cytoplasmic tails in long-term potentiation. J Neurosci 30:2676–2678
Kawamoto S, Hattori S, Sakimura K et al (1995) N Linked glycosylation of the AMPA-selective glutamate receptor channel alpha2 subunit is essential for essential for the acquisition of ligand-binding activity. J Neurochem 64:1258–1266
Laurie DJ, Bartke I, Schoepfer R et al (1997) Regional, developmental and interspecies expression of the four NMDAR2 subunits examined using monoclonal antibodies. Mol Brain Res 51:23
Cavada BS, Barbosa T, Arruda S et al (2001) Revisiting proteus: do minor changes in lectin structure matter in biological activity? Lessons from and potential biotechnological uses of the Diocleinae subtribe lectins. Curr Prot Pep Sci 2:1–13
Loris R (2002) Principles of structures of animal and plant lectins. Biochim Biophys Acta 1572:198–208
Ambrosi M, Cameron NR, Davis BG (2005) Lectins: tools for the molecular understanding of the glycocode. Org Biomol Chem 3:1593–1608
Sumner JB, Howell SF (1936) Identification of hemagglutinin of Jack Bean with Concanavalin A. J Bacteriol 32:227–237
Edelman GM, Cunningham BA, Reeke GN et al (1972) The covalent and three-dimensional structure of concanavalin A. Proc Natl Acad Sci USA 69:2580–2584
Hardman KD, Ainsworth CF (1972) Structure of concanavalin A at 2.4-A resolution. Biochemistry 11:4910–4919
Derewenda Z, Yariv J, Helliwell JR et al (1989) The structure of the saccharide-binding site of concanavalin A. EMBO J 8:2189–2193
Lin SS, Levitan IB (1991) Concanavalin A: a tool to investigate neuronal plasticity. Trends Neurosci 14:273–277
Scherer WJ, Udin SB (1994) Concanavalin A reduces habituation in the tectum of the frog. Brain Res 667:209–215
Kirner A, Deutsch S, Weiler E et al (2003) Concanavalin A application to the olfactory epithelium reveals different sensory neuron populations for the odour pair D- and L-carvone. Behav Brain Res 138:201–206
Suzuki T, Okumura-Noji K (1995) NMDA receptor subunits epsilon 1 (NR2A) and epsilon 2 (NR2B) are substrates for Fyn in the postsynaptic density fraction isolated from the rat brain. Biochem Biophys Res Commun 216:582–588
Clark RA, Gurd JW, Bissoon N et al (1998) Identification of lectin-purified neural glycoproteins, GPs 180, 116, and 110, with NMDA and AMPA receptor subunits: conservation of glycosylation at the synapse. J Neurochem 70:2594–2605
Partin KM, Patneau DK, Winters CA et al (1993) Selective modulation of desensitization at AMPA versus kainate receptors by cyclothiazide and concanavalin A. Neuron 11:1069–1082
Hoffman KB, Kessler M, Ta J et al (1998) Mannose-specific lectins modulate ligand binding to AMPA-type glutamate receptors. Brain Res 795:105–111
Thalhammer A, Everts I, Hollmann M (2002) Inhibition by lectins of glutamate receptor desensitization is determined by the lectin’s sugar specificity at kainate but not AMPA receptors. Mol Cell Neurosci 21:521–533
Yue KT, MacDonald JF, Pekhletski R et al (1995) Differential effects of lectins on recombinant glutamate receptors. Eur J Pharmacol 291:229–235
Everts I, Petroski R, Kizelsztein P et al (1999) Lectin-induced inhibition of desensitization of the kainate receptor GluR6 depends on the activation state and can be mediated by a single native or ectopic N-linked carbohydrate side chain. J Neurosci 19:916–927
Fay AM, Bowie D (2006) Concanavalin-A reports agonist-induced conformational changes in the intact GluR6 kainate receptor. J Physiol 572:201–213
Everts I, Villmann C, Hollmann M (1997) N-Glycosylation is not a prerequisite for glutamate receptor function but Is essential for lectin modulation. Mol Pharmacol 52:861–873
Sanz-Aparicio J, Hermoso J, Granjeiro TB et al (1997) The crystal structure of Canavalia brasiliensis lectin suggests a correlation between its quaternary conformation and its distinct biological properties from Concanavalin A. FEBS Letters 405:114–118
Barauna SC, Kaster MP, Heckert BT et al (2006) Antidepressant-like effect of lectin from Canavalia brasiliensis (ConBr) administered centrally in mice. Pharmacol Biochem Behav 85:160–169
Hardingham GE (2009) Coupling of the NMDA receptor to neuroprotective and neurodestructive events. Biochem Soc Trans 37:1147–1160
Schwarcz R, Pellicciari R (2002) Manipulation of brain kynurenines: glial targets, neuronal effects, and clinical opportunities. J Pharmacol Exp Ther 303:1–10
Schwarcz R, Guidetti P, Sathyasaikumar KV et al (2010) Of mice, rats and men: revisiting the quinolinic acid hypothesis of Huntington’s disease. Prog Neurobiol 90:230–245
Tavares RG, Schmidt AP, Tasca CI et al (2008) Quinolinic acid-induced seizures stimulate glutamate uptake into synaptic vesicles from rat brain: effects prevented by guanine-based purines. Neurochem Res 33:97–102
Tavares RG, Schmidt AP, Abud J et al (2005) In vivo quinolinic acid increases synaptosomal glutamate release in rats: reversal by guanosine. Neurochem Res 30:439–444
Moreira RA, Cavada BS (1984) Lectin from Canavalia brasiliensis Mart. Isolation, characterization and behavior during germination. Biol Plant Praga Checoslov 26:113–120
Schmidt AP, Lara DR, de FariaMaraschin J et al (2000) Guanosine and GMP prevent seizures induced by quinolinic acid in mice. Brain Res 864:40–43
Cruz SL, Gauthereau MY, Camacho-Munoz C et al (2003) Effects of inhaled toluene and 1, 1, 1-trichloroethane on seizures and death produced by N-methyl-d-aspartic acid in mice. Behav Brain Res 140:195–202
Marganella C, Bruno V, Matrisciano F et al (2005) Comparative effects of levobupivacaine and racemic bupivacaine on excitotoxic neuronal death in culture and N-methyl-D-aspartate-induced seizures in mice. Eur J Pharmacol 518:111–115
Cordova FM, Rodrigues AL, Giacomelli MB et al (2004) Lead stimulates ERK1/2 and p38MAPK phosphorylation in the hippocampus of immature rats. Brain Res 998:65–72
Molz S, Decker H, Dal-Cim T et al (2008) Glutamate-induced toxicity in hippocampal slices involves apoptotic features and p38 MAPK signaling. Neurochem Res 33:27–36
Boeck CR, Ganzella M, Lottermann A et al (2004) NMDA preconditioning protects against seizures and hippocampal neurotoxicity induced by quinolinic acid in mice. Epilepsia 45:745–750
Oliveira CS, Rigon AP, Leal RB et al (2008) The activation of ERK1/2 and p38 mitogen-activated protein kinases is dynamically regulated in the developing rat visual system. Int J Dev Neurosci 26:355–362
Peterson GL (1977) A simplification of the protein assay method of Lowry et al. which is more generally applicable. Anal Biochem 83:346–356
Bjerrum OJ, Heegaard NHH (1988) CRC handbook of immunoblotting of proteins, vol I: Technical Descriptions. CRC Press, Boca Raton, FL
Rigon AP, Cordova FM, Oliveira CS et al (2008) Neurotoxicity of cadmium on immature hippocampus and a neuroprotective role for p38 MAPK. Neurotoxicology 29:727–734
Posser T, de Aguiar CB, Garcez RC et al (2007) Exposure of C6 glioma cells to Pb(II) increases the phosphorylation of p38(MAPK) and JNK1/2 but not of ERK1/2. Arch Toxicol 81:407–414
Ferrer I, Blanco R, Carmona M (2001) Differential expression of active, phosphorylation-dependent MAP kinases, MAPK/ERK, SAPK/JNK and p38, and specific transcription factor substrates following quinolinic acid excitotoxicity in the rat. Mol Brain Res 94:48–58
Pierozan P, Zamoner A, Soska AK et al (2010) Acute intrastriatal administration of quinolinic acid provokes hyperphosphorylation of cytoskeletal intermediate filament proteins in astrocytes and neurons of rats. Exp Neurol 224:188–196
Bento CAM, Cavada BS, Oliveira JTA et al (1993) Rat paw edema and leucocyte migration induced by plant lectins. Agents Actions 38:48–54
Rodriguez D, Cavada BS, Abreu-de-Oliveira JT et al (1992) Differences in macrophage stimulation and leukocyte accumulation in response to intraperitoneal administration of glucose/mannose-binding plant lectins. Braz J Med Biol Res 25:823–826
Barbosa T, Arruda S, Cavada B et al (2001) In vivo lymphocyte activation and apoptosis by lectins of the diocleinaesubtribo. Mem Inst Oswaldo Cruz 96:673–678
Ferreira RR, Cavada BS, Moreira RA et al (1996) Characteristics of the histamine release from hamster cheek pouch mast cells stimulated by lectins from Brazilian beans and concanavalin A. Inflamm Res 45:442–447
Lopes FC, Cavada BS, Pinto VP et al (2005) Differential effect of plant lectins on mast cells of different origins. Braz J Med Biol Res 38:935–941
Andrade JL, Arruda S, Barbosa T et al (1999) Lectin-induced nitric oxide production. Cell Immunol 194:98–102
Pemberton KE, Belcher SM, Ripellino JA, et.al. (1998) High-affinity kainate-type ion channels in rat cerebellar granule cells. J Physiol 510(Pt 2):401–420
Machaidze GG, Mikeladze D (2001) Different effects of lectins on the ligand binding of the NMDA receptors and sigma sites in rat brain hippocampus synaptic membranes. Neurochem Res 26:457–462
Lapin IP (1978) Stimulant and convulsive effects of kynurenines injected into brain ventricles in mice. J Neural Trans 42:37–43
Stone TW, Perkins MN (1981) Quinolinic acid: a potent endogenous excitant at amino acid receptors in CNS. Eur J Pharmacol 72:411–412
Kuroki Y, Fukushima K, Kanda Y, Mizuno K, Watanabe Y (2001) Neuroprotection by estrogen via extracellular signal-regulated kinase against quinolinic acid-induced cell death in the rat hippocampus. Eur J Neurosci 13:472–476
Brecht S, Kirchhof R, Chromik A, Willesen M, Nicolaus T, Raivich G, Wessig J, Waetzig V, Goetz M, Claussen M, Pearse D, Kuan CY, Vaudano E, Behrens A, Wagner E, Flavell RA, Davis RJ, Herdegen T (2005) Specific pathophysiological functions of JNK isoforms in the brain. Eur J Neurosci 21:363–377
Zhao Y, Herdegen T (2009) Cerebral ischemia provokes a profound exchange of activated JNK isoforms in brain mitochondria. Mol Cell Neurosci 41:186–195
Waetzig V, Zhao Y, Herdegen T (2006) The bright side of JNKs-Multitalented mediators in neuronal sprouting, brain development and nerve fiber regeneration. Prog Neurobiol 80:84–97
Kessels HW, Malinow R (2009) Synaptic AMPA receptor plasticity and behavior. Neuron 61:340–350
Santos SD, Carvalho AL, Caldeira MV et al (2009) Regulation of AMPA receptors and synaptic plasticity. Neuroscience 158:105–125
Zanetta JP, Meyer A, Kuchler S et al (1987) Isolation and immunochemical study of a soluble cerebellar lectin delineating its structure and function. J Neurochem 49:1250–1257
Marschal P, Reeber A, Neeser JR et al (1989) Carbohydrate and glycoprotein specificity of two endogenous cerebellar lectins. Biochimie 71:645–653
Lehmann S, Kuchler S, Theveniau M et al (1990) An endogenous lectin and one of its neuronal glycoprotein ligands are involved in contact guidance of neuron migration. Proc Natl Acad Sci USA 87:6455–6459
Kuchler S, Lehmann S, Vincendon G et al (1992) Endogenous lectin cerebellar soluble lectin involved in myelination is absent from nonmyelinating Schwann cells. J Neurochem 58:1768–1772
Lekishvili T, Hesketh S, Brazier MW et al (2006) Mouse galectin-1 inhibits the toxicity of glutamate by modifying NR1 NMDA receptor expression. Eur J Neurosci 24:3017–3025
Acknowledgments
CNPq (#305194/2010-0), CAPES/PROCAD (#167/2007), CAPES/DGU (#173/2008), FINEP research grant “Rede Instituto Brasileiro de Neurociência (IBN-Net; #01.06.0842-00”) and FAPESC (# 6336/2011-3) supported this work. EHT, BSC, CIT and RBL are recipients of CNPq fellowships.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Russi, M.A., Vandresen-Filho, S., Rieger, D.K. et al. ConBr, a Lectin from Canavalia brasiliensis Seeds, Protects Against Quinolinic Acid-Induced Seizures in Mice. Neurochem Res 37, 288–297 (2012). https://doi.org/10.1007/s11064-011-0608-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-011-0608-x