Abstract
Previous studies have shown that hyperoxia results in cerebral cortical neuronal apoptosis. Studies have also shown that phosphorylation of anti-apoptotic proteins Bcl-2 and Bcl-xl results in loss of their anti-apoptotic potential leading to alteration in mitochondrial membrane permeability and the release of apoptogenic proteins in the neuronal cell of the newborn piglets. The present study tests the hypothesis that cerebral hyperoxia will result in increased serine phosphorylation of apoptotic proteins Bcl-2, Bcl-xl, Bax, and Bad in the mitochondrial membranes of the cerebral cortex of newborn piglets. Twelve newborn piglets were divided into normoxic (Nx, n = 6) exposed to an FiO2 of 0.21 for 1 h and hyperoxic (Hyx, n = 6) exposed to FiO2 of 1.0 for 1 h. In the Hyx group, PaO2 was maintained above 400 mmHg while the Nx group was kept at 80–100 mmHg. Cerebral cortical tissue was harvested and mitochondrial fractions were isolated. Mitochondrial membrane proteins were separated using 12% SDS-PAGE, and probed with anti-serine phosphorylated Bcl-2, Bcl-xl, Bax, and Bad antibodies. Protein bands were detected, analyzed by imaging densitometry and density expressed as absorbance (OD × mm2). Phosphorylated Bcl-2 (p-Bcl-2) protein density (OD × mm2) was 81.81 ± 9.24 in Nx and 158.34 ± 10.66 in Hyx (P < 0.05). Phosphorylated Bcl-xl (p-Bcl-xl) protein density was 52.98 ± 3.59 in Nx and 99.62 ± 18.22 in Hyx (P < 0.05). Phosphorylated Bax (p-Bax) protein was 161.13 ± 6.27 in Nx and 174.21 ± 15.95 in Hyx (P = NS). Phosphorylated Bad (p-Bad) protein was 166.24 ± 9.47 in Nx 155.38 ± 12.32 in Hyx (P = NS). The data show that there is a significant increase in serine phosphorylation of Bcl-2 and Bcl-xl proteins while phosphorylation of Bad and Bax proteins were not altered during hyperoxia in the mitochondrial fraction of the cerebral cortex of newborn piglets. We conclude that hyperoxia results in differential post-translational modification of anti-apoptotic proteins Bcl-2 and Bcl-xl as compared to pro-apoptotic proteins Bax and Bad in mitochondria. We speculate that phosphorylation of Bcl-2 and Bcl-xl will result in loss of their anti-apoptotic potential by preventing their dimerization with Bax leading to activation of the caspase cascade of neuronal death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoxic–ischemic injury to the newborn brain has been shown to result in rapid cell death with features of both necrosis and apoptosis [1]. Apoptosis is a tightly controlled, highly ordered, physiological form of cell death, also referred to as programmed cell death [2]. Apoptosis occurs in the context of hyperoxia-induced organ injury [3]. It is well recognized that oxygen concentrations higher than physiologic levels exert toxicity to the developing retinas and lungs of the premature infant [4]. Oxygen is also a potent trigger for apoptotic neuronal death in the developing brain [3, 5]. Hyperoxia generates reactive oxygen species (ROS) similar to reoxygenation following hypoxia/ischemia [2, 3]. Hyperoxia may exacerbate, rather than ameliorate, oxygen free radical mediated cerebral tissue injury [2, 3]. It has also been shown by Gill et al. that following hypoxia/ischemia, 100% O2 resuscitation led to increased Bax mediated activation of endoplasmic reticulum cell death signaling and subsequent inflammation and injury by increasing necrotic like cell death [6]. Following 24 h of hyperoxia, Hu et al. [2] have demonstrated increased levels of DNA fragmentation in the cerebral cortex of newborn rats [7].
As neural tissue PO2 increases, the body’s antioxidant defenses are overwhelmed due to increased production of ROS in the mitochondria, cytoplasm, membranes, and extracellular fluid compartments [8–10]. Oxidative stress damages lipids, proteins, and other cell constituents, and ultimately leads to neuronal cell death [11–13]. Intracellular ROS produced during exposure to hyperoxia are responsible for both the lung injury observed in intact animals and the death of cells in culture following hyperoxia [14, 15]. ROS may disrupt regulation of DNA repair mechanisms, signal transduction, DNA and RNA synthesis, protein synthesis, and enzyme biosynthesis [11, 16].
Studies have shown that hyperoxia causes an elevation in the steady state of nitric oxide (NO) concentration in cerebral cortex of both rats and mice. Hyperoxia causes an increase in NO synthesis as part of a response to oxidative stress [17]. Hoehn et al. demonstrated that hyperoxia induces up-regulation of inducible-NOS mRNA and synthesis of inducible-NOS-protein in microglial cells in several areas of the immature rat brain. This increased protein synthesis leads to the formation of peroxynitrite, which indicates potential damage to structures of the neonatal brain [18].
During neonatal resuscitation, oxygen at levels greater than room air is routinely used for treatment of neonatal hypoxia–ischemia [19, 20]. Vento et al. were able to show that newborn infants who were resuscitated with 100% oxygen have an increased oxidative stress for at least a month, in contrast to infants resuscitated with room air [21]. Oxidative stress implies increased ROS and this increase is associated with programmed cell death [3]. In a recent study, hyperoxia was identified as a risk factor for abnormal neurologic outcome of preterm infants [3]. This indicates that apoptotic neurodegeneration triggered by a high oxygen environment during a critical stage of brain development may account for cognitive and also motor impairment in premature infants [3].
The Bcl-2 multigene family of proteins is an important determinant of apoptotic cell death. It consists of pro-apoptotic (Bax, Bcl-Xs, Bak and Bad) and anti-apoptotic (Bcl-2, Bcl-XL and Bcl-w) proteins. Bcl-2 and Bax proteins play a crucial role in regulating cell survival and cell death. Bcl-2 family members determine cell death and survival by controlling mitochondrial membrane ion permeability, cytochrome c release, and the subsequent activation of caspase mediated executor functions [2, 22]. Bax is a 21 kDa protein that shares homology with Bcl-2, and heterodimerizes with Bcl-2 or homodimerizes with itself. When Bax is over-expressed in cells, apoptotic death in response to a death signal is accelerated. When Bcl-2 is over-expressed, it heterodimerizes with Bax and cell death is repressed. Therefore, the ratio of Bcl-2 to Bax appears to be important in determining susceptibility to apoptosis [7, 23]. Previously in our laboratory we have shown that during hyperoxia the expression of Bax protein was increased and Bcl-2 protein expression was decreased [11].
There is evidence to support that hyperoxia leads to changes in phosphorylation of proteins that control neuronal survival during development [3]. Phosphorylation may affect the function of Bcl-2 or Bax by altering the ability of these proteins to form heterodimers or act independently of dimerization. Post-translational modification of Bcl-2 and Bax proteins through phosphorylation changes the function of these proteins by altering cell cycle events, by regulating cell proliferation as well as programmed cell death [23, 24]. Studies have shown that treatment of cells with a number of agents results in phosphorylation of Bcl-2 and is associated with inhibition of the anti-apoptotic function of Bcl-2 [7, 25, 26]. The present study tests the hypothesis that cerebral hyperoxia results in increased serine phosphorylation of anti-apoptotic proteins Bcl-2 and Bcl-xl, in the mitochondrial membranes of the cerebral cortex of the newborn piglet.
Experimental Methods
Animal Protocol
Studies were performed in 2–5 days old newborn piglets using an experimental protocol, approved by the Institutional Animal Care and Use Committee of Drexel University. We studied 12 anesthetized, ventilated piglets, randomly assigned to two groups: normoxia and hyperoxia. Anesthesia was induced with isoflurane 4% and then lowered to 1%, while allowing the animals to breathe spontaneously through a mask. Lidocaine 1% was used for all instrumentation. A tracheostomy was performed and endotracheal tube secured. Femoral arterial polyvinyl chloride catheters were inserted for continuous monitoring and intravenous catheters used for drug administration. After instrumentation, isoflurane was discontinued and supplemental intravenous fentanyl (50 μg/kg), and pancuronium (0.1 mg/kg) were administered as needed while the animals were mechanically ventilated. In both groups, pH was maintained between 7.35 and 7.45, and pCO2 between 35 and 45 mmHg throughout the study. After an initial stabilization period at FiO2 of 0.21, the normoxic group was continued at an FiO2 of 0.21 for 1 h and the PaO2 kept at 80–100 mmHg. The hyperoxic group was subjected to FiO2 of 1.0 for 1 h and the PaO2 was maintained above 400 mmHg. At the conclusion of the 1 h period, the brain tissue was immediately removed under anesthesia placed in mitochondrial isolation buffer or in liquid nitrogen and stored at −80°C prior to biochemical analysis.
Determination of High Energy Phosphates
To assess tissue oxygenation, cerebral energy metabolism with brain tissue concentrations of ATP and phosphocreatine (PCr) were determined by a coupled enzyme reaction using the method of Lamprecht et al. [27].
Isolation of Cerebral Cortical Mitochondrial Fraction
Cerebral tissue mitochondrial fraction was isolated using the method of Booth and Clark [28]. One gram of cerebral cortical tissue was homogenized using a Dounce-type glass homogenizer in 30 ml of fresh isolation medium containing 0.32 M sucrose, 1 mM EDTA and 20 mM Tris–HCl buffer, pH 7.1. The homogenate was centrifuged for 3 min at 1,500×g and the resulting supernatant was centrifuged at 15,000×g for 10 min to provide the crude mitochondrial pellet. To purify mitochondria, the crude mitochondrial pellet was suspended in 2.5 ml of isolation buffer and mixed with 12.5 ml of 12% Ficoll solution and placed on the bottom of an ultracentrifuge centrifuge tube. Ten milliliter of 7% Ficoll solution was layered over it followed by 10 ml of isolation medium. The gradient was centrifuged for 30 min at 100,000×g. The mitochondrial pellet was washed and re-suspended in the isolation medium. The purity of mitochondrial preparation with respect to the possibility of contamination with cell nuclei was determined by immunoblotting using nuclear marker proteins lamin A and lamin C. No lamin A or C were detected in the mitochondrial fraction, demonstrating that the mitochondrial preparation was free from nuclear contamination. Protein concentration was determined by the method of Lowry et al. [29]. The mitochondrial preparation was diluted to a final concentration of 150 μg protein/100 μl.
Immunoprecipitation and Western Blot Analysis
Proteins were separated on a 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) gel and transferred onto nitrocellulose membrane and blocked with 6% phosphate-buffered saline (PBS)–milk at 4°C with constant agitation for 4–6 h. The membranes were then incubated with primary polyclonal antibodies (Santa Cruz Biotech, Santa Cruz, CA, USA) anti-Bad, anti-Bax, anti-Bcl-xl, anti-Bcl-2, antiphosphoserine-Bad, antiphosphoserine-Bcl-xl and antiphosphoserine-Bcl-2 antibodies in 3% PBS–milk, overnight at 4°C. The proteins for Bax phosphorylation were immunoprecipitated with phosphorylated anti-serine antibody and then immunoblotted with anti-Bax antibody. Subsequently the nitrocellulose was washed with distilled water and incubated with horseradish peroxidase conjugated secondary antibody (Rockland, Gilbertsville, PA, USA) in 3% milk for 1.5 h at room temperature with constant agitation. Specific complexes were detected by enhanced chemiluminescence method using the ECL detection system (Amersham Pharmacia Biotech, Little Chalfont, Buckinghamshire, UK) and analyzed by imaging densitometry (GS-700 densitometer, Bio-Rad, Hercules, CA, USA). The densitometric scanning data were expressed as autoradiographic values (OD × mm2) per immunoblot protein representing Bax, Bad, Bcl-2, and Bcl-xl proteins densities. Actin was used as a loading control.
Statistical Analysis
Statistical analysis of biochemical measurements was performed using an unpaired t test for comparison between groups. A P value < 0.05 was considered significant. All values are shown as mean ± standard deviation (SD).
Results
ATP and Phosphocreatine
The ATP concentrations in the normoxic and hyperoxic groups were 4.83 ± 0.50 and 5.09 ± 0.36 μmol/g brain, respectively (P = NS vs. Nx). The phosphocreatine concentrations in the normoxic and hyperoxic groups were 3.87 ± 0.30 and 3.93 ± 0.55 μmol/g brain, respectively, (P = NS vs. Nx).
Expression of Serine Phosphorylated Bax, Bad, Bcl-2, Bcl-xl
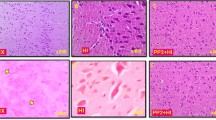
The expression of phosphorylated serine (OD × mm2) changed from 81.8 ± 9.2 to 158.3 ± 10.7 (P < 0.05) in Bcl-2 and from 52.9 ± 3.6 to 99.6 ± 18.2 in Bcl-xl (P < 0.05) when compared from normoxia to hyperoxia (Fig. 1). The expression of serine phosphorylated pro-apoptotic proteins Bax and Bad (OD × mm2) did not significantly change when compared from normoxia to hyperoxia 161.1 ± 6.3 to 174.2 ± 15.9 in Bax and 166.2 ± 9.5 to 155.3 ± 12.3 in Bad (Fig. 1).
Expression of Bax, Bad, Bcl-2, Bcl-xl
Bax expression (OD × mm2) was 75.2 ± 23.8 in the normoxic and 145.6 ± 5.0 in the hyperoxic group (P < 0.01) (Fig. 2). Bad expression (OD × mm2) was 37.2 ± 3.9 in the normoxic and 85.6 ± 6.2 in the hyperoxic group (P < 0.01) (Fig. 2). Expression of the anti-apoptotic proteins Bcl-2 and Bcl-xl did not change significantly with Bcl-2 145.6 ± 6.9–148.4 ± 6.6 and with Bcl-xl 37.2 ± 3.9–85.6 ± 6.2 (Fig. 2).
Representative immunoblots demonstrating serine phosphorylated Bax, Bad, Bcl-2, and Bcl-xl expression are shown in (Fig. 3). During hyperoxia, serine phosphorylated Bax and Bad proteins in the mitochondrial fraction in the cerebral cortex of newborn piglet demonstrated no change in their expression in normoxia compared to hyperoxia. The serine phosphorylated Bcl-2, and Bcl-xl showed increased expression in the hyperoxic group when compared to the normoxic group.
Discussion
The data demonstrate that 1 h of hyperoxia resulted in increased in the expression of pro-apoptotic proteins Bax and Bad and the expression of Bcl-2 and Bcl-xl was not significantly changed. However, under the same condition of hyperoxia, there was increased levels of serine phosphorylated Bcl-2 and Bcl-xl when compared to normoxia. Bax and Bad protein expression did not change. Bax and Bcl-2 expression results were comparable to previous data shown in our laboratory.
During hyperoxia, the production of ROS leads to the activation of the mitochondrial-dependent cell death pathway through activation of the mitogen-activated protein (MAP) kinase pathways and the proapoptotic proteins Bax or Bad, with subsequent mitochondrial membrane permeability resulting in cell death [30, 31]. Exposure to hyperoxia results in mitochondrial membrane damage with subsequent loss of ATP [32]. This study was performed in isolated cell system in vitro and cannot be compared with our data for an in vivo animal model. Mitochondria-dependent apoptotic signaling is characterized by the release of proapoptotic molecules such as cytochrome c and apoptosis inducing factor (AIF) from mitochondria [32].
Phosphorylation of Bcl-2 protein was shown originally in leukemic cells where treatment with phosphatase inhibitors results in cell death, suggesting that phosphorylation of Bcl-2 protein leads to loss of its function [7, 19, 26]. Therefore, post-translational modification of Bcl-2 family members by phosphorylation regulates apoptosis [33]. Previous studies have shown that phosphorylation disrupts the association of Bcl-2 with Bax, an effect that could lead to Bax-induced apoptosis [19, 25]. Phosphorylation of Bcl-2 has been reported in response to multiple stimuli, and it can be mediated by a variety of kinases, including Raf-1 kinase, protein kinase C, protein kinase A, c-Jun N-terminal kinase, and CDC2 kinase [19, 34–36]. If Bcl-2 phosphorylation results in a loss of its anti-apoptotic function, then higher Bcl-2 levels may not provide additional protection against apoptosis. Once activated, the pathway leading to phosphorylation of Bcl-2 could result in the complete loss of anti-apoptotic potential, irrespective of Bcl-2 level [19, 26].
Studies suggest that phosphorylation modifies the function of Bcl-2 family members by changing patterns of dimerization [25, 37]. However, other studies found that phosphorylation of Bcl-2 did not affect dimerization [24, 38]. In support of the latter, Hu et al. demonstrated that phosphorylated Bcl-2 after either all trans retinoic acid (ATRA) or taxol treatment does not change its capacity to form heterodimers with Bax. The discrepancy in findings from different studies may be due to variation in the cellular systems or immunoprecipitation methods utilized [33].
In the present study, we have shown that 1 h of hyperoxia was sufficient to increase the expression of the pro-apoptotic proteins, Bax and Bad that will lead to cell death. We have also shown that following 1 h of hyperoxia, there was increased levels of serine phosphorylated Bcl-2 and Bcl-xl and no changes were noted in Bax and Bad. Therefore, unlike Bax and Bad proteins, during hyperoxia, Bcl-2 and Bcl-xl proteins have a greater potential to undergo phosphorylation on their serine residue. The loss of the anti-apoptotic potential of Bcl-2 and Bcl-xl leads to further apoptosis; this is likely due to an increase in Bax, Bad to Bcl-2, Bcl-xl ratio. Furthermore, the results show that mitochondrial cerebral energy metabolism (measured by ATP and PCr) is not statistically different during hyperoxia when compared to normoxia. This is different when compared to hypoxia where cerebral energy metabolism is lower when compared to normoxia. Indicating that, alterations in apoptotic proteins during hyperoxia are independent of energy metabolism.
It is possible that these changes during hyperoxia are brought about by oxygen free radicals which are generated during hyperoxic exposure. Perhaps the increased free radicals inactivate serine phosphatases thereby leading to the increase in phosphorylated Bcl-2 and Bcl-xl. In previous studies, we have shown that hypoxia, a condition that leads to increase generation of free radicals, results in decreased activity of protein phosphatase 2A (a serine phosphatase) in cerebral cortex of newborn piglets [39]. The results show that there is a differential phosphorylation of anti-apoptotic proteins as compared to pro-apoptotic proteins. This differential phosphorylation may have to do with the accessibility of specific proteins to serine phosphatases and the microenvironment of these proteins in the membrane.
Mitochondria-dependent apoptosis is initiated by the translocation or activation of the proapoptotic Bcl-2 family members Bax or Bak and prevented by the overexpression of anti-apoptotic molecules from the same family (Bcl-xl or Bcl-2) [14, 40]. Previous studies have shown that the anti-apoptotic effects of over-expression of several Bcl-2 family members arise at least in part from their ability to inhibit mitochondrial cytochrome c release [41, 42]. Bax translocation to mitochondria and mitochondria permeability transition pore (PTP) opening are known to be responsible for cytochrome c release [43]; and both processes are hindered by Bcl-2 [44].
During apoptosis, Bcl-2 remains bound to the mitochondrial membranes, but the cytosolic forms of Bax, Bid, and Bcl-xl have been found to redistribute from the cytosol into the cell’s membranes, in particular the mitochondrial membranes [45, 46]. The role of Bcl-2 family members in mitochondrial membrane permeability is supported by the observation that several family members, including Bid, Bax, and Bak, are capable of inducing cytochrome c release from purified mitochondria [42, 47, 48]. Furthermore, in vitro studies have shown that the insertion of Bax in the mitochondrial membranes results in the release of cytochrome c from mitochondria [46, 47].
In summary, the present study investigated the effect of hyperoxia-induced changes on the expression of pro-apoptotic and anti-apoptotic proteins and their posttranslational modification by phosphorylation. The results show that exposure to hyperoxia leads to an increase in the pro-apoptotic protein Bad without changes in the anti-apoptotic protein Bcl-xl in hyperoxia compared to normoxia. The data demonstrate that, during hyperoxia, there is an increase in serine phosphorylation of Bcl-2 and Bcl-xl in the mitochondrial fraction of the cerebral cortex of newborn piglets, and that the phosphorylation of Bax and Bad was not altered. During hyperoxia, tissue oxygenation was unchanged, both the normoxic and hyperoxic groups have a comparable level of cerebral high energy phosphates.
We conclude that hyperoxia results in post-translational modification, particularly, serine phosphorylation of the anti-apoptotic proteins Bcl-2 and Bcl-xl in the mitochondrial fraction of the cerebral cortex of newborn piglets. Serine phosphorylation of Bcl-2 and Bcl-xl will result in loss of their anti-apoptotic potential by preventing their dimerization with pro-apoptotic proteins Bax and Bad. We speculate that increased free Bax and Bad will lead to activation of the caspase cascade and result in neuronal death in the cerebral cortex of the newborn piglets.
References
Banasiak KJ, Xia Y, Haddad GG (2000) Mechanisms underlying hypoxia-induced neuronal apoptosis. Prog Neurobiol 62:215–249. doi:10.1016/S0301-0082(00)00011-3
Hu X, Qiu J, Grafe MR et al (2003) Bcl-2 family members make different contributions to cell death in hypoxia and/or hyperoxia in rat cerebral cortex. Int J Dev Neurosci 21:371–377. doi:10.1016/S0736-5748(03)00089-3
Felderhoff-Mueser U, Bittigau P, Sifringer M et al (2004) Oxygen causes cell death in the developing brain. Neurobiol Dis 17:273–282. doi:10.1016/j.nbd.2004.07.019
Sirinyan M, Sennlaub F, Dorfman A et al (2006) Hyperoxic exposure leads to nitrative stress and ensuing microvascular degeneration and diminished brain mass and function in the immature subject. Stroke 37:2807–2815. doi:10.1161/01.STR.0000245082.19294.ff
Taglialatela G, Perez-Polo JR, Rassin DK (1998) Induction of apoptosis in the CNS during development by the combination of hyperoxia and inhibition of glutathione synthesis. Free Radic Biol Med 25:936–942. doi:10.1016/S0891-5849(98)00131-2
Gill MB, Bockhorst K, Narayana P et al (2008) Bax shuttling after neonatal hypoxia-ischemia: hyperoxia effects. J Neurosci Res 86:3584–3604. doi:10.1002/jnr.21795
Ashraf QM, Zanelli SA, Mishra OP et al (2001) Phosphorylation of Bcl-2 and Bax proteins during hypoxia in newborn piglet. Neurochem Res 26:1–9. doi:10.1023/A:1007654912421
Dean JB, Mulkey DK, Garcia AJ 3rd et al (2003) Neuronal sensitivity to hyperoxia, hypercapnia, and inert gases at hyperbaric pressures. J Appl Physiol 95:883–909
Dean JB, Mulkey DK, Henderson RAIII et al (2004) Hyperoxia, reactive oxygen species, and hyperventilation: oxygen sensitivity of brain stem neurons. J Appl Physiol 96:784–791. doi:10.1152/japplphysiol.00892.2003
Mulkey DK, Henderson RAIII, Olson JE et al (2001) Oxygen measurements in brain stem slices exposed to normobaric hyperoxia and hyperbaric oxygen. J Appl Physiol 90:1887–1899. doi:10.1063/1.1383259
Chang E, Hornick K, Fritz KI et al (2007) Effect of hyperoxia on cortical neuronal nuclear function and programmed cell death mechanisms. Neurochem Res 32:1142–1149. doi:10.1007/s11064-007-9282-4
Clement MV, Pervaiz S (1999) Reactive oxygen intermediates regulate cellular response to apoptotic stimuli: an hypothesis. Free Radic Res 30:247–252. doi:10.1080/10715769900300271
Saugstad OD (1996) Mechanisms of tissue injury by oxygen radicals: implications for neonatal disease. Acta Paediatr 85:1–4. doi:10.1111/j.1651-2227.1996.tb13880.x
Budinger GR, Tso M, McClintock DS et al (2002) Hyperoxia-induced apoptosis does not require mitochondrial reactive oxygen species and is regulated by Bcl-2 proteins. J Biol Chem 277:15654–15660. doi:10.1074/jbc.M109317200
Freeman BA, Crapo JD (1981) Hyperoxia increases oxygen radical production in rat lungs and lung mitochondria. J Biol Chem 256:10986–10992
Droge W (2002) Free radicals in the physiological control of cell function. Physiol Rev 82:47–95
Thom SR, Bhopale V, Fisher D et al (2002) Stimulation of nitric oxide synthase in cerebral cortex due to elevated partial pressures of oxygen: an oxidative stress response. J Neurobiol 51:85–100. doi:10.1002/neu.10044
Hoehn T, Felderhoff-Mueser U, Maschewski K et al (2003) Hyperoxia causes inducible nitric oxide synthase-mediated cellular damage to the immature rat brain. Pediatr Res 54:179–184. doi:10.1203/01.PDR.0000075220.17631.F1
Blagosklonny MV, Giannakakou P, el-Deiry WS et al (1997) Raf-1/bcl-2 phosphorylation: a step from microtubule damage to cell death. Cancer Res 57:130–135
Delivoria-Papadopoulos M, Mishra OP (2000) Mechanisms of perinatal cerebral injury in fetus and newborn. Ann N Y Acad Sci 900:159–168
Saugstad OD (2001) Is oxygen more toxic than currently believed? Pediatrics 108:1203–1205. doi:10.1542/peds.108.5.1203
Vexler ZS, Ferriero DM (2001) Molecular and biochemical mechanisms of perinatal brain injury. Semin Neonatol 6:99–108. doi:10.1053/siny.2001.0041
Oltvai ZN, Milliman CL, Korsmeyer SJ (1993) Bcl-2 heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programmed cell death. Cell 74:609–619. doi:10.1016/0092-8674(93)90509-O
Ito T, Deng X, Carr B et al (1997) Bcl-2 phosphorylation required for anti-apoptosis function. J Biol Chem 272:11671–11673. doi:10.1074/jbc.272.18.11671
Haldar S, Chintapalli J, Croce CM (1996) Taxol induces Bcl-2 phosphorylation and death of prostate cancer cells. Cancer Res 56:1253–1255
Haldar S, Jena N, Croce CM (1995) Inactivation of Bcl-2 by phosphorylation. Proc Natl Acad Sci USA 92:4507–4511. doi:10.1073/pnas.92.10.4507
Lamprecht WSP, Heinz F, Weissner H (1974) Creatine phosphate. In: Bergmeyer HU (ed) Methods of enzymatic analysis, vol 4. Academic Press, New York, pp 1777–1781
Booth RF, Clark JB (1978) A rapid method for the preparation of relatively pure metabolically competent synaptosomes from rat brain. Biochem J 176:365–370
Lowry OH, Rosebrough NJ, Farr AL et al (1951) Protein measurement with the folin phenol reagent. J Biol Chem 193:265–275
Barazzone C, White CW (2000) Mechanisms of cell injury and death in hyperoxia: role of cytokines and Bcl-2 family proteins. Am J Respir Cell Mol Biol 22:517–519
Chandel NS, Budinger GR (2007) The cellular basis for diverse responses to oxygen. Free Radic Biol Med 42:165–174. doi:10.1016/j.freeradbiomed.2006.10.048
Metrailler-Ruchonnet I, Pagano A, Carnesecchi S et al (2007) Bcl-2 protects against hyperoxia-induced apoptosis through inhibition of the mitochondria-dependent pathway. Free Radic Biol Med 42:1062–1074. doi:10.1016/j.freeradbiomed.2007.01.008
Hu ZB, Minden MD, McCulloch EA (1998) Phosphorylation of BCL-2 after exposure of human leukemic cells to retinoic acid. Blood 92:1768–1775
Ruvolo PP, Deng X, Carr BK et al (1998) A functional role for mitochondrial protein kinase Calpha in Bcl2 phosphorylation and suppression of apoptosis. J Biol Chem 273:25436–25442. doi:10.1074/jbc.273.39.25436
Shitashige M, Toi M, Yano T et al (2001) Dissociation of Bax from a Bcl-2/Bax heterodimer triggered by phosphorylation of serine 70 of Bcl-2. J Biochem 130:741–748
Yamamoto K, Ichijo H, Korsmeyer SJ (1999) BCL-2 is phosphorylated and inactivated by an ASK1/Jun N-terminal protein kinase pathway normally activated at G(2)/M. Mol Cell Biol 19:8469–8478
Zha J, Harada H, Yang E et al (1996) Serine phosphorylation of death agonist BAD in response to survival factor results in binding to 14–3-3 not Bcl-X(L). Cell 87:619–628. doi:10.1016/S0092-8674(00)81382-3
Chang BS, Minn AJ, Muchmore SW et al (1997) Identification of a novel regulatory domain in BCL-X(L) and Bcl-2. EMBO J 16:968–977. doi:10.1093/emboj/16.5.968
Truttmann AC, Ashraf Q, Mishra OP et al (2004) Effect of hypoxia on protein phosphatase 2A activity, subcellular distribution and expression in cerebral cortex of newborn piglets. Neuroscience 127:355–363. doi:10.1016/j.neuroscience.2004.05.033
Vander Heiden MG, Chandel NS, Schumacker PT et al (1999) Bcl-xL prevents cell death following growth factor withdrawal by facilitating mitochondrial ATP/ADP exchange. Mol Cell 3:159–167. doi:10.1016/S1097-2765(00)80307-X
Kluck RM, Bossy-Wetzel E, Green DR et al (1997) The release of cytochrome c from mitochondria: a primary site for Bcl-2 regulation of apoptosis. Science 275:1132–1136. doi:10.1126/science.275.5303.1132
Olson M, Kornbluth S (2001) Mitochondria in apoptosis and human disease. Curr Mol Med 1:91–122. doi:10.2174/1566524013364239
Desagher S, Osen-Sand A, Nichols A et al (1999) Bid-induced conformational change of Bax is responsible for mitochondrial cytochrome c release during apoptosis. J Cell Biol 144:891–901. doi:10.1083/jcb.144.5.891
Mikhailov V, Mikhailova M, Pulkrabek DJ (2001) Bcl-2 prevents Bax oligomerization in the mitochondrial outer membrane. J Biol Chem 276:18361–18374. doi:10.1074/jbc.M100655200
Hsu YT, Wolter KG, Youle RJ (1997) Cytosol-to-membrane redistribution of Bax and Bcl-X(L) during apoptosis. Proc Natl Acad Sci USA 94:3668–3672. doi:10.1073/pnas.94.8.3668
Smaili SS, Hsu YT, Carvalho AC et al (2003) Mitochondria, calcium and pro-apoptotic proteins as mediators in cell death signaling. Braz J Med Biol Res 36:183–190
Jurgensmeier JM, Xie Z, Deveraux Q et al (1998) Bax directly induces release of cytochrome c from isolated mitochondria. Proc Natl Acad Sci USA 95:4997–5002. doi:10.1073/pnas.95.9.4997
Luo X, Budihardjo I, Zou H et al (1998) Bid, a Bcl2 interacting protein, mediates cytochrome c release from mitochondria in response to activation of cell surface death receptors. Cell 94:481–490. doi:10.1016/S0092-8674(00)81589-5
Acknowledgments
This study was supported by the National Institutes of Health grant HD-20337 and by iNO therapeutics. The authors express their gratitude to Ms. Anli Zhu for her expert technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brutus, N.A., Hanley, S., Ashraf, Q.M. et al. Effect of Hyperoxia on Serine Phosphorylation of Apoptotic Proteins in Mitochondrial Membranes of the Cerebral Cortex of Newborn Piglets. Neurochem Res 34, 1219–1225 (2009). https://doi.org/10.1007/s11064-008-9898-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-008-9898-z