Abstract
Background
En bloc spondylectomy is the gold standard for surgical resection of sacral chordomas (CHO), but the effect of extent of resection on recurrence and survival in patients with CHO of the cervical spine remains elusive.
Methods
MEDLINE, Embase, Scopus, and Cochrane were systematically reviewed. Patients with cervical CHO treated at three tertiary-care academic institutions were reviewed for inclusion. We performed an individual participant data meta-analysis to assess the overall survival (OS) and progression free survival (PFS) after en bloc-gross total resection (GTR) and intralesional-GTR compared to subtotal resection (STR). We then performed an intention-to-treat analysis including all patients with attempted en bloc resection in the en bloc group, regardless of the surgical margins.
Results
There was a total of 13 series including 161 patients with cervical CHO, including our current series of 22 patients. GTR (en bloc-GTR + intralesional-GTR) was associated with a significant decrease in the risk of local progression (pooled hazard ratio (PHR) = 0.22; 95% CI 0.08–0.59; p = 0.003) and risk of death (PHR 0.31; 95%; CI 0.12–0.83; p = 0.020). A meta-regression analyses determined that intralesional-GTR improved PFS (PHR 0.35; 95% CI 0.16–0.76; p = 0.009) as well as OS (PHR 0.25; 95% CI 0.08–0.79; p = 0.019) when compared to STR. En bloc-GTR was associated with a significant reduction in the risk of local progression (PHR 0.06; 95% CI 0.01–0.77; p = 0.030), but not a decreased OS (PHR 0.50; 95% CI 0.19–1.27; p = 0.145). Our intention-to-treat analyses revealed a near significant improvement in OS for the en bloc group (PHR: 0.15; 95% CI 0.02–1.22; p = 0.054), and nearly identical improvement in PFS. Radiation data was not available for the studies included in the meta-analysis.
Conclusion
This is the first and only meta-analysis of patients with cervical CHO. We found that both en bloc-GTR and intralesional-GTR resulted in improved local tumor control when compared to STR.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chordomas (CHO) are the most common primary malignant spinal bone tumor with an age-adjusted incidence of 0.088 per 100,000 persons per year [1, 2]. CHOs of the cervical spine are especially troublesome, as close association or even juxtaposition of critical structures such as the vertebral arteries, esophagus, cervical nerve roots, or the spinal cord itself make surgery a daunting task. Studies have shown that patients with cervical CHOs appear to have worsened overall survival (OS) when compared to patients with CHO of other spinal regions [3]. Intuitively, this should be expected association, as tumor extension toward the aforementioned structures will lead to significantly diminished quality of life and eventual death. Gross total resection (GTR) can be either intralesional, with piecemeal removal of the tumor, or en bloc, and there is ample evidence that en bloc resection results in improved local control for patients with sacral CHOs [4,5,6]. The sin qua non of chordoma management is en bloc resection of the tumor, as CHO will nearly inevitably return unless it is resected with clear margins. This can often be accomplished with tedious pre-surgical planning, using the preoperative imaging as a guide. The Weinstein, Boriani, Biagnini (WBB) surgical staging system classifies the tumors according their zone of infiltration surrounding the spinal cord, and can be useful to describe the location of the tumor [7, 8]. While en bloc resection is typically feasible in the sacral spine, it is not typically possible with cervical CHOs and therefore intralesional resection is often the standard of care.
With the advent of focused image guided proton-based radiation, there have been reports of increased progression free survival (PFS) for patients with high-dose radiation [9,10,11,12]. There has been a surge of interest in the development of novel targeted therapies to combat these tumors [13, 14], and there now exists an orthotopic animal model of spinal CHO to test these therapies [15]. While CHO is still certainly a surgical tumor, the advancement of adjuvant therapies calls for us as clinicians and surgeons to reassess the benefit to be gained from large, morbid surgeries compared to smaller decompressive surgeries in certain high-risk regions such as the cervical spine. Literature regarding cervical CHOs are predominantly limited to case reports and case series [16,17,18,19], with no high-level assessment of survival and progression outcomes in this patient cohort. Because any single case series would be unlikely to result in any useful data, a meta-analysis is necessary for this rare but debilitating tumor. In this manuscript, we review our series of patients with cervical CHO at three academic tertiary care institutions, and perform a comprehensive systematic review and meta-analysis of previously published reports to form the highest level of evidence to assess the influence of extent of resection on progression free survival (PFS) and overall survival (OS) for patients with cervical CHO. We hypothesize that there is a significant benefit in PFS and OS by performing GTR in patients with cervical CHO.
Methods
Case series
All patients with primary cervical CHO treated at three tertiary care academic institutions (Mayo Clinic Florida, Minnesota, and Arizona) were retrospectively reviewed after Internal Review Board (IRB) approval. Inclusion criteria were follows: (1) patients with surgical resection of cervical CHO, (2) histopathological confirmation of diagnosis with typical physaliferous cells, (3) complete records available for extraction, (4) available postoperative magnetic resonance imaging (MRI). Exclusion criteria were as follows: (1) patients with CHO of another location besides the cervical spine that metastasized to the cervical spine, (2) patients with lack of information regarding extent of resection, (3) patients without post-operative imaging, and (4) patients with biopsy but no surgical resection of their tumor. Extent of resection was based on intraoperative reports, post-operative imaging, and pathology reports to determine margins of resection for cases of attempted en bloc resection. Patients were noted as having en bloc-GTR resection of their tumor, intralesional GTR (intralesional-GTR), or subtotal resection (STR) of their tumors. Patients with attempted en bloc resection but violated margins positive for tumor were grouped with the intralesional-GTR group. The pre-operative and post-operative MRIs were used to determine the extent of resection through active contour segmentation [20]. The T2-weighted images were used for this measurement. We collected information regarding age, gender, tumor location, extent of resection, use of radiation, radiation dosage, complications, recurrence, and use of molecular targeted therapy (MTT). For radiation, we counted this variable if the patient had immediate preoperative or postoperative radiation with any radiation modality at the time of their primary surgery.
Systematic review
Search strategy
Studies were identified by a medical librarian developing and running searches in the MEDLINE (1946–Present), Embase (1974–Present), Cochrane Central Register of Controlled Trials (1991–Present), and Cochrane Database of Systematic Review (2005–Present) [all via the Ovid interface], Scopus (1823–Present), Science Citation Index Expanded (1975–Present) and Emerging Sources Citation Index (2015–Present) [via the Web of Science interface] and Epistemonikos databases. Grey literature resources were also searched. There were no limits to language or publication date. Filters to remove animal studies were employed. Search terms included database-specific-controlled vocabulary (MeSH, Embase/Emtree terms) and additional free-text terms/keywords such as cervical chordoma, surgical resection, radiation, and radiotherapy. All databases and grey literature resources were searched on November 14th, 2020 and the search strategy was performed according to PRISMA guidelines [21]. The full search strategies are available in Online Appendix.
Study selection
Inclusion criteria were as follows: (1) Manuscripts including patients who underwent resection of their cervical CHO, (2) retrospective and prospective series. Exclusion criteria were as follows: (1) studies that did not report individual patient data for cervical cases, (2) case reports, (3) case series with fewer than three patients.
Data extraction and quality evaluation
We extracted data regarding patient age, sex, tumor location, extent of resection, use of radiation, complications, local recurrence, metastasis, death, and pathology. For extent of resection, patients were grouped according to extent of resection with groups being en bloc resection with negative margins, intralesional-GTR (en bloc resection with positive margins + intralesional-GTR), and subtotal resection (STR). En bloc resection with positive margins and intralesional-GTR were grouped together as intralesional-GTR. Because the process of attempting an en bloc resection is very different from a planned intralesional resection, and there may be a benefit to attempting an en bloc resection even if the outcome was violated margins, we also performed an intention-to-treat analysis, and included all patients with attempted en bloc resection into the en bloc group, regardless of the outcome. For the comparison of upper cervical to lower cervical cases, any tumor that involves the C1 or C2 level was included in the upper cervical group. We assessed quality of evidence using MOOSE Assessment for Quality of Evidence for All Included Studies and Oxford Centre for Evidence-Based Medicine—Levels of Evidence and Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) framework [22]. Risk of bias assessment was assessed using the National Health’s Institute Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [23].
Meta-analysis
Quantitative synthesis of results
In order to quantitatively compare the effect of GTR and STR on PFS and OS, we performed individual participant data meta-analysis of time-to-event outcomes following the recommendations of de Jong et al. [24]. We opted for an individual participant data meta-analysis as the studies presented data on an individual participant level, and an individual participant data meta-analysis offers several advantages compared to “classical” meta-analysis based on aggregated data (such as the possibility of better modelling time-to-event outcomes, and the assessment of intervention-covariate interactions at the participant level). Given the low number of participants per primary study, we opted for a one-stage approach with a log-normal frailty and random-effects (so as to account for within-trial clustering of participants). Results are presented as pooled hazard ratio (HR) with 95% confidence intervals (CI). Heterogeneity was assessed by estimating median hazard ratios, corresponding to the median relative difference in the hazard of the occurrence of the outcome variable when two identical participants from two randomly selected different studies are compared [24]. To identify potential sources of heterogeneity, we built models including covariates and intervention-covariate interactions. In particular, we tested the age and sex of the participants, the number of operated levels, the location of the lesion (upper cervical chordomas, corresponding to all lesions including at least a segment at the level of C2 or above, and lower cervical chordomas corresponding to those below the level of C2 without involving C2). These covariates were centered by their mean values within trials, so as to avoid potential ecological biases resulting from mixing within- and across-study information. The remaining variables were not tested due to large quantities missing data (precluding us from resorting to methods of imputation of missing data). A sensitivity analysis was performed comparing intralesional GTR (including lesions described as “En bloc with positive margins”) versus STR, as it is still uncertain whether removing all visible lesional tissue (even with positive margins) is associated with better outcomes than removing only a part of the lesion. A sensitivity analysis comparing lesions described as en bloc-GTR (including other descriptions of gross total resection with negative margins) versus STR was not performed, on account of the low number of participants undergoing en bloc-GTR. The comparison between en bloc-GTR and intralesional-GTR was not reported due to the low estimates of the precision and very high heterogeneity.
Statistical analysis
All statistical analyses were completed using R software (v 4.0). The correlation between the pre-operative tumor volume and the extent of resection was determined through Pearson correlation coefficient.
Results
Case series
We found 190 patients with surgical resection of CHO treated at our institutions, and then screened for patients with primary cervical CHO. After exclusion of patients with incomplete data, 25 patients were found. We excluded 3 patients with only biopsy and no surgical resection of their lesion resulting in 22 patients included in our analyses (Table 1). There were two patients with en bloc-GTR, six with intralesional-GTR, and fourteen patients with STR (Fig. 1). There was a median PFS of 45 (Standard deviation: 54.1) months for patients with GTR (en bloc + IL GTR) and a PFS of 15.8 (SD: 8.2) months for those with STR of their tumor. The median PFS for patients that had high dose (> 70 Gy) radiation was 49 (SD: 14.4) months, while those patients who received < 70 Gy had a PFS of 31 (SD: 47.9) months. There were only three patients who had preoperative radiation, with all of these patients having STR of their tumors. One of these patients had local recurrence 13 months after surgery, and the other two remain recurrence free 9 and 29 months after surgery. Patients with upper cervical CHO had a median PFS of 12.5 (SD: 44.9) months, while those in the subaxial spine had a median PFS of 35 (SD: 12.9) months. There were 12 recurrences for the cohort combined, with 4 being in the patients with GTR and 8 being in the STR group. The median OS for patients with GTR (en bloc + IL GTR) was 104.8 (SD: 67.4) months while the OS for those with STR was 24.1 (SD: 33.8) months. There were two patients with en bloc resection, and one of these patients had her surgery 12 months prior to this analysis and remains disease free. There was a moderate correlation between preoperative tumor volume and extent of resection achieved, with lower tumor volumes being more likely to have a more extensive resection (Fig. 2). The median extent of resection for patients with STR was 78.6%. There were three complications reported in our cohort, with two being in those with en bloc or IL-GTR of their tumor (dehiscence of posterior pharyngeal wall flap and hemidiaphragm paresis), with the other complication being in a patient with STR of their tumor (brachial plexopathy).
Combined magnetic resonance imaging and artist illustration of different surgical strategies for cervical chordoma. a Preoperative imaging for a patient with upper cervical chordoma. b–d depict cervical chordomas after en bloc gross total resection with ligation of the vertebral artery (b), intralesional gross-total resection (c), and sub-total resection (d)
Meta-analyses
The search strategy resulted in 1524 articles, with 934 remaining after de-duplication. We then excluded 864 articles on the title and abstract. 70 articles underwent full-text review. Our search resulted in 12 articles including 139 patients with cervical CHO (Fig. 3) [17,18,19, 25,26,27,28,29,30,31,32,33]. Including our series resulted in 13 case series and 161 total patients with cervical CHO. There were 118 patients with GTR of their tumor, with 29 of these being an en bloc spondylectomy with negative margins. There were 89 patients with intralesional-GTR of their tumor, which includes 4 patients with attempted en bloc resection that had violated margins. There were 43 patients with STR of their tumor. The mean follow up for included studies ranged from 27 to 67 months, with 8 of the 13 studies having greater than 50 months of mean follow-up for the included patients. The characteristics for each study are included in Table 2.
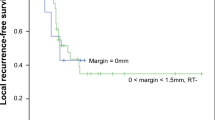
Progression-free survival
A total of nine studies provided data on PFS, including 109 participants, with 49 events of local progression (Table 3). GTR was associated with a significant decrease in the risk of local progression (pooled HR 0.22; 95% CI 0.08–0.59; p = 0.003). The median HR was 2.72, representing high heterogeneity. Age, location, gender and the number of levels were not found to be moderators of heterogeneity. There was a trend towards significance for tumor location (pooled HR 2.56, 95% CI 0.95–6.88; p = 0.063), with tumors involving the atlantoaxial spine (C1/C2) having a worsened prognosis. This trend indicates that if there were more numbers, this variable would likely reach significance.
A meta-regression analysis determined that en bloc-GTR was associated with a significant reduction in the risk of local progression (pooled hazard ratio 0.06; 95% CI 0.01–0.77; p = 0.030). The median HR was 3.49, representing high heterogeneity. Age, gender, location and the number of levels being operated were not found to be moderators of heterogeneity. Similar results were observed when comparing intralesional-GTR to STR—with significant reduction in the risk of local progression (pooled HR 0.35; 95% CI 0.16–0.76; p = 0.009), with only moderate heterogeneity (median HR 1.77) and with no moderator variables identified.
Overall survival
A total of twelve studies provided data on overall survival, encompassing a total of 143 participants, with 41 events of death (Table 4). GTR was associated with a significant decrease in the risk of death (pooled HR 0.31; 95% CI 0.12–0.83; p = 0.020). The median HR was 1.04, representing moderate heterogeneity. Age and gender were not found to be moderators of heterogeneity. By contrast, the number of levels was identified as a variable that potentially explains heterogeneity. In fact, despite the lack of association between the number of levels and overall survival (pooled HR 0.83; 95% CI 57–1.21; p = 0.322), we found significant association for the interaction between the number of levels and the type of resection achieved (pooled HR 2.16; 95% CI 1.10–4.26; p = 0.026).
En bloc-GTR was not associated with a significant decrease in the risk of death (pooled HR 0.14; 95% CI 0.01–1.27; p = 0.134). The median HR was 2.65, representing high heterogeneity. Age, gender, and number of levels were not found to be moderators of heterogeneity. We were unable to evaluate the lesion location as a variable moderator of heterogeneity due to lack of precision of the estimates. Intralesional-GTR was associated with a significant decrease in the risk of death when compared with STR (pooled hazard ratio = 0.25; 95% CI 0.08–0.79; p = 0.019) The median HR was 1.50 indicating moderate heterogeneity. Age and gender were not found to be moderators of heterogeneity. The number of levels being operated was the only variable potentially identified as a moderator of heterogeneity, as we found a significant association for the interaction between the number of levels and the type of resection achieved (pooled HR 2.54; 95% CI 1.12–5.78; p = 0.026).
Intention to treat analyses
It is unclear whether intending to complete an en bloc resection has an effect on patient outcomes, even if the resection results in a violated margin. To account for this, we performed an intent-to-treat analysis and included patients who underwent en bloc resection with violated margins into the en bloc group. There was a nearly identical improvement in PFS for in this analysis of en bloc versus STR (pooled HR: 0.06; 95% CI 0.01–0.77 p = 0.031) when compared to the analysis above (pooled hazard ratio = 0.06; 95% CI 0.01–0.77; p = 0.030). The primary difference between the intent to treat analysis and the original analysis is that there was a nearly significant improvement in OS for the en bloc cohort when compared to the STR cohort (pooled HR: 0.15; 95% CI 0.02–1.22; p = 0.054). The results for the intention-to-treat analysis are displayed in supplementary Tables 1 and 2.
Quality assessment and risk of bias
The outcomes assessed for quality were OS and PFS for GTR vs. STR, en bloc-GTR vs. STR, and intralesional-GTR vs. STR. The certainty was graded as low for these analyses (Table 5). The GRADE assessment is included in Table 6, with a low certainty for the included analyses. Risk of bias assessment is included in Fig. 4.
Discussion
Cervical CHOs are distinct from CHOs of other areas of the neuro-axis in that there is significant risk associated with close relation and often times juxtaposition of structures such as the vertebral arteries, cervical spinal cord, and esophagus. Surgical resection with en bloc spondylectomy is typically regarded as more challenging than resection of a tumor in another region such as the lumbar spine or sacrum, because damage to the aforementioned structures will lead to catastrophic complications and even death. GTR with either en bloc spondylectomy or intralesional-GTR of CHOs requires extensive planning and should typically be performed by spine surgeons at high volume tertiary academic centers with extensive experience managing these tumors. Literature has typically favored en bloc resection of CHOs in the sacrum, but there is limited data for or against this resection strategy in the cervical spine [6].
Our study represents the first and only meta-analysis of patients with cervical CHO. This manuscript is also unique in that we performed an individual patient data meta-analysis which gives us the opportunity to assess PFR and OS for the all of the groups together to assess the effect of extent of resection on PFS and OS. We discovered that patients with GTR of their tumor did have an increased PFS and OS compared to those with STR of their tumor. This forms the highest level of evidence to advocate for GTR of cervical CHOs and is consistent with previously published articles for sacral CHOs. Of note, the GTR group includes intralesional-GTR which involves piecemeal resection of the tumor, as well as en bloc spondylectomy with clear margins. Patients with positive margins were included in the intralesional-GTR group. Because these resection strategies are completely different, we performed a meta-regression analyses to determine if one particular type of GTR strategy should be favored over another. We also performed an intention-to-treat analysis including all patients with attempted en bloc resection in one group, regardless of the postoperative margins.
PFS was improved by GTR of the tumors in patients with cervical CHO. Unfortunately, our study was unable to compare the intralesional-GTR and en bloc cases, as the number of events was insufficient for this comparison. However, it is important to note that there was a significant decrease in disease progression for patients en bloc spondylectomy (pooled HR 0.06; 95% CI 0.01–0.77; p = 0.030) and intralesional-GTR (pooled HR 0.25; 95% CI 0.08–0.79; p = 0.019) when compared to STR. Although we could not compare the intralesional-GTR and en bloc groups, the HR for en bloc was higher, which could at least indicate more benefit in risk of recurrence with en bloc resection of tumors. Although our case series was underpowered, using volumetric assessment of the pre-and postoperative tumors volumes, we were able to determine that there is a moderate correlation between the preoperative tumor size and the extent of resection, with smaller tumors being more likely to result in a more extensive resection. For OS, there was a significant improvement with intralesional-GTR, but not with en bloc-GTR. While this could be attributed to low numbers for this assessment, it is reasonable to conclude that. En bloc spondylectomy is a high-risk technique that requires specialized training; thus, should only be performed by experienced spinal surgeons. It is possible that more extensive surgeries may result in greater morbidity and delayed radiation. Unfortunately, there was no way to determine the specific cause of death in the patients, which would provide more insight into this analysis. Our intent-to-treat analysis revealed that when all patients that had attempted en bloc resection (including those with violated margins) were compared to the STR cohort, there was a nearly significant improvement in OS (pooled HR: 0.15; 95% CI 0.02–1.22; p = 0.054). The surgical steps for performing an en bloc resection are much different than those for performing an intralesional resection of a tumor and subject a patient to a different set of complications and morbidity, but also may have more benefit that performing a planned intralesional resection. The improvement in OS when including all patients with attempted en bloc resection indicates that there may be a benefit in the procedure of en bloc resection, even if the surgery results in violated margins.
Radiation therapy with either proton or protons is considered the standard of care for patients with CHO of the skull base or spine. In this study, we sought the better understand the effect of radiation on patients with surgical resection of their CHO. Unfortunately, not all of the included studies commented on the use of radiation, and for the studies that did, there were very few patients who did not receive radiation, which is to be expected. Furthermore, these studies did not report on dosage, or timing of radiation. However, we were able to review the data from our series to determine the effect of high dose (> 70 Gy) radiation. There was a higher mean PFS for patients that had high dose proton-based radiation (49 months), while patients who received < 70 Gy radiation had a PFS of 31 months. Although this analysis was not significant due to low numbers, this poses the question of whether the differences in PFS for the surgical groups are partially related to the dose of radiation given to the patients, but unfortunately, this data was not available in the meta-analysis. In the case series, 43% of the patients with GTR received high dose radiation, while 54% of patients with STR received high dose radiation, which indicates that patients who had residual tumor were slightly more likely to have received high dose radiation which possibly played a role in the outcomes.
Although there was more than two-fold increase in PFS for patients with primary cervical tumors of the subaxial spine when compared to those with tumors involving the atlas or axis, there was no significant difference in this analysis, but would likely have been significant if there were more numbers. When we look at the meta-analysis data, there was a trend toward significance for the effect of tumor location (upper versus lower cervical) on PFS (p = 0.063), with upper cervical tumors having worsened PFS. In addition to this, there was a trend toward significance for the effect that tumor location had on the type of resection achieved, with subaxial tumors being more likely to receive an extensive GTR (p = 0.075). In our cohort, we also assessed the effect of targeted therapy on PFS, but there was no significant difference between the groups. This is likely due to the fact that most patients undergoing targeted therapy for CHO had progressive and advanced disease at the time of initiation of the drug.
Limitations and strengths
Cervical chordomas are rare tumors, and thus the case series was limited by numbers, which is why a meta-analysis was needed to be able to draw conclusions on this topic. This manuscript is subject to the inherent limitations of meta-analyses papers, as the quality of this manuscript primarily relies on the quality of the included studies. This manuscript was unable to quantitatively assess the use of high dose radiation in the large cohort due to lack of data from some of the included manuscripts. We were unable to separate patients with recurrent CHO from those with primary CHO, which may lead to slight skewing of the data, but this remains the highest level of evidence for patients with cervical CHO. Also, ideally our study would stratify STR patients into categories such as < 50% resection and 50–99% resection, to determine if there is benefit from the amount of tumor resection, even if a GTR cannot be achieved, but the study design did not allow for this in-depth analysis. Also, we were unable to confirm the extent of resection for the included studies. Our quality assessment revealed that quality of most of the assessments were rated as low certainty. This is not surprising due to the low numbers available for this specific pathology and should be considered when interpreting the results. CHOs are slow growing tumors, and follow-up of 5–10 years would be ideal for studies involving patients with CHO. This study was limited by variable follow-up of the included studies, but 8 of the included studies had a mean follow-up of at least 50 months. Future studies should consider assessing the percentage of resection using volumetric assessment to help guide clinicians when a GTR cannot be safely achieved. In our series, we were able to obtain a percentage for extent of resection, but this information was not included in any of the other studies in the meta-analysis. We were able to perform an individual participant data meta-analysis, which provides an advantage over normal meta-analyses studies with time-to-event outcomes for this large cohort. An additional strength of this study is the geographic location of the included institutions in the case series, with representation from the Southwest, Southeast, and Midwest.
Conclusions
Despite inherent confounders and the limitations of this study, this is the largest assessment of extent of resection in patients with cervical CHO. Our study indicates that GTR with either with piecemeal resection or en bloc spondylectomy may improve PFS more than STR of CHOs in the cervical spine. A meta-regression analysis of en bloc resection and intralesional-GTR compared to STR found that while they were both were associated with an improved PFS over STR, en bloc resection was associated with a lower HR, which indicates that there may be more benefit with this resection model, when feasible. Although en bloc resection appears to be the gold standard to prevent recurrence in cervical CHOs, surgeons should assess each patient’s tumor carefully, as larger tumors are more difficult to completely remove.
Data availability
Available upon request.
References
Das P, Soni P, Jones J, Habboub G, Barnholtz-Sloan JS, Recinos PF, Kshettry VR (2020) Descriptive epidemiology of chordomas in the United States. J Neurooncol 148:173–178. https://doi.org/10.1007/s11060-020-03511-x
McMaster ML, Goldstein AM, Bromley CM, Ishibe N, Parry DM (2001) Chordoma: incidence and survival patterns in the United States, 1973–1995. Cancer Causes Control 12:1–11. https://doi.org/10.1023/a:1008947301735
Zou MX, Huang W, Wang XB, Li J, Lv GH, Deng YW (2015) Prognostic factors in spinal chordoma: A systematic review. Clin Neurol Neurosurg 139:110–118. https://doi.org/10.1016/j.clineuro.2015.09.012
Ruosi C, Colella G, Di Donato SL, Granata F, Di Salvatore MG, Fazioli F (2015) Surgical treatment of sacral chordoma: survival and prognostic factors. Eur Spine J 24(Suppl 7):912–917. https://doi.org/10.1007/s00586-015-4276-4
Colangeli S, Muratori F, Bettini L, Frenos F, Totti F, D’Arienzo A, Campo FR, Scoccianti G, Beltrami G, Campanacci DA, Capanna R (2018) Surgical treatment of sacral chordoma: en bloc resection with negative margins is a determinant of the long-term outcome. Surg Technol Int 33:343–348
D’Amore T, Boyce B, Mesfin A (2018) Chordoma of the mobile spine and sacrum: clinical management and prognosis. J Spine Surg 4:546–552. https://doi.org/10.21037/jss.2018.07.09
Hart RA, Boriani S, Biagini R, Currier B, Weinstein JN (1997) A system for surgical staging and management of spine tumors. A clinical outcome study of giant cell tumors of the spine. Spine (Phila Pa 1976) 22:1773–1782. https://doi.org/10.1097/00007632-199708010-00018
Yamazaki T, McLoughlin GS, Patel S, Rhines LD, Fourney DR (2009) Feasibility and safety of en bloc resection for primary spine tumors: a systematic review by the Spine Oncology Study Group. Spine (Phila Pa 1976) 34:S31-38. https://doi.org/10.1097/BRS.0b013e3181b8b796
Rotondo RL, Folkert W, Liebsch NJ, Chen YL, Pedlow FX, Schwab JH, Rosenberg AE, Nielsen GP, Szymonifka J, Ferreira AE, Hornicek FJ, DeLaney TF (2015) High-dose proton-based radiation therapy in the management of spine chordomas: outcomes and clinicopathological prognostic factors. J Neurosurg Spine 23:788–797. https://doi.org/10.3171/2015.3.SPINE14716
Jin CJ, Berry-Candelario J, Reiner AS, Laufer I, Higginson DS, Schmitt AM, Lis E, Barzilai O, Boland P, Yamada Y, Bilsky MH (2019) Long-term outcomes of high-dose single-fraction radiosurgery for chordomas of the spine and sacrum. J Neurosurg Spine. https://doi.org/10.3171/2019.7.SPINE19515
Gatfield ER, Noble DJ, Barnett GC, Early NY, Hoole ACF, Kirkby NF, Jefferies SJ, Burnet NG (2018) Tumour volume and dose influence outcome after surgery and high-dose photon radiotherapy for chordoma and chondrosarcoma of the skull base and spine. Clin Oncol (R Coll Radiol) 30:243–253. https://doi.org/10.1016/j.clon.2018.01.002
Pennicooke B, Laufer I, Sahgal A, Varga PP, Gokaslan ZL, Bilsky MH, Yamada YJ (2016) Safety and local control of radiation therapy for chordoma of the spine and sacrum: a systematic review. Spine (Phila Pa 1976) 41(Suppl 20):S186–S192. https://doi.org/10.1097/BRS.0000000000001831
Crunkhorn S (2019) Targeted therapy for chordoma. Nat Rev Drug Discov 18:174. https://doi.org/10.1038/d41573-019-00022-x
Cote GM, Barysauskas CM, DeLaney TF, Schwab J, Raskin K, Lozano-Calderon S, Bernstein K, Mullen JT, Haynes AB, Hornicek F, Chen YE, Choy E (2018) A phase 1 study of nilotinib plus radiation in high-risk chordoma. Int J Radiat Oncol Biol Phys 102:1496–1504. https://doi.org/10.1016/j.ijrobp.2018.07.2013
Sarabia-Estrada R, Ruiz-Valls A, Shah SR, Ahmed AK, Ordonez AA, Rodriguez FJ, Guerrero-Cazares H, Jimenez-Estrada I, Velarde E, Tyler B, Li Y, Phillips NA, Goodwin CR, Petteys RJ, Jain SK, Gallia GL, Gokaslan ZL, Quinones-Hinojosa A, Sciubba DM (2017) Effects of primary and recurrent sacral chordoma on the motor and nociceptive function of hindlimbs in rats: an orthotopic spine model. J Neurosurg Spine 27:215–226. https://doi.org/10.3171/2016.12.SPINE16917
Aoun SG, Elguindy M, Barrie U, El Ahmadieh TY, Plitt A, Moreno JR, Truelson JM, Bagley CA (2018) Four-level vertebrectomy for en bloc resection of a cervical chordoma. World Neurosurg 118:316–323. https://doi.org/10.1016/j.wneu.2018.07.153
Wang X, Eichbaum E, Jian F, Chou D (2018) Two-stage en bloc resection of multilevel cervical chordomas with vertebral artery preservation: operative technique. Oper Neurosurg (Hagerstown) 14:538–545. https://doi.org/10.1093/ons/opx178
Molina CA, Ames CP, Chou D, Rhines LD, Hsieh PC, Zadnik PL, Wolinsky JP, Gokaslan ZL, Sciubba DM (2014) Outcomes following attempted en bloc resection of cervical chordomas in the C-1 and C-2 region versus the subaxial region: a multiinstitutional experience. J Neurosurg Spine 21:348–356. https://doi.org/10.3171/2014.5.SPINE121045
Wang Y, Xiao J, Wu Z, Huang Q, Huang W, Zhu Q, Lin Z, Wang L (2012) Primary chordomas of the cervical spine: a consecutive series of 14 surgically managed cases. J Neurosurg Spine 17:292–299. https://doi.org/10.3171/2012.7.SPINE12175
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, Gerig G (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31:1116–1128. https://doi.org/10.1016/j.neuroimage.2006.01.015
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
National Heart Lung and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services (2018) Study quality assessment tools: Quality assessment tool for observational cohort and cross‐sectional studies. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
de Jong VMT, Moons KGM, Riley RD, Tudur Smith C, Marson AG, Eijkemans MJC, Debray TPA (2020) Individual participant data meta-analysis of intervention studies with time-to-event outcomes: a review of the methodology and an applied example. Res Synth Methods 11:148–168. https://doi.org/10.1002/jrsm.1384
Lockney DT, Shub T, Hopkins B, Lockney NA, Moussazadeh N, Lis E, Yamada Y, Schmitt AM, Higginson DS, Laufer I, Bilsky M (2017) Spinal stereotactic body radiotherapy following intralesional curettage with separation surgery for initial or salvage chordoma treatment. Neurosurg Focus 42:E4. https://doi.org/10.3171/2016.9.FOCUS16373
Wang Y, Xu W, Yang X, Jiao J, Zhang D, Han S, Xiao J (2013) Recurrent upper cervical chordomas after radiotherapy: surgical outcomes and surgical approach selection based on complications. Spine (Phila Pa 1976) 38:E1141-1148. https://doi.org/10.1097/BRS.0b013e31829c2bb0
Zhong N, Yang X, Yang J, Meng T, Yang C, Yan W, Xiao J (2017) Surgical consideration for adolescents and young adults with cervical chordoma. Spine (Phila Pa 1976) 42:E609–E616. https://doi.org/10.1097/BRS.0000000000001911
Zileli M, Kilincer C, Ersahin Y, Cagli S (2007) Primary tumors of the cervical spine: a retrospective review of 35 surgically managed cases. Spine J 7:165–173. https://doi.org/10.1016/j.spinee.2006.04.027
Potluri S, Jefferies SJ, Jena R, Harris F, Burton KE, Prevost AT, Burnet NG (2011) Residual postoperative tumour volume predicts outcome after high-dose radiotherapy for chordoma and chondrosarcoma of the skull base and spine. Clin Oncol (R Coll Radiol) 23:199–208. https://doi.org/10.1016/j.clon.2010.09.011
Hyun SJ, Kim JW, Kim KJ, Jahng TA, Roh SW, Ra YS, Kim HJ, Rhim SC (2018) Long-term results following surgical resection of chordomas in the craniocervical junction and the upper cervical spine: review of 12 consecutive cases. Oper Neurosurg (Hagerstown) 14:112–120. https://doi.org/10.1093/ons/opx082
Zhou H, Jiang L, Wei F, Yu M, Wu F, Liu X, Liu Z, Dang G (2014) Chordomas of the upper cervical spine: clinical characteristics and surgical management of a series of 21 patients. Chin Med J (Engl) 127:2759–2764
Barrenechea IJ, Perin NI, Triana A, Lesser J, Costantino P, Sen C (2007) Surgical management of chordomas of the cervical spine. J Neurosurg Spine 6:398–406. https://doi.org/10.3171/spi.2007.6.5.398
Bergh P, Kindblom LG, Gunterberg B, Remotti F, Ryd W, Meis-Kindblom JM (2000) Prognostic factors in chordoma of the sacrum and mobile spine: a study of 39 patients. Cancer 88:2122–2134. https://doi.org/10.1002/(sici)1097-0142(20000501)88:9%3c2122::aid-cncr19%3e3.0.co;2-1
Acknowledgements
Tara Brigham MLIS, AHIP-D.
Funding
AQH was supported by the Mayo Clinic Professorship, the Mayo Clinic Clinician Investigator award, the Florida Department of Health Cancer Research Chair Fund, as well as the National Institutes of Health (Grant Nos. R43CA221490, R01CA200399, R01CA195503, R01CA216855 and R33CA24018).
Author information
Authors and Affiliations
Contributions
OOA: writing manuscript, search for systematic review, statistical analysis, reviewed final, DG: writing manuscript, tables, figures, RD: tables, figures, search for systematic review, TV: figures, edited manuscript, BS: statistical analysis, MB: critically revised manuscript, MJC: critically revised manuscript, ZLG: critically revised manuscript, MAK: critically revised manuscript, KA: critically revised manuscript, AQ: critically revised manuscript, study supervision.
Corresponding author
Ethics declarations
Conflict of interest
Authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Akinduro, O.O., Garcia, D.P., Domingo, R.A. et al. Cervical chordomas: multicenter case series and meta-analysis. J Neurooncol 153, 65–77 (2021). https://doi.org/10.1007/s11060-021-03742-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03742-6