Abstract
Background
The recurrence rate of cervical chordomas is high, and hence it is important to discern the prognostic factors for local relapse and overall survival (OS).
Methods
A retrospective review of 52 patients with cervical chordoma operated in our institution from January 1999 to March 2015 was performed. The association of clinicopathologic characteristics with local relapse-free survival (LRFS) and OS was analyzed. Univariate analysis was performed to determine whether tumor characteristics and types of therapy affected prognosis, and a multivariate Cox proportional hazard model was developed to further investigate local recurrence and mortality.
Results
Mean follow-up time was 50 months. The cumulative 5- and 10-year LRFS was 35 and 0%, respectively, while the cumulative 5- and 10-year OS was 69 and 53%, respectively. The univariate analysis identified contiguous segments involved, intralesional surgical margin at primary surgery, primary surgery in local hospital, incisional biopsy, and without adjuvant radiotherapy as negative prognostic factors for LRFS, whereas for OS, only tumor location in the upper cervical spine was statistically significant. In the multivariate analysis, contiguous vertebral segments involved, intralesional surgical margins, and incisional biopsy were identified as negative prognostic factors for LRFS, whereas for OS, again only tumor location in the upper cervical spine was statistically significant.
Conclusions
Contiguous vertebral segments involved, intralesional surgical margin, without adjuvant radiotherapy, and incisional biopsy significantly increase local recurrence, while tumor location in the upper cervical spine significantly increases tumor-related mortality. Thus, computed tomography-guided fine-needle aspiration biopsy and total spondylectomy with marginal excision may improve survival of patients with cervical chordoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chordomas are rare malignant primary bone tumors that occur exclusively in the axial skeleton.1 Surgery continues to be the primary treatment modality in the management of chordoma because of its resistance to conventional-dose radiotherapy.2 , 3 and unresponsiveness to cytotoxic chemotherapy.4 , 5 Achieving a wide or marginal resection is crucial for surgical outcomes;6 however, the anatomical structures that surround the cervical spine make resection with clean margins very difficult.7 The main cause of treatment failure in cervical chordoma is local relapse,8 which results in poor long-term prognosis.9 Tumors located in the craniocervical junction have an inferior relapse-free survival (RFS) and overall survival (OS) compared with those located in the cervical spine.10 We previously reported the high recurrence rate of chordomas located in the upper cervical spine;11 however, due to the low incidence of this condition, its study has been limited and the currently available evidence mostly stems from case series.
The purpose of this study was to expand our previous findings11 with a longer follow-up time and the inclusion of more patients. Our objective was to identify prognostic factors of local relapse and OS by evaluating the clinical outcomes of 52 patients with cervical spine chordomas treated surgically in a single referral center in China.
Materials and Methods
A retrospective review was performed to identify all cases of cervical chordoma treated at the Peking University Third Hospital from January 1999 to March 2015. The inclusion criteria were conventional chordomas located in the cervical spine that received surgical treatment at our institution, either for a primary tumor or a relapse, and with a minimum follow-up period of 6 months unless the patient died before this time point, in which case they were still included. Patients were excluded if the chordoma subtype was not conventional, but was chondroid or dedifferentiated, or if they were not treated surgically. Ethical permission was granted by the Ethics Committee of Peking University of Health Science Center (No. IRB00001052-08044) and written informed consent was obtained from all patients.
Of the 61 patients with chordoma treated in our hospital, one patient had a chondroid chordoma, three patients had dedifferentiated chordomas, and five refused to undergo surgery. Thus, a total of 52 consecutive patients met the inclusion criteria and were included in this study.
Data extraction comprised patient age, sex, duration of preoperative symptoms, neurological symptoms, tumor location, number of segments affected, type of biopsy used as the diagnostic method, institution in which the primary surgical procedure was performed, type of surgical margins of the primary surgery, and adjuvant radiotherapy, as well as further follow-up information such as local relapse, distant metastases, and survival.
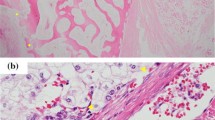
In our center, total spondylectomy was the procedure of choice to achieve total gross tumor resection. Whenever possible, total spondylectomy was performed and our surgical procedure was based on two types of exposed surgical margin. Preoperative planning involved the tumor capsule being kept intact until the edges were clearly exposed. If the planned marginal margin was exposed, which meant the exposed surgical margin was marginal (Fig. 1), then the tumor and the involved vertebral body was resected to achieve total spondylectomy. If the planned marginal margin could not be exposed from the surrounding tissue, the exposed surgical margin was considered intralesional.
Male, 32 years of age, C2 chordoma. a Sagittal CT showed osteolytic destruction with a pathological fracture. b Sagittal MRI showed the vertebral and paravertebral tumor. c The most important step of the posterior approach was to dissect and isolate the vertebral arteries (arrow refers to the vertebral artery). d The anterior transmandibular approaches, and e the tumor capsule was kept intact until the edges were clearly exposed. The tumor and the involved vertebral body can be removed until the planned margin is achieved. f, g Twelve months after operation, Sagittal CT showed internal fixation and confirmed total spondylectomy of C2. CT computed tomography, MRI magnetic resonance imaging
All cases were performed using combined approaches. The posterior midline approach was performed in the prone position to expose extracapsular elements by muscle retraction. The most important step was to dissect and isolate the vertebral arteries (Fig. 1c). Fixation was achieved using a cervical rod, or an occipital plate with a cervical rod, in patients with tumors in the upper cervical spine. Chordomas located in the upper cervical spine (C1–C2) were removed using the high retropharyngeal12 or transoral/transmandibular approaches,13 whereas tumors located in the lower cervical spine (C3–C7) were removed using anterolateral approaches.9 In all cases, extreme care was taken to ensure that the tumor capsule was kept intact until the edges were clearly exposed. Once this was achieved, both the tumor and the involved vertebral body were resected. All patients were further treated according to the same follow-up protocol. Clinical follow-up was conducted at 3, 6, 12, 18, and 24 months, and annually thereafter.
Clinicopathologic characteristics were evaluated with regard to their potential prognostic value for local RFS (LRFS) and OS. LRFS was defined as the time interval from surgery to the first local relapse; however, in the case of a patient’s death or loss to follow-up, the date of the last available follow-up was used for censoring. OS was defined as the time interval from surgery to death; however, in the case of loss to follow-up, the date of the last available follow-up was used for censoring. Kaplan–Meier survival analyses were performed to evaluate LRFS and OS, and Greenwood’s estimate was used to construct asymptotic confidence intervals (CIs) for the survival distribution. Univariate analysis was performed using the log-rank test in order to identify prognostic variables, and the significance level was set at p ≤ 0.05. Subsequently, for the development of a multivariate Cox proportional hazard model, clinically relevant variables with a p value ≤ 0.15 in the univariate analysis were included to investigate their predictive value for LRFS and OS. Due to the issue of multicollinearity, some variables could not be included in the Cox regression model. Statistical analysis was performed using STATA version 14.0 (StataCorp LLC, College Station, TX, USA).
Results
Mean follow-up time was 50 months (median 31 months, range 1–228 months), the study group comprised 28 men and 24 women with a mean age of 47.1 ± 16.7 years (range 5–70), and the mean duration of preoperative symptoms was 12.3 ± 12.2 months (range 2–60). Surgery improved neurologic symptoms so that 29 patients (56%) had neurological symptoms prior to surgery, whereas only ten patients (19%) still had symptoms after surgery. The site of origin was the upper cervical spine (C1–C2) in 29 patients (56%) and the lower cervical spine (C3–C7) in 23 patients (44%). The preoperative diagnostic biopsy was based on computed tomography (CT)-guided fine-needle aspiration (FNA) in 29 cases (56%) and incisional biopsy in 23 cases (44%). All conventional chordomas were Enneking stage IB,14 except for two cases that were stage IA. At the time of the first observation in our hospital, 35 patients (67%) had primary disease, whereas 17 patients (33%) had undergone the primary surgical procedure in a local hospital and had been transferred to our institution due to local tumor recurrence. The primary procedure, regardless of whether it was carried out at our institution or elsewhere, was performed with intralesional surgical margins in 32 patients (62%) and marginal surgical margins in 20 patients (38%). In all patients with intralesional margins, two or more contiguous levels were involved. Thirty-six patients (69%) received adjuvant radiation therapy, whereas none of the patients received chemotherapy.
Four patients were lost to follow-up in the second year after the procedure, two of whom had their primary procedure performed with marginal margins in our hospital. The remaining two patients had undergone incisional biopsy for diagnosis and had their primary procedure performed with intralesional margins in a local hospital.
Over a 10-year period, the cumulative LRFS rate was 0%, with a median time to local relapse of 2.7 years (Fig. 2), while the cumulative 10-year OS rate was 53.2% (95% CI 32.7–70.1%) (Fig. 3). When evaluating the two endpoints over a 5-year period, the cumulative LRFS rate was 35.3% (95% CI 19.3–51.7%) and the cumulative OS rate was 68.8% (95% CI 51.7–80.9%).
Kaplan–Meier analysis of cumulative local relapse-free survival following surgery. Number at risk indicates the number of patients included in the analysis, and tick marks indicate censored observations. Note that the last patient in the analysis had a local relapse 118 months after surgery, therefore, from this time point onwards, the cumulative local relapse-free survival was 0%
Univariate analysis (Table 1) identified involvement of multiple contiguous segments (p = 0.018), intralesional surgical margin at primary surgery (p < 0.001), primary surgical procedure not performed at our institution (p < 0.001), and use of incisional biopsy as the diagnostic method (p = 0.007) as prognostic factors for local recurrence, while location of the tumor in the upper cervical spine (p = 0.027) was identified as a prognostic factor for mortality.
Based on the results of the univariate analysis, multivariate Cox regression models were built. Due to the effect of multicollinearity (the hospital performing the primary surgical procedure was highly associated with the type of diagnostic biopsy and type of surgical margin, which did not allow for the inclusion of more than one of these variables in any of the models), three separate models were developed. Two of the models investigated prognostic factors for local recurrence and another model investigated prognostic factors for mortality (Table 2). According to Model 1 for recurrence, which included contiguous segments, adjuvant radiotherapy, and type of surgical margin as independent variables, there was a significant association between local recurrence and the involvement of contiguous segments (p = 0.016), no adjuvant radiotherapy (p = 0.032), and intralesional margins (p = 0.001). In Model 2 for recurrence, where the type of surgical margin was replaced with the diagnostic method, we found that incisional biopsy significantly increased the risk of local recurrence (p = 0.007), whereas the effect of adjuvant radiotherapy was attenuated compared with Model 1. The model investigating mortality identified one prognostic factor, namely the location of the tumor in the upper cervical spine (p = 0.032).
Discussion
In this series of 52 surgical cases, we identified several prognostic factors for LRFS and OS. Our univariate analysis results showed that age, sex, duration of preoperative symptoms, preoperative neurological impairment, and distant metastasis had no prognostic value for LRFS or OS in cervical chordomas.
In the multivariate regression models, contiguous segments involved, intralesional surgical margin at primary surgery, without adjuvant radiotherapy, and incisional biopsy were negative prognostic factors for LRFS, while tumor location in the upper cervical spine was a negative prognostic factor for OS.
Tumor Characteristics: Stage and Histology
Other researchers have shown that besides tumor size, characteristics such as histological grade and stage of chordoma are major prognostic factors. Zou et al.15 showed that invasion of the surrounding muscle was a predictor of recurrence, while Mukherjee et al.16 demonstrated that the extent of local tumor invasion was a prognostic factor for recurrence. However, in our series, all tumors were conventional chordomas, and all but two tumors were stage IB. For two stage IA cases, there was obvious intercellular myxoid matrix, and some nuclei of tumor cells show obvious atypical (pictures not shown); however, no cytoplasmic eosinophilic hyaline globules were observed in the tumor cell. Although there was overlap in immunohistochemical reactivity of benign notochord tumors and chordomas,17 , 18 we still prefer the diagnosis of chordoma. Therefore, neither histological grade nor tumor stage could be analyzed with regard to their prognostic value.
Tumor Size
Our finding that the involvement of two or more contiguous vertebral segments is a negative prognostic factor for LRFS corresponds well to the findings of Stacchiotti et al.,19 who identified tumor size as a negative prognostic factor for both LRFS and OS. This may be explained by the difficulty in achieving marginal resection in large tumors,19 which is a complex surgical procedure and marginal resection is much more difficult than in single segments.20 Hence, in our series, only 24 of 32 tumors expanding over contiguous spinal levels could be excised with planned margins.
Location of Tumor
In our series, location of the chordoma in the lower cervical spine was identified as a positive prognostic factor for OS. This corresponds to the findings of Meng et al.,21 who also showed that patients with a tumor located in C3–L5 survived longer than patients with tumors located in C1–C2. In contrast to us, Meng et al. performed wide surgical resection; however, the anatomical conditions of the upper cervical spine make wide resection technically demanding and therefore hard to achieve. Contrary to our findings, as well as those of Meng et al., other researchers suggest that the sites of chordoma were of uncertain prognostic value; however, their conclusion is derived from a comparison of all spinal regions, such as lumbar vs. high sacrum [S1–S2] versus low sacrum [S3–coccyx], C1–2 versus C3–L5,15 or C1–2 versus C3–S5.20 Since the results of our series come from a relatively homogeneous group of 52 surgical patients with conventional chordomas in the cervical spine, we believe this minimized confounding effects brought upon by including too many different location categories.
When interpreting the site of the tumor in the upper cervical spine as a negative prognostic factor, it should be considered that in this region, total en bloc spondylectomy is impossible due to the surrounding anatomical structures.22 Instead, tumors undergo piecemeal excisions with specific approaches, such as transoral, transmandibular, or lateral extrapharyngeal.22 , 23 Although local recurrence was not a significant predictor for OS in our series (p = 0.105), this has been reported in other publications.24 Another possible reason for the high local recurrence rate of upper cervical chordomas in some centers is that low-dose adjuvant radiation is administered; results appear to be superior with higher radiation doses delivered with protons or other advanced radiation techniques.25 – 28
Surgical Margin
Our study has further demonstrated that marginal resection is a positive prognostic factor for LRFS. This finding is similar to what has been reported for chordomas located in the sacral29 , 30 or mobile spine.7 Marginal resection is usually the prime goal of surgical treatment of chordomas located at the cervical spine because, even though resection with wide margins would be preferable, local anatomic conditions hardly ever allow this.
Local Hospital Procedures: Diagnostic Tools and Type of Resection
Some factors we analyzed for potential prognostic value are primarily determined by the individual hospital’s standard of care. This is reflected by the multicollinearity of the following variables: hospital performing the primary procedure (local hospital or our hospital), diagnostic biopsy method (FNA or incisional), and type of resection (marginal or intralesional).
Our institution is a specialized referral center, but, unfortunately in China, access to this type of institution is not always easy due to the costs and long distances involved. Undergoing the primary procedure at our institution was a significant positive prognostic factor for LRFS in univariate analysis, and multivariate analysis demonstrated the positive effect of FNA as a diagnostic procedure and excision technique with marginal margins. This is well in line with the recommendations given by other researchers that preoperative histological diagnosis should be performed, but incisional biopsy should be avoided due to the risk of unrecoverable seeding.31 , 32 In general, our results regarding factors that are determined by local hospital routine, such as the use of diagnostic procedures and the technique used for tumor excision, imply that patients benefit from the routine procedures that were developed in referral centers, based on their vast experience.
Adjuvant Radiotherapy
Although some researchers suggest that conventional dose radiotherapy is ineffective for treating chordoma,33 , 34 it has been widely used as an adjuvant treatment for chordomas of the spine.35 Recent data have suggested that proton therapy is an effective adjuvant to surgery when en bloc is not feasible or when margins are violated.25 – 27 In our study, the tumors subjected to adjuvant radiotherapy could be controlled better than those not subjected to radiotherapy, which is consistent with previous results reported from other spinal regions.33
Strengths and Limitations of the Study
To our knowledge, the present study is the largest series of uniform patients with cervical chordomas from a single institution. The rarity of chordoma makes appropriately powered randomized clinical trials challenging, which is why case series provide a significant contribution to the available evidence.
Nonetheless, our study also has limitations. First, the study group is small, which resulted in limited options for statistical analysis, e.g. the multivariate models would not allow inclusion of more than three variables. Second, the study group is a mix of patients with primary surgery and surgery for recurrence, which had an impact on the homogeneity of our study group. Third, the median follow-up of 31 months is still relatively short for this disease since recurrences can occur after 5 years.
Conclusion
Contiguous vertebral segments involved, intralesional surgical margin, and incisional biopsy were prognostic factors for local recurrence, while chordoma location in the upper cervical spine was a prognostic factor for mortality.
References
Bergh P, Kindblom LG, Gunterberg B, Remotti F, Ryd W, Meis-Kindblom JM. Prognostic factors in chordoma of the sacrum and mobile spine: a study of 39 patients. Cancer. 2000; 9:2122–34.
Sahgal A, Chan MW, Atenafu EG, Masson-Cote L, Bahl G, Yu G, et al. Image-guided, intensity-modulated radiation therapy (Ig-Imrt) for skull base chordoma and chondrosarcoma: preliminary outcomes. Neuro Oncol. 2015; 6:889–94.
Tsai EC, Santoreneos S, Rutka JT. Tumors of the skull base in children: review of tumor types and management strategies. Neurosurg Focus. 2002; 5:1–13.
Diaz RJ, Guduk M, Romagnuolo R, Smith CA, Northcott P, Shih D et al. High-resolution whole-genome analysis of skull base chordomas implicates Fhit loss in chordoma pathogenesis. Neoplasia. 2012; 9:788–98.
Dhall G, Traverso M, Finlay JL, Shane L, Gonzalez-Gomez I, Jubran R. The role of chemotherapy in pediatric clival chordomas. J Neurooncol. 2011; 3:657–62.
Amendola L, Cappuccio M, De Iure F, Bandiera S, Gasbarrini A, Boriani S. En bloc resections for primary spinal tumors in 20 years of experience: effectiveness and safety. Spine J. 2014; 11:2608–17.
Boriani S, Bandiera S, Biagini R, et al. Chordoma of the mobile spine: fifty years of experience. Spine. 2006; 4:493–03.
Dasenbrock HH, Chiocca EA. Skull base chordomas and chondrosarcomas: a population-based analysis. World Neurosurg. 2015; 4:468–70.
Molina CA, Ames CP, Chou D, et al. Outcomes following attempted en bloc resection of cervical chordomas in the C-1 and C-2 region versus the subaxial region: a multiinstitutional experience. J Neurosurg Spine. 2014; 3:348–56.
Yasuda M, Bresson D, Chibbaro S, et al. Chordomas of the skull base and cervical spine: clinical outcomes associated with a multimodal surgical resection combined with proton-beam radiation in 40 patients. Neurosurg Rev. 2012; 2:171–83.
Zhou H, Jiang L, Wei F, et al. Chordomas of the upper cervical spine: clinical characteristics and surgical management of a series of 21 patients. Chin Med J (Engl). 2014; 15:2759–64.
Wei F, Liu Z, Liu X, et al. (2015) An approach to primary tumors of the upper cervical spine with spondylectomy using a combined approach: our experience with 19 cases. Spine doi:10.1097/BRS.0000000000001007.
Jiang L, Liu Z, Liu X, et al. Upper cervical spine chordoma of C2–C3. Eur Spine J. 2009; 3:293–300.
Enneking WF, Spanier SS, Goodman MA. The classic: a system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 2003; 415:4–18.
Zou MX, Huang W, Wang XB, Li J, Lv GH, Deng YW. Prognostic factors in spinal chordoma: a systematic review. Clin Neurol Neurosurg. 2015; 139:110–8.
Mukherjee D, Chaichana KL, Parker SL, Gokaslan ZL, McGirt MJ. Association of surgical resection and survival in patients with malignant primary osseous spinal neoplasms from the Surveillance, Epidemiology, and End Results (Seer) Database. Eur Spine J. 2013; 6:1375–82.
Kreshak J, Larousserie F, Picci P, et al. Difficulty distinguishing benign notochordal cell tumor from chordoma further suggests a link between them. Cancer Imaging. 2014; 14:4.
Zhou H, Liu Z, Liu C, et al. Cervical chordoma in childhood without typical vertebral bony destruction: case report and review of the literature. Spine. 2009; 14:E493–7.
Stacchiotti S, Casali PG, Lo Vullo S, et al. Chordoma of the mobile spine and sacrum: a retrospective analysis of a series of patients surgically treated at two referral centers. Ann Surg Oncol. 2010;17(1):211–9.
Zhou H, Chen CB, Lan J, et al. Differential proteomic profiling of chordomas and analysis of prognostic factors. J Surg Oncol. 2010; 7:720–7.
Meng T, Yin H, Li B, et al. Clinical features and prognostic factors of patients with chordoma in the spine: a retrospective analysis of 153 patients in a single center. Neuro Oncol. 2015; 5:725–32.
Choi D, Melcher R, Harms J, Crockard A. Outcome of 132 operations in 97 patients with chordomas of the craniocervical junction and upper cervical spine. Neurosurgery. 2010; 1:59–65.
Wewel JT, Nunna RS, Tan LA, Kasliwal MK, O’Toole JE. Novel reconstruction of the anterior craniocervical junction using an expandable cage with integrated fixation after total C2 spondylectomy for chordoma. J Clin Neurosci. 2016;30:157–60.
Schonegger K, Gelpi E, Prayer D, et al. Recurrent and metastatic clivus chordoma: systemic palliative therapy retards disease progression. Anti-cancer Drug. 2005; 10:1139–43.
Weber DC, Malyapa R, Albertini F, et al. Long term outcomes of patients with skull-base low-grade chondrosarcoma and chordoma patients treated with pencil beam scanning proton therapy. Radiother Oncol. 2016; 1:169–74.
Kabolizadeh P, Chen YL, Liebsch N, et al. Updated outcome and analysis of tumor response in mobile spine and sacral chordoma treated with definitive high-dose photon/proton radiation therapy. Int J Radiat Oncol Biol Phys. 2017; 2:254–62.
Pennicooke B, Laufer I, Sahgal A, et al. Safety and local control of radiation therapy for chordoma of the spine and sacrum: a systematic review. Spine. 2016; 20:S186–92.
Holliday EB, Mitra HS, Somerson JS, et al. Postoperative proton therapy for chordomas and chondrosarcomas of the spine: adjuvant versus salvage radiation therapy. Spine 2015; 8:544–9.
Varga PP, Szoverfi Z, Fisher CG, et al. Surgical treatment of sacral chordoma: prognostic variables for local recurrence and overall survival. Eur Spine J. 2015; 5:1092–101.
Baratti D, Gronchi A, Pennacchioli E, et al. Chordoma: natural history and results in 28 patients treated at a single institution. Ann Surg Oncol. 2003; 3:291–6.
Stacchiotti S, Sommer J. Building a global consensus approach to chordoma: a position paper from the medical and patient community. Lancet Oncol. 2015; 2:e71–83.
Fisher CG, Goldschlager T, Boriani S, et al. An evidence-based medicine model for rare and often neglected neoplastic conditions. J Neurosurg Spine. 2014; 5:704–10.
Rotondo RL, Folkert W, Liebsch NJ, et al. High-dose proton-based radiation therapy in the management of spine chordomas: outcomes and clinicopathological prognostic factors. J Neurosurg Spine. 2015;23(6):788–97.
DeLaney TF, Liebsch NJ, Pedlow FX, et al. Long-term results of phase II study of high dose photon/proton radiotherapy in the management of spine chordomas, chondrosarcomas, and other sarcomas. J Surg Oncol. 2014; 2:115–22.
Yang L, Bai HX, Lee AM, et al. The role of radiotherapy in the treatment of spinal chordomas: an integrative analysis of 523 cases. Neuro Oncol. 2015; 10:1419–20.
Acknowledgement
The author was supported by the AO Foundation via an AOSpine fellowship at AO Clinical Investigation and Documentation (AOCID). Special thanks go to the ACID staff. The authors would also like to thank Dr. Shao-min Yang, Professor of Pathology, Department of Pathology, Peking University Health Science Center, for help with pathologic diagnosis.
Funding
This work was supported by Grants from the Specialized Research Fund for the Doctoral Program of Higher Education of China (No. 20130001120091).
Disclosures
Hua Zhou, Liang Jiang, Feng Wei, Alexander Joeris, Anahí Hurtado-Chong, Vasiliki Kalampoki, Elke Rometsch, Miao Yu, Fengliang Wu, Lei Dang, Xiaoguang Liu, and Zhongjun Liu have no potential conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Zhou, H., Jiang, L., Wei, F. et al. Prognostic Factors in Surgical Patients with Chordomas of the Cervical Spine: A Study of 52 Cases from a Single Institution. Ann Surg Oncol 24, 2355–2362 (2017). https://doi.org/10.1245/s10434-017-5884-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5884-5