Abstract
Purpose
Many publications report laser-interstitial thermal therapy (LITT) as a viable alternative treatment to craniotomy for radiation necrosis (RN) and re-growing tumor occurring after stereotactic radiosurgery (SRS) for brain metastases. No studies to-date have compared the two options. The aim of this study was to retrospectively compare outcomes after LITT versus craniotomy for regrowing lesions in patients previously treated with SRS for brain metastases.
Methods
Data were collected from a single-institution chart review of patients treated with LITT or craniotomy for previously irradiated brain metastasis.
Results
Of 75 patients, 42 had recurrent tumor (56%) and 33 (44%) had RN. Of patients with tumor, 26 underwent craniotomy and 16 LITT. For RN, 15 had craniotomy and 18 LITT. There was no significant difference between LITT and craniotomy in ability to taper off steroids or neurological outcomes. Progression-free survival (PFS) and overall survival (OS) were similar for LITT versus craniotomy, respectively: %PFS-survival at 1-year = 72.2% versus 61.1%, %PFS-survival at 2-years = 60.0% versus 61.1%, p = 0.72; %OS-survival at 1-year = 69.0% versus 69.3%, %OS-survival at 2-years = 56.6% versus 49.5%, p = 0.90. Craniotomy resulted in higher rates of pre-operative deficit improvement than LITT (p < 0.01). On subgroup analysis, the single factor most significantly associated with OS and PFS was pathology of the lesion. About 40% of tumor lesions needed post-operative salvage with radiation after both craniotomy and LITT.
Conclusions
LITT was as efficacious as craniotomy in achieving local control of recurrent irradiated brain metastases and facilitating steroid taper, regardless of pathology. Craniotomy appears to be more advantageous for providing symptom relief in those with pre-operative symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stereotactic radiosurgery (SRS) is now being used as first line treatment for oligometastatic brain metastases and is becoming increasingly commonplace as focal treatment of multiple brain metastases, with acceptable rates of response and morbidity. Despite its success, it is now known that in 5–15% of patients with longer survival, regrowth of tumor or development of lesion regrowth devoid of tumor cells, considered adverse radiation effect but more commonly termed radiation necrosis, can occur. In both scenarios, for those lesions that are easily surgically amenable, craniotomy for surgical resection allows for (1) accurate differential diagnosis between tumor and radiation necrosis and (2) removal of the offending lesion aiding in rapid resolution of perilesional edema, local mass effect and any associated neurological symptoms. For patients with more deep-seated lesions where surgical management complications may lead to further decline in neurological function, or in patients in whom craniotomy is not an acceptable option, few good alternative treatments have been available.
MRI-guided laser interstitial thermotherapy (LITT) is an emerging procedure which can achieve both pathological diagnosis and ablative therapy. Its use has been reported particularly for those lesions that are sub-optimal for conventional surgical resection due to lesion location. With its increasing availability, however, the choice of using LITT for treatment of these lesions rather than craniotomy has also become an issue of patient preference. Previous studies by multiple groups, including those at our institution, have demonstrated the safety and efficacy of LITT [1,2,3,4,5]. Recently, a multicenter retrospective study encompassing 30 patients across four centers by Chaunzwa et al. [6] demonstrated relatively low complication rates, short hospitalization stays, and effective reduction of perilesional edema in the majority of LITT-treated patients [6]. However, to date there are no studies that have compared the efficacy of LITT to standard surgical resection or analyzed the factors that make one approach more favorable over the other. To address this question, we performed a single institution retrospective review of patients who were previously treated with SRS for brain metastases and subsequently underwent either LITT or surgical resection for SRS-treated lesion regrowth.
Methods
Patient selection
Institutional review board approval was obtained to retrospectively review the clinical information for all patients who underwent craniotomies or LITT procedures for brain metastases after failing SRS between 2007 and 2016 at Yale University. Lesional regrowth was defined as an increase in 20% in any single dimension of the lesion as defined by RECIST criteria. Lesion volume was measured utilizing the ABC/2 formula measuring greatest dimensions in the axial, coronal, and sagittal planes. In all cases of LITT, stereotactic brain biopsy was obtained prior to the laser thermal ablation. Final pathological diagnosis was determined based on review of samples by neuro-pathologists. Lesions considered to be radiation necrosis demonstrated no viable tumor cells after histological analysis. Samples comprised of a mixture of necrosis and viable tumor cells were classified as recurrent tumor in this study. The electronic medical records of the included patients were retrospectively reviewed for demographic data, clinical outcomes including survival measures, and all records of medical, radiation, and surgical treatments prior to and after LITT or craniotomy. The decision to pursue craniotomy versus LITT was based upon surgeon judgment and patient preference on a case-by-case basis, the details of which are discussed later.
Surgical technique and management
All LITT procedures were performed in an intraoperative 3.0T MR scanner (IMRIS, Mannitoba, Canada) using the NeuroBlate laser system produced by Monteris Medical Inc. (Minnesota, USA), as well as navigation guidance with the ClearPoint system produced by MRI Interventions Inc. (California, USA). Each LITT procedure was carried out in standard fashion, as previously described in our earlier studies [1, 6].
Post-operative management
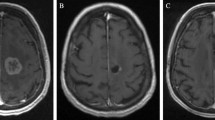
Follow-up MRIs and clinical outpatient visits typically occurred at 1, 3, and 6 months after surgery. Failure of the surgical procedure was defined as regrowth of the ablated or resected lesion on T1-weighted post-contrast MRI with associated increased surrounding fluid-attenuated inversion-recovery (FLAIR), regardless of whether there was symptom recurrence.
Results
Patient demographics and clinical features
Seventy-five patients were included in this study with a mean age at time of surgery of 60.2 ± 11.2 years. Gender breakdown was 41 females (54.7%) and 34 males (45.3%). Among the 75 patients, 41 underwent craniotomy and 34 underwent LITT. Subjects were further sub-divided into one of four cohorts based on treatment modality and final pathology. Of the 41 treated with craniotomy, 15 patients had radiation necrosis and 26 had recurrent tumor. Among the 34 treated with LITT, 18 patients had radiation necrosis and 16 had recurrent tumor. There were no statistically significant differences in gender or age at time of surgery among the four cohorts (Table 1).
The most common primary pathology was lung cancer (33/75, 44%) followed by melanoma (27/75, 36%) and breast cancer (7/75, 9.3%). The remaining cases were comprised of embryonal germ cell tumor (n = 2), bladder cancer (n = 1), renal cell cancer (n = 1), mesothelioma (n = 1) and colorectal cancer (n = 3). The lesions were located in the frontal lobe (n = 34), parietal lobe (n = 11), temporal lobe (n = 10), occipital lobe (n = 10), cerebellum (n = 8), thalamus (n = 1), and basal ganglia (n = 1). The mean volume of the target lesions was 6.29 cm3 and was significantly larger for the craniotomy group versus the LITT group (8.1 versus 4.1 cm3, p = 0.02). The mean dose of radiation delivered to the lesion margin was 20.4 Gy (range 16 to 30 Gy) and was similar across all cohorts (p > 0.99) (Table 2).
At the time of surgery, 46 (61.3%) patients had active/progressive systemic disease while 29 (38.7%) patients had controlled systemic disease (N.S. across cohorts). Among the 41 patients treated with craniotomy, 23 (56.1%) had active/progressive systemic disease, while 18 (43.9%) had controlled systemic disease. In the 34 patients who underwent LITT, 23 (67.6%) had active/progressive systemic disease, while 11 (32.4%) had controlled systemic disease (Table 1). Of the 75 lesions, 15 had previously been treated with WBRT (20.0%) and 9 had been previously treated with SRS (12.0%) to the same lesion. Among the 15 previously treated with WBRT, 6 (40.0%) had recurrent tumor, and 9 (60.0%) had radiation necrosis, while among the 9 previously treated with SRS, 6 (66.6%) had recurrent tumor, and 3 (33.3%) had radiation necrosis (Table 1). Five patients had previously had craniotomy for their lesion before undergoing SRS and subsequently were included in our study via repeat craniotomy (n = 1) or LITT (n = 4). The average time from SRS to surgery was 1.14 years among all patients and was significantly longer in patients who harbored radiation necrosis (1.5 years) versus recurrent tumor (0.85 years) (p < 0.01).
Reasons for choosing LITT over craniotomy were: patient preference when both craniotomy and LITT offered (n = 21), concern for greater risk of additional neurological morbidity with surgical approach in deep seated lesions (n = 9), primary intent of surgery was to obtain tissue diagnosis in asymptomatic patient and therefore minimally invasive procedure preferred (n = 2), not a suitable open surgical candidate due to wound healing issues (n = 1), and smaller incision thought to limit time off from systemic therapy (n = 1).
Clinical outcomes
The mean length of hospital stay after LITT was 3.1 days, compared to 3.9 days for craniotomy (p = 0.03). The mean duration of the surgical procedure including anesthesia induction and extubation was 7.6 h for LITT, significantly longer than 4.5 h for craniotomy (p < 0.001) (Table 3). All lesions treated via craniotomy achieved gross total resection or near total resection (> 90% radiographic removal of the targeted lesion). Likewise, all lesions treated with LITT were ablated to encompass 100% of the targeted tumor volume using standard computing software from Monteris Medical Inc.
At time of surgery, 23 patients were asymptomatic while the remaining 52 patients were symptomatic. Chief complaints included: headaches (n = 17), seizures (n = 14), motor deficits (n = 11), dysphasia (n = 5), visual deficits (n = 3), and sensory changes (n = 2). There were no significant differences between LITT (23/34, 67.6%) versus craniotomy (29/41, 70.7%) groups in prevalence of pre-operative symptomatology (p = 0.81). Degree of post-operative symptom relief was further analyzed based on lesion size and treatment modality. Among the 34 lesions treated with LITT, 20 (58.8%) were < 2 cm in greatest dimension, 11 (32.4%) were 2–3 cm, and 3 (8.8%) were > 3 cm while among the 41 lesions treated with craniotomy, 12 (29.3%) were < 2 cm, 18 (43.9%) were 2–3 cm, and 11 (26.8%) were > 3 cm. As expected, percentage of symptomatic patients increased with lesion size − 17/32 patients (53%) for lesions < 2 cm, 22/29 (76%) for 2–3cm lesions, and (13/14) 93% for lesions > 3 cm.
Improvement (complete or partial) in symptoms was seen in 87% (20/23) of LITT patients and 90% (26/29) craniotomy patients. Complete resolution of pre-operative symptoms, however, was reported in 21/29 (72.4%) of those treated with craniotomy compared with 6/23 (26.1%) treated with LITT (p < 0.01). Symptoms that significantly improved included headaches (n = 13), seizures (n = 7), motor deficits (n = 3), dyphasia (n = 2), visual deficits (n = 1), and sensory changes (n = 1). Partial improvement in pre-operative symptoms were seen in 5/29 (17.2%) in the craniotomy group and in 14/23 (60.9%) in the LITT group (p < 0.01). These symptoms included motor deficits (n = 7), seizures (n = 6), dysphasia (n = 3), headache (n = 1), visual deficits (n = 1), and sensory change (n = 1). These data are summarized in Supplementary Table 1.
Prior to surgery, 19 patients (46%) in the craniotomy group required steroids for symptom control, compared to 23 patients (68%) in the LITT group. At 1-month follow-up, despite a significant difference in the amount of symptom reduction between the two groups, an equivalent 9/19 (47.4%) patients in the craniotomy group and 8/23 (34.8%) in the LITT group had been able to be weaned off steroids (p = 0.53) (Table 3).
There were no significant differences in the rate of peri-operative complications (within 30 days of surgery) between the LITT (12/34, 35.3%) and craniotomy (10/41, 24.4%) groups (p = 0.32). In the craniotomy group, complications included worsened visual deficits (n = 2), motor weakness (n = 3), seizures (n = 2), dysphasia (n = 2) and hyperglycemia (n = 1). For the LITT group, complications included motor weakness (n = 3), hyperglycemia (n = 2), thrombocytopenia (n = 1), deep venous thrombosis (n = 1), dysphasia (n = 1), visual disturbance (n = 2), and seizure (n = 2) (Table 3).
As expected, post-operatively, patients harboring recurrent tumor pathology underwent additional radiation, at significantly higher rates (17/42; 40.5%) compared to those with radiation necrosis (1/33; 3.0%) (p < 0.003). There were no significant differences in rates of post-operative radiation for patients with recurrent tumor between those treated with LITT, 6/16 (37.5%) versus those who underwent craniotomy, 11/26 (42.3%) (p > 0.99). In patients who had radiation necrosis, there were likewise no significant differences in rates of post-operative bevacizumab therapy between those treated with LITT, 7/18 (38.9%), compared to those treated with craniotomy, 3/15 (20%) (p = 0.28) (Table 2).
Local control and survival outcomes
Local progression free survival (PFS) was measured as the length of time from surgery to the radiographic evidence of local progression and/or recurrence. In the craniotomy group, PFS rates were 70.5% at 6 months and remained 61.1% at 12, 18, and 24 months. In the LITT group, PFS rates were not significantly different and were 75.6% at 6 months, 72.2% at 12 months, 66.6% at 18 months, and 60.0% at 24 months (p = 0.722) (Fig. 1a). When analyzed for final pathology, PFS for patients with radiation necrosis was significantly longer than those with recurrent tumor: 87.4% at 6, 12, and 18 months and 81.5% at 24 months compared to 61.5% at 6 months, 48.8% at 12 months, and 44.7% at 18 and 24 months, respectively (p < 0.01) (Fig. 1b). Among patients treated for radiation necrosis, PFS was similar between those undergoing craniotomy (86.7% at 6, 12, 18, and 24 months) and those who had LITT (87.8% at 6, 12, and 18 and 73.2% at 24 months) (p = 0.68). Likewise, in patients who had recurrent tumor, PFS for craniotomy (61.0% at 6, 44.4% at 12, 18, and 24 months) was similar to LITT (62.5% at 6, 54.7% at 12, 43.8% at 18 and 24 months) (p = 0.99) (Fig. 1c).
Kaplan–Meier survival curves comparing progression-free survival for patients grouped by a treatment modality—LITT versus craniotomy, b lesion pathology—radiation necrosis versus tumor, and c subgroup analysis—LITT for radiation necrosis, LITT for tumor, craniotomy for radiation necrosis, craniotomy for tumor. Kaplan–Meier survival curves comparing overall survival for patients grouped by d treatment modality—LITT versus craniotomy, e lesion pathology—radiation necrosis versus tumor, and f subgroup analysis—LITT for radiation necrosis, LITT for tumor, craniotomy for radiation necrosis, craniotomy for tumor
Overall survival (OS) was measured as length of time from surgery to time of death from any cause. In the craniotomy group, OS rates were 92.7% at 6 months, 69.3% at 12 months, 52.4% at 18 months, and 49.5% at 24 months, which was not significantly different from the LITT group with OS rates of 79.4% at 6 months, 69.0% at 12 months, 65.3% at 18 months, and 56.6% at 24 months (p = 0.904) (Fig. 1d). Like PFS, OS was significantly greater for patients with radiation necrosis versus those with tumor regrowth (97.0% at 6 months, 83.5% at 12 months, 72.1% at 18 months, and 63.3% at 24 months versus 78.6% at 6 months, 57.5% at 12 months, 46.4% at 18 months, and 43.5% at 24 months, respectively) (p < 0.01) (Fig. 1e). When analyzed by cohort, differences in OS trended towards but did not achieve statistical significance (p = 0.071). Overall survival for patients undergoing craniotomy for radiation necrosis was 100% at 6 months, 93.3% at 12 months, 71.8% at 18 months, and 64.6% at 24 months, those undergoing LITT for radiation necrosis was 94.4% at 6 months, 73.8% at 12 and 18 months, and 63.2% at 24 months, craniotomy for tumor was 88.5% at 6 months, 54.3% at 12 months, 40.2% at 18 and 24 months, and LITT for tumor was 62.5% at 6 and 12 months, 55.6% at 18 months, and 48.6% at 24 months (Fig. 1f). Survival outcomes were also analyzed based on cancer type, grouped into melanoma, NSCLC, breast, and other. There were no significant differences in PFS (p = 0.0735) or OS (p = 0.437) across all the cancer types together. Within melanoma and NSCLC, for which there were enough samples to analyze for statistical significance, there were no differences in PFS when comparing LITT versus craniotomy (p = 0.431 and p = 0.193, respectively). Interestingly, however, it was noted that patients with melanoma (88.7% at 6 months, 83.8% at 12 months, 78.6% at 18 and 24 months) demonstrated significantly longer PFS rates than those with NSCLC (60.0% at 6 months, 56.7% at 12, 18, and 24 months) or breast cancer (80.0% at 6 months, 53.3% at 12 and 18 months, and 26.7% at 24 months) (p = 0.0434). This was not dependent upon RN pathology, as there were no significant differences in prevalence of RN between patients with melanoma (14/27, 51.9%), NSCLC (12/33, 36.4%), breast cancer (4/7, 57.1%), or other cancers grouped as a whole (3/8, 37.5%) (p = 0.55). On sub-analysis of melanoma patients, patients who underwent craniotomy had significantly higher rates of radiographically decreased or resolved peri-lesional edema at 1-month follow-up (10/16, 62.5%) compared to those treated with LITT (1/11, 9.1%) (p < 0.01). However, there were no significant differences in rates of steroid cessation at 1-month follow-up between the two treatment modalities (craniotomy: 13/16, 81.3% versus LITT: 9/11, 81.8%; p > 0.99). Likewise, there were no differences between craniotomy and LITT in the ability to initiate or resume immunotherapy post-operatively (craniotomy: 10/16, 62.5% versus LITT: 8/11, 72.7%; p = 0.69).
To eliminate part of the size bias in our cohort, namely that lesions over 3 cm in diameter were more likely to undergo craniotomy than LITT, outcomes were further analyzed for only lesions that were less than or equal to 3 cm in diameter. This group was comprised of 31 patients who underwent LITT (16 for RN, 15 for recurrent tumor) and 30 patients treated with craniotomy (14 for RN, 16 for recurrent tumor). Again, there were no significant differences in PFS in patients who underwent LITT (80.6% at 6 months, 77.0% at 12 months, 69.3% at 18 and 24 months) versus craniotomy (76.7% at 6 months, 73.2% at 12 months, 69.7% at 18 months, and 65.6% at 24 months) (p = 0.92) (Fig. 2a). OS likewise did not different between LITT (83.9% at 6 months, 77.4% at 12 and 18 months, and 73.3% at 24 months) and craniotomy (100% at 6 months, 90.0% at 12 months, 80.0% at 18 months, and 66.7% at 24 months) (p = 0.81) (Fig. 2b). Among patients treated for radiation necrosis, PFS was similar between those undergoing craniotomy (85.7% at 6, 12, 18, and 24 months) and those who had LITT (86.2% at 6, 12, and 18 and 71.8% at 24 months) (p = 0.67) (Fig. 2c). Likewise, in patients who had recurrent tumor, PFS for craniotomy (55.6% at 6, 47.6% at 12, 18, and 24 months) was similar to LITT (51.4% at 6 and 12 months, 38.6% at 18 and 24 months) (p = 0.82) (Fig. 2d). As expected, PFS and OS were significantly greater for patients with radiation necrosis versus those with tumor regrowth (PFS: 86.0% at 6, 12, and 18 months, and 79.9% at 24 months versus 53.6% at 6 months, 49.5% at 12 months, 44.0% at 18 and 24 months, respectively; p < 0.01) (Fig. 2e) (OS: 96.7% at 6 months, 89.1% at 12 months, 76.3% at 18 months, and 71.5% at 24 months versus 74.1% at 6 months, 50.5% at 12 months, 40.1% at 18 months, and 36.5% at 24 months, respectively; p < 0.01) (Fig. 2f).
Kaplan–Meier survival curves for lesions < 3 cm in diameter comparing a progression-free survival and b overall survival grouped by treatment modality—LITT versus craniotomy, comparing c progression-free survival and d overall survival based on subgroup analysis—LITT for radiation necrosis, LITT for tumor, craniotomy for radiation necrosis, craniotomy for tumor, and comparing e progression-free survival and f overall survival based on lesion pathology—radiation necrosis versus tumor
Discussion
Laser thermocoagulation for brain tumor treatment was first explored by Sugiyama et al. in animal models and small cohort of patients using a computed tomography-stereotactic technique [7] and subsequently recapitulated by various other groups in the 1990s for treatment of both primary and metastatic brain tumors [8,9,10]. Initially hindered by a lack of ability to accurately and precisely monitor heat delivery to targeted tissues, the advent of MRI-guided thermometry, based on changes in gradient echo MR signal, has allowed for real-time monitoring of tissue temperature. In addition, the availability of an intraoperative MRI within the operating room has facilitated pre-thermocoagulation biopsy of the tissue followed by stereotactic placement of the laser fiber and subsequent adjustment and repositioning of the fiber tip with MRI confirmation making laser treatment more controllable. We first described our experience utilizing these practices in a case series of six patients undergoing LITT for treatment of radiographically regrowing deep lesions following SRS [1]. Subsequently, we along with other institutions recently reported a multicenter retrospective study of MRI-guided LITT for brain metastases failing SRS and recapitulated this technology as a safe and viable alternative to traditional treatment options in this patient population [6]. As one of the first centers in the United States to adopt LITT, the cases performed during the first few years of development of the technology were fraught with software challenges provided by the combination of use of a new intra-operative MRI system, the evolving Monteris NeuroBlate system and the development of the adaptation of the Clearpoint navigation system for use in tumors rather than functional cases. As such, the increased operating times for LITT reported here, compared to the current literature [11, 12], reflects these challenges and a learning curve both for the surgeon as well as involved assistants and staff. As the number of centers with intraoperative MRI technology grows around the country, further reports detailing outcomes after MRI-guided LITT are expected to emerge and guide future applications of this technology. Likewise, there is an ongoing multicenter prospective observational cohort study registered as a clinical trial (NCT02392078), analyzing outcomes after laser thermocoagulation for both primary and metastatic brain tumors.
Ever since the landmark study by Patchell et al. [13] demonstrating that surgical resection plus radiation resulted in reduced rates of local recurrence, improved functional outcomes, and increased overall survival, compared to radiation alone [13], surgical resection has become part of the standard options for treatment for patients with a symptomatic isolated lesion or oligometastases both at initial presentation as well as at time of salvage. Likewise, LITT has grown in its application towards a variety of pathologies, including primary and metastatic brain tumors, radiation necrosis, and epilepsy among others [2,3,4,5, 14]. However, our study remains the first to compare outcomes between surgical resection and LITT for recurrent tumor or radiation necrosis after radiosurgery, and we found similar efficacy between the two treatment modalities.
This study shows that both progression free survival and overall survival in our patient cohort were determined more by pathology than surgical treatment tool used. Similarly, ability to wean off steroids was not significantly different between craniotomy and LITT. However, our data shows that craniotomy may be more effective than LITT in symptom relief as a greater portion of patients treated with craniotomy experienced significant improvement of their preoperative deficits compared to those treated with LITT with no difference in complication rates between the two procedures. Although we found that the majority of symptomatic patients who underwent LITT still experienced mild improvement of their preoperative deficits, craniotomy may be the more effective treatment modality in patients for whom symptom relief is the primary aim of operative intervention. In addition, a minority (23/75, 30.7%) of the lesions treated in this study was in asymptomatic patients, most measuring < 3 cm in size, and were equally distributed among the LITT (n = 11) and craniotomy (n = 12) groups (Supplementary Table 1). Although there was no single guiding paradigm in the decision to treat these patients, these lesions were generally observed to be increasing in size with serial surveillance MRI, and a tissue diagnosis was needed in order to guide future systemic therapy. In particular, over half of the asymptomatic patients were comprised of melanoma patients (13/23, 56.5%) who were either undergoing or were in consideration for immunotherapy and were not on steroids at the time. As such, tissue diagnosis of the regrowing lesion was needed, given a presumed diagnosis of radiation necrosis would have necessitated cessation of immunotherapy and initiation of steroid therapy.
As discussed by the recent multicenter study by Chaunzwa et al., a common indication for use of LITT in a lesion regrowing after radiosurgery was steroid resistance. An inability to come off steroids after radiosurgery brings about a multitude of medical complications including infections, hypertension, hyperglycemia, weight gain, poor wound healing, and gastrointestinal ulcers and, for cancers like melanoma and increasingly for lung cancer, an inability to be treated using immunotherapy. In the current study, we found that almost half of all patients had been successfully weaned off steroids within 1 month after their procedure with no significant differences existing between the LITT and craniotomy groups despite differences in pre-treatment lesion size or completeness of symptom relief post-treatment. These findings suggest that the ability to wean off steroids may be affected by factors other than symptoms. Examples of this could include scenarios such as (1) patients with headaches that are not necessarily caused by the LITT lesion who feel better on steroids, (2) patients with overall appetite improvement on steroids or (3) patients and/or physicians who feel uncomfortable weaning steroids given lack of change in FLAIR signal lesion size on MRI regardless of symptomatology. Lastly, we further sub-analyzed melanoma patients in our cohort to investigate whether treatment modality may affect adjuvant immunotherapy in the post-operative period. Despite lesions treated with LITT demonstrating significantly lower rates of post-operative edema resolution or reduction, this did not impact the ability to wean steroids off by 1-month follow-up compared to those treated with craniotomy. Likewise, treatment modality did not seem to affect the ability to initiate or resume immunotherapy in the post-operative period. Together, our data suggest that LITT may be as effective as craniotomy in perioperative steroid cessation and facilitation of immunotherapy shortly after operative intervention.
Six-month PFS rates for LITT (75.6%) and craniotomy (70.5%) demonstrated by this study are similar to the reported 75.8% by Rao et al. in their study of 16 patients undergoing LITT for recurrent lesions after SRS for brain metastasis [3]. While these rates are diminished compared to the overall 92.9% local control rate reported in our recent multicentered retrospective study [6], this likely reflects differences in prevalence of radiation necrosis pathology in our previous study (19/24 lesions, 79%) compared to the current study (33/75 lesions, 44%) since PFS for those with RN was significantly longer than those with recurrent tumor, regardless of treatment modality (87.4% versus 61.5% at 6-months, respectively.
This study has a number of limitations, related to the retrospective nature of the data. We acknowledge that the heterogeneity of treatments administered prior to and after surgical intervention for the previously irradiated brain metastasis makes conclusions regarding the effects of craniotomy versus LITT difficult in assessing impact on survival outcomes, particularly overall survival. Furthermore, we recognize that a biopsy, particularly in LITT cases, is limited by sampling of only a small part of the regrowing lesion and thus, those cases considered radiation necrosis in our cohort may be over-represented and would have constituted recurrent tumor had further parts of the lesion been histopathologically analyzed. As such, the outcomes of patients in our radiation necrosis cohort may be under-estimated. Although additional pre-operative modalities, such as MR perfusion, are routinely utilized at our institution, these factors did not impact the decision to classify a regrowing lesion as recurrent tumor versus radiation necrosis in this study. However, we did analyze rates of postoperative adjuvant therapy in our patients and did not find significant differences between the craniotomy and LITT cohorts, further strengthening our conclusions of equal efficacy in local control with either treatment modality. We also acknowledge that the lesions treated with craniotomy tended to be significantly larger in volume than those with LITT (8.1 versus 4.1 cm3, p = 0.02). These measured volumes may have been further limited by the relative inaccuracies of the ABC/2 method, but further methods were deferred given the heterogeneity of imaging techniques in our patient cohort, often comprised of scans from outside institutions. Of the 34 lesions treated with LITT, only 5 (14.7%) were larger than the mean volume of the lesions treated with craniotomy with the largest lesion treated with LITT measuring 14.9 cm3. The smaller size of the lesions treated with LITT likely reflects surgeon bias in treatment modality preference, and it remains to be seen whether comparably sized lesions treated with LITT demonstrate comparable outcome measures to those resected via craniotomy. Our sub-analysis of outcomes for both PFS and OS in tumors with diameters under 3 cm did not demonstrate any significant differences between treatment modalities. A randomized study would be needed to ensure valid direct comparison.
The results of this study continue to endorse LITT as a viable alternative to standard of care craniotomy in patients with brain metastases regrowing after SRS treatment. Based on this study, craniotomy should continue to be considered for surgically easily-accessible lesions in patients for whom symptom relief remains a priority with operative intervention. Likewise, craniotomy should also remain an option for local disease control in those with a strong preoperative suspicion for radiation necrosis. In cases of recurrent tumor however, LITT should be considered as one of the first line options in asymptomatic patients given the equal opportunity to come off steroids with shorter hospitalization and recovery times without significant difference in PFS, OS or complication rates. Given the small, retrospective and single institution nature of this study, however, our findings need to be confirmed with further multicenter studies.
Our single institution retrospective analysis of craniotomy versus LITT for regrowing lesions in previously irradiated brain metastases showed comparable results between the two modalities. Specifically, LITT appears to be as efficacious as craniotomy in achieving desirable functional outcomes, the ability to wean off steroids, and for local control of brain metastases regrowing tumor after radiosurgery with similar overall survival and local control rates. Further prospective studies are needed to confirm these findings and to help determine if overall survival is improved by craniotomy in those with radiation necrosis.
References
Torres-Reveron J, Tomasiewicz HC, Shetty A, Amankulor NM, Chiang VL (2013) Stereotactic laser induced thermotherapy (LITT): a novel treatment for brain lesions regrowing after radiosurgery. J Neurooncol 113:495–503. https://doi.org/10.1007/s11060-013-1142-2
Sloan AE, Ahluwalia MS, Valerio-Pascua J, Manjila S, Torchia MG, Jones SE, Sunshine JL, Phillips M, Griswold MA, Clampitt M, Brewer C, Jochum J, McGraw MV, Diorio D, Ditz G, Barnett GH (2013) Results of the NeuroBlate System first-in-humans Phase I clinical trial for recurrent glioblastoma: clinical article. J Neurosurg 118:1202–1219. https://doi.org/10.3171/2013.1.JNS1291
Rao MS, Hargreaves EL, Khan AJ, Haffty BG, Danish SF (2014) Magnetic resonance-guided laser ablation improves local control for postradiosurgery recurrence and/or radiation necrosis. Neurosurgery 74:658–667. https://doi.org/10.1227/NEU.0000000000000332 discussion 667
Kang JY, Wu C, Tracy J, Lorenzo M, Evans J, Nei M, Skidmore C, Mintzer S, Sharan AD, Sperling MR (2016) Laser interstitial thermal therapy for medically intractable mesial temporal lobe epilepsy. Epilepsia 57:325–334. https://doi.org/10.1111/epi.13284
Carpentier A, McNichols RJ, Stafford RJ, Guichard JP, Reizine D, Delaloge S, Vicaut E, Payen D, Gowda A, George B (2011) Laser thermal therapy: real-time MRI-guided and computer-controlled procedures for metastatic brain tumors. Lasers Surg Med 43:943–950. https://doi.org/10.1002/lsm.21138
Chaunzwa TL, Deng D, Leuthardt EC, Tatter SB, Mohammadi AM, Barnett GH, Chiang VL (2018) Laser thermal ablation for metastases failing radiosurgery: a multicentered retrospective study. Neurosurgery 82:56–63. https://doi.org/10.1093/neuros/nyx142
Sugiyama K, Sakai T, Fujishima I, Ryu H, Uemura K, Yokoyama T (1990) Stereotactic interstitial laser-hyperthermia using Nd-YAG laser. Stereotact Funct Neurosurg 54–55:501–505. https://doi.org/10.1159/000100263
Feyh J, Gutmann R, Leunig A, Jager L, Reiser M, Saxton RE, Castro DJ, Kastenbauer E (1996) MRI-guided laser interstitial thermal therapy (LITT) of head and neck tumors: progress with a new method. J Clin Laser Med Surg 14:361–366. https://doi.org/10.1089/clm.1996.14.361
Menovsky T, Beek JF, van Gemert MJ, Roux FX, Bown SG (1996) Interstitial laser thermotherapy in neurosurgery: a review. Acta Neurochir (Wien) 138:1019–1026
Hata N, Morrison PR, Kettenbach J, Black PM, Kikinis R, Jolesz FA (1998) Computer-assisted intra-operative magnetic resonance imaging monitoring of interstitial laser therapy in the brain: a case report. J Biomed Opt 3:304–311. https://doi.org/10.1117/1.429857
Patel P, Patel NV, Danish SF (2016) Intracranial MR-guided laser-induced thermal therapy: single-center experience with the Visualase thermal therapy system. J Neurosurg 125:853–860. https://doi.org/10.3171/2015.7.JNS15244
Salehi A, Kamath AA, Leuthardt EC, Kim AH (2018) Management of intracranial metastatic disease with laser interstitial thermal therapy. Front Oncol 8:499. https://doi.org/10.3389/fonc.2018.00499
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322:494–500. https://doi.org/10.1056/NEJM199002223220802
Norred SE, Johnson JA (2014) Magnetic resonance-guided laser induced thermal therapy for glioblastoma multiforme: a review. Biomed Res Int 2014:761312 https://doi.org/10.1155/2014/761312
Funding
The authors have no sources of funding to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The senior author of this paper (VC) is a consultant for Monteris Medical Inc. (Minnesota, USA.) No other authors have any conflicts of interest to disclose.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hong, C.S., Deng, D., Vera, A. et al. Laser-interstitial thermal therapy compared to craniotomy for treatment of radiation necrosis or recurrent tumor in brain metastases failing radiosurgery. J Neurooncol 142, 309–317 (2019). https://doi.org/10.1007/s11060-019-03097-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03097-z