Abstract
This study aims to evaluate the cost-effectiveness of surgical resection (S) and Cesium-131 (Cs-131) [S + Cs-131] intraoperative brachytherapy versus S and stereotactic radiosurgery (SRS) [S + SRS] for the treatment of brain metastases. Treatment records as well as hospital and outpatient charts of 49 patients with brain metastases between 2008 and 2012 who underwent S + Cs-131 (n = 24) and S + SRS (n = 25) were retrospectively reviewed. Hospital charges were compared for the single treatment in question. Means and curves of survival time were defined by the Kaplan–Meier estimator, with the cost analysis focusing on the time period of the relevant treatment. Quality adjusted life years (QALY) and Incremental cost-effectiveness ratios (ICER) were calculated for each treatment option as a measure of cost-effectiveness. The direct hospital costs of treatments per patient were: S + Cs131 = $19,271 and S + SRS = $44,219. The median survival times of S + Cs-131 and S + SRS were 15.5 and 11.3 months, and the 12 month survival rates were 61 % and 49 % (P = 0.137). The QALY for S + SRS when compared to S + Cs-131 yielded a p < 0.0001, making it significantly more cost-effective. The ICER also revealed that when compared to S + Cs-131, S + SRS was significantly inferior (p < 0.0001). S + Cs-131 is more cost-effective compared with S + SRS based on hospital charges as well as QALYs and ICER. Cost effectiveness, in addition to efficacy and risk, should factor into the comparison between these two treatment modalities for patients with surgically resectable brain metastases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain metastases are the most common form of intracranial neoplasm [1, 2], occurring in 20–40 % of patients with cancer and with an increasing incidence [3–5]. Brain metastases are often associated with poor prognosis and the natural history and survival of treatment with steroids alone has been shown to be 1–2 months [6]. Whole brain radiotherapy (WBRT) treatment techniques increase survival to 3–6 months [7–9]. Surgical resection (S) of brain metastases in addition to WBRT has been shown to extend survival to 11 months [10, 11]. However, due to the increased risk of neurocognitive decline associated with WBRT [12–15] attention has shifted to focal post-operative treatment options.
Recent innovations in radiotherapy have introduced partial and focused forms of radiation techniques such as stereotactic radiosurgery (SRS) as another treatment option to a patient with a limited number of lesions [12, 16–21] or as a boost to WBRT [22–25]. The reported mean survival following SRS alone varies depending on RPA class [19] but frequently ranges between 8 and 10 months [16, 18]. The local control of the resection cavity is reported to be similar to post-operative WBRT, ranging from 70 to 100 % [26]. However, SRS in the post-operative setting has certain limitations in its application for the treatment of brain metastases. A delay of several weeks between surgery and irradiation can lead to repopulation of cancer cells during the waiting period [27]. Moreover, SRS is not an optimal treatment option for large (>3 cm) or non-round (irregularly shaped) surgical cavities, which have been shown to be associated with inferior local control compared with smaller lesions [28–30]. Therefore, other treatment modalities such as intraoperative brachytherapy have been investigated, which offers immediate therapy before cellular repopulation begins and targets large, irregular cavities as well as small round ones [31]. Initial studies using iodine-125 (I-125) brachytherapy reported favorable local control and median survival rates [32, 33]. However, the use of I-125 has also been associated with high rates of radiation necrosis (up to 26 %) [32, 33].
Cs-131, an FDA cleared isotope, presents an excellent alternative. Its t1/2 is only 9.7 days, delivering the majority of the intended dose within 1 month. Wernicke et al. recently reported excellent outcomes with low rates of radiation necrosis in a Phase II trial intraoperative Cs-131 brachytherapy [31]. However, the cost effectiveness of intraoperative brachytherapy has not yet been studied in comparison with post-resection SRS. Comprehensive comparison of these two treatment modalities requires consideration of cost as well as for efficacy and risk. In this study we focus on the cost of these two competing therapies to a single brain metastasis. The costs of additional treatments to additional synchronous or metachronous local or distant metastases were eliminated from consideration so as not to bias the results.
Materials and methods
Patients
With the IRB-approval, treatment records and the hospital and out-patient receipts of 49 patients with brain metastases were retrospectively reviewed at New York Presbyterian/Weill Cornell Medical Center between 2008 and 2012. Treatments included S + Cs-131 (n = 24) and S + SRS (n = 25). Our institution began using intracavitary Cs-131 inpatients who required surgery to a brain metastasis for diagnosis or relief of mass effect. Patients that chose not to go on the Cs-131 trial, or who needed surgery before the Cs-131 could be ordered to the hospital were treated with S + SRS. Moreover, patients treated from 2008 to 2010 before Cs-131 was utilized and who received S + SRS were also included in this study. Additional synchronous or metachronous distant metastases were treated with SRS, although the cost of this additional treatment was not included in this study since not all patients had the same number of additional metastases.
Treatment techniques
Surgery
Patients underwent resection of lesions for which surgery was clinically indicated i.e. relief of mass effect, need for tissue diagnosis, size >3 cm, single easily accessible lesion. The extent of resection was noted from post-operative MRI scans performed within 48 h of surgery and read by a neuro-radiologist.
Intraoperative Cs-131 brachytherapy
At the time of resection, Cs-131 stranded seeds (IsoRay, Richland, WA) with an activity of 3–5 mCi were implanted with a planned dose of 80 Gy to a 5 mm depth from the surface of the resection cavity. The implant was pre-calculated based on pre-operative data of tumor size and our institutional physics nomogram and adjusted real time for the resulting intracavitary volume of the resected metastasis. The 10 cm Cs-131 suture-stranded seeds (0.5 cm inter-seed spacing) were delivered in strings of 10 seeds per string and subsequently cut into smaller lengths as per the nomogram and placed as a permanent volume implant along the cavity in a tangential pattern to maintain a 7–10 mm spacing between strings. The seeds are then covered with surgicel (Ethicon) to prevent seed migration and alteration of dosimetry and tisseel (Baxter) is used to line the cavity to limit cavity shrinkage and further prevent seed dislodgement.
Stereotactic radiosurgery (SRS)
For the SRS, the planning target volume (PTV) included the GTV plus 2–3 mm margins, to account for patient setup and target motion uncertainty. Since 2010, 2 mm margins were made standard to account for uncertainty in resection cavity delineation. The prescribed dose was used to RTOG protocol 90-05 [34]. Treatment was delivered with either intensity-modulated static fields (IMRS), volumetric modulated arc therapy (VMAT) or dynamic conformal arcs (DCA). IMRS or VMAT was prescribed so that at least 95 % of the PTV received at least 100 % of the prescribed dose, and DCA therapy was prescribed at the 80 % isodose line. Patients uniformly were treated with a frameless radiosurgery technique using the Novalis TxTM linear accelerators (Varian Medical Systems, Palo Alto, CA). Cone beam CT (CBCT) scans with six of freedom registration allowed for precise positioning prior to treatment [35, 36].
Imaging examinations and follow-up
Regular follow-up was performed in the outpatient setting. Follow-up exams consisted of MRI scans and physical evaluation every 2 months. MRI exams were performed utilizing the following sequences: T1-weighted, FLAIR, T2-weighted, GRE and diffusion weighted imaging. Also, post-contrast gadolinium enhanced T1-weighted images were obtained in axial, sagittal and coronal planes with 3 mm slice thickness. Additionally, patients were assessed clinically with physical examination every 2 months with specific attention drawn to any new neurological deficits. At the time of disease progression, new metastases were treated with SRS or WBRT, depending on the number of lesions.
Cost effective analysis endpoints and statistical methods
In this analysis, the receipts were collected and analyzed at the New York Presbyterian/Weill Cornell Medical Center. The cost consisted of the direct hospital related costs of each treatment. The costs in this study included direct patient care costs and excluded administrative overhead, facility maintenance, and other non-patient care costs. Costs did not take into consideration reimbursement as this varied widely based on the insurance plan of the individual. Moreover, length of stay was not included in this analysis since at our institution length of stay varies based on the availability of rehabilitation beds, the patient’s insurance plan, the approval of transfer to rehabilitation, the availability of transportation. These socio-economic factors would bias the results and thus length of stay was not factored into cost. Survival was also analyzed in this study, rather than local control rates, since survival is critical to calculating QALYs. Local control rates, radiation necrosis, and other complications have been reported in a separate study controlling for size of tumor and pathology [31]. In this study, Wernicke et al. demonstrated local freedom from progression (FFP) was 100 %. There was 1 adjacent leptomeningeal recurrence, resulting in a 1 year regional FFP of 93.8 % (95 % CI 63.2–99.1 %). 1 year distant FFP was 48.4 % (95 % CI 26.3–67.4 %). Median OS was 9.9 months (95 % CI 4.8 months, upper limit not estimated) and 1 year OS was 50.0 % (95 % CI 29.1–67.8 %). Complications included CSF leak (1), seizure (1), and infection (1). There was no radiation necrosis.
Median and curves of survival time were defined by the Kaplan–Meier estimator; further, the cost analysis focused on the time period of the relevant treatment. Cost effectiveness was defined as cost in dollars for a particular therapy per unit clinical outcome, defined as the median survival in years.
The cost-effective analysis was based on the quality-adjusted life years (QALY). QALY are utilized as a measure to quantify the quality of the survival each treatment modality provides. In order to accurately quantify the quality QALY were defined using two different scales: QALY A was defined as normal life, 1; mild disability, 0.8; moderate disability, 0.5; severe disability, 0.3; vegetative state, 0.2, and mortality, 0 [37–39]. QALY B utilized the Karnofsky performance status (KPS) grading system [40]. Incremental cost-effectiveness ratios (ICER) were calculated as cost per incremental cost/incremental effect. The ICER measures the incremental cost of each modality and evaluates its incremental rise in cost associated with its incremental rise in benefit as determined by the QALY. ICER indicate how much extra cost is incurred to produce any extra gains in QALY owing to implementation of a particular strategy compared with an alternative strategy.
Results
Patient characteristics and survival
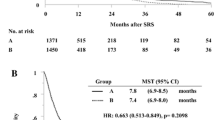
Demographic and clinical characteristics of the 49 patients in this study are presented in Table 1. The mean age of patients in the S + Cs-131 group was 65 years (range, 45–84 years) and in the S + SRS group it was 61 years (range, 32–84 years). The most common site of the metastatic tumors to the brain originated in the lungs, breast, and colon. All patients received surgery via a single craniotomy. The median radiation dose was 80 Gy for the S + Cs-131 group and 20 Gy for the S + SRS group. The median survival of S + Cs-131 and S + SRS were 15.5 and 11.3 months, and the 12 month survival rates were 61 and 49 %, respectively.
Cost-effective analysis
Table 2 summarizes the cost-effective analysis. The direct hospital costs of treatment per patient were: S + Cs131 = $19,271 and S + SRS = $44,219. Utilizing the two methods to quantify the QALY yielded similar results between each method using the median survivals for each group as reported above (p < 0.0001). The total costs divided by the QALY yields the cost-effectiveness for each treatment option. S + Cs-131 was significantly the more cost-effective method (p < 0.0001) when comparing the cost-effectiveness to S + SRS.
Additionally, evaluation of the cost-effectiveness using an ICER further shows the benefit of S + Cs-131. In the ICER analysis, summarized in Table 3, when compared to S + SRS, S + Cs-131, is viewed as being strongly dominant. A negative ICER value means that there is a less expensive and more effective treatment option, which in this case is S + Cs-131. Figure 1 compares the relative median survival times, 12 month survival rate, and hospital related costs between groups.
Discussion
There are several treatment options for patients with brain metastases and the cost effectiveness of each should be taken into account when the options are being weighed. Historically, WBRT has been the standard of care therapy for most patients with brain metastases [7–9, 41]. Although WBRT is effective at preventing local recurrence and controlling distant disease, it is associated with detriments in quality-of-life (QoL) measures [42, 43] and deterioration in neurocognitive abilities [12–15]. Additionally, WBRT offers no overall survival benefit compared with local therapy [16, 21, 44].
Surgical resection has been utilized for several reasons such as providing rapid relief of symptoms resulting from the mass effect of a large tumor, improving local control of brain metastases, and establishing a histological diagnosis when a brain metastasis is suspected [45]. Unfortunately, tumor recurrence with surgery alone is relatively high, around 46 % [44]. Rates of recurrence correlate with factors such as tumor size, location, histology, and en bloc resection. Therefore, adjuvant WBRT has been employed in the post-operative setting and has been shown to reduce local recurrences by 29 % [10]. However, such reduction in local recurrence comes at the expense of neurocognitive complications [10, 12, 46]. For this reason, attention has been turned to the addition of focal radiation to the resection bed in an effort to reduce the incidence of local failure while preserving neurocognitive abilities.
Recently, the use of post-operative SRS has been becoming more popular [47–50]. The local control of the resection cavity is reported to be similar to WBRT, ranging from 70 to 100 %, incidence of radiation necrosis is 0–33 %, and intracranial distant failure is 28–65 % [26]. The volume of irradiated tissue has been determined a predictor of symptomatic radiation necrosis in patients irradiated with SRS. Blonigen et al. reported that symptomatic radiation necrosis was observed in 10 % and asymptomatic radiation necrosis in 4 % for patients who received SRS to a mean dose of 18 Gy. Following multivariate regression analysis showed tumor volume (V8–V16 Gy) to be most predictive of symptomatic radiation necrosis (p < 0.0001) [51]. However, post-operative SRS presents a challenge in producing conformal plans targeting tumor cavities of a larger size (>3 cm) or irregular shapes (a round cavity makes an ideal target for SRS). In fact, larger tumor cavities treated with this technique may render poor local control (actuarial local tumor control rate at 1 year for lesions ≤3 cc was 96 % (95 % CI: 90–100 %) and >3 cc was 59 % (95 % CI: 39–79 %) [30], resulting from less conformal treatment plans [47, 51].
Intraoperative brachytherapy is an alternative method to improve local control after resection of brain metastases. This process involves lining the resection cavity with radiation sources at the time of resection. Brain metastases are usually focal and very well-circumscribed, in contrast to intrinsic brain tumors that may infiltrate deeply into surrounding brain. Adjunctive intraoperative visualization techniques (i.e. intraoperative MRI, intraoperative ultrasound) may be employed by the surgeon to make sure that GTR or residual tumor <1 cm3 be achieved in order for intraoperative Cs-131 to be applied. Intraoperative brachytherapy allows a high dose of radiation to be given to a localized area with a very steep dose fall-off, covering the tumor bed but sparing normal brain tissue beyond the vicinity of the tumor bed. Studies have shown local control of the resection cavity to be between 80 and 95 % [32, 33].
The coordination of intraoperative brachytherapy requires a team effort from a number of participants outside the operating room as well as inside: dosimetrists, physicists, radiation oncologists, neurosurgeon and radiation safety work together to carry out this procedure. All parties involved must be aware of the implant, carry out pre-implant planning (this involves our institutional monogram calculation which approximates the number of seeds to be ordered), informing radiation safety and preparing them and our dosimetrists and physics team for post-operative measurements of exposure and dose delivered. Such coordination ensures not only proper execution of an implant but also safety precarious to the personnel and family.
There have been several cost-effectiveness analyses regarding the treatment of brain metastases. Vuong et al. [52, 53], Rutigliano et al. [39] and Mehta et al. [54] have reported that SRS is more cost-effective than resection alone. Lee et al. [38] reported that SRS is more cost-effective than WBRT. Lal et al. [55] reported that SRS and observation is more cost effective than SRS and WBRT. Although, these studies did show SRS to be the more cost-effective treatment option, none of them compared them to Cs-131 brachytherapy.
In this study, we were able to compare S + SRS to S + Cs-131 brachytherapy. We have demonstrated that S + Cs-131 is a cost effective alternative to S + SRS. This was determined utilizing the median overall survival and various measures to calculate QALY and ICER. In our study the QALY that were determined utilizing both measures consistently showed that S + Cs-131 was better when compared to S + SRS (p < 0.0001). The ICER value for S + Cs-131 falls within the range of what is considered reasonable and acceptable in the literature for the cost per QALY ($50,000) while the QALY of modalities S + SRS fell outside this range [56].
Although not statistically significant, survival was higher with S + Cs-131 compared with S + SRS, which is consistent I-125 brachytherapy data [32]. However, survival is more a function of systemic disease control and is only useful in the calculation of QALYs. In addition, the median OS for patients receiving S + SRS was consistent with those reported in the literature [16, 18, 57, 58]. In order for the costs of S + SRS to compete with those of S + Cs-131, even assuming an equal quality of life for both arms, the overall survival from the S + SRS arm would need to be more than double the S + Cs-131 group. If one assumes an equal OS between the arms, the quality of life from the S + SRS arm would need to be more than double that as from the S + Cs-131 group. Therefore, even given the possible bias regarding patient allocation to the treatment arms, this analysis confirmed S + Cs-131 as the more cost-effective treatment arm when considering the direct hospital related costs of treatment.
It is important to discuss some of the limitations of this study. Our study is a single-center study that is characterized by small sample size yet has the advantage of being able to more accurately record the costs, both professional and technical. Criticisms of this study relate to its retrospective nature. Patient selection factors may have influenced the decision to perform one treatment modality over another. This study examines cost-effectiveness as they relate to hospital related costs and not patient costs. Follow-up costs and possible subsequent treatment was not part of this current analysis. We have assumed a similar distribution of such costs across the multiple treatment modalities. Although necrosis requiring re-operation would sharply raise the costs associated with that treatment, our results yielded no cases of radiation necrosis with S + Cs-131.
Conclusions
S + Cs-131 is a more cost effective alternative to S + SRS of brain metastases. Median survival was greater for this treatment arm and resulted in a greater QALY. Relative to S + Cs-131, S + SRS resulted in a negative ICER as it was more expensive yet provided a lower QALY. Therefore, from a resource allocation perspective, S + Cs-131 for brain metastases is the more cost-effective treatment option. There were lower costs directly charged by the hospital for S + Cs-131. Therefore, the overall cost-effectiveness of each treatment option should be taken into careful consideration when deciding the appropriate treatment for patients with brain metastases.
Abbreviations
- Cs-13:
-
Cesium-131
- I-125:
-
Iodine-125
- ICER:
-
Incremental cost-effectiveness ratio
- KPS:
-
Karnofsky performance status
- LINAC:
-
Linear accelerators
- QALY:
-
Quality adjusted life year
- SRS:
-
Stereotactic radiosurgery
- S:
-
Surgical resection
- WBRT:
-
Whole brain radiotherapy
References
Counsell CE, Collie DA, Grant R (1996) Incidence of intracranial tumours in the Lothian region of Scotland, 1989–90. J Neurol Neurosurg Psychiatry 61:143–150
Walker AE, Robins M, Weinfeld FD (1985) Epidemiology of brain tumors: the national survey of intracranial neoplasms. Neurology 35:219–226
Bradley KA, Mehta MP (2004) Management of brain metastases. Semin Oncol 31:693–701
Cappuzzo F, Mazzoni F, Maestri A, Di Stefano A, Calandri C, Crino L (2000) Medical treatment of brain metastases from solid tumours. Forum (Genova) 10:137–148
Varlotto JM, Flickinger JC, Niranjan A, Bhatnagar A, Kondziolka D, Lunsford LD (2005) The impact of whole-brain radiation therapy on the long-term control and morbidity of patients surviving more than one year after gamma knife radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 62:1125–1132
Cairncross JG, Posner JB (1983) The management of brain metastases. In: Walker MD (ed) Oncology of the nervous system. Cancer treatment and research. Martinus Nijhoff, Boston, pp 341–377
Berry HC, Parker RG, Gerdes AJ (1974) Irradiation of brain metastases. Acta Radiol Ther Phys Biol 13:535–544
Kurtz JM, Gelber R, Brady LW, Carella RJ, Cooper JS (1981) The palliation of brain metastases in a favorable patient population: a randomized clinical trial by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 7:891–895
Order SE, Hellman S, Von Essen CF, Kligerman MM (1968) Improvement in quality of survival following whole-brain irradiation for brain metastasis. Radiology 91:149–153
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322:494–500
Vecht CJ, Haaxma-Reiche H, Noordijk EM, Padberg GW, Voormolen JH, Hoekstra FH, Tans JT, Lambooij N, Metsaars JA, Wattendorff AR, Brand R, Hermans J (1993) Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery. Ann Neurol 33:583–590
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044. doi:10.1016/S1470-2045(09)70263-3
Crossen JR, Garwood D, Glatstein E, Neuwelt EA (1994) Neurobehavioral sequelae of cranial irradiation in adults: a review of radiation-induced encephalopathy. J Clin Oncol 12:627–642
DeAngelis LM, Delattre JY, Posner JB (1989) Radiation-induced dementia in patients cured of brain metastases. Neurology 39:789–796
Nieder C, Schwerdtfeger K, Steudel WI, Schnabel K (1998) Patterns of relapse and late toxicity after resection and whole-brain radiotherapy for solitary brain metastases. Strahlenther Onkol 174:275–278
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi G (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491
Chidel MA, Suh JH, Reddy CA, Chao ST, Lundbeck MF, Barnett GH (2000) Application of recursive partitioning analysis and evaluation of the use of whole brain radiation among patients treated with stereotactic radiosurgery for newly diagnosed brain metastases. Int J Radiat Oncol Biol Phys 47:993–999
Frazier JL, Batra S, Kapor S, Vellimana A, Gandhi R, Carson KA, Shokek O, Lim M, Kleinberg L, Rigamonti D (2010) Stereotactic radiosurgery in the management of brain metastases: an institutional retrospective analysis of survival. Int J Radiat Oncol Biol Phys 76:1486–1492. doi:10.1016/j.ijrobp.2009.03.028
Kocher M, Maarouf M, Bendel M, Voges J, Müller RP, Sturm V (2004) Linac radiosurgery versus whole brain radiotherapy for brain metastases: a survival comparison based on the RTOG recursive partitioning analysis. Strahlenther Onkol 180:263–267
Rades D, Pluemer A, Veninga T, Hanssens P, Dunst J, Schild SE (2007) Whole-brain radiotherapy versus stereotactic radiosurgery for patients in recursive partitioning analysis classes 1 and 2 with 1 to 3 brain metastases. Cancer 110:2285–2292
Sneed PK, Suh JH, Goetsch SJ, Sanghavi SN, Chappell R, Buatti JM, Regine WF, Weltman E, King VJ, Breneman JC, Sperduto PW, Mehta MP (2002) A multi-institutional review of radiosurgery alone versus radiosurgery with whole brain radiotherapy as the initial management of brain metastases. Int J Radiat Oncol Biol Phys 53:519–526
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ Jr (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363:1665–1672
Kondziolka D, Patel A, Lunsford LD, Kassam A, Flickinger JC (1999) Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys 45:427–434
Rades D, Kueter J, Pluemer A, Veninga T, Schild SE (2009) A matched-pair analysis comparing whole-brain radiotherapy plus stereotactic radiosurgery versus surgery plus whole-brain radiotherapy and a boost to the metastatic site for one or two brain metastases. Int J Radiat Oncol Biol Phys 73:1077–1081. doi:10.1016/j.ijrobp.2008.05.035
Rades D, Kueter J, Veninga T, Gliemroth J, Schild SE (2009) Whole brain radiotherapy plus stereotactic radiosurgery (WBRT + SRS) versus surgery plus whole brain radiotherapy (OP + WBRT) for 1-3 brain metastases: results of a matched pair analysis. Eur J Cancer 45:400–404. doi:10.1016/j.ejca.2008.10.033
Gans JH, Raper DM, Shah AH, Bregy A, Heros D, Lally BE, Morcos JJ, Heros RC, Komotar RJ (2013) The role of radiosurgery to the tumor bed after resection of brain metastases. Neurosurgery 72:317–324. doi:10.1227/NEU.0b013e31827fcd60
Jarvis LA, Simmons NE, Bellerive M, Erkmen K, Eskey CJ, Gladstone DJ, Hug EB, Roberts DW, Hartford AC (2012) Tumor bed dynamics after surgical resection of brain metastases: implications for postoperative radiosurgery. Int J Radiat Oncol Biol Phys 84:943–948. doi:10.1016/j.ijrobp.2012.01.067
Jagannathan J, Yen CP, Ray DK, Schlesinger D, Oskouian RJ, Pouratian N, Shaffrey ME, Larner J, Sheehan JP (2009) Gamma knife radiosurgery to the surgical cavity following resection of brain metastases. J Neurosurg 111:431–438. doi:10.3171/2008.11.JNS08818
Hartford AC, Galvin JM, Beyer DC, Eichler TJ, Ibbott GS, Kavanagh B, Schultz CJ, Rosenthal SA, American College of Radiology, American Society for Radiation Oncology (2012) American College of Radiology (ACR) and American Society for Radiation Oncology (ASTRO) Practice Guideline for Intensity-modulated Radiation Therapy (IMRT). Am J Clin Oncol35:612–617. doi: 10.1097/COC.0b013e31826e0515
Aoyama H, Shirato H, Onimaru R, Kagei K, Ikeda J, Ishii N, Sawamura Y, Miyasaka K (2003) Hypofractionated stereotactic radiotherapy alone without whole-brain irradiation for patients with solitary and oligo brain metastasis using noninvasive fixation of the skull. Int J Radiat Oncol Biol Phys 56:793–800
Wernicke AG, Yondorf MZ, Peng L, Trichter S, Nedialkova L, Sabbas A, Kulidzhanov F, Parashar B, Nori D, Clifford Chao KS, Christos P, Kovanlikaya I, Pannullo S, Boockvar JA, Stieg PE, Schwartz TH (2014) Phase I/II study of resection and intraoperative cesium-131 radioisotope brachytherapy in patients with newly diagnosed brain metastases. J Neurosurg 121:338–348. doi:10.3171/2014.3.JNS131140
Dagnew E, Kanski J, McDermott MW, Sneed PK, McPherson C, Breneman JC, Warnick RE (2007) Management of newly diagnosed single brain metastasis using resection and permanent iodine-125 seeds without initial whole-brain radiotherapy: a two institution experience. Neurosurg Focus 22:E3
Huang K, Sneed PK, Kunwar S, Kragten A, Larson DA, Berger MS, Chan A, Pouliot J, McDermott MW (2009) Surgical resection and permanent iodine-125 brachytherapy for brain metastases. J Neurooncol 91:83–93. doi:10.1007/s11060-008-9686-2
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of rtog protocol 90-05. Int J Radiat Oncol Biol Phys 47:291–298
Dhabaan A, Schreibmann E, Siddiqi A, Elder E, Fox T, Ogunleye T, Esiashvili N, Curran W, Crocker I, Shu HK (2012) Six degrees of freedom cbct-based positioning for intracranial targets treated with frameless stereotactic radiosurgery. J Appl Clin Med Phys 13:3916. doi:10.1120/jacmp.v13i6.3916
Prabhu RS, Dhabaan A, Hall WA, Ogunleye T, Crocker I, Curran WJ, Shu HK (2013) Clinical outcomes for a novel 6 degrees of freedom image guided localization method for frameless radiosurgery for intracranial brain metastases. J Neurooncol 113:93–99. doi:10.1007/s11060-013-1093-7
Cho DY, Tsao M, Lee WY, Chang CS (2006) Socioeconomic costs of open surgery and gamma knife radiosurgery for benign cranial base tumors. Neurosurgery 58:866–873
Lee WY, Cho DY, Lee HC, Chuang HC, Chen CC, Liu JL, Yang SN, Liang JA, Ho LH (2009) Outcomes and cost-effectiveness of gamma knife radiosurgery and whole brain radiotherapy for multiple metastatic brain tumors. J Clin Neurosci 16:630–634. doi:10.1016/j.jocn.2008.06.021
Rutigliano MJ, Lunsford LD, Kondziolka D, Strauss MJ, Khanna V, Green M (1995) The cost effectiveness of stereotactic radiosurgery versus surgical resection in the treatment of solitary metastatic brain tumors. Neurosurgery 37:445–455
Picot J, Cooper K, Bryant J, Clegg AJ (2011) The clinical effectiveness and cost-effectiveness of bortezomib and thalidomide in combination regimens with an alkylating agent and a corticosteroid for the first-line treatment of multiple myeloma: a systematic review and economic evaluation. Health Technol Assess 15:1–204. doi:10.3310/hta15410
Cairncross JG, Kim JH, Posner JB (1980) Radiation therapy for brain metastases. Ann Neurol 7:529–541
Chow E, Davis L, Holden L, Tsao M, Danjoux C (2005) Prospective assessment of patient-rated symptoms following whole brain radiotherapy for brain metastases. J Pain Symptom Manage 30:18–23
Kondziolka D, Niranjan A, Flickinger JC, Lunsford LD (2005) Radiosurgery with or without whole-brain radiotherapy for brain metastases: the patients’ perspective regarding complications. Am J Clin Oncol 28:173–179
Patchell RA, Tibbs PA, Regine WF, Dempsey RJ, Mohiuddin M, Kryscio RJ, Markesbery WR, Foon KA, Young B (1998) Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA 280:1485–1489
Sawaya R, Hammoud M, Schoppa D, Hess KR, Wu SZ, Shi WM, Wildrick DM (1998) Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors. Neurosurgery 42:1044–1055
Filley CM, Kleinschmidt-DeMasters BK (2001) Toxic leukoencephalopathy. N Engl J Med 345:425–432
Do L, Pezner R, Radany E, Liu A, Staud C, Badie B (2009) Resection followed by stereotactic radiosurgery to resection cavity for intracranial metastases. Int J Radiat Oncol Biol Phys 73:486–491. doi:10.1016/j.ijrobp.2008.04.070
Jensen CA, Chan MD, McCoy TP, Bourland JD, Deguzman AF, Ellis TL, Ekstrand KE, McMullen KP, Munley MT, Shaw EG, Urbanic JJ, Tatter SB (2011) Cavity-directed radiosurgery as adjuvant therapy after resection of a brain metastasis. J Neurosurg 114:1585–1591. doi:10.3171/2010.11.JNS10939
Karlovits BJ, Quigley MR, Karlovits SM, Miller L, Johnson M, Gayou O, Fuhrer R (2009) Stereotactic radiosurgery boost to the resection bed for oligometastatic brain disease: challenging the tradition of adjuvant whole-brain radiotherapy. Neurosurg Foc 27:E7. doi:10.3171/2009.9.FOCUS09191
Quigley MR, Fuhrer R, Karlovits SM, Karlovits BJ, Johnson M (2008) Single session stereotactic radiosurgery boost to the post-operative site in lieu of whole brain radiation in metastatic brain disease. J Neurooncol 87:327–332. doi:10.1007/s11060-007-9515-z
Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, Breneman JC (2010) Irradiated volume as a predictor of brain radionecrosis after linear accelerator stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 77:996–1001. doi:10.1016/j.ijrobp.2009.06.006
Vuong DA, Rades D, Le AN, Busse R (2012) The cost-effectiveness of stereotactic radiosurgery versus surgical resection in the treatment of brain metastasis in Vietnam from the perspective of patients and families. World Neurosurg 77:321–328. doi:10.1016/j.wneu.2011.05.050
Vuong DA, Rades D, van Eck AT, Horstmann GA, Busse R (2013) Comparing the cost-effectiveness of two brain metastasis treatment modalities from a payer’s perspective: stereotactic radiosurgery versus surgical resection. Clin Neurol Neurosurg 115:276–284. doi:10.1016/j.clineuro.2012.05.005
Mehta M, Noyes W, Craig B, Lamond J, Auchter R, French M, Johnson M, Levin A, Badie B, Robbins I, Kinsella T (1997) A cost-effectiveness and cost-utility analysis of radiosurgery versus resection for single-brain metastases. Int J Radiat Oncol Biol Phys 39:445–454
Lal LS, Byfield SD, Chang EL, Franzini L, Miller LA, Arbuckle R, Reasonda L, Feng C, Adamus A, Swint JM (2012) Cost-effectiveness analysis of a randomized study comparing radiosurgery with radiosurgery and whole brain radiation therapy in patients with 1 to 3 brain metastases. Am J Clin Oncol 35:45–50. doi:10.1097/COC.0b013e3182005a8f
Evans C, Tavakoli M, Crawford B (2004) Use of quality adjusted life years and life years gained as benchmarks in economic evaluations: a critical appraisal. Health Care Manag Sci 7:43–49
Datta R, Jawahar A, Ampil FL, Shi R, Nanda A, D’Agostino H (2004) Survival in relation to radiotherapeutic modality for brain metastasis: whole brain irradiation versus gamma knife radiosurgery. Am J Clin Oncol 27:420–424
Kalkanis SN, Kondziolka D, Gaspar LE, Burri SH, Asher AL, Cobbs CS, Ammirati M, Robinson PD, Andrews DW, Loeffler JS, McDermott M, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Ryken TC, Linskey ME (2010) The role of surgical resection in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96:33–43. doi:10.1007/s11060-009-0061-8
Acknowledgments
Parts of this manuscript were presented at the Society for Neuro-Oncology in 2012, Washington, DC. Doctor Wernicke supported by the funds from the National Institute of Health CTSC KL2 Comparative Effectiveness Research Award UL1-TR000457.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
The 1st authorship is shared between the authors A. Gabriella Wernicke and Menachem Z. Yondorf.
Rights and permissions
About this article
Cite this article
Wernicke, A.G., Yondorf, M.Z., Parashar, B. et al. The cost-effectiveness of surgical resection and cesium-131 intraoperative brachytherapy versus surgical resection and stereotactic radiosurgery in the treatment of metastatic brain tumors. J Neurooncol 127, 145–153 (2016). https://doi.org/10.1007/s11060-015-2026-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-2026-4