Abstract
The aim of this study was to determine the predictability of vertebral compression fracture (VCF) development applying the spinal instability neoplastic score (SINS) prior to delivery of stereotactic spinal radiosurgery (SSRS) for spinal metastases. From two prospective cohorts of SSRS for spinal metastases, we selected patients with a low degree of cord compression or cauda equine from C3 to S1 and analyzed 79 patients enrolled according to binary SINS criteria. The primary endpoint was the development of a de novo VCF or progression of an existing fracture after SSRS. We identified 32 fractures (40.5 %): 19 de novo and 13 progressive. The mean time to fracture after SSRT was 3.3 months (range, 0.4–34.1 months). In 41 patients with low SINS (0–6), 7 patients (17.1 %) developed a fracture after SSRS. In 38 patients with high SINS (7–12), 25 (65.8 %) developed a fracture. Among the 32 fractures, 15 were symptomatic. Patients with high SINS were more likely to experience symptomatic fractures (31.6 %) than were patients with lower SINS (7.4 %). On univariate and multivariate analysis, 24-month fracture-free rates were 78.7 and 33.7 % in low and high SINS group, respectively and high SINS was found to be a significant risk factor for VCFs and symptomatic fractures (respectively, HR 5.6, p = 0.04; HR 5.3, p = 0.01). SINS is a useful tool for predicting the development of VCF after SSRS for spinal metastases. Prophylactic cement augmentation should not be considered for patients with lower SINS, since the risk of fracture is low.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The spine is the most common location for osseous metastases, with up to 40 % of cancer patients affected [1]. Conventional fractionated radiation therapy has traditionally played an important role in pain palliation, resulting in a near 70 % incidence of pain improvement; however, the dose is limited by a relatively low spinal cord radiation tolerance [1–3]. Spine stereotactic body radiotherapy, also known as spine stereotactic radiosurgery (SSRS), is growing practice for select patients with spinal metastases [2, 3]. Numerous studies have demonstrated the safety and efficacy of SSRS for the treatment of spinal metastases with encouraging results both as a primary modality and in the setting of repeat irradiation after conventional radiation treatment failures [4–6]. However, SSRS may increase the risk of certain serious adverse events, and evidence-based description of these risks ought to precede widespread adoption of this technology in the clinic.
In particular, the most significant potential complications of SSRS are radiation myelopathy and vertebral compression fracture (VCF), with the latter increasingly being recognized as a significant and common adverse event [2, 3, 7–11]. Authors of biomechanical and imaging studies have attempted to create risk models to predict VCF in spinal metastases [8, 10, 11]. A more recent expert consensus from the Spine Oncology Study Group (SOSG) has led to the identification of spinal instability factors including clinical symptoms and radiologic findings and introduced spinal instability neoplastic score (SINS) [12, 13].
In this study, we retrospectively reviewed data from two previous spinal metastatic disease prospective protocols at our institution. The primary purpose of this study was to determine if the SINS could predict VCF. Our secondary objective was to determine risk factors for VCF in patients treated with SSRS for spinal metastases.
Materials and methods
Patient selection
Two hundred nine patients enrolled in two prospective cohorts for spinal and paraspinal metastatic disease and treated with SSRS between March 2004 and March 2011 at the MD Anderson Cancer Center (National Clinical Trial identifier NCT00508443 and NCT00492817) were reviewed for inclusion in this study. All patients received SSRS based on recommendations from a multidisciplinary evaluation by neurosurgeons, radiation oncologists, and medical oncologist. Patients had confirmed spinal metastases based on primary tumor diagnosis and spinal magnetic resonance (MR) imaging.
We performed a retrospective review of the MR imaging immediately before the SSRS in all patients enrolled in both prospective cohorts and scored the levels to be treated according to the epidural spinal cord compression classification (ESCC) proposed by Bilsky et al. [14]. The individuals who met the following criteria were included in the current study: (1) spinal metastasis with no (ESCC grade 0) or a low (ESCC grades 1a and 1b) degree of epidural spinal cord compression from the C3 to S1 vertebrae, (2) single level or multiple levels of treatment, up to three contiguous levels within one radiation field, with or without prior radiation, up to but not exceeding 45 Gy; and (3) a minimum clinical and radiologic follow-up of 6 months. The following exclusion criteria were applied: (1) unstable spinal architecture (a SINS of greater than 13); (2) history of vertebroplasty, kyphoplasty, and open surgery at the index level; (3) paraspinal tumors not involving a vertebra, or neurological compromise from cord compression; (4) multiple radiation fields; (5) age less than 18 years old; (6) insufficient information to provide a baseline SINS; and (7) loss to follow-up within 6 months. The records of all patients were retrieved through a review of the patients’ charts and radiology reports. Demographic data were collected, including age, sex, location, primary histology, and affected period as well. The study was independently reviewed and approved by the institutional review board of MD Anderson Cancer Center (2005-0445 and 2005-0446).
Stereotactic spinal radiosurgery
The spine SSRS technique has been previously reported [5, 6]. All cases were reviewed in a multidisciplinary spine radiosurgery tumor board. The neurosurgery team evaluated all patients for unstable spinal lesions prior to treatment. Patients whose spines were mechanically unstable were ineligible for the study. Based on MR imaging immediately before SSRS, each treated vertebral segment was scored according to the SINS criteria as described by Fisher et al. [12]. In brief, the individual SINS criteria consist of location, type of pain, spinal misalignment, presence of baseline VCF, type of lesion, and whether the tumor involves the posterolateral elements. Lytic, sclerotic, or mixed tumors were classified based on appearance on CT (Table 1). The SINS scoring system classifies patients as stable (SINS 0–6), potentially unstable (SINS 7–12), and unstable (SINS 13–18) based on the overall score. In cases in which multiple vertebrae were treated in a single target volume, each vertebral segment was not considered independent and was analyzed as one segment according to our protocol.
Assessments of follow up outcomes after SSRS
Patients were evaluated at 2, 4 and 2 months following completion of radiation therapy by telephone, fax, or mail. Patients were seen for follow-up visits at 3, 6, 9, 12, 18 and 24 months and then every 6 months thereafter. Medical history, neurological exam, and neurologic function were assessed at these visits. Dates of fracture (based on the last imaging follow-up) and death were recorded. Other general and radiation-related complications after SSRS were also monitored during the follow-up period.
MR images of the spine were obtained prior to treatment and at 3, 6, 9 and 12 months after treatment and every 6 months thereafter. MR images were evaluated for radiologic tumor progression and VCF. VCF was measured by comparing the vertebra’s height on prior MR imaging or, if unavailable, an average height of the vertebrae immediately superior and inferior and then classifying it on a quintile ordinal scale. End plate–only fractures were included in the study, as were all other fractures. The length of the clinical and radiologic follow-ups were defined as the period from the date of SSRS to the date of the last clinical visit and the date of the patient’s most recent MR imaging, respectively.
During follow-up, the types and dates of additional surgical procedures to relieve pain or neurologic deterioration due to symptomatic compression fracture, tumor progression, and other causes were recorded. Patients were also assessed for toxicity using the Common Toxicity Criteria for Adverse Effect (CTCAE version3.0).
Analysis of prognostic factors related to survival
The outcome variable of interest was the time to development of a de novo VCF or progression of preexisting fractures prior to SSRS. These time-to-event data were calculated in months from the start date of SSRS to the event date or last follow-up imaging study if fracture-free. De novo VCF was defined as any kind of fracture, including end plate fracture, developed from normal vertebrae. A progression of preexisting fractures was defined as an increase in loss of height from end plate-only fractures or as an increase in the loss of height sufficient to move into the next quintile percentage of compression, as per a prior report [8].
Analyzed risk factors for VCF were age, sex, type of primary malignancy, overall SINS and each criteria of SINS, spinal canal encroachment (Bilsky classification), level of lesion, and radiation dose per fraction. Additional factors analyzed included whether any targeted systemic therapy had been given within 2 months before SSRS, prior radiation to the treated segment, total dose prescribed, and number of fractions.
Statistical analysis
The student’s t test was used for continuous and parametric values, and the Chi squared test and Fisher’s exact test were used for categorical dates and values, respectively. Overall survival and fracture-free survival were estimated using the Kaplan–Meier method. Kaplan–Meier Curves was constructed using GraphPad Prism version 6 (GraphPad Software, La Jolla, CA). The univariable cox regression analysis was used to compare period of free fracture with a potential predictor of interest. All variables associated with VCF with a significance level <0.1 were entered in a multivariate analysis to obtain adjusted hazard ratios for categorized SINS. A Cox proportional hazards regression model was used as a multivariate analysis to determine the joint effect of potential factors that were found to be significant on univariate analysis. Continuous variables such as age, whole spine involvement rate, vertebral body osteolystic rate, SINS, and radiation dose were categorized as two groups. These statistical analyses were conducted using SPSS statistics version 22.0 (IBM SPSS, Chicago, IL). A p-value <0.05 was regarded as statistically significant.
Results
Patient demographics and details of SSRS
From the prospective cohorts, 79 patients, including 40 men and 39 women, who underwent SSRS were eligible for inclusion in the current study. The baseline characteristics of these 79 patients are summarized in Table 2 and grouped according to total SINS as either stable (0–6) or potentially unstable (7–12). The overall mean age at SBRT was 57 years (range, 23–80 years). Regarding the lesion level, seven tumors were located in the cervical region, 42 in the thoracic region, and 30 in the lumbosacral spine. Prior to SSRS, preexisting fractures were identified in 22 patients (28 %), with 17 of those fractures involving the end plate only. SINS ranged from 3 to 12 (median, 6). The median clinical and imaging follow-up periods were 21.2 and 15.3 months, respectively.
In this cohort of 79 patients, 100 spinal segments were treated. Sixty percent (60 spinal segments) were single targets, and the remaining had multiple (two or three) spinal segments treated within a single target volume. Treatment plans consisted of one or three fractions for median doses of 18 and 27 Gy, respectively. Doses were constrained so that the maximum dose to the spinal cord was 9–10 Gy. Details of SSRS, and additional surgery in the 79 patients are summarized in Table 3.
Development of fractures
Overall, 32 (40.5 %) out of the 79 patients presented a VCF, of those 20 (62.5 %) were de novo fractures and 12 (37.5 %) were fractures that had progressed. The median and mean times to fracture for the entire group who experienced fracture after SSRS were 3.3 months and 5.7 months, respectively (range, 0.4–34.1 months). The distribution of fractures according to monthly post-SSRS interval is described in Fig. 1a, b. Sixty-three percent of all VCFs occurred within the first 4 months post-SSRS. We also summarized the proportion of vertebral segments treated and fractured according to each SINS component. An overview of the follow-up status of the patients after SSRS is shown in Fig. 1c.
a The distribution of vertebral compression fractures according to monthly post-stereotactic spinal radiosurgery (SSRS) interval. b The proportion of vertebral segments treated and fractured according to each spinal instability neoplastic score (SINS) component. c An overview diagram of the follow-up status in 79 patients after SSRS, Asterisk indicates the case of compression fracture combined radiation failure
Complications and salvage interventions after SSRS
There were no CTCAE Grade 3 and 4 toxicities, such as esophagitis and radiation myelopathy. Salvage interventions were performed for 15 out of 32 (46.9 %) of the VCFs because of pain. Of these 15 patients, five underwent salvage with instrumented spinal reconstructive surgery, and the remaining 10 underwent salvage with a vertebral augmentation procedure alone. During follow-up, tumor progression following SSRS was noted in 15 patients (19.0 %) with a median length of 5 months to tumor progression. Nine patients showed de novo fracture or progression of fracture during follow-up. Surgery was performed for four patients due to accompanying fracture and in another two patients due to tumor progression without fracture.
Survival and prognosis-related factors
At the time of analysis, 15 patients were still alive and 64 had died. The median and mean overall survival periods were 22.6 and 35.5 months, respectively. The 1- and 2-year overall survival rates were 77.2 and 49.4 %, respectively. The 6- and 12-month fracture-free rates were 68.8 and 59.5 %, respectively (2-year, 52.7 %).
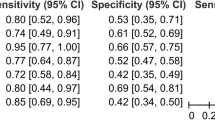
According to univariate analyses, old age, high ESCC grade 1a and 1b, high dose per fraction, radiation failure and high SINS were significant predictors of VCF. Kaplan–Meier plots for age ≥65 years (hazard ratio [HR] 2.47, 95 % confidence interval [CI] 1.23–4.95, p = 0.008), ESCC grade 1a and 1b (HR 3.91 95 % CI 1.37–11.19, p = 0.006), dose per fraction >20 Gy (HR 2.91, 95 % CI 1.33–6.33, p = 0.05), tumor progression (HR 2.19, 95 % CI 1.00–4.82, p = 0.045) and a SINS of ≥ 7 (HR 6.01, 95 % CI 2.58–13.99, p = 0.000) were significantly different (Fig. 2). However, a multivariate analysis of those factors found to be significant on univariate analysis identified only age (HR 2.15, 95 % CI 1.07–4.32, p = 0.032) and SINS (HR 5.63, 95 % CI 2.41–13.13, p = 0.000) as the independent predictors of VCF (Table 4). 24-month fracture-free rates in patients <65 and ≥65 years-old were 69.5 %, and 32.2 %,and in patients low and high SINS were 78.7 and 33.7 % respectively.
Kaplan–Meier fracture-free survival curves. a For age at stereotatic spinal radiosurgery (SSRS) ≥65 years (hazard ratio [HR] 2.47, 95 % confidence interval [CI] 1.23–4.95, p = 0.008), median free of fracture period was undefined and 6.13 months in each group. b Spinal instability neoplastic score (SINS) of ≥7 (HR 6.01, 95 % CI 2.58–13.99, p < 0.0001), median free of fracture period was undefined and 5.84 months in each group
Univariate analysis of symptomatic fracture identified ESCC grade 1a and 1b (HR 7.30, 95 % CI 1.03–55.56, p = 0.025) and high SINS score (HR 5.33, 95 % CI 1.50–18.93, p = 0.004) as significant factor of VCF and multivariate analysis identified only high SINS score (HR 5.33, 95 % CI 1.50–18.93, p = 0.01) to be at significant factor showed higher hazard rate of VCF. 24-momths symptomatic fracture-free rates in low and high SINS were 91.8 and 65.0 %, respectively.
Discussion
Local control of metastatic spine lesions is usually accomplished with radiation therapy, surgery, or a combination of both [1, 15–20]. Recently, the use of SSRS has increased for the management of radio-resistant metastatic and primary spinal tumours [3]. SSRS represents a major advance in radiotherapy planning and delivery, and outcomes show excellent local control and pain control rate for spine metastases [2, 5, 6]. In this study, the overall long-term radiologic control rate was 81 % during the median 21-month follow-up, in accordance with previous reports [5, 6]. Although SSRS appears more effective than conventional palliative radiotherapy, it may also increase the risk of serious adverse events that would otherwise not occur, such as transient radiculitis or radiation myelitis, as well as compression fracture [4, 5].
VCF is a fairly low-risk adverse event (approximately 5 % risk) after conventional radiotherapy, whereas a broad risk estimates for VCF after spinal SSRS range from 11 to 39 % [8–11]. A study by Rose et al. revealed that 39 % of treated sites had new or progressive fractures after SSRS, and the median time to VCF was 25 months [10]. Subsequently, two other reports suggested that the risk may be closer to 11–20 %, with a median time to VCF of 2–3 months [8, 9, 11]. Similarly, our study showed 12-month cumulative radiologic and symptomatic fracture risks of 40.5 and 19 %, respectively. With respect to risk factors for VCF, there is also variability among published studies. Significant factors identified included vertebral body tumor involvement by at least 41–60 %, age greater than 55 years, pre-SSRS VCF, spinal deformity, and an SSRS dose per fraction of 20 Gy. On multivariable proportional hazards analysis, the only consistent predictor among the three major investigations was that lytic tumors had a greater risk of SSRS-induced VCF, and the hazard ratios (HR) ranged from 3.9 to 12.2 [4, 9]. However, these studies only focused on the primary radiologic factors shown to be significant individual predictors of VCF.
Additionally, factors unique to the current study include the significant effects of an older age more than 65 years. An increased age as factors predicting further fracture are consistent with results of other studies. In previous studies, age more than 55–57 years were proposed as cut-off value based on mean age of their study, whereas our study were based on the definition of geriatric oncology [8, 10, 11].
Recently, the SOSG introduced the SINS, which is a standardized framework to help physicians assess and categorize spinal instability from tumorous conditions [12, 13, 21]. Prior to the development of the SINS classification, the assessment of spinal integrity lacked standardization and proved difficult, especially for non-surgical members of the multidisciplinary care team.
The reliability of SINS has already been evaluated among members of the SOSG and other spine surgeons [13, 21]. SINS showed excellent interobserver and intraobserver reliability in determining 3 clinically relevant categories of stability. Considering the multidisciplinary aspect of care of metastatic cancer patients, the reliability of SINS was also tested among radiation oncologists and radiologists [22, 23]. Recently, Versteeg et al. validated SINS in the clinical setting with a retrospective database review of patients who underwent palliative surgery or radiotherapy [24].
Sahgal et al. evaluated the adverse event of VCF and the use of SINS in predicting VCF in their experience with SSRS [11]. With respect to predictive factors, they suggest that baseline VCF, lytic tumor, and misalignment were predictive among the six SINS criteria, whereas the others were not. They also concluded that SINS can be an important tool to identify patients at greater risk for SSRS-induced VCF, but the overall score was not predictive. We suspect that their limitations originated from subjectivity in assessment and the likelihood that patients describing severe mechanical pain or neurologically compromised patients would have been surgically stabilized and not included in their analysis. In our study, however, patients with a high SINS were more likely to experience fractures after SSRS for spinal metastases than were patients with a low SINS (66 and 17 %, respectively, p < 0.0001), independent of symptoms, primary tumor, and functional status. Similarly, the proportions of symptomatic VCF for patients with lower SINS and those with higher SINS were 7.3 and 31.6 %, respectively p = 0.009). Based on our results, we suggest that SINS may predict radiologic and symptomatic fracture after SSRS. However, it was interesting point that the proportion of symptomatic fracture in fracture patients of each SINS group was similar, at 42.9 and 48 % respectively (p = 1.0).
Recent studies are encouraging because they indicate the potential for SINS to identify patients who could benefit from a prophylactic stabilization procedure or early surgical intervention if signs or symptoms of VCF begin to develop after SSRS [11]. It is important to note that we investigated the role of SINS in predicting for this specific end point, and these results not only reflect the utility of SINS as a tool to communicate spinal instability but also clarify its ability to predict those at higher risk of VCF post-SSRS.
A potential limitation of this, however, is that radiologists, radiation oncologists, and other medical specialists may determine different SINS than spinal surgeons because of differences in image interpretation and the amount of available clinical information [21–23]. Several cases rated as stable by surgeons were considered potentially unstable by radiation oncologists in a validation study of radiologists and radiation oncologists [21, 22]. Such variability may be originated from the lack of familiarity with some of the terms in SINS in less experienced physicians. It indicates that some form of training may be required for less experienced physicians.
Conclusion
SINS may be a useful tool to predict the risk of VCF development after SSRS for spinal metastases. In the absence of level 1 data, prophylactic cement augmentation or stabilization using a minimally invasive surgical procedure should not be considered for patients with lower SINS, since the risk of fracture is low. A SINS of ≥7 should prompt consultation with a spine surgeon, who can highlight the available surgical options during collaborative discussions on a patient’s optimal treatment.
References
Klimo P Jr, Schmidt MH (2004) Surgical management of spinal metastases. Oncologist 9:188–196
Lo SS, Chang EL, Yamada Y, Sloan AE, Suh JH, Mendel E (2007) Stereotactic radiosurgery and radiation therapy for spinal tumors. Expert Rev Neurother 7(1):85–93
Pan H, Simpson DR, Mell LK, Mundt AJ, Lawson JD (2011) A survey of stereotactic body radiotherapy use in the United States. Cancer 117(19):4566–4572
Sahgal A, Whyne CM, Ma L, Larson DA, Fehlings MG (2013) Vertebral compression fracture after stereotactic body radiotherapy for spinal metastases. Lancet Oncol 14(8):e310–e320
Garg AK, Shiu AS, Yang J, Wang XS, Allen P, Brown BW, Grossman P, Frija EK, McAleer MF, Azeem S, Brown PD, Rhines LD, Chang EL (2012) Phase 1/2 trial of single-session stereotactic body radiotherapy for previously unirradiated spinal metastases. Cancer 118(20):5069–5077
Garg AK, Wang XS, Shiu AS, Allen P, Yang J, McAleer MF, Azeem S, Rhines LD, Chang EL (2011) Prospective evaluation of spinal reirradiation by using stereotactic body radiation therapy: the University of Texas MD Anderson Cancer Center experience. Cancer 117(15):3509–3516
Sahgal A, Bilsky M, Chang EL, Ma L, Yamada Y, Rhines LD, Létourneau D, Foote M, Yu E, Larson DA, Fehlings MG (2011) Stereotactic body radiotherapy for spinal metastases: current status, with a focus on its application in the postoperative patient. A review. J Neurosurg Spine 14(2):151–166
Boehling NS, Grosshans DR, Allen PK, McAleer MF, Burton AW, Azeem S, Rhines LD, Chang EL (2012) Vertebral compression fracture risk after stereotactic body radiotherapy for spinal metastases. Clinical article. J Neurosurg Spine 16(4):379–386
Cunha MV, Al-Omair A, Atenafu EG, Masucci GL, Letourneau D, Korol R, Yu E, Howard P, Lochray F, da Costa LB, Fehlings MG, Sahgal A (2012) Vertebral compression fracture (VCF) after spine stereotactic body radiation therapy (SBRT): analysis of predictive factors. Int J Radiat Oncol Biol Phys 84(3):e343–e349
Rose PS, Laufer I, Boland PJ, Hanover A, Bilsky MH, Yamada J, Lis E (2009) Risk of fracture after single fraction image-guided intensity-modulated radiation therapy to spinal metastases. J Clin Oncol 27(30):5075–5079
Sahgal A, Atenafu EG, Chao S, Al-Omair A, Boehling N, Balagamwala EH, Cunha M, Thibault I, Angelov L, Brown P, Suh J, Rhines LD, Fehlings MG, Chang E (2013) Vertebral compression fracture after spine stereotactic body radiotherapy: a multi-institutional analysis with a focus on radiation dose and the spinal instability neoplastic score. J Clin Oncol 31(27):3426–3431
Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, Harrop JS, Fehlings MG, Boriani S, Chou D, Schmidt MH, Polly DW, Biagini R, Burch S, Dekutoski MB, Ganju A, Gerszten PC, Gokaslan ZL, Groff MW, Liebsch NJ, Mendel E, Okuno SH, Patel S, Rhines LD, Rose PS, Sciubba DM, Sundaresan N, Tomita K, Varga PP, Vialle LR, Vrionis FD, Yamada Y, Fourney DR (2010) A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976) 35(22):e1221–e1229
Fourney DR, Frangou EM, Ryken TC, Dipaola CP, Shaffrey CI, Berven SH, Bilsky MH, Harrop JS, Fehlings MG, Boriani S, Chou D, Schmidt MH, Polly DW, Biagini R, Burch S, Dekutoski MB, Ganju A, Gerszten PC, Gokaslan ZL, Groff MW, Liebsch NJ, Mendel E, Okuno SH, Patel S, Rhines LD, Rose PS, Sciubba DM, Sundaresan N, Tomita K, Varga PP, Vialle LR, Vrionis FD, Yamada Y, Fisher CG (2011) Spinal instability neoplastic score: an analysis of reliability and validity from the spine oncology study group. J Clin Oncol 29(22):3072–3077
Bilsky MH, Laufer I, Fourney DR, Groff M, Schmidt MH, Varga PP, Vrionis FD, Yamada Y, Gerszten PC, Kuklo TR (2010) Reliability analysis of the epidural spinal cord compression scale. J Neurosurg Spine 13(3):324–328
Wang JC, Boland P, Mitra N, Yamada Y, Lis E, Stubblefield M, Bilsky MH (2004) Single-stage posterolateral transpedicular approach for resection of epidural metastatic spine tumors involving the vertebral body with circumferential reconstruction: results in 140 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine 1(3):287–298
Aghayev K, Papanastassiou ID, Vrionis F (2011) Role of vertebral augmentation procedures in the management of vertebral compression fractures in cancer patients. Curr Opin Support Palliat Care 5(3):222–226
Berenson J, Pflugmacher R, Jarzem P, Zonder J, Schechtman K, Tillman JB, Bastian L, Ashraf T, Vrionis F, Cancer Patient Fracture Evaluation (CAFE) Investigators (2011) Balloon kyphoplasty versus non-surgical fracture management for treatment of painful vertebral body compression fractures in patients with cancer: a multicentre, randomised controlled trial. Lancet Oncol 12(3):225–235
Gerszten PC, Germanwala A, Burton SA, Welch WC, Ozhasoglu C, Vogel WJ (2005) Combination kyphoplasty and spinal radiosurgery: a new treatment paradigm for pathological fractures. J Neurosurg Spine 3(4):296–301
Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J (2005) A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976) 30(19):2186–2191
Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T (2001) Surgical strategy for spinal metastases. Spine (Phila Pa 1976) 26(3):298–306
Campos M, Urrutia J, Zamora T, Román J, Canessa V, Borghero Y, Palma A, Molina M (2014) The spine instability neoplastic score: an independent reliability and reproducibility analysis. Spine J 14(8):1466–1469
Fisher CG, Schouten R, Versteeg AL, Boriani S, Varga PP, Rhines LD, Kawahara N, Fourney D, Weir L, Reynolds JJ, Sahgal A, Fehlings MG, Gokaslan ZL (2014) Reliability of the spinal instability neoplastic score (SINS) among radiation oncologists: an assessment of instability secondary to spinal metastases. Radiat Oncol 9:69
Fisher CG, Versteeg AL, Schouten R, Boriani S, Varga PP, Rhines LD, Heran MK, Kawahara N, Fourney D, Reynolds JJ, Fehlings MG, Gokaslan ZL (2014) Reliability of the spinal instability neoplastic scale among radiologists: an assessment of instability secondary to spinal metastases. Am J Roentgenol 203(4):869–874
Versteeg AL, Fisher CG, Oner C, Verlaan JJ (2015) Validation of the spinal instability neoplastic score: a retrospective analysis. Global Spine J 5(Suppl 1):A225. doi:10.1055/s-0035-1554329
Funding
This work was not supported by any grant or research funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict interest.
Ethics committee approval
The study was independently reviewed and approved by the institutional review board of MD Anderson Cancer Center (2005-0445 and 2005-0446).
Rights and permissions
About this article
Cite this article
Lee, SH., Tatsui, C.E., Ghia, A.J. et al. Can the spinal instability neoplastic score prior to spinal radiosurgery predict compression fractures following stereotactic spinal radiosurgery for metastatic spinal tumor?: a post hoc analysis of prospective phase II single-institution trials. J Neurooncol 126, 509–517 (2016). https://doi.org/10.1007/s11060-015-1990-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1990-z