Abstract
Radiotherapy is often used in the management of primary brain tumors, but late cerebrovascular risks remain incompletely characterized. We examined the relationship between radiotherapy and the risk of death from cerebrovascular disease (CVD) in this population. We used the Surveillance, Epidemiology, and End Results Program to identify 19,565 patients of any age diagnosed with a primary brain tumor between 1983–2002. Multivariable competing risks analysis and an interaction model were used to determine whether receipt of radiotherapy was associated with an increased risk of CVD-specific death, adjusting for tumor proximity to central arterial circulations of the brain. The median follow up in surviving patients was 12.75 years. Baseline characteristics were similar in patients who did and did not receive radiotherapy. Ten-year CVD-specific mortality in patients with tumors near central arterial circulations who did and did not receive radiotherapy were 0.64 % (95 % CI 0.42–0.93 %) versus 0.16 % (95 % CI 0.055–0.40 %), p = 0.01. After adjustment for demographic, tumor-related, and treatment-related covariates, patients with tumors near central arterial circulations were significantly more likely to experience CVD-specific mortality after radiotherapy (HR 2.81; 95 % CI 1.25–6.31; p = 0.01); no association was observed among patients with more distant tumors (HR 0.77; 95 % CI 0.50–1.16; p = 0.21). The interaction model showed that tumor location was a key predictor of the risk of radiotherapy-associated, CVD-specific mortality (p-interaction = 0.004). Patients receiving radiotherapy for tumors near but not distant from the central vasculature of the brain are at increased risk for death secondary to CVD, which should be considered when counseling patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vascular disease is an increasingly recognized long-term toxicity of radiotherapy [1]. This toxicity is particularly devastating because it often occurs in patients who are disease free with regard to the oncologic condition that warranted the use of radiation. A large body of literature pertaining to ischemic cardiovascular disease after radiation therapy exists [1–5], yet less is known about cerebrovascular disease (CVD). Most prior reports of CVD after radiotherapy have either focused on the pediatric population [6–9] or on adults with head and neck cancers [10–12], and less is known about risks in the adult brain tumor population. Previous studies in adults have focused narrowly on the risk of CVD after irradiation of the pituitary, with mixed conclusions [13–17].
Accordingly, we used the Surveillance, Epidemiology, and End Results (SEER) Program to characterize the impact of radiotherapy on CVD-specific mortality among patients with primary brain tumors, and to identify populations at higher risk for the development of this late toxicity.
Materials and methods
Patient population
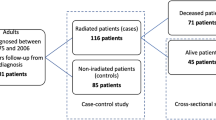
We used the SEER database to retrospectively identify 29,745 patients of any age diagnosed with a primary brain tumor over a 20 year period between 1983–2002. Sponsored by the National Cancer Institute, the SEER program collects and publishes cancer incidence, treatment, and survival data from population-based cancer registries. The program captures approximately 97 % of incident cancers, and the tumor registries now cover approximately 28 % of the United States population [18]. The first year of eligibility for our study was 1983 given that certain covariates utilized in our study are only available in SEER from this point afterwards; 2002 was the last year of inclusion for diagnosis to allow sufficient follow-up time to assess for potential impact of radiotherapy on CVD-related outcomes. Patients with glioblastoma were excluded given their short median survival [19]. Patients who were diagnosed at autopsy, had metastatic disease at diagnosis (including spread to distant sites within the central nervous system), were diagnosed with another malignancy prior to developing a primary brain tumor, or who had clinical information that was not complete were excluded, leaving 19,565 patients eligible for analysis. Patients were considered to have received adjuvant radiotherapy if radiation was administered within four and twelve months of diagnosis for patients diagnosed up to and after 1998, respectively, per coding guidelines established by SEER [20].
Study design and statistical analysis
Baseline patient characteristics were compared with the t-test for continuous variables (all were normally distributed) and the Chi square test for categorical variables. Death due to cerebrovascular disease, the primary endpoint of the study, was displayed using cumulative incidence curves and compared with Gray’s test [21]. Fine and Gray’s competing risks regression [22] was employed to assess the impact of adjuvant radiotherapy on CVD-specific mortality after adjustment for the following covariates: age, gender, race (non-white vs. white), median household income, educational status (percentage of adults ≥25 years of age with a high school education), residence type (urban vs. rural), employment of cancer-directed surgery to the primary site vs not, and tumor histology. Income, education, and residence type were assessed at the county level by linkage to the 2003 United States Department of Agriculture rural–urban continuum codes [23], 2000 United States Census [24], and 2004 small area income and poverty estimates from the United States Census, respectively [25]. Death due to cerebrovacular disease included deaths attributed to occlusion/stenosis of cerebral/precerebral arteries, intracranial hemorrhage, and cerebrovascular disease that was ill-defined. The apriori hypothesis was that radiotherapy would increase the risk of CVD-related death for patients with tumors near the central arterial circulations (i.e. those near the base of skull, including the circle of Willis, carotid arteries, or the vertebrobasilar circulation) but not patients with more remote tumors. Therefore, an interaction model was employed in which the adjusted impact of radiotherapy on CVD-specific mortality was analyzed in patients with tumors near vs remote from the central arterial circulations. Tumors near the central arterial circulations were defined as those involving the brainstem or infratentorial brain, as well as tumors that either originated supratentorially and extended infratentorially or originated infratentorially and extended supratentorially. Tumors defined as distant from central arterial circulations included those with cerebral primaries. Because some tumors of the frontal or temporal lobe can be located in close proximity to the central arterial circulations, a sensitivity analysis was performed in which such patients were excluded.
The median follow up among surviving patents was 12.75 years (range 0.1–28.9 years). All p values are two sided. The threshold of 0.05 was used to determine significance. Statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC). Competing risks regression was performed using R version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria). This study was approved by our institutional review board; informed consent was waived.
Results
Patient characteristics
Baseline and clinically relevant patient characteristics are depicted in Table 1. Patients who received radiotherapy were older than those who did not (p < 0.001) although the upper quartile of age was similar in both cohorts (59–98 and 60–99 years of age, respectively). In addition, patients receiving radiotherapy were more likely to be male, white, reside in rural environments, come from areas of higher educational level, and not have surgery on the primary site, although the magnitude of such differences was small. No differences in county level income were seen between the two cohorts.
CVD-specific mortality
Cumulative incidence curves displaying CVD-specific mortality in patients with tumors near and distant from central arterial circulations, as stratified by receipt of radiotherapy vs not, are depicted in Fig. 1. Among patients with tumors near central vasculature, CVD-specific mortality was higher in patients who did, vs did not, receive radiotherapy (p = 0.01, Fig. 1a). Among this subset, estimates of 10- and 20-year CVD-specific mortality in patients who did and did not receive radiotherapy were 0.64 % (95 % CI 0.42–0.93 %) versus 0.16 % (95 % CI 0.055–0.40 %) and 1.10 % (95 % CI 0.75–1.56 %) versus 0.39 % (95 % CI 0.16–0.81 %), respectively. Among patients with tumors distant from the central vasculature, those receiving radiotherapy were less likely to experience CVD-specific death (p = 0.01, Fig. 1b).
The multivariable Fine and Gray’s interaction-based regression model (Table 2) indicated that, after adjustment for baseline demographic, socioeconomic, tumor-related, and treatment-related patient characteristics, patients with tumors near the central arterial circulations displayed an increased rate of CVD-specific mortality when treated with radiotherapy vs not (hazard ratio [HR] 2.81; 95 % CI 1.25–6.31; p = 0.01). Conversely, there was no significant association between receipt of radiotherapy and CVD-specific mortality in patients with more distant tumors (HR 0.77; 95 % CI 0.50–1.16; p = 0.21). The impact of radiotherapy on the risk of CVD-specific death was significantly different depending on the relative location of the tumor (p-interaction = 0.004). As a sensitivity analysis, after patients with frontal and temporal tumors were excluded, the analysis remained largely unchanged, with a p-interaction of 0.01.
Discussion
In this study, we examined the impact of radiotherapy on CVD-specific mortality in a large cohort of adult and pediatric patients with primary brain tumors, and identified that radiotherapy significantly increased the risk of death from CVD, compared to those patients who did not receive radiotherapy. Tumor location modified this risk, wherein patients with tumors near the central arterial circulations were at risk for development of CVD-specific mortality after receiving radiotherapy, whereas patients with tumors distant from the central vasculature had no increased risk.
The results of our study are significant because CVD-related mortality represents one of the few lethal long-term toxicities of radiotherapy. Given the emphasis of prior investigations on either pediatric patients [1–5] or adults with head and neck cancer or pituitary adenoma [6–9], our results contribute an important new finding to the body of literature on radiotherapy-associated CVD. In addition, most prior studies utilized an endpoint of CVD, not CVD-specific mortality. Our use of the latter outcome measure allowed us to identify CVD of highest impact, especially as some CVD are clinically silent and detected only on surveillance neuro-imaging [26]. In addition, the use of a competing risks analysis, which has not been commonly used in this body of literature, allowed us to adjust for competing causes of death, such as death due to tumor progression, which is particularly relevant for the brain tumor population. For example, had a Cox proportional hazards model been used for analysis, the results would have shown an even larger effect of radiotherapy on the primary endpoint (HR for association of radiotherapy with CVD-specific mortality in the cohort with tumors near central arterial circulations = 3.37; 95 % CI 1.56–7.26; p = 0.002) yet the magnitude of the association would have been overestimated, given that patients who die from other causes can no longer experience CVD-specific mortality, which the Cox model does not account for.
Among adults, prior investigations linking radiotherapy to CVD have largely been conducted in patients with head/neck cancers, such as squamous cell carcinomas of the oropharynx [10, 12], in patients with pituitary adenoma [13–17] and in patients with arteriovenous malformations [27]. Haynes et al. evaluated 413 patients treated with radiotherapy to the head and neck. Over the duration of the follow up period, 20 patients experienced CVD (2–146 months post-treatment). All patients who experienced CVD were estimated to have received high doses of radiation (generally ≥60 Gy), suggesting a link between dose to the central arterial circulations in the neck and CVD risk. The hypothesis connecting radiotherapy dose to CVD risk is further supported by another SEER-Medicare cohort analyzed by Smith et al., who found that definitive but not adjuvant radiation was associated with an increased risk of CVD in patients with head and neck cancers [11]. The authors point out that that the higher radiation doses utilized in definitive radiation (up to 70–72 Gy) were higher than those used in the adjuvant setting (generally 57–66 Gy) [11]. These findings are echoed in the pediatric population, wherein a study of 4227 childhood cancer survivors demonstrated that CVD mortality was elevated among patients who received the highest radiotherapy doses to the base of skull, but not among those who received lower doses [28].
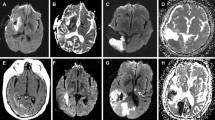
Among pediatric patients with brain tumors, prior literature suggests a relationship between receipt of radiotherapy and CVD [6, 28, 29]. Mechanistically, radiotherapy-related atherosclerotic changes in the arterial wall, endothelial damage, subintimal fibrosis and hypertrophy, dysfunction of the elastic membrane, and thickening and fibrosis of the muscular wall may be the changes that predispose patients to vascular compromise and ischemic events [6, 7]. Large arterial occlusive vasculopathy has been reported in several investigations of childhood brain tumor survivors who received prior cranial radiotherapy compared to those who did not, and is often visualized using magnetic resonance angiography [9, 30–32]. The impact of vascular dysfunction within the central circulations of the brain in particular may result in the most deadly of CVD [29, 33, 34]. Our results support the results of prior investigations but also add to the body of literature on the subject by suggesting a link between anatomic proximity to the central arterial circulations in the brain and risk of CVD mortality in adults, presumably through higher radiotherapy dose received by the nearby vasculature. For example, a prior study among 431 pediatric patients found that dose received by the circle of Willis was correlated with CVD risk [9], and another pediatric study found the highest risk of cerebrovascular events occurred in patients who received increasing radiotherapy doses specifically to the prepontine cistern, which also abuts the base of skull [28]. Our use of the CVD-specific mortality endpoint and the interaction analysis based on tumor location allowed us to identify a link between receipt of radiotherapy, tumor location, and lethal CVD.
Several limitations of our study warrant mention. First, SEER does not record CVD as isolated events; it only records CVD-related mortality. Accordingly, rates of CVD-specific mortality in our study were relatively modest. Second, most patients in our study had malignant brain tumors, as SEER did not incorporate large numbers of patients with benign brain tumors until 2004. Given that patients with benign tumors are less likely to die of their disease than patients with malignant tumors, they are at greater risk of dying of other causes, like CVD. It is therefore possible that our results underestimate the deleterious impact of radiation on CVD-related death in patients with benign brain tumors. Third, SEER only records radiation administration between 4-12 months after diagnosis; patients who received radiation thereafter would not have been recorded as having received radiation in SEER. Therefore, the results of our study may be artificially biased towards the null, given that many patients with low-grade malignant tumors may defer the use of upfront radiotherapy in lieu of radiotherapy at the time of disease progression [35]. Fourth, SEER does not record details of radiotherapy, such as the dose/fractionation utilized. We therefore used tumor location as a proxy of radiation dose to the central arterial circulations. We have no reason to suspect that patients with tumors near the central vasculature received a higher dose of radiation than tumors in other locations. In fact, given the proximity to the brainstem and optic chiasm, it is possible tumors near the central vasculature may have received slightly lower doses of radiation, due to purposeful dose-sparing of nearby critical structures. Further study will be required to definitively assess the precise relationship between radiation dose to the central vasculature of the brain and CVD-related endpoints. Fifth, information relating to smoking status or comorbidities such as hypertension, hyperlipidemia, diabetes are not available in SEER; we used a robust multivariable model to adjust for other confounders, including age. In addition, we would not expect patients with brain tumors near the central vasculature to be systematically different with regard to comorbidities and smoking status than patients with more distant tumors. Regardless, radiotherapy may represent only one of several risk factors for vascular damage in this patient cohort. Lastly, it is possible that patients with frontal/temporal tumors may have had primaries that were near the central arterial circulations of the brain, which would also bias our results towards the null. As a sensitivity analysis, however, we excluded such patients from the analysis and the results did not substantially change.
In conclusion, our study suggests that radiotherapy carries a non-negligible risk of CVD-related death in patients with tumors near the central arterial circulations. This effect was not seen for tumors located elsewhere in the brain. Radiation oncologists treating patients with primary brain tumors with reasonable life expectancies should consider limiting high radiation doses to the central vasculature when possible. At-risk patients should be cautioned about the risk of a radiotherapy-associated CVD before and after receipt of radiotherapy, and dose to the central vessels should be minimized. In such patients, other comorbidities predictive for CVD, such as hypertension, should be controlled optimally. Most importantly, the risk of radiotherapy-associated CVD mortality should be factored in by clinicians when determining whether or not to administer radiotherapy to patients with brain tumors adjacent to central arterial circulations.
References
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Bronnum D, Correa C, Cutter D, Gagliardi G, Gigante B, Jensen MB, Nisbet A, Peto R, Rahimi K, Taylor C, Hall P (2013) Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 368:987–998. doi:10.1056/NEJMoa1209825
Giordano SH, Kuo YF, Freeman JL, Buchholz TA, Hortobagyi GN, Goodwin JS (2005) Risk of cardiac death after adjuvant radiotherapy for breast cancer. J Natl Cancer Inst 97:419–424. doi:10.1093/jnci/dji067
Harris EE, Correa C, Hwang WT, Liao J, Litt HI, Ferrari VA, Solin LJ (2006) Late cardiac mortality and morbidity in early-stage breast cancer patients after breast-conservation treatment. J Clin Oncol 24:4100–4106. doi:10.1200/JCO.2005.05.1037
Correa CR, Litt HI, Hwang WT, Ferrari VA, Solin LJ, Harris EE (2007) Coronary artery findings after left-sided compared with right-sided radiation treatment for early-stage breast cancer. J Clin Oncol 25:3031–3037. doi:10.1200/JCO.2006.08.6595
Mueller S, Sear K, Hills NK, Chettout N, Afghani S, Gastelum E, Haas-Kogan D, Fullerton HJ (2013) Risk of first and recurrent stroke in childhood cancer survivors treated with cranial and cervical radiation therapy. Int J Radiat Oncol Biol Phys 86:643–648. doi:10.1016/j.ijrobp.2013.03.004
Bowers DC, Liu Y, Leisenring W, McNeil E, Stovall M, Gurney JG, Robison LL, Packer RJ, Oeffinger KC (2006) Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: a report from the Childhood Cancer Survivor Study. J Clin Oncol 24:5277–5282. doi:10.1200/JCO.2006.07.2884
Bowers DC, McNeil DE, Liu Y, Yasui Y, Stovall M, Gurney JG, Hudson MM, Donaldson SS, Packer RJ, Mitby PA, Kasper CE, Robison LL, Oeffinger KC (2005) Stroke as a late treatment effect of Hodgkin’s Disease: a report from the Childhood Cancer Survivor Study. J Clin Oncol 23:6508–6515. doi:10.1200/JCO.2005.15.107
Mueller S, Fullerton HJ, Stratton K, Leisenring W, Weathers RE, Stovall M, Armstrong GT, Goldsby RE, Packer RJ, Sklar CA, Bowers DC, Robison LL, Krull KR (2013) Radiation, atherosclerotic risk factors, and stroke risk in survivors of pediatric cancer: a report from the Childhood Cancer Survivor Study. Int J Radiat Oncol Biol Phys 86:649–655. doi:10.1016/j.ijrobp.2013.03.034
Campen CJ, Kranick SM, Kasner SE, Kessler SK, Zimmerman RA, Lustig R, Phillips PC, Storm PB, Smith SE, Ichord R, Fisher MJ (2012) Cranial irradiation increases risk of stroke in pediatric brain tumor survivors. Stroke 43:3035–3040. doi:10.1161/STROKEAHA.112.661561
Hong JC, Kruser TJ, Gondi V, Mohindra P, Cannon DM, Harari PM, Bentzen SM (2013) Risk of cerebrovascular events in elderly patients after radiation therapy versus surgery for early-stage glottic cancer. Int J Radiat Oncol Biol Phys 87:290–296. doi:10.1016/j.ijrobp.2013.06.009
Smith GL, Smith BD, Buchholz TA, Giordano SH, Garden AS, Woodward WA, Krumholz HM, Weber RS, Ang KK, Rosenthal DI (2008) Cerebrovascular disease risk in older head and neck cancer patients after radiotherapy. J Clin Oncol 26:5119–5125. doi:10.1200/JCO.2008.16.6546
Haynes JC, Machtay M, Weber RS, Weinstein GS, Chalian AA, Rosenthal DI (2002) Relative risk of stroke in head and neck carcinoma patients treated with external cervical irradiation. Laryngoscope 112:1883–1887. doi:10.1097/00005537-200210000-00034
Flickinger JC, Nelson PB, Taylor FH, Robinson A (1989) Incidence of cerebral infarction after radiotherapy for pituitary adenoma. Cancer 63:2404–2408
Brada M, Ashley S, Ford D, Traish D, Burchell L, Rajan B (2002) Cerebrovascular mortality in patients with pituitary adenoma. Clin Endocrinol (Oxf) 57:713–717
Brada M, Burchell L, Ashley S, Traish D (1999) The incidence of cerebrovascular accidents in patients with pituitary adenoma. Int J Radiat Oncol Biol Phys 45:693–698
Erfurth EM, Bulow B, Svahn-Tapper G, Norrving B, Odh K, Mikoczy Z, Bjork J, Hagmar L (2002) Risk factors for cerebrovascular deaths in patients operated and irradiated for pituitary tumors. J Clin Endocrinol Metab 87:4892–4899. doi:10.1210/jc.2002-020526
Sattler MG, Vroomen PC, Sluiter WJ, Schers HJ, van den Berg G, Langendijk JA, Wolffenbuttel BH, van den Bergh AC, van Beek AP (2013) Incidence, causative mechanisms, and anatomic localization of stroke in pituitary adenoma patients treated with postoperative radiation therapy versus surgery alone. Int J Radiat Oncol Biol Phys 87:53–59. doi:10.1016/j.ijrobp.2013.05.006
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) Research Data (1973–2011), National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2014, based on the November 2013 submission
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. doi:10.1056/NEJMoa043330
Iezzoni LI, Ngo LH, Li D, Roetzheim RG, Drews RE, McCarthy EP (2008) Early stage breast cancer treatments for younger Medicare beneficiaries with different disabilities. Health Serv Res 43:1752–1767. doi:10.1111/j.1475-6773.2008.00853.x
Gray RJ (1988) A Class of K-Sample Tests for Comparing the Cumulative Incidence of a Competing Risk. Ann Stat 16:1141–1154
Fine JP, Gray RJ (1999) A proportional hazards model for the sub distribution of a competing risk. J Am Stat Assoc 94:496–509
United States Department of Agriculture Rural-Urban Continuum Codes. http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed 13 Jan 2013
United States Census Bureau. Census 2000 Gateway. http://www.census.gov/main/www/cen2000.html. Accessed 12 Dec 2012
United States Census. Small Area Income and Poverty Estimates. http://www.census.gov/did/www/saipe/data/statecounty/data/2004.html. Accessed 12 Dec 2012
Fouladi M, Langston J, Mulhern R, Jones D, Xiong X, Yang J, Thompson S, Walter A, Heideman R, Kun L, Gajjar A (2000) Silent lacunar lesions detected by magnetic resonance imaging of children with brain tumors: a late sequela of therapy. J Clin Oncol 18:824–831
Gross BA, Ropper AE, Du R (2013) Vascular complications of stereotactic radiosurgery for arteriovenous malformations. Clin Neurol Neurosurg 115:713–717. doi:10.1016/j.clineuro.2012.08.008
Haddy N, Mousannif A, Tukenova M, Guibout C, Grill J, Dhermain F, Pacquement H, Oberlin O, El-Fayech C, Rubino C, Thomas-Teinturier C, Le-Deley MC, Hawkins M, Winter D, Chavaudra J, Diallo I, de Vathaire F (2011) Relationship between the brain radiation dose for the treatment of childhood cancer and the risk of long-term cerebrovascular mortality. Brain 134:1362–1372. doi:10.1093/brain/awr071
Caplan L, Chung CS, Wityk R, Glass T, Tapia J, Pazdera L, Chang HM, Dashe J, Chaves C, Vemmos K, Leary M, Dewitt L, Pessin M (2005) New England medical center posterior circulation stroke registry: I. Methods, data base, distribution of brain lesions, stroke mechanisms, and outcomes. J Clin Neurol 1:14–30. doi:10.3988/jcn.2005.1.1.14
Nishizawa S, Ryu H, Yokoyama T, Ninchoji T, Shimoyama I, Yamamoto S, Uemura K (1991) Post-irradiation vasculopathy of intracranial major arteries in children–report of two cases. Neurol Med Chir (Tokyo) 31:336–341.
Brant-Zawadzki M, Anderson M, DeArmond SJ, Conley FK, Jahnke RW (1980) Radiation-induced large intracranial vessel occlusive vasculopathy. AJR Am J Roentgenol 134:51–55. doi:10.2214/ajr.134.1.51
Omura M, Aida N, Sekido K, Kakehi M, Matsubara S (1997) Large intracranial vessel occlusive vasculopathy after radiation therapy in children: clinical features and usefulness of magnetic resonance imaging. Int J Radiat Oncol Biol Phys 38:241–249.
Schonewille WJ, Algra A, Serena J, Molina CA, Kappelle LJ (2005) Outcome in patients with basilar artery occlusion treated conventionally. J Neurol Neurosurg Psychiatry 76:1238–1241. doi:10.1136/jnnp.2004.049924
Lindsberg PJ, Mattle HP (2006) Therapy of basilar artery occlusion: a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke 37:922–928. doi:10.1161/01.STR.0000202582.29510.6b
van den Bent MJ, Afra D, de Witte O, Ben Hassel M, Schraub S, Hoang-Xuan K, Malmstrom PO, Collette L, Pierart M, Mirimanoff R, Karim AB (2005) Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: the EORTC 22845 randomised trial. Lancet 366:985–990. doi:10.1016/S0140-6736(05)67070-5
Acknowledgments
The authors have no acknowledgments to report. This study has not been presented elsewhere.
Disclosures
The authors have no financial disclosures to report.
Funding
No funding was required for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aizer, A.A., Du, R., Wen, P.Y. et al. Radiotherapy and death from cerebrovascular disease in patients with primary brain tumors. J Neurooncol 124, 291–297 (2015). https://doi.org/10.1007/s11060-015-1839-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1839-5