Abstract
Bevacizumab is widely used for treatment of high-grade gliomas and other malignancies. Because bevacizumab has been shown to be associated with neurocognitive decline, this study is designed to investigate whether prolonged treatment with bevacizumab is also associated with brain atrophy. We identified 12 high-grade glioma patients who received bevacizumab for 12 months at the first recurrence and 13 matched controls and blindly compared the volumes of the contralateral hemispheres and contralateral ventricle in these two groups at baseline and after 12 ± 2 months of the baseline scan by two independent analyses. The volumes of the contralateral hemispheres and ventricles did not differ significantly between the two groups at baseline. Whereas, in the control group the volumes of the contralateral hemisphere changed subtly from baseline to follow-up (p = 0.23), in the bevacizumab-treated group the volumes significantly decreased from baseline to follow-up (p = 0.03). There was significant increase in the contralateral ventricle volume from base line to follow-up scans in both the control group (p = 0.01) and in the bevacizumab group (p = 0.005). Both the absolute and the percentage changes of contralateral hemisphere volumes and contralateral ventricular volumes between the two patient groups were statistically significant (p < 0.05). Results of this study demonstrate prolonged treatment with bevacizumab is associated with atrophy of the contralateral brain hemisphere.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vascular endothelial growth factor (VEGF) is a subfamily of growth factors that are involved in both vasculogenesis and angiogenesis. VEGFA, which is often referred to as VEGF, is the most studied factor regulating angiogenesis. It activates VEGF receptors (VEGFR1 and VEGFR2) and plays a critical role during embryonic development, as well as in homeostatic functions in fully developed brain.
In the adult brain, VEGF plays an essential role in homeostasis of normal neuronal and astrocyte functions. The most prominent site of VEGF expression is in the choroid plexus, and VEGF plays an important role in choroid plexus endothelial cell survival and fenestrae formation [1]. In brain parenchyma, astrocytes are the primary source of VEGF [2–6], where VEGF plays a major role in upregulation of different genes in response to altered cerebral perfusion and metabolism [7]. Recent evidence shows that VEGF is also expressed in the adult brain in a region specific manner and executes nontraditional homeostatic functions that are not angiogenesis-dependent or even perfusion dependent. [8] Of the many known functions, VEGF has an important role as a neurogenic factor that is essential for neuronal stem cell production and neuronal differentiation in the hippocampus [3, 9–11], and in the subventricular zone [10–14], and it also functions in neuroblast migration and neuronal maturation [8]. Additionally, it has been shown that upregulation of VEGF in the hippocampus improves memory as a result of increasing plasticity of mature hippocampal neurons [3], and hippocampal neurogenesis [9]. In addition VEGF has been shown to enhance hippocampal memory by stabilization of hypoxia inducible factor (HIF) in the hippocampus [15].
VEGF plays a crucial role in the physiology of high-grade gliomas. There is upregulation of VEGF production in high-grade gliomas mediated by autocrine and paracrine production in the hypoxic microenvironment of the tumor tissue [16–19]. Excessive production of VEGF leads to new blood vessel formation. However, VEGF-induced tumor vessels in glioblastoma (GBM) are disorganized and highly permeable, resulting in loss of blood brain barrier (BBB) integrity. The impaired BBB results in brain edema, which often causes serious clinical symptoms in GBM patients. Furthermore, higher VEGF expression in gliomas correlates with increased tumor invasiveness and higher histological grade [20]. These findings provide a rationale for the development of anti-angiogenesis therapy. Of the many developed antiangiogenic drugs, bevacizumab, a humanized monoclonal antibody against VEGF, is most commonly used for the treatment of recurrent GBM [21, 22].
With the wide spread use of bevacizumab in GBM and in other cancers, new adverse biological effects are gradually being recognized. Bevacizumab treatment can significantly change the glioma physiology by promoting tumor cell invasiveness through activation of MET signaling that is induced by inhibition of VEGF [23, 24]. Also, a recently completed phase III clinical trial comparing the efficacy of bevacizumab with the standard of care treatment in newly diagnosed GBM patients showed a significant neurocognitive decline in patients treated with bevacizumab [25]. In clinical practice, we have noticed that more prominent enlargement of brain ventricles in patients treated with bevacizumab, as compared to the patients treated with the standard of care. These observations led to our hypothesis that treatment with bevacizumab is associated with brain atrophy.
In this retrospective study, we compared the volume of the contralateral (non-tumor side) brain hemisphere and contralateral lateral ventricular volume in patients treated with bevacizumab plus standard of care treatment (bevacizumab group) with patients treated only with standard of care treatment regimen including radiation and temozolomide (control group) in a blinded fashion.
Methodology
Study set up and patient selection
The University of Alabama at Birmingham Institutional Review Board approved this Health Insurance Portability and Accountability Act (HIPAA) compliant study and waived the requirement of informed consent. Patients with histopathologically confirmed high-grade gliomas were included in the study. Higher-grade gliomas developing from previously known WHO grade II tumors were excluded from the study because these tumors have a different time course of disease and heterogeneous treatment experience. In addition, we excluded all patients who were treated with more than one course of fractionated radiation therapy or who received a second dose of radiation therapy at tumor recurrence (Table 1). The inclusion criteria were: (1) overall survival longer than 1 year from the initiation of bevacizumab therapy, (2) availability of a baseline MRI that included a 3D post contrast T1 weighted sequence within prior 1 month of initiation of bevacizumab therapy, (3) availability of a follow-up MRI that included a 3D post contrast T1 weighted sequence after 12 ± 2 months initiation of the bevacizumab treatment, (4) treated with standard Stupp protocol [26] at the diagnosis and (5) bevacizumab treatment was started at first recurrence. All patients with bi-hemispheric involvement, tumor extension to the ventricles, midline tumor (corpus callosum involvement), midline deviation and significant mass effect to the ventricles were excluded. All the volumetric analysis were performed on the contralateral hemisphere (non tumor bearing), not in the ipsilateral (tumor containing) brain hemisphere in order to avoid treatment-related changes of brain and or ventricular volumes such as anti-edema effect of bevacizumab, steroids and variable size of the resection.
Bevacizumab group
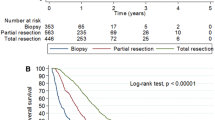
We retrospectively evaluated all the patients with high grade gliomas (n = 154) who received bevacizumab therapy in the Division of Neuro-oncology in the Neurology Department at the University of Alabama at Birmingham (UAB) between December 2007 and January 2013. Only 62/154 patients lived longer than 1 year. Details of the bevacizumab therapy were not known in 6 patients because they were treated at different hospitals after initiation of their treatment. Of the remaining 56 patients, only 12 patients (Table 1) met the inclusion and exclusion criteria: 7 patients had primary GBM, 3 patients had anaplastic astrocytoma (AA) and 2 patients had anaplastic oligoastrocytoma (AO). Most of the patients were excluded because the 3D post contrast T1 weighted sequence was not available for analysis either at the baseline or at the second follow-up scan (n = 28). Furthermore, 7 patients had bi-hemispheric tumors, 4 patients had tumor extension to the ventricles, and 5 patients had midline involvement (Fig. 1).
Of the 12 patients in the bevacizumab group, 11 patients were initially treated with tumor resection and 1 patient had a biopsy only (thalamic tumor). After initial resection or biopsy, all patients were treated with concurrent radiation and temozolomide therapy (75 mg/m2) followed by maintenance temozolomide therapy (150–200 mg/m2) for 5 consecutive days every month). Of the included 12 patients, 8 patients received ≥12 cycles of temozolomide therapy at the time of follow-up MRI and the remaining 4 patients received ≤12 cycles of temozolomide therapy at the time of follow-up MRI. Fractionated radiation therapy was delivered at UAB in 6 patients (60 Gy = 5, 50 Gy = 1). The remaining 6 patients were treated at different hospitals and the dose of radiation was not documented. Only 4 patients were treated with oral dexamethasone at a daily dose varying between 0.5 and 4 mg at the time of baseline scan and 5 patients were treated with oral dexamethasone at a daily dose varying between 0.5 and 8 mg at the time of follow-up scan.
Control group
In the control group, we included primary GBM patients who were treated at UAB between January 2006 and December 2007. Diagnosis of primary GBM was based on clinico-radiological findings that met the following three criteria: (1) neurological symptoms for less than 3 months with no clinical or histopathological evidence of a preexisting less malignant precursor lesions, (2) brain imaging findings at presentation that are suggestive of high-grade infiltrative tumor, and (3) histopathologically proven GBM [27, 28]. As the median time difference between the diagnosis and initiation of bevacizumab treatment in the bevacizumab group was 9 months, the baseline scan for the control group was obtained 9 ± 2 months after the initial diagnosis and the follow up scan was obtained 12 ± 2 months after the base line scan. One patient had tumor recurrence before the baseline scan and additional 2 patients had recurrence between the baseline and follow-up scans. All the recurrent tumors were treated with resection and chemotherapy. Radiation therapy was not used to treat any of the recurrent tumors.
All 13 patients (Table 1) in the control group were treated with standard treatment protocol) at diagnosis: resection followed by concurrent radiation and temozolomide therapy (75 mg/m2) followed by maintenance temozolomide therapy (200 mg/m2) for 5 consecutive days every month. Radiation therapy was delivered at UAB in 8 patients. The remaining 5 patients were treated at different hospitals and the dose of radiation was not documented. Of the 13 patients, 8 patients received ≥12 cycles of temozolomide therapy at the time of follow-up MRI and the remaining 5 patients received ≤12 cycles of temozolomide therapy at the time of follow-up MRI. The steroid dose at the time of baseline scans and at the time of follow-up scans was not documented in the medical record in 12 of 13 patients. One patient was treated with 2 mg of dexamethasone at the baseline and 3 mg at follow-up.
Image acquisition
Post contrast gradient echo 3D T1 weighted MRI was used for brain segmentation with administration of 0.1 mmol/kg of gadoteridol (ProHance, Bracco Diagnostic Inc, Princeton, NJ). MRI was performed either on 1.5 T magnets (Echospeed, GE Medical Systems, Milwaukee, Wisconsin and Achieva, Phillips Medical System, Netherlands) or 3 T magnet (Achieva, Phillips Medical System, Netherlands). 3D fast spoiled gradient echo sequence (fSPGR) in the axial plane (TR = 16.528 ms, TE = 7.472 ms, FOV = 25 cm, slice thickness = 1.8 mm) was used in the GE magnets, high resolution sensitivity encoded T1 weighted sequence (sT1 W 3D HR SENSE) in the axial plane (TR = 25 ms, TE = 4.339 ms, FOV = 25 cm, slice thickness = 1.8 mm) was used in the 1.5 T Phillips magnet and 3D T1 turbo field echo (TFE) (TR = 15.0888 ms, TE = 4.60005 ms, FOV = 25 cm, slice thickness = 1.8 mm) was used in the 3 T Philips magnet. The image matrix size of both the control group and the bevacizumab varied from 0.79–1.86 mm3.
Image analysis
All images were processed and analyzed by an imaging scientist blinded to patient treatment history and then validated by another imaging scientist who was also blinded to the initial results as well as the treatment history. The entire brain was segmented using an automated brain segmentation tool, Object Extractor, which is supported by a commercial image processing software package, Analyze (version 11.0; Biomedical Imaging Resource, Mayo Clinic, Rochester, MN). The ipsilateral hemisphere region (tumor containing) was removed first, and then the brainstem and cerebellum remaining in the contralateral hemisphere region were excluded manually using ImageJ (version 1.48o; National Institutes of Health, Bethesda, MD). A global threshold technique was applied to deselect regions that appeared darker than grey matter, such as ventricles and fissures. 3-dimensional median filtering (7 × 7 × 7) was applied to suppress noise and to smooth out the object boundary. The brain volume was calculated as the sum of all voxels within the boundary multiplied by the unit voxel size. The lateral ventricle in the contralateral hemisphere region was segmented using a variational region-growing method [12]. The ventricular volume was segmented excluding the volume of the choroid plexus. The quality of segmentation was checked for all the images. During the validation analysis, all segmented images were compared with the original brain images, and any segmentation errors were fixed. Finally, a neuroradiologist manually reassured the quality of the segmentation.
Statistical methods
Differences in the change in absolute brain and ventricle volume and percent change in these values were analyzed with repeated measures ANOVA. Data are presented as mean ± standard deviation, and p values less than 0.05 were considered significant. To assess inter-rater agreement, we calculated intra-class correlations initial analysis and the validation analysis for each time point both for the control group and for the bevacizumab group. SAS, version 9.4 (SAS Institute Inc., Cary, NC) were used to analyze all data.
Results
Supplementary Fig. 2 demonstrates 3D volume rendered images of contralateral hemispheres and ventricles in the baseline and follow-up scans of one representative patient from the bevacizumab treated group (Fig. 2a) and one representative patient from the control group (Fig. 2b). Contralateral hemisphere volumes in the control group at the baseline and follow-up scans were 536.1 ± 50 cm3 (range 568.3–623.3 cm3) and 541 ± 46 cm3 (range 462.0–601.0 cm3) respectively. This change of volume from baseline to follow-up imaging was not statistically significant (p = 0.23). Contralateral ventricular volumes at baseline and at follow-up scans of the same patient group were 13 ± 8 cm3 (range 5.5–29.1 cm3) and 16 ± 9 cm3 (range 6.7–33.6 cm3) respectively (Supplementary Table 1). This change of volume was statistically significant (p < 0.01). In the bevacizumab treated group, the mean hemisphere volumes at the baseline and follow-up scans were 579 ± 59 cm3 (range 491.4–672.8 cm3) and 559.7 cm3 (range 409.6–668.4 cm3) respectively. The ventricular volumes at the baseline and at the follow-up scan of the same patient group were 11 ± 7 cm3 (range 3.0–26.5 cm3) and 15 ± 10 cm3 (range 4.6–34.7 cm3). There was no statistical difference in the base line contralateral hemisphere (p = 0.0678) and contralateral ventricular volume (p = 0.3878) between the patients in the control group and the bevacizumab-treated group. Supplementary Fig. 1 shows box plots of the contralateral brain hemisphere and contralateral ventricle volumes.
Bar diagram showing percentage change of volumes of contralateral hemisphere and contralateral ventricle from baseline scan to follow-up scan from the initial analysis. a Percentage change of contralateral hemisphere volume in each patient in the control group (blue bars) and in the bevacizumab group (red bars). Contralateral hemisphere volume is considered 100 % for each patient at the baseline. b Percentage change of contralateral ventricle volume in each patient in the control group (blue bars) and in the bevacizumab group (red bars). Contralateral ventricle volume is considered 100 % for each patient at the baseline
Mean absolute contralateral hemisphere volume change in the bevacizumab group was −18.3 ± 25.8 cm3. Mean absolute contralateral hemisphere volume change in the control group was 4.4 ± 13.2 cm3 (Table 2). The difference in change of absolute contralateral hemisphere volume between the two treatment groups was statistically significant (p = 0.0093). Mean absolute contralateral ventricle volume change in the bevacizumab group was (4.1 ± 4.1 cm3) compared to the control group (1.4 ± 1.7 cm3). This difference in change of ventricle volume was also statistically significant (p = 0.0388).
The percentage change of volume of the contralateral hemisphere and contralateral lateral ventricle in each patient from both the control group and the bevacizumab treated group is shown in Fig. 2 and Table 2. Mean of the percentage change of brain volume in the control group was 1 ± 0.6 % compared to −3.2 ± 1.5 % in the bevacizumab group. Mean of the percentage change of ventricle volume in the control group was 11.0 ± 2.6 % versus 33.2 ± 9 % in the bevacizumab group. The percentage changes in brain volume (p = 0.0114) and ventricle volume (p = 0.0144) between the base line scan and the follow-up scan are significantly different between bevacizumab and the control group.
The results of the validation analysis (Table 3) by the second imaging scientist were similar to the original analysis (Supplementary Table 2). At baseline contralateral hemisphere volume of the control group was 535 ± 14 cm3 and of the bevacizumab group was 578 ± 16 cm3 (p = 0.0646). At baseline contralateral ventricle volume of the control group was 14 ± 2 cm3 and of the bevacizumab group was 11 ± 2 cm3 (p = 0.3876). Percentage change of the contralateral hemisphere from baseline to follow-up MRI in the control group was 0.79 ± 0.61 % (p = 0.2061) and in the bevacizumab group was −3.4 ± 1.42 % (p = 0.0106). Percentage change of the contralateral ventricle from baseline to follow-up MRI in the control group was 10.01 ± 3.19 % and in the bevacizumab group was 40.28 ± 11.13 % (p = 0.0126). There was almost perfect agreement between the initial analysis and the validation analysis with intra-class correlation coefficient of >0.99 in all the measurements except for the measurement of the contralateral hemisphere volume measurement at follow-up that demonstrates intra-class correlation coefficient of 0.85 (Supplementary Table 3).
Discussion
VEGF is one of the key proangioangemic molecules expressed in high-grade gliomas [29, 30]. In addition to angiogenesis, recent studies have discovered that autocrine and paracrine VEGF signaling contribute to key aspects of tumorigenesis, independently of angiogenesis in high grade glioma [31, 32]. This led to the development of anti-angiogenic therapy, either VEGF- or VEGFR-targeted agents, for the treatment of high grade gliomas [33] In 2009, the US Food and Drug Administration (FDA) granted accelerated approval of bevacizumab for treatment of recurrent GBM based on two phase II trials showing improved response rates and 6-month progression-free survival compared to historical controls [21, 22]. Bevacizumab-mediated inhibition of VEGF is currently the predominant mode of anti-angiogenic therapy in high-grade gliomas and in cancers of many other body parts [33, 34]. We believe that the results of our study identifies a potential adverse event of long term bevacizumab therapy and should be validated with a large number of patients. The results of our study are particularly important to patients who have longer overall survival.
Two recently published large phase III trials aimed at determining the efficacy of first-line bevacizumab in newly diagnosed GBM show somewhat different outcomes. Radiation Therapy Oncology Group Study 0825 (RTOG8025) found no improvement in overall survival nor a significant prolongation of PFS, while the industry-sponsored AVAglio trial found improved PFS and patient-reported outcomes, but no improvement in overall survival [25, 35].
Interestingly, RTOG8025 study also incorporated assessment of neurocognitive function, and confirmed a significantly decline in neurocognitive function in the bevacizumab treated group in a large cohort of patients with appropriate control group. The authors did not propose any biologic explanation of neurocognitive decline. Neurocognitive decline in patients with GBM can be related to treatment such as radiation therapy, chemotherapy or even surgery (if medial temporal lobe or frontal lobe have been removed) or can be due to tumor infiltration of the key areas brain responsible for memory and executive functions. It is difficult to precisely identify the cause of neurocognitive decline. In the RTOG 0825 clinical trial, patients in both the control and the bevacizumab groups were treated with radiation, chemotherapy and surgery. The only difference between the two groups was use of bevacizumab versus placebo. This raises a concern if neurocognitive decline is related to bevacizumab treatment particularly with the known fact that VEGF has many critical memory functions. Our study did not include any neuropsychiatric evaluation and the relationship of neurocognitive decline and brain atrophy cannot be established from our study. As atrophy of different brain regions is strongly associated with neurocognitive decline in many neurodegenerative diseases such as Alzheimer’s dementia, frontotemporal dementia, it may be possible that bevacizumab induced brain atrophy is associated with bevacizumab induced neurocognitive decline. This hypothesis needs to be validated in a properly designed clinical trial, preferably in patients with cancers of other body parts without brain metastasis undergoing treatment with bevacizumab.
Our study demonstrates that patients who received bevacizumab had a significant decrease in brain volume and a significant increase in ventricular volume from baseline to follow-up imaging as compared to a control group patients who did not receive bevacizumab. We analyzed the volume of the contralateral hemisphere to avoid the anti-edema effect of bevacizumab and steroids that are frequently co-administered. Although there was an increase in the brain volume in the control group from baseline to follow-up imaging, the difference was not statistically significant (p = 0.23). The underlying cause of this apparent increase of the brain volume over time is not clear. This could be related to different hydration status [36], different dose of steroids [37], different image acquisition techniques or different magnets, between the baseline and follow-up scan or due to limitation in the segmentation technique.
Astrocytes are the major producers of VEGF in adult brain parenchyma [5], but VEGF is also expressed in other cells including CA1 pyramidal neurons in the hippocampus [38, 39], pyramidal neurons in the cortex [38], and Purkinje cells in the cerebellum [1, 40]. While the physiological function of VEGF in the adult brain is not well understood, recent evidence showed that VEGF is functionally important in maintaining neural stem cells, in neuroblast production and in neuronal differentiation in the hippocampus [3, 9–11] and in the subventricular zone [10–14]. It is noteworthy that all of these sites of constitutive VEGF expression are angiogenically quiescent, thus suggesting non-angiogenic roles of VEGF. Perturbation of VEGF by bevacizumab could have a direct effect on these neurogenic processes. The atrophy of the brain could be related to blockade of homeostatic functions of VEGF by bevacizumab.
The current study is limited by its retrospective nature and small sample size. The small sample size can be explained by very short overall survival of patients with recurrent high-grade gliomas and strict inclusion criteria. Only 40.25 % of the patients in the bevacizumab arm lived >1 year. Neurocognitive data and exact steroid dose in the control group were not available. Another limitation is radiation dose spills to the contralateral hemisphere could not be assessed in all the patients. In addition, we are unable to segment grey matter, white matter, or hippocampus due to poor contrast to define the region boundary. Different image acquisition protocols and different magnetic field strength might be other concerns, although the slice thickness and image resolution were comparable throughout all images. Future analysis of a larger data set with concurrent image acquisition and neurocognitive assessment will help to overcome the limitations.
In conclusion, the results of this pilot study suggest that prolonged administration of bevacizumab is associated with brain atrophy. This study sets the stage for prospective clinical trials that will include a large number of patients at many different time points, simultaneous neurocognitive assessment and regional brain volume assessment to evaluate temporal as well as regional variation of brain volume loss associated with bevacizumab therapy.
References
Maharaj AS, Saint-Geniez M, Maldonado AE, D’Amore PA (2006) Vascular endothelial growth factor localization in the adult. Am J Pathol 168:639–648
Licht T, Eavri R, Goshen I, Shlomai Y, Mizrahi A, Keshet E (2010) VEGF is required for dendritogenesis of newly born olfactory bulb interneurons. Development 137:261–271. doi:10.1242/dev.039636
Licht T, Goshen I, Avital A, Kreisel T, Zubedat S, Eavri R, Segal M, Yirmiya R, Keshet E (2011) Reversible modulations of neuronal plasticity by VEGF. Proc Natl Acad Sci U S A 108:5081–5086. doi:10.1073/pnas.1007640108
Bengoetxea H, Argandona EG, Lafuente JV (2008) Effects of visual experience on vascular endothelial growth factor expression during the postnatal development of the rat visual cortex. Cereb Cortex 18:1630–1639
Acker T, Beck H, Plate KH (2001) Cell type specific expression of vascular endothelial growth factor and angiopoietin-1 and -2 suggests an important role of astrocytes in cerebellar vascularization. Mech Dev 108:45–57
Barouk S, Hintz T, Li P, Duffy AM, MacLusky NJ, Scharfman HE (2011) 17beta-estradiol increases astrocytic vascular endothelial growth factor (VEGF) in adult female rat hippocampus. Endocrinology 152:1745–1751. doi:10.1210/en.2010-1290
Weidemann A, Kerdiles YM, Knaup KX, Rafie CA, Boutin AT, Stockmann C, Takeda N, Scadeng M, Shih AY, Haase VH, Simon MC, Kleinfeld D, Johnson RS (2009) The glial cell response is an essential component of hypoxia-induced erythropoiesis in mice. J Clin Investig 119:3373–3383. doi:10.1172/JCI39378
Licht T, Keshet E (2013) Delineating multiple functions of VEGF-A in the adult brain. Cell Mol Life Sci 70:1727–1737. doi:10.1007/s00018-013-1280-x
Cao L, Jiao X, Zuzga DS, Liu Y, Fong DM, Young D, During MJ (2004) VEGF links hippocampal activity with neurogenesis, learning and memory. Nat Genet 36:827–835
Jin K, Zhu Y, Sun Y, Mao XO, Xie L, Greenberg DA (2002) Vascular endothelial growth factor (VEGF) stimulates neurogenesis in vitro and in vivo. Proc Natl Acad Sci U S A 99:11946–11950
Schanzer A, Wachs FP, Wilhelm D, Acker T, Cooper-Kuhn C, Beck H, Winkler J, Aigner L, Plate KH, Kuhn HG (2004) Direct stimulation of adult neural stem cells in vitro and neurogenesis in vivo by vascular endothelial growth factor. Brain Pathol 14:237–248
Gao P, Shen F, Gabriel RA, Law D, Yang E, Yang GY, Young WL, Su H (2009) Attenuation of brain response to vascular endothelial growth factor-mediated angiogenesis and neurogenesis in aged mice. Stroke 40:3596–3600. doi:10.1161/STROKEAHA.109.561050
Louissaint A Jr, Rao S, Leventhal C, Goldman SA (2002) Coordinated interaction of neurogenesis and angiogenesis in the adult songbird brain. Neuron 34:945–960
Wang Y, Jin K, Mao XO, Xie L, Banwait S, Marti HH, Greenberg DA (2007) VEGF-overexpressing transgenic mice show enhanced post-ischemic neurogenesis and neuromigration. J Neurosci Res 85:740–747
Adamcio B, Sperling S, Hagemeyer N, Walkinshaw G, Ehrenreich H (2010) Hypoxia inducible factor stabilization leads to lasting improvement of hippocampal memory in healthy mice. Behav Brain Res 208:80–84. doi:10.1016/j.bbr.2009.11.010
Ferrara N, Gerber HP, LeCouter J (2003) The biology of VEGF and its receptors. Nat Med 9:669–676
Sundberg C, Nagy JA, Brown LF, Feng D, Eckelhoefer IA, Manseau EJ, Dvorak AM, Dvorak HF (2001) Glomeruloid microvascular proliferation follows adenoviral vascular permeability factor/vascular endothelial growth factor-164 gene delivery. Am J Pathol 158:1145–1160
van Bruggen N, Thibodeaux H, Palmer JT, Lee WP, Fu L, Cairns B, Tumas D, Gerlai R, Williams SP, van Lookeren Campagne M, Ferrara N (1999) VEGF antagonism reduces edema formation and tissue damage after ischemia/reperfusion injury in the mouse brain. J Clin Investig 104:1613–1620
Salmaggi A, Eoli M, Frigerio S, Silvani A, Gelati M, Corsini E, Broggi G, Boiardi A (2003) Intracavitary VEGF, bFGF, IL-8, IL-12 levels in primary and recurrent malignant glioma. J Neurooncol 62:297–303
Schmidt NO, Westphal M, Hagel C, Ergun S, Stavrou D, Rosen EM, Lamszus K (1999) Levels of vascular endothelial growth factor, hepatocyte growth factor/scatter factor and basic fibroblast growth factor in human gliomas and their relation to angiogenesis. Int J Cancer 84:10–18
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, Paleologos N, Nicholas MK, Jensen R, Vredenburgh J, Huang J, Zheng M, Cloughesy T (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27:4733–4740. doi:10.1200/JCO.2008.19.8721
Kreisl TN, Kim L, Moore K, Duic P, Royce C, Stroud I, Garren N, Mackey M, Butman JA, Camphausen K, Park J, Albert PS, Fine HA (2009) Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol 27:740–745. doi:10.1200/JCO.2008.16.3055
Lu KV, Chang JP, Parachoniak CA, Pandika MM, Aghi MK, Meyronet D, Isachenko N, Fouse SD, Phillips JJ, Cheresh DA, Park M, Bergers G (2012) VEGF inhibits tumor cell invasion and mesenchymal transition through a MET/VEGFR2 complex. Cancer Cell 22:21–35. doi:10.1016/j.ccr.2012.05.037
Soda Y, Myskiw C, Rommel A, Verma IM (2013) Mechanisms of neovascularization and resistance to anti-angiogenic therapies in glioblastoma multiforme. J Mol Med 91:439–448. doi:10.1007/s00109-013-1019-z
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, Colman H, Chakravarti A, Pugh S, Won M, Jeraj R, Brown PD, Jaeckle KA, Schiff D, Stieber VW, Brachman DG, Werner-Wasik M, Tremont-Lukats IW, Sulman EP, Aldape KD, Curran WJ Jr, Mehta MP (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Eng J Med 370:699–708. doi:10.1056/NEJMoa1308573
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for R, Treatment of Cancer Brain T, Radiotherapy G, National Cancer Institute of Canada Clinical Trials G (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Eng J Med 352:987–996. doi:10.1056/NEJMoa043330
Kleihues PBP, Aldape Kd et al (2007) WHO classification of tumors of the central nervous system. IARC Press, Lyon
Bag AK, Cezayirli PC, Davenport JJ, Gaddikeri S, Fathallah-Shaykh HM, Cantor A, Han XS, Nabors LB (2014) Survival analysis in patients with newly diagnosed primary glioblastoma multiforme using pre- and post-treatment peritumoral perfusion imaging parameters. J Neurooncol 120:361–370. doi:10.1007/s11060-014-1560-9
Linkous AG, Yazlovitskaya EM (2011) Angiogenesis in glioblastoma multiforme: navigating the maze. Anticancer Agents Med Chem 11:712–718
Jain RK, di Tomaso E, Duda DG, Loeffler JS, Sorensen AG, Batchelor TT (2007) Angiogenesis in brain tumours. Nat Rev Neurosci 8:610–622
Knizetova P, Ehrmann J, Hlobilkova A, Vancova I, Kalita O, Kolar Z, Bartek J (2008) Autocrine regulation of glioblastoma cell cycle progression, viability and radioresistance through the VEGF-VEGFR2 (KDR) interplay. Cell Cycle 7:2553–2561
Hoelzinger DB, Demuth T, Berens ME (2007) Autocrine factors that sustain glioma invasion and paracrine biology in the brain microenvironment. J Natl Cancer Inst 99:1583–1593
Welti J, Loges S, Dimmeler S, Carmeliet P (2013) Recent molecular discoveries in angiogenesis and antiangiogenic therapies in cancer. J Clin Ivestig 123:3190–3200. doi:10.1172/JCI70212
Goel HL, Mercurio AM (2013) VEGF targets the tumour cell. Nat Rev Cancer 13:871–882. doi:10.1038/nrc3627
Chinot OL, Wick W, Mason W, Henriksson R, Saran F, Nishikawa R, Carpentier AF, Hoang-Xuan K, Kavan P, Cernea D, Brandes AA, Hilton M, Abrey L, Cloughesy T (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Eng J Med 370:709–722. doi:10.1056/NEJMoa1308345
Duning T, Kloska S, Steinstrater O, Kugel H, Heindel W, Knecht S (2005) Dehydration confounds the assessment of brain atrophy. Neurology 64:548–550. doi:10.1212/01.WNL.0000150542.16969.CC
Rao AB, Richert N, Howard T, Lewis BK, Bash CN, McFarland HF, Frank JA (2002) Methylprednisolone effect on brain volume and enhancing lesions in MS before and during IFNbeta-1b. Neurology 59:688–694
Li SF, Sun YB, Meng QH, Li SR, Yao WC, Hu GJ, Li ZJ, Wang RZ (2009) Recombinant adeno-associated virus serotype 1-vascular endothelial growth factor promotes neurogenesis and neuromigration in the subventricular zone and rescues neuronal function in ischemic rats. Neurosurgery 65:771–779. doi:10.1227/01.NEU.0000349931.61771.52
Kim BW, Choi M, Kim YS, Park H, Lee HR, Yun CO, Kim EJ, Choi JS, Kim S, Rhim H, Kaang BK, Son H (2008) Vascular endothelial growth factor (VEGF) signaling regulates hippocampal neurons by elevation of intracellular calcium and activation of calcium/calmodulin protein kinase II and mammalian target of rapamycin. Cell Signal 20:714–725. doi:10.1016/j.cellsig.2007.12.009
Ruiz de Almodovar C, Coulon C, Salin PA, Knevels E, Chounlamountri N, Poesen K, Hermans K, Lambrechts D, Van Geyte K, Dhondt J, Dresselaers T, Renaud J, Aragones J, Zacchigna S, Geudens I, Gall D, Stroobants S, Mutin M, Dassonville K, Storkebaum E, Jordan BF, Eriksson U, Moons L, D’Hooge R, Haigh JJ, Belin MF, Schiffmann S, Van Hecke P, Gallez B, Vinckier S, Chedotal A, Honnorat J, Thomasset N, Carmeliet P, Meissirel C (2010) Matrix-binding vascular endothelial growth factor (VEGF) isoforms guide granule cell migration in the cerebellum via VEGF receptor Flk1. J Neurosci 30:15052–15066. doi:10.1523/JNEUROSCI.0477-10.2010
Conflict of interests
AKB: Consultant to Dotarem Advisory board. Guerbet LLc. HK: No disclosure. YG: No disclosure. MB: No disclosure. PPW: No disclosure. HMF: No disclosure. DG: No disclosure. JMM: Leadership role, Stocks, Consultancy, Intellectual property and Research Funding: Catherex Inc. & Aettis Inc.; Research funding: ICT. JF: Research funding: Varian Oncology. TMB: No disclosure. AK: No disclosure. GKF: No disclosure. PRC: No disclosure. LBN: Consultant, Merck Inc.; Travel allowance: BMS. XH: No disclosure.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
11060_2015_1751_MOESM3_ESM.tiff
Box plots showing contralateral hemisphere and ventricle volumes from the initial analysis. (A, B) Contralateral hemisphere volumes at baseline and follow-up scans of patients treated with (A) combination of bevacizumab and standard of the care (labeled as Bevacizumab) or (B) only standard of the care (labeled as control). (C, D) Contralateral ventricle volumes at baseline and follow-up scans of patients treated with (A) combination of bevacizumab and standard of the care or (B) only standard of the care. Supplementary material 3 (TIFF 332 kb)
11060_2015_1751_MOESM2_ESM.tiff
3D volume renderings of contralateral hemisphere and ventricle at baseline and follow-up scans of two representative patients treated with (A) combination of bevacizumab and standard of the care (labeled as Bevacizumab) and (B) only standard of the care (labeled as Control). Same size scale was applied for all hemispheres (or ventricles). This image is from the initial analysis. Supplementary material 2 (TIFF 428 kb)
Rights and permissions
About this article
Cite this article
Bag, A.K., Kim, H., Gao, Y. et al. Prolonged treatment with bevacizumab is associated with brain atrophy: a pilot study in patients with high-grade gliomas. J Neurooncol 122, 585–593 (2015). https://doi.org/10.1007/s11060-015-1751-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1751-z