Abstract
Choroid plexus carcinoma (CPCs) is a rare, malignant, primary brain tumor with a poor prognosis. Currently, there is no consensus on the use of adjuvant therapy, and few large-scale studies focus exclusively on the pediatric population. We performed a comprehensive systematic review of pediatric CPCs to determine the effects of various adjuvant therapy modalities on overall survival (OS). A literature search was performed to identify studies reporting children with CPC who underwent surgical resection. Only patients who had clearly received adjuvant therapy, or were described as not selected for adjuvant therapy were analyzed in our comparison groups. Kaplan–Meier and multivariate Cox regression survival analyses were performed to determine the effects of different types of adjuvant therapies on OS. A total of 135 children (age ≤ 18 years) with CPC who had known adjuvant therapy status and OS were identified from 53 articles. Kaplan–Meier analysis showed that while adjuvant therapy overall improved OS (p = 0.001), different modes of adjuvant therapies had varying effects on OS (p = 0.034). Specifically, combined chemo-radiotherapy as well as chemotherapy alone improved OS (p = 0.001), but radiation did not (p = 0.129). Multivariate Cox proportional hazard model adjusting for confounding factors showed that combined therapy was associated with better OS compared to chemotherapy alone (HR: 0.291, p = 0.027). Both chemotherapy alone and combined chemo-radiation improved OS independent of age, gender, tumor location and extent of resection, while radiation alone did not.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Choroid plexus carcinoma (CPC) is a rare, malignant primary brain tumor with a poor prognosis. It is classified by the World Health Organization (WHO) as a grade III neoplasm, and the 5-year survival rate for patients is approximately 40 % [1, 2]. There are a few factors that have been shown to affect overall survival (OS) for patients with CPC, including extent of resection (EOR) and use of adjuvant therapy in addition to surgery [3–6]. However, there is currently no standard of care with regard to the use or choice of adjuvant therapy. While some evidence suggests that chemotherapy and radiation may independently increase survival [4, 6], little data exist that compare the relative survival benefits of these two modalities. More importantly, there is limited evidence on whether combined chemotherapy and radiation provides additional survival benefit compared to any single modality adjuvant therapy. Finally, the rarity of this tumor makes it difficult to conduct randomized clinical trials in this patient population.
There have been very few systematic studies purely focused on children, despite a higher incidence in this group than in adults [7]. The treatment for childhood tumors differs substantially from adults, primarily due to the impact of adjuvant therapy on development and long-term effects such as endocrinopathies and cognitive deficits [8, 9]. Additionally, it remains unclear whether any of the known prognostic factors are applicable to the pediatric population. Although not a substitute for class I data, information obtained from systematic literature reviews, or large institutional series, can help in guiding treatment decisions by describing current treatment options and possible clinical outcomes obtained with those treatments. We therefore performed a systematic review of literature in pediatric CPC patients to study not only the relative benefit of chemotherapy and radiation on OS, but also whether combined chemotherapy and radiation is the best adjuvant modality for extending OS.
Methods
Article selection
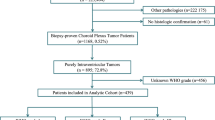
A comprehensive systematic review of the English-language literature was performed. An initial online search of the PubMed database using the key word “choroid plexus carcinoma” resulted in 409 articles published until December 2011. Only articles published since 1980 were then included, when microsurgical techniques and use of CT imaging in the management of brain tumors became more widespread. All manuscripts were individually reviewed to identify CPC patients with confirmed diagnosis and available individual clinical information. Pediatric patients were defined as those 18 years of age and under at the time of diagnosis. Cases published as aggregated data sets, where individual patient data were grouped, were omitted and not included in this analysis. The database was reviewed for redundancies and potential overlapping reports to ensure no single patient was represent twice in the database. We identified a final set of 53 articles with a total of 135 patients who met the inclusion criteria. An integrative analysis was performed, where individual patient data from studies were pooled and statistically analyzed.
Data extraction
Data from case reports and institutional series were extracted with the following information: age, gender, EOR (GTR vs. STR), adjuvant radiotherapy, adjuvant chemotherapy, mortality, time to mortality, tumor location (supratentorial including: lateral ventricle, third ventricle, supratentorial cerebral; infratentorial including: fourth ventricle, cerebellopontine angle, cerebellum), and duration of follow-up. All mean values were presented with standard error of mean (SEM).
Statistical analysis
Survival analyses of OS were analyzed via Kaplan–Meier curves and differences assessed by log-rank test. Multivariate Cox proportional hazards models were fitted by backward stepwise model selection while accounting for potentially confounding variables, including: gender, age, EOR, tumor location, adjuvant therapy (radiation, chemotherapy or both). Lower hazard ratios represent improved OS. Means of continuous variable were analyzed using t tests and ANOVA, and categorical values were analyzed using the Pearson’s Chi square test. Fisher’s exact test was used if the expected cell count in a contingency table was <5. p values less than 0.05 were considered statistically significant. Analyses were performed using the statistical software package SPSS 20 (IBM Inc.).
Results
Patient demographics
Disaggregated clinical information obtained from 53 articles resulted in an overall cohort of 135 patients with a diagnosis of CPC who were less than or equal to 18 years of age, and in whom both the status of adjuvant therapy use and OS information were known. Due to the rarity of the disease, the majority of the articles were case reports. The total number of patients included in each article ranged from 1 to 21 (Fig. 1a). The mean and median ages of patients were 3.38 and 1.67 years, respectively, and age ranged from 1 week old to 18 years of age. The age distribution of this cohort showed that the vast majority of CPCs occur in very young children, with a distribution skewed to the right (Fig. 1b). When this population was divided into quartiles by age, 25 % of patients were 9 months or younger, 50 % of patients were 20 months or younger, and 75 % of patients were 4 years or younger. The mean follow-up time was 32 months, and follow-up time ranged from 1 to 238 months. Only 17 % of patients had follow-up less than 6 months, and those corresponded mostly with patients who had OS less than 6 months.
Patient demographics. a Distribution of the number of CPC patients contained in each article. Most articles contained 1 patient, with fewer articles containing 2–5, 6–10, and more than 10 patients, with an overall range of 1–21 patients. b Distribution of CPC patients by age. The mean age of diagnosis for these 135 patients was 3.38 years, with a standard deviation of 4.09 years. c The percentages of patients either younger or older than 3 years of age with known status of use of radiotherapy were compared by Chi square test (p = 0.113). Many providers are reluctant to recommend radiation for patients younger than 3 due to concerns of neurological sequelae
There were 110 patients who received adjuvant therapy and 25 who did not. Mean age, gender, and tumor location did not differ between those who did and did not receive adjuvant therapy, while EOR was significantly different (p = 0.037) (Table 1). There were proportionally more patients who had STR among those who received no adjuvant therapy compared to those who did (Table 1).
For more detailed statistical analyses involving adjuvant therapy, we categorized the type of adjuvant therapy that the patients received, including the option of not receiving adjuvant therapy, into the following 4 groups: no adjuvant therapy, chemotherapy only, radiation only, and combined chemotherapy and radiation. There were no significant differences between these 4 groups in terms of male to female ratio (p = 0.919), EOR (p = 0.059), and supratentorial or infratentorial location (p = 0.705) (Table 2). Notably, there was a trend toward greater number of patients receiving chemotherapy after GTR compared to STR, even though this difference was not statistically significant (p = 0.059). There were also significant differences in mean ages between the different adjuvant therapy groups (p = 0.038) (Table 2). Those receiving combined chemotherapy and radiation had the highest mean age of 5.03, radiation only was the second highest at 3.57, followed by no adjuvant at 2.96 and chemotherapy only the lowest at 2.52 years (Table 2). Due to avoidance of radiation-related adverse events in very young children, patients younger than 3 years old were less likely to have received radiation compared to older patients (Fig. 1c), although this difference was not statistically significant (p = 0.113). Because of these differences, gender, age, tumor location, and EOR were all incorporated into the multivariate Cox regression analyses testing the effect of adjuvant therapy use on survival.
Adjuvant therapies have differential effects on overall survival
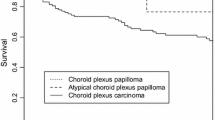
First, we found that the use of adjuvant therapy overall was associated with better OS, as expected, in a Kaplan–Meier analysis comparing those who did to those who did not receive any adjuvant therapy (p = 0.001) (Fig. 2a). To control for potential confounding effects of gender, age, tumor location (supratentorial vs. infratentorial), and EOR (GTR vs. STR), we performed a multivariate Cox regression analysis and found that the use of adjuvant therapy independently improved survival with a hazard ratio of 0.414 (95 % CI: 0.216–0.796, p = 0.008). We also performed a subgroup analysis using multivariate cox regression (controlling for gender, age, and tumor location) on those who had STR, and found that adjuvant therapy independently improved survival with a hazard ratio of 0.262 (95 % CI: 0.129–0.533, p < 0.001). However, we were unable to perform a similar subgroup analysis on the GTR group, due to a combination of the number of instances of censoring and smaller sample size that resulted in the lack of a true cox regression model.
Differential effects of adjuvant therapies on overall survival. a Kaplan–Meier analysis shows that adjuvant therapy improves OS (p = 0.001). b Kaplan–Meier analysis shows a statistically significant difference in OS between groups receiving either radiation, chemotherapy or both. c Different modes of adjuvant therapies are associated with varying degrees of benefit for extending OS. The trends in Kaplan–Meier analysis were confirmed by multivariate Cox regression analysis (Table 4)
Given that the mode of adjuvant therapy received differed by whether radiation, chemotherapy or both were received, we next investigated whether there were differences in survival between groups based on the specific adjuvant therapy. Kaplan–Meier analysis showed a significant difference in OS between the adjuvant groups (p = 0.034) (Fig. 2b), suggesting that specific modes of adjuvant therapies may have differential effects on OS.
To further investigate the specific effects of each mode of adjuvant therapy on OS, we first performed Kaplan–Meier survival analyses to test whether each adjuvant therapy option was individually associated with improved OS compared to not receiving adjuvant. While both combined therapy and chemotherapy alone significantly improved OS compared to those not receiving adjuvant therapy (logrank test, p = 0.001 for both), radiation alone did not (p = 0.429) (Table 3, Left). These effects could be observed from the trends in survival curves of the Kaplan–Meier analysis (Fig. 2c).
Multivariate Cox-Regression model confirmed the Kaplan–Meier findings. Both combined therapy (p = 0.001) and chemotherapy alone (p = 0.048) each independently improved OS, with hazard ratios of 0.144 and 0.492, respectively (Table 3, Right). Radiation alone, on the other hand, did not significantly improve OS (p = 0.735). The results from the multivariate analyses were therefore consistent with univariate Kaplan–Meier analyses and suggested that both chemotherapy and combined therapy could increase OS.
Combined therapy may have additional overall survival benefit over chemotherapy alone
While both chemotherapy and combined therapy may have increased OS, the hazard ratio for OS associated with combined therapy was lower than chemotherapy alone, raising the possibility that the survival benefit of combined therapies may be greater than chemotherapy alone. To investigate whether there was an additional survival benefit when combined with radiation and whether combined therapy was associated with the greatest survival benefit, we directly compared it to the chemotherapy only group using multivariate Cox regression while restricting the data analyzed to only those two groups. Combined therapy had a hazard ratio of 0.291 (p = 0.027, CI: 0.097–0.868) (Table 4) compared to chemotherapy alone.
Discussion
Although adjuvant therapy for CPC has been used by many groups and described in many reports, the relative benefits of chemotherapy, radiation, and combination therapy have not been well studied. In addition, the rarity of this tumor type precludes the feasibility of large, randomized studies. Consequently, the choice of adjuvant therapy remains controversial because no specific adjuvant regimen has been clearly demonstrated to exhibit superiority to others. Reports from institutional series vary widely with respect to usage and efficacy of each modality [2, 10–19]. One such controversy is whether chemotherapy is indicated in children with CPC after gross-total resection [6]. The use of radiation, especially in pediatric patients, is also problematic when weighing the potential benefits against long-term risks associated with radiation. Moreover, meta-analyses published to date have not addressed whether chemotherapy or radiation is better for extending OS, and whether combined therapies might be superior to both of these single modalities. This is particularly problematic in the pediatric population, given the known significant side effects of both chemotherapy and radiation.
We therefore performed a comprehensive review of literature by performing an integrative analysis (in which the previously reported individual cases are pooled and analyzed) to determine whether the most aggressive adjuvant treatment modality, using combined chemotherapy and radiation, provides significantly greater benefit compared to single modality adjuvant therapy among pediatric CPC patients. Validating previous findings, we first found that adjuvant therapy overall improved survival independent of other factors such as age, gender, tumor location, and EOR. Specifically, our data validated a commonly held belief among clinicians that those who have had STR would benefit from adjuvant therapy. On the other hand, we do not have strong data (in the form of a true subgroup analysis) to suggest GTR patients specifically benefit from adjuvant therapy, nor that one should not administer adjuvant therapy simply because GTR was achieved. At this point, our data supporting the use of adjuvant therapy come from the multivariate analysis that corrects for EOR suggesting adjuvant therapy may have an effect regardless of EOR.
Secondly, our results validated previous findings that chemotherapy is independently associated with better OS [6]. However, unlike results from previous studies, our analysis shows that radiation alone is not independently associated with significantly better OS [4]. While previous studies did find a survival benefit associated with radiation [3, 4], they did not exclude those who also received chemotherapy in addition to radiation when evaluating the benefits of radiation. In view of our data showing that chemotherapy alone provided survival benefit, it is possible that the inclusion of those receiving both radiation and chemotherapy when assessing the effects of radiation could have confounded previous findings. Therefore we investigated whether the combination of chemotherapy and radiation provides the greatest OS, even after adjusting for EOR, age, gender, and tumor location. While the multivariate Cox regression showed a significant additional OS benefit, it was nevertheless an unexpected result given that the Kaplan–Meier curves for OS did not differ significantly between the two groups. This apparent discrepancy between the results from Cox regression and Kaplan–Meier analysis may be due to the possibility that other variables in the multivariate analysis have significantly modified the effects of adjuvant therapy alone on OS. While our data does not overwhelmingly favor a conclusion that combined adjuvant therapy is strictly superior for OS, it does suggest that for some patients, when taking into account other clinically important factors, giving both chemotherapy and radiation may be the best option if the side effects can be tolerated.
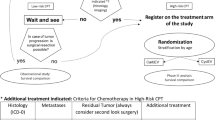
One potential concern regarding the use of radiation is the possibility of neurocognitive impairment due to its direct effects on the developing brain of young children [20–23]. Because neurogenesis is known to be particularly sensitive to radiation [22, 23] and is likely to be affected to a greater degree in very young children, many providers avoid radiation in this age group. As an example, children under the age of 3 are not given radiation in the ongoing European clinical trial on choroid plexus tumors [24]. Therefore, we also performed an additional multivariate Cox regression analysis adjusting for age as a dichotomous categorical variable (<3 vs. >3 years) to evaluate whether the age group a pediatric patient was in could influence the efficacy of combined therapy. The results showed that combined therapy was still significantly associated with a hazard ratio of less than 1 compared to chemotherapy, regardless of age group, suggesting that perhaps pediatric patients of all ages potentially could benefit from combined therapy (data not shown). We recognize that a subgroup analysis of only patients under the age of 3 may more directly address the question of whether combined therapy could specifically benefit patients under the age of 3 who were most prone to the adverse effects of radiation, but the statistics did not reach significance due to insufficient sample size (data not shown). Clearly, more definitive evidence is needed before a strong recommendation could be made for patients under the age of 3 to receive combined therapy.
Even though we limited our database to include only cases with disaggregated clinical information, we believe that there is strong external validity. For example, estimated 5-year survivals based on our Kaplan–Meier analysis (Supplemental Fig. 1) were similar to previously reported rates at 46.4 ± 6.1 % (one standard deviation) and 27.6 ± 4.8 % for those who received chemotherapy and those who did not receive chemotherapy, respectively [6].
There are many limitations inherent to the design of this study. We recognize that a systematic review of literature cannot equal the quality of data obtained from a prospective randomized study. Many of the limitations associated with retrospective study design are applicable in this study. First, because the data were not prospectively collected, many of the potential confounders could not be assessed due to lack of data availability in the reported literature. Specifically, pre-operative KPS, tumor size, tumor locations that prevented GTR, and goals of therapy were not assessed and factored in our multivariate analysis. Because in many instances the goals of therapy, including the specific adjuvant modality as well as dose and duration of chemotherapy were not specifically mentioned, we were unable to perform an “intent-to-treat” analysis. Therefore, a potential bias could result from assigning patients, who otherwise would have received adjuvant therapy, into the group that did not receive adjuvant therapy cause they were too sick to receive adjuvant therapy. While we were able to control for EOR in our multivariate analyses, we noticed that greater proportion of patients received adjuvant therapy (p = 0.037) after GTR, and that there was a trend toward greater use of chemotherapy (p = 0.059). While it is not clear why fewer patients after STR received adjuvant therapy, perhaps specifically chemotherapy, this could either be a reflection of historical institutional practices or that some patients who received STR were also too sick to receive chemotherapy. While it would be difficult to control for the overall health of these patients in a retrospective study, we acknowledge that this could be a potential source of bias.
Because this was not a prospective randomized controlled trial, the specific chemotherapy regimen used for patients varied. Unfortunately, we were unable to ascertain the specific chemotherapy regimen that had the greatest effect on survival. We also lacked information on the specific modalities of radiation used, which included both focal and craniospinal radiation. Additionally, long-term neurocognitive outcome of these patients were generally not reported, and therefore we were unable to ascertain the long-term adverse effects of radiation and chemotherapy on the pediatric CPC patients. Future studies, preferably done in a prospective manner, should therefore investigate both the effectiveness of particular chemotherapy regimens and modalities of radiation, as well as their long-term neurocognitive effects.
Given the rarity of this disease contributing to the lack of available data from prospective studies, our systematic analysis of literature provides the best current evidence. Moreover, considering the results of this study, randomization to either of the 4 adjuvant groups defined in this study would seem rather unethical and therefore difficult to justify. Because aggregated patient data (where individual patient data are grouped) were not used in this study in order to perform survival analyses, our results could be biased by individual case reports or smaller studies presented by institutions with relatively less experience in treating patients with CPC. However, even though we excluded studies that did not report individual patient data, a number of publications used in our study still contained cohorts of more than 15 patients from institutions with significant experience with CPC surgery.
From a statistical analysis standpoint, the benefit of using only disaggregated data is the ability to perform survival analyses such as Kaplan–Meier and Cox regression based on time-dependent data points, rather than being limited to logistic regression methods that often introduce additional bias because of binary data at fixed time points contained in aggregated data reports. Thus, even though we excluded some CPC cases that are presented as aggregated data, we are nevertheless able to perform robust statistical analysis as a result.
In summary, our results indicate that both chemotherapy and combined adjuvant therapy may independently extend the OS of pediatric CPC patients, when taking into account the EOR, age, and tumor location. More studies are needed before combined chemotherapy and radiation is deemed strictly superior to single modality adjuvant therapy. Given that younger children may not be suitable for radiation, chemotherapy alone is recommended if they can tolerate it.
Conclusion
Our results indicate that while chemotherapy alone may independently prolong OS of pediatric CPC patients, combined chemotherapy and radiation may have the further impact on OS for some patients when other clinical factors are taken into account. Given that younger children may not be suitable for radiation, chemotherapy as the only adjuvant may still be a viable option for significantly extending survival.
Abbreviations
- CPC:
-
Choroid plexus carcinoma
- OS:
-
Overall survival
- EOR:
-
Extent of resection
References
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds) (2007) WHO classification of tumours of the central nervous system. International Agency for Research on Cancer, Lyon
Berger C, Thiesse P, Lellouch-Tubiana A, Kalifa C, Pierre-Kahn A, Bouffet E (1998) Choroid plexus carcinomas in childhood: clinical features and prognostic factors. Neurosurgery 42:470–475
Wolff JE, Sajedi M, Brant R, Coppes MJ, Egeler RM (2002) Choroid plexus tumours. Br J Cancer 87:1086–1091. doi:10.1038/sj.bjc.6600609
Wolff JE, Sajedi M, Coppes MJ, Anderson RA, Egeler RM (1999) Radiation therapy and survival in choroid plexus carcinoma. Lancet 353:2126
Wrede B, Liu P, Ater J, Wolff JE (2005) Second surgery and the prognosis of choroid plexus carcinoma–results of a meta-analysis of individual cases. Anticancer Res 25:4429–4433
Wrede B, Liu P, Wolff JE (2007) Chemotherapy improves the survival of patients with choroid plexus carcinoma: a meta-analysis of individual cases with choroid plexus tumors. J Neurooncol 85:345–351. doi:10.1007/s11060-007-9428-x
Fitzpatrick LK, Aronson LJ, Cohen KJ (2002) Is there a requirement for adjuvant therapy for choroid plexus carcinoma that has been completely resected? J Neurooncol 57:123–126
Ogiwara H, Dipatri AJ, Alden TD, Bowman RM, Tomita T (2011) Choroid plexus tumors in pediatric patients. Br J Neurosurg. doi:10.3109/02688697.2011.601820
Packer RJ, Perilongo G, Johnson D, Sutton LN, Vezina G, Zimmerman RA, Ryan J, Reaman G, Schut L (1992) Choroid plexus carcinoma of childhood. Cancer 69:580–585
Allen J, Wisoff J, Helson L, Pearce J, Arenson E (1992) Choroid plexus carcinoma–responses to chemotherapy alone in newly diagnosed young children. J Neurooncol 12:69–74
Due-Tonnessen B, Helseth E, Skullerud K, Lundar T (2001) Choroid plexus tumors in children and young adults: report of 16 consecutive cases. Childs Nerv Syst 17:252–256
Geerts Y, Gabreëls F, Lippens R, Merx H, Wesseling P (1996) Choroid plexus carcinoma: a report of two cases and review of the literature. Neuropediatrics 27:143–148. doi:10.1055/s-2007-973765
Kang HS, Wang KC, Kim YM, Kim IO, Kim SK, Chi JG, Cho BK (1997) Choroid plexus carcinoma in an infant. J Korean Med Sci 12:162–167
Kumabe T, Tominaga T, Kondo T, Yoshimoto T, Kayama T (1996) Intraoperative radiation therapy and chemotherapy for huge choroid plexus carcinoma in an infant–case report. Neurol Med Chir (Tokyo) 36:179–184
Meyers SP, Khademian ZP, Chuang SH, Pollack IF, Korones DN, Zimmerman RA (2004) Choroid plexus carcinomas in children: mRI features and patient outcomes. Neuroradiology 46:770–780. doi:10.1007/s00234-004-1238-7
Paulus W, Janisch W (1990) Clinicopathologic correlations in epithelial choroid plexus neoplasms: a study of 52 cases. Acta Neuropathol 80:635–641
Pierga JY, Kalifa C, Terrier-Lacombe MJ, Habrand JL, Lemerle J (1993) Carcinoma of the choroid plexus: a pediatric experience. Med Pediatr Oncol 21:480–487
Shinoda J, Kawaguchi M, Matsuhisa T, Deguchi K, Sakai N (1998) Choroid plexus carcinoma in infants: report of two cases and review of the literature. Acta Neurochir (Wien) 140:557–563
Strojan P, Popovic M, Surlan K, Jereb B (2004) Choroid plexus tumors: a review of 28-year experience. Neoplasma 51:306–312
Donahue B (1992) Short- and long-term complications of radiation therapy for pediatric brain tumors. Pediatr Neurosurg 18:207–217
Wara WM, Sheline GE (1978) Radiation therapy of malignant brain tumors. Clin Neurosurg 25:397–402
Burrell K, Hill RP, Zadeh G (2012) High-resolution in vivo analysis of normal brain response to cranial irradiation. PLoS One 7:e38366. doi:10.1371/journal.pone.0038366
Blomstrand M, Brodin NP, Munck Af, Rosenschold P, Vogelius IR, Sanchez Merino G, Kiil-Berthlesen A, Blomgren K, Lannering B, Bentzen SM, Bjork-Eriksson T (2012) Estimated clinical benefit of protecting neurogenesis in the developing brain during radiation therapy for pediatric medulloblastoma. Neuro Oncol 14:882–889. doi:10.1093/neuonc/nos120
Wrede B, Hasselblatt M, Peters O, Thall PF, Kutluk T, Moghrabi A, Mahajan A, Rutkowski S, Diez B, Wang X, Pietsch T, Kortmann RD, Paulus W, Jeibmann A, Wolff JE (2009) Atypical choroid plexus papilloma: clinical experience in the CPT-SIOP-2000 study. J Neurooncol 95:383–392. doi:10.1007/s11060-009-9936-y
Acknowledgments
None.
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Funding
M.Z. Sun is a Howard Hughes Medical Institute Medical Research Fellow. M. Safaee was supported by a grant from the Doris Duke Charitable Foundation. Dr. Oh received a National Research Service Award from the National Institutes of Health (F32NS073326-01). Dr. Ivan is funded by the National Research Education Foundation through the American Association of Neurological Surgeons. Dr. Parsa is currently the Michael J. Marchese Professor and Chair at Northwestern University, Feinberg School of Medicine.
Author information
Authors and Affiliations
Corresponding author
Additional information
Michael E. Ivan and Michael C. Oh have contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sun, M.Z., Ivan, M.E., Oh, M.C. et al. Effects of adjuvant chemotherapy and radiation on overall survival in children with choroid plexus carcinoma. J Neurooncol 120, 353–360 (2014). https://doi.org/10.1007/s11060-014-1559-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-014-1559-2