Abstract
Introduction
Choroid plexus tumors (CPTs) represent one of the most common intraventricular tumors. Although most are benign, they often reach considerable sizes before clinical manifestation, challenging their surgical management. We aim to describe the clinical characteristics and the impact of current management on the survival of patients harboring intraventricular CPT.
Methods
The National Cancer Database (NCDB) was queried to identify biopsy-proven intraventricular CPT patients (2004–2015). Demographic and patterns of care were described, the log-rank method was used to independently analyze survival according to age, WHO grade and extent of resection (EOR). Multivariate analysis was performed to investigate the impact of prognostic factors on overall survival (OS).
Results
A total of 439 CPT patients with known WHO grade were included. WHO grade I tumors were more frequent in adults, while WHO grade III tumors were more common in pediatric population. Most CPTs were benign, with a median tumor size of 3–4 cm. Mean tumor size in pediatric population was greater than in adult population (4.39 cm vs. 2.7 cm; p < 0.01). Frequency was similar between males and females (51.7% vs. 48.3%; p > 0.0.5). Five- and ten-year OS among all patients was 87% and 84%, respectively. EOR was not associated with survival for any WHO grade. On multivariable analysis, only patient age (p = 0.022), WHO grade (p = 0.003) and medical comorbidity scores (p = 0.002) were independently associated with OS after diagnosis.
Conclusion
Patients with CPTs present at different stages of life, with sizable tumor burden and distinct WHO grade prevalence. Considering their favorable survival, efforts to improve tumor control should be meticulously weighed against the long-term risk associated with surgery, radiation, and chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Choroid plexus tumors (CPTs) are rare primary intracranial tumors, comprising < 1% of all brain neoplasms. CPTs are almost entirely located in the ventricle system, where they represent one of the most common neoplasms, especially in younger pediatric population [1, 2]. It has been previously described that the majority of CPTs occur predominantly in children and infants, being diagnosed within the first decade of life in 74% of cases. The average annual incidence for all CPTs is as low as 0.3 out of 1,000,000 per year, which may be related to the scattered number of reports about their management and outcomes [3,4,5,6].
CPTs arise from the differentiated epithelial tissue of the choroid plexus. The spectrum of CPTs includes WHO grade I choroid plexus papilloma (CPP), grade II atypical choroid plexus papilloma (aCPP), and grade III choroid plexus carcinoma (CPC). CPPs are considered benign tumors, with a reported 5-year overall survival (OS) rate of 90–100%. On the other hand, CPCs are rare and more aggressive tumors carrying the worst prognosis among the group [4, 5, 7]. Distant metastases from CPTs possess a high impact on patient survival, occurring in 12–50% of cases and being much more common in CPCs than CPPs [1, 8, 9].
Although commonly benign in regard to pathology, CPTs often grow into considerable size before clinical manifestation, which typically occur due to hydrocephalus. However, symptoms are often subtle within the pediatric population due to cranial expansibility. Overall, this fact may lead to challenging and potential dangerous surgical scenarios and morbidity and not clearly defined neuro-oncological managements [3, 4]. Currently, there is only a few numbers of studies reporting on CPTs in the literature, and most of the published series are small and tend to present uneven results [10]. Here, we perform a national registry analysis of biopsy-proven intraventricular CPT patients accumulated from 2004 to 2015. First, we describe the epidemiology of these tumors; then we assess clinical and tumor characteristics; and finally, we look at management patterns to identify associations with survival in this specific group of relatively rare tumors.
Material and methods
Data source
Established in 1989, the National Cancer Database (NCBD) is a nationally recognized clinical oncology database, sponsored by the American College of Surgeons and the American Cancer Society. The NCDB collects data from > 1500 facilities accredited by the Commission on Cancer and contains information on treatments and outcomes for patients with malignant disease. The current database gathers > 70% of new cancer diagnoses in the US and contains > 34 million historical records.
Data was obtained from the NCDB for patients diagnosed with brain tumors between January 1, 2004 to December 31, 2015 (223,404 patients). Patients excluded were those with non-CPT histology confirmation, non-purely intraventricular tumor, or unknown WHO grade (Fig. 1). The remaining 439 patients were then stratified and analyzed based on available database information.
Statistical analyses
The primary outcome for this study was overall survival (OS) measured from date of diagnosis. Secondary goals included the description of the baseline clinical characteristics of patients with intraventricular CPTs, as well as the patterns of care that they received. In order to prevent bias based on sites with underreporting of data (favoring the inclusion of some centers over others) and improve result validity, all patients complying with the previously described criteria were evaluated, even if they contained one or more missing data elements. Important prognostic factors including gender, age, race, median income, distance to hospital, Charlson/Deyo score, WHO tumor grade, tumor size, extent of resection, radiation therapy, and chemotherapy were evaluated. The Kaplan Meier method, with log-rank test, was used to independently analyzed the impact of specific variables on survival distribution. Multivariable analysis was performed via Cox proportional hazards models to further investigate factors associated with OS. The Welch t-test was run to determine if there were differences between tumor size of pediatric and adult population. Chi-square test or Fisher-exact test were used to compare categorical variables. All statistical analyses were performed using the SPSS program (SPSS, version 24.0; SPSS Inc., Chicago, IL) and p < 0.05 was considered statistically significant.
Results
Clinical characteristics
Patient characteristics are shown in Table 1. Among 223,404 patients with brain tumors in the National Cancer Database (NCDB), cases of biopsy-proven CPT represent 0.52% of the total population. From these patients, 439 were diagnosed with an intraventricular CPT and known WHO grade classification (Fig. 1). Although patients under 11 years concentrated almost 40% of the total population, it was noteworthy that 54.4% were non-pediatric patients (> 18 years old). Eighteen percent of patients were diagnosed at 1 year old or younger. WHO grade I tumors were more frequent in the adult population (> 18 years old), while both WHO grade II and III were more common in patients less than 1 year old (p < 0.01; Fig. 1a of Supplemental Material). Median tumor size was 3–4 cm. Mean tumor size in the pediatric population (4.39 ± 0.15 cm) was greater than in the adult population (2.7 ± 0.1 cm), with a statistically significant difference of 1.6 cm between both groups (95% CI 1.25 to 1.96, p < 0.01).
Most of the tumors were low grade lesions. In fact, CPP (WHO grade I) accounted for 69.2% of all tumors, whereas aCPP accounted for 16.9% (WHO grade II) and CPC (WHO grade III) for 13.9%. Frequency was similar between males and females in general (51.7% vs 48.3% respectively; p = 0.066), but there was a male predominance in WHO grade II and WHO grade III patients (p = 0.039, Fig. 1b of Supplemental Material); 71.3% of the tumors appeared in white population (p = 0.048).
Treatment characteristics
Surgery and extent of resection
All patients included underwent biopsy or resection (Table 1). EOR was unknown in 163 patients (37.1%), while 166 (37.8%) underwent GTR, 55 (12.5%) underwent subtotal resection (STR), and 55 (12.5%) underwent biopsy alone. As extent of resection is described as cornerstone aspect in the management of CPT patients, we analyzed the known data regarding EOR and found that there were no differences in the distribution of biopsy, STR or GTR among different age groups, WHO grades or tumor sizes (p > 0.05; Table 1 of Supplemental Material). Despite the importance of GTR, our data show that this is achieved only in 52.2% to 66.7% of cases. Surprisingly, although GTR seemed to favor 5-year OS in patients with WHO grade I tumors (p < 0.35) (Fig. 2d), extent of resection was not associated with improved OS on multivariable analysis (p > 0.05). (Table 2).
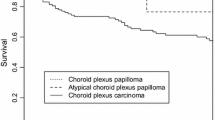
Kaplan–Meier curves of overall survival among 439 patients diagnosed with intraventricular choroid plexus tumor in the National Cancer Database 2004–2015. Five-year overall survival among all patients was 87%, while 10-year overall survival was 84% (a); Kaplan–Meier curve of overall survival following diagnosis of intraventricular choroid plexus tumor based on group of age. Five-year overall survival among patients under 18 years old (pediatrics), between 18 and 60 years old (adults), and older than 60 years old (elderly), was 91%, 90%, and 52%, respectively. Age was independently associated with worse survival after diagnosis (log rank p < 0.001) (b); Kaplan–Meier curve of overall survival following diagnosis of intraventricular choroid plexus tumor based on WHO grade. Five-year overall survival among patients classified as WHO grade I, WHO grade II, and WHO grade III was 92%, 79%, and 70%, respectively. WHO grade was independently associated with worse survival after diagnosis (log rank p < 0.001) (c); Kaplan–Meier curve of overall survival following diagnosis of choroid plexus papilloma (WHO grade I) based on extent of resection. Five-year overall survival among patients that underwent biopsy, STR, or GTR was 84%, 91% and 95%, respectively. Extent of resection was not associated to significantly influence overall survival after diagnosis (log rank p < 0.001) (d). WHO World Health Organization, STR subtotal resection, GTR gross total resection
Radiation and chemotherapy
Among all CPT patients, only a minority received radiotherapy (5.7%) or chemotherapy (7.6%) (Table 1). However, when stratified by WHO grade, it was evident that most of the patients receiving adjuvant therapy had a WHO grade II (aCPP) or III (CPC) tumor (p < 0.001). Although only three WHO grade III patients received combined chemotherapy and radiation therapy, 63.9% of them received some type of adjuvant therapy, where radiotherapy was administered in 25% and chemotherapy in 44.3% of cases (Table 2 of Supplemental Material and Fig. 3a). In general, the mean age for patients receiving chemotherapy was 2.3 years old (range, 0 to 15 years old; 54.4% in < 1 year) and for those receiving radiotherapy the mean age was 35.7 years old (range, 1 to 70 years old; 76% in > 18 years old). When the impact of adjuvant therapy on survival distribution was evaluated in the group of WHO grade 3 patients, no survival benefit was found (p > 0.05) (Fig. 3b).
Overall survival
Five-year and ten-year OS among all patients was 87% and 84%, respectively (Fig. 2a). The impact of individual factors on 5-year OS was evaluated using the Kaplan–Meier method. According the age groups, patients diagnosed after 60 years old presented with less favorable survival (p < 0.001) (Fig. 2b), as well as patients with higher WHO grade (p < 0.001) (Fig. 2c). Similarly, impact of EOR was evaluated in each of the WHO grades. For patients diagnosed with CPP (WHO grade I) who underwent GTR, 5-year OS was 95%, whereas it was 91% with STR and 84% with biopsy alone. However, these differences were not significant in this group (p < 0.35) (Fig. 2d) and neither in WHO grade 2 nor WHO grade 3 CPT patients (Fig. 2 of Supplemental Material).
On multivariable analysis, neither EOR, utilization of radiotherapy or chemotherapy, or tumor size were predictive for improved survival (p > 0.05 for each one). However, accordingly to our previous results, patient age (p = 0.022), WHO grade (p = 0.003) and medical comorbidity scores (p = 0.002) remained independently and significantly associated with OS after diagnosis (Table 2). Overall, although the use of radiotherapy and chemotherapy was significantly associated with WHO grade, the use of adjuvant therapy was not predictive of improved survival (Table 2; and Table 2 of Supplemental Material).
Discussion
CPTs are rare intracranial tumors that often represent challenging clinical scenarios. Biopsy proven CPTs account for 0.52% of all brain tumors within this large patient cohort. As expected, patients with advanced age (particularly those over 60 years old), higher medical comorbidities, or higher WHO grade presented a worsened OS after diagnosis. However, despite the median tumor size being around 3–4 cm, OS was excellent (87% and 84% for all at 5 and 10 years, respectively) and particularly favorable for those diagnosed with CPP who underwent GTR (95% at 5 years). Considering the long-term survival of patients with CPT demonstrated in the present study, therapies that aim to maximize tumor control and limit further complications are critical for the overall management in these patients.
It is worth mentioning some key epidemiological findings of our study given the large cohort that was studied. First, 54.4% of patients were older than 18 years, contrary to the current belief that most of these tumors occur in children [11]. Although there exist multiple reports on CPTs presenting in the adult population, most of them consist of small series and they may be more commonly distributed in this age group than what it is currently described in the literature [12,13,14,15]. However, it is fair to say that patients before adolescence concentrated almost 40% of the total population (< 11 years old).
Second, we found nearly identical incidence of males and females patients for the whole series of CPTs, which is in contrast with the current series suggesting a male preponderance [6] with a male to female ratio of 1.4:1 for the same group of patients. On the other hand, our results support a Surveillance Epidemiology and End Results (SEER) data report of 349 CPTs that found no gender predilection but a significant association between male gender and worse OS [7]. In our study, after performing a stratified analysis according to WHO grade, we show a statistically significant male preponderance only for the more aggressive WHO grade II and III tumors, which may connect and explain all the previously reported results. Third, the frequency of CPTs was confirmed in our series, representing 0.52% of all brain tumors. Similar to our findings, CPTs have been reported at rates of < 1% of all brain tumors [16, 17]. Fourth, most of CPTs have been reported to appear in white patients. In fact, previous reports of malignant brain tumors in children less than 1 year old also show higher incidence in white patients than in other races [18]. Although we also report a higher incidence of CPTs in white patients, this information must be contextualized with the country’s racial distribution.
In accordance with previously described studies, WHO grade III CPT (CPCs) were found more frequently in the pediatric population (77% of the cases in patients < 18 years old, representing 23.5% of the tumors in this age group, but only 5.8% of the tumors in those ≥ 18 years old), with the group of patients < 1 years old accounting for 40% of CPCs cases (Table 1). WHO grade I (CPPs) were observed more frequently in non-pediatric patients and given that CPPs represent almost 70% of all CPTs, this led to the fact that 54.4% of all CPTs patients were non-pediatric [19, 20]. Furthermore, mean tumor size of pediatric patients was significantly greater than mean tumor size of adult population, which may be in line with the higher prevalence of more aggressive disease in pediatric population and also the higher cranial vault expansibility and subtle symptoms upon the presence of high intracranial pressure and hydrocephalus.
Age older than 60 years, as well as higher medical comorbidities, was significantly associated with worse OS, most probably due to the inherent relationship between these two variables after 60 years complications of surgery remained unknown, and further studies should analyze EOR-associated complications. Since previous studies have analyzed CPT outcomes predominantly in children and there are few reports regarding the adult population, our findings may be important during daily clinical decision making in an attempt to better weigh therapeutic efforts, survival and quality of life.
Although the treatment of intraventricular tumors is controversial due to the challenges presented by their location, size, functionality of surrounded anatomy and presence of hydrocephalus; maximal safe resection remains the mainstay of the treatment. In fact, GTR has been reported as the most important predictor of survival, particularly in WHO grade III CPTs. However, even after complete surgical removal, many patients still experience recurrence, and adjuvant radiation therapy or chemotherapy is often used for optimizing tumor control and patient survival [6, 21].
Since EOR is considered a major prognostic factor for CPCs, GTR has been recommended in CPCs even if it is often difficult due to the high risk of intraoperative hemorrhage [22]. Reported CPCs 5-year survival rate reaches around 58% after complete tumor resection and only 20% after partial resection [4, 12, 23]. However, we did not find survival benefits from more aggressive resections when EORs were compared in a stratified manner in each of the WHO grades. Although the number of WHO grade 2 and 3 patients with complete follow-up included in our analysis may have been not big enough to detect significant differences and the data about tumor size did not include tumor volumes, it is important to highlight that the role of EOR has been challenged in CPT and other pathologies [7, 21]. Zhou et al. reported on 96 pediatric patients and describe that GTR did not offer survival benefits probably due to the use of adjuvant therapy in cases of partial tumor resection [21]. Thus, Thompson et al. reevaluated the role of EOR in medulloblastoma surgery, and after a careful analysis according to different molecular subgroups found that it may not be as relevant as claimed before [24, 25]. In this setting, it is worth mentioning, that due to the very vascularized nature of CPCs, a significant cause of morbidity and mortality is the excessive perioperative blood loss [26, 27]. Thus, the benefits of aggressive surgery must be carefully weighed against the risk of causing new neurological deficits and other serious complications [28].
Surgery is also important in cases of WHO grade I CPTs, as the need for both pathologic confirmation and symptom relief is always present [26, 29,30,31]. Previous reports describe survival benefits from GTR at 5 years for patients with CPPs [5]. Studies show that GTR is associated with a significant increase in OS compared to STR and biopsy alone in either adult or pediatric population [6, 32, 33]. However, our series that contains a largest number of CPT patients, showed no survival benefit from GTR. A careful analysis on the impact of EOR in CPT is necessary in order to determine the role of EOR on survival outcomes of CPT patients.
Furthermore, our series identified similar rates of GTR among different WHO grades, which is in contrast to previous studies reporting increasing rates of GTR with increasing WHO grades [22]. We report rates of GTR of approximately 60% for each of the WHO grades, it assumes that despite the grade, surgeons are resecting the tumor. However; according to the literature and our study WHO grade I CPT patients have excellent prognosis even when adjuvant therapy is often not performed after partial excision, which may suggest that a conservative approach during surgery can still be associated with good outcomes and that there is no reason to risk patient integrity in order to pursue aggressive surgery in this group of patients [11].
Radiotherapy (6.8%) and chemotherapy (8.2%) were less commonly utilized in general, but as expected, their use was positively correlated with higher WHO grade. In fact, 25% of patients diagnosed with WHO grade 3 tumors received radiation therapy and 45% received chemotherapy. Interestingly, when the use of radiation or chemotherapy was analyzed in this group of patients, there were no significant differences in OS. This, together with the fact that WHO grade was a proven prognostic factor in our two separate analyses (Long rank test and Cox regression), lead us to recommend a careful patient selection before treatment initiation.
As with any retrospective study, there is the risk of confounding variables that were not accounted for in our analysis, such as symptomatology, location, radiotherapy dose and technique, and others. The principal limitation of the current study is the number of patients with unknown EOR, which made difficult to determine the impact of EOR for WHO grade 2 and 3 patients, in this regard, we encourage the volumetric studies of EOR in order to elucidate a more precise effect of EOR on patient survival [34,35,36,37,38,39,40,41,42]. Furthermore, another potential limitation from using the NCDB is that the information is collected directly from the medical records by certified tumor registrars. Thus, although EOR is determined based on neurosurgeons’ experience or imaging techniques, we cannot specify which method was used to gather the EOR. Additionally, local tumor control, toxicity following therapy, and cause of death are not available in the NCDB. Regardless, given the limited published data on CPTs, the current study provides a significant contribution to the understanding of clinical characteristics and the impact of the current pattern of management on CPT patients’ outcomes.
Conclusion
Patients with CPTs present at different stages of life, often with sizable tumor burden. In our analysis, both WHO grade and age were significantly associated with survival. Considering the favorable survival of CPTs, efforts to improve tumor control should be meticulously weighed against the long-term risk associated with surgery, radiation therapy, and chemotherapy.
Data availability
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
References
Wolff JE, Sajedi M, Brant R, Coppes MJ, Egeler RM (2002) Choroid plexus tumours. Br J Cancer 87(10):1086–1091. https://doi.org/10.1038/sj.bjc.6600609
Bettegowda C, Chen LC, Mehta VA, Jallo GI, Rutka JT (2012) Supratentorial tumors in the pediatric population. In: Schmidek and sweet operative neurosurgical techniques. pp 669–683. https://doi.org/10.1016/b978-1-4160-6839-6.10056-5
Pendleton C, Olivi A, Jallo GI, Quinones-Hinojosa A (2011) Unique challenges faced by pediatric neurosurgeon Harvey Cushing in 1909 at Johns Hopkins: a choroid plexus tumor of the lateral ventricle mimicking a cerebellar lesion. Childs Nerv Syst 27(7):1145–1148. https://doi.org/10.1007/s00381-011-1444-7
Sun MZ, Oh MC, Ivan ME, Kaur G, Safaee M, Kim JM, Phillips JJ, Auguste KI, Parsa AT (2014) Current management of choroid plexus carcinomas. Neurosurg Rev 37(2):179–192. https://doi.org/10.1007/s10143-013-0499-1
Lam S, Lin Y, Cherian J, Qadri U, Harris DA, Melkonian S, Jea A (2013) Choroid plexus tumors in children: a population-based study. Pediatr Neurosurg 49(6):331–338. https://doi.org/10.1159/000367974
Mallick S, Benson R, Melgandi W, Rath GK (2017) Effect of surgery, adjuvant therapy, and other prognostic factors on choroid plexus carcinoma: a systematic review and individual patient data analysis. Int J Radiat Oncol Biol Phys 99(5):1199–1206. https://doi.org/10.1016/j.ijrobp.2017.08.012
Cannon DM, Mohindra P, Gondi V, Kruser TJ, Kozak KR (2015) Choroid plexus tumor epidemiology and outcomes: implications for surgical and radiotherapeutic management. J Neurooncol 121(1):151–157. https://doi.org/10.1007/s11060-014-1616-x
Yoshida K, Sato K, Kitai R, Hashimoto N, Kubota T, Kikuta K (2013) Coincident choroid plexus carcinoma and adrenocortical tumor in an infant. Brain Tumor Pathol 30(2):104–108. https://doi.org/10.1007/s10014-012-0112-2
McCall T, Binning M, Blumenthal DT, Jensen RL (2006) Variations of disseminated choroid plexus papilloma: 2 case reports and a review of the literature. Surg Neurol 66(1):62–67. https://doi.org/10.1016/j.surneu.2005.09.023
Bettegowda C, Adogwa O, Mehta V, Chaichana KL, Weingart J, Carson BS, Jallo GI, Ahn ES (2012) Treatment of choroid plexus tumors: a 20-year single institutional experience. J Neurosurg Pediatr 10(5):398–405. https://doi.org/10.3171/2012.8.PEDS12132
Bahar M, Hashem H, Tekautz T, Worley S, Tang A, de Blank P, Wolff J (2017) Choroid plexus tumors in adult and pediatric populations: the Cleveland Clinic and University Hospitals experience. J Neurooncol 132(3):427–432. https://doi.org/10.1007/s11060-017-2384-1
Wrede B, Liu P, Wolff JE (2007) Chemotherapy improves the survival of patients with choroid plexus carcinoma: a meta-analysis of individual cases with choroid plexus tumors. J Neurooncol 85(3):345–351. https://doi.org/10.1007/s11060-007-9428-x
Anderson M, Babington P, Taheri R, Diolombi M, Sherman JH (2014) Unique presentation of cerebellopontine angle choroid plexus papillomas: case report and review of the literature. J Neurol Surg Rep 75(1):e27–32. https://doi.org/10.1055/s-0033-1358378
Ozdogan S, Gergin YE, Gergin S, Senol O, Tiryaki M, Tatarli N, Hicdonmez T (2015) Choroid plexus carcinoma in adults: an extremely rare case. Pan Afr Med J 20:302. https://doi.org/10.11604/pamj.2015.20.302.5854
Lozier AP, Arbaje YM, Scheithauer BW (2009) Supratentorial, extraventricular choroid plexus carcinoma in an adult: case report. Neurosurgery 65(4):E816–817. https://doi.org/10.1227/01.NEU.0000348291.48810.C2
Wilhelm M, Hirsch W, Merkenschlager A, Stepan H, Geyer C, Kiess W (2012) A rare case of congenital choroid plexus carcinoma. Pediatr Hematol Oncol 29(7):643–646. https://doi.org/10.3109/08880018.2012.710298
Lin H, Leng X, Qin CH, Du YX, Wang WS, Qiu SJ (2019) Choroid plexus tumours on MRI: similarities and distinctions in different grades. Cancer Imaging 19(1):17. https://doi.org/10.1186/s40644-019-0200-1
Bishop AJ, McDonald MW, Chang AL, Esiashvili N (2012) Infant brain tumors: incidence, survival, and the role of radiation based on Surveillance, Epidemiology, and End Results (SEER) Data. Int J Radiat Oncol Biol Phys 82(1):341–347. https://doi.org/10.1016/j.ijrobp.2010.08.020
Dhillon RS, Wang YY, McKelvie PA, O'Brien B (2013) Progression of choroid plexus papilloma. J Clin Neurosci 20(12):1775–1778. https://doi.org/10.1016/j.jocn.2012.11.027
Niikawa S, Ito T, Murakawa T, Hirayama H, Ando T, Sakai N, Yamada H (1993) Recurrence of choroid plexus papilloma with malignant transformation–case report and lectin histochemistry study. Neurol Med Chir (Tokyo) 33(1):32–35. https://doi.org/10.2176/nmc.33.32
Zhou WJ, Wang X, Peng JY, Ma SC, Zhang DN, Guan XD, Diao JF, Niu JX, Li CD, Jia W (2018) Clinical features and prognostic risk factors of choroid plexus tumors in children. Chin Med J (Engl) 131(24):2938–2946. https://doi.org/10.4103/0366-6999.247195
Wrede B, Liu P, Ater J, Wolff JE (2005) Second surgery and the prognosis of choroid plexus carcinoma–results of a meta-analysis of individual cases. Anticancer Res 25(6C):4429–4433
Pencalet P, Sainte-Rose C, Lellouch-Tubiana A, Kalifa C, Brunelle F, Sgouros S, Meyer P, Cinalli G, Zerah M, Pierre-Kahn A, Renier D (1998) Papillomas and carcinomas of the choroid plexus in children. J Neurosurg 88(3):521–528. https://doi.org/10.3171/jns.1998.88.3.0521
Thompson EM, Hielscher T, Bouffet E, Remke M, Luu B, Gururangan S, McLendon RE, Bigner DD, Lipp ES, Perreault S, Cho YJ, Grant G, Kim SK, Lee JY, Rao AAN, Giannini C, Li KKW, Ng HK, Yao Y, Kumabe T, Tominaga T, Grajkowska WA, Perek-Polnik M, Low DCY, Seow WT, Chang KTE, Mora J, Pollack IF, Hamilton RL, Leary S, Moore AS, Ingram WJ, Hallahan AR, Jouvet A, Fevre-Montange M, Vasiljevic A, Faure-Conter C, Shofuda T, Kagawa N, Hashimoto N, Jabado N, Weil AG, Gayden T, Wataya T, Shalaby T, Grotzer M, Zitterbart K, Sterba J, Kren L, Hortobagyi T, Klekner A, Laszlo B, Pocza T, Hauser P, Schuller U, Jung S, Jang WY, French PJ, Kros JM, van Veelen MC, Massimi L, Leonard JR, Rubin JB, Vibhakar R, Chambless LB, Cooper MK, Thompson RC, Faria CC, Carvalho A, Nunes S, Pimentel J, Fan X, Muraszko KM, Lopez-Aguilar E, Lyden D, Garzia L, Shih DJH, Kijima N, Schneider C, Adamski J, Northcott PA, Kool M, Jones DTW, Chan JA, Nikolic A, Garre ML, Van Meir EG, Osuka S, Olson JJ, Jahangiri A, Castro BA, Gupta N, Weiss WA, Moxon-Emre I, Mabbott DJ, Lassaletta A, Hawkins CE, Tabori U, Drake J, Kulkarni A, Dirks P, Rutka JT, Korshunov A, Pfister SM, Packer RJ, Ramaswamy V, Taylor MD (2016) Prognostic value of medulloblastoma extent of resection after accounting for molecular subgroup: a retrospective integrated clinical and molecular analysis. Lancet Oncol 17(4):484–495. https://doi.org/10.1016/S1470-2045(15)00581-1
Hargrave D (2016) Extent of resection in medulloblastoma: time to reconsider? Lancet Oncol 17(4):409–410. https://doi.org/10.1016/S1470-2045(16)00143-1
Ogiwara H, Dipatri AJ Jr, Alden TD, Bowman RM, Tomita T (2012) Choroid plexus tumors in pediatric patients. Br J Neurosurg 26(1):32–37. https://doi.org/10.3109/02688697.2011.601820
St Clair SK, Humphreys RP, Pillay PK, Hoffman HJ, Blaser SI, Becker LE (1991) Current management of choroid plexus carcinoma in children. Pediatr Neurosurg 17(5):225–233. https://doi.org/10.1159/000120602
Sun MZ, Ivan ME, Clark AJ, Oh MC, Delance AR, Oh T, Safaee M, Kaur G, Bloch O, Molinaro A, Gupta N, Parsa AT (2014) Gross total resection improves overall survival in children with choroid plexus carcinoma. J Neurooncol 116(1):179–185. https://doi.org/10.1007/s11060-013-1281-5
Crea A, Bianco A, Cossandi C, Forgnone S, Fornaro R, Crobeddu E, Marino D, Piras G, Scalia G, Saglietti C, Boldorini R, Galzio R, Panzarasa G (2020) Choroid plexus carcinoma in adults: literature review and first report of a location into the third ventricle. World Neurosurg 133:302–307. https://doi.org/10.1016/j.wneu.2019.10.051
Zaky W, Dhall G, Khatua S, Brown RJ, Ginn KF, Gardner SL, Yildiz VO, Yankelevich M, Finlay JL (2015) Choroid plexus carcinoma in children: the Head Start experience. Pediatr Blood Cancer 62(5):784–789. https://doi.org/10.1002/pbc.25436
Zaky W, Finlay JL (2018) Pediatric choroid plexus carcinoma: biologically and clinically in need of new perspectives. Pediatr Blood Cancer 65(7):e27031. https://doi.org/10.1002/pbc.27031
Safaee M, Oh MC, Sughrue ME, Delance AR, Bloch O, Sun M, Kaur G, Molinaro AM, Parsa AT (2013) The relative patient benefit of gross total resection in adult choroid plexus papillomas. J Clin Neurosci 20(6):808–812. https://doi.org/10.1016/j.jocn.2012.08.003
Levy ML, Goldfarb A, Hyder DJ, Gonzales-Gomez I, Nelson M, Gilles FH, McComb JG (2001) Choroid plexus tumors in children: significance of stromal invasion. Neurosurgery 48(2):303–309. https://doi.org/10.1097/00006123-200102000-00010
Lu VM, Goyal A, Graffeo CS, Perry A, Burns TC, Parney IF, Quinones-Hinojosa A, Chaichana KL (2019) Survival benefit of maximal resection for glioblastoma reoperation in the temozolomide era: a meta-analysis. World Neurosurg 127:31–37. https://doi.org/10.1016/j.wneu.2019.03.250
Adams H, Adams HH, Jackson C, Rincon-Torroella J, Jallo GI, Quinones-Hinojosa A (2016) Evaluating extent of resection in pediatric glioblastoma: a multiple propensity score-adjusted population-based analysis. Childs Nerv Syst 32(3):493–503. https://doi.org/10.1007/s00381-015-3006-x
Mampre D, Ehresman J, Pinilla-Monsalve G, Osorio MAG, Olivi A, Quinones-Hinojosa A, Chaichana KL (2018) Extending the resection beyond the contrast-enhancement for glioblastoma: feasibility, efficacy, and outcomes. Br J Neurosurg 32(5):528–535. https://doi.org/10.1080/02688697.2018.1498450
Almeida JP, Chaichana KL, Rincon-Torroella J, Quinones-Hinojosa A (2015) The value of extent of resection of glioblastomas: clinical evidence and current approach. Curr Neurol Neurosci Rep 15(2):517. https://doi.org/10.1007/s11910-014-0517-x
Chaichana KL, Jusue-Torres I, Lemos AM, Gokaslan A, Cabrera-Aldana EE, Ashary A, Olivi A, Quinones-Hinojosa A (2014) The butterfly effect on glioblastoma: is volumetric extent of resection more effective than biopsy for these tumors? J Neurooncol 120(3):625–634. https://doi.org/10.1007/s11060-014-1597-9
Chaichana KL, Cabrera-Aldana EE, Jusue-Torres I, Wijesekera O, Olivi A, Rahman M, Quinones-Hinojosa A (2014) When gross total resection of a glioblastoma is possible, how much resection should be achieved? World Neurosurg 82(1–2):e257–265. https://doi.org/10.1016/j.wneu.2014.01.019
Chaichana KL, Jusue-Torres I, Navarro-Ramirez R, Raza SM, Pascual-Gallego M, Ibrahim A, Hernandez-Hermann M, Gomez L, Ye X, Weingart JD, Olivi A, Blakeley J, Gallia GL, Lim M, Brem H, Quinones-Hinojosa A (2014) Establishing percent resection and residual volume thresholds affecting survival and recurrence for patients with newly diagnosed intracranial glioblastoma. Neuro Oncol 16(1):113–122. https://doi.org/10.1093/neuonc/not137
McGirt MJ, Chaichana KL, Attenello FJ, Weingart JD, Than K, Burger PC, Olivi A, Brem H, Quinones-Hinojosa A (2008) Extent of surgical resection is independently associated with survival in patients with hemispheric infiltrating low-grade gliomas. Neurosurgery 63(4):700–707. https://doi.org/10.1227/01.NEU.0000325729.41085.73
McGirt MJ, Chaichana KL, Gathinji M, Attenello FJ, Than K, Olivi A, Weingart JD, Brem H, Quinones-Hinojosa AR (2009) Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J Neurosurg 110(1):156–162. https://doi.org/10.3171/2008.4.17536
Funding
This publication was made possible through the support of the Eveleigh Family Career Development Award for Cancer Research at Mayo Clinic in Florida.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflict of interests to report or financial disclosures related to this manuscript.
Ethical approval
There is compliance with ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11060_2020_3603_MOESM1_ESM.pdf
Supplementary file1 (PDF 163 kb). Fig. 1a, b WHO grade distribution according to age (A) and sex (B).WHO: World Health Organization.
11060_2020_3603_MOESM2_ESM.pptx
Supplementary file2 (PPTX 1874 kb). Fig. 2 Kaplan-Meier curve of overall survival based on extent ofresection in WHO grade 2 (A) and WHO grade 3 (B) patients. WHO: World Health Organization.
11060_2020_3603_MOESM3_ESM.docx
Supplementary file3 (DOCX 31 kb). Tables 1, 2 Extend of resection according to age, WHO grade classification and tumor size; Use of radiation therapy or chemotherapy according to WHO grade classification.
Rights and permissions
About this article
Cite this article
Ruiz-Garcia, H., Huayllani, M.T., Incontri, D. et al. Intraventricular choroid plexus tumors: clinical characteristics and impact of current management on survival. J Neurooncol 149, 283–292 (2020). https://doi.org/10.1007/s11060-020-03603-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03603-8