Abstract
In the treatment of glioblastoma (GBM) the impact of radical tumor resection as first line therapy is beyond controversy. The significance of a second resection in case of tumor-recurrence remains unclear and is an issue of debate. Since GBMs always recur, it is important to determine whether or not patients will benefit from repeat surgery. We performed a retrospective analysis of our prospectively collected database and evaluated all re-resected patients with primary GBM who underwent second surgery during a 3 years period. All patients underwent early postoperative magnetic resonance imaging. We determined survival after re-resection with regard to possible prognostic factors using Kaplan–Meier estimates and Cox regression analyses. Forty patients were included in this study. Median age was 58 years and median KPS score was 80. Average tumor volume was 5.5 cm3. A radiologically confirmed complete resection was achieved in 29 patients (72.5 %). Median follow-up was 18.8 months, and median survival after re-resection was 13.5 months. Only complete removal of contrast enhancing tumor was significantly correlated with survival after re-resection according to multivariate analysis. There was a statistical trend for KPS score influencing survival. In contrast, time between first diagnosis and tumor-recurrence, tumor volume at recurrence, MGMT status and MSM score were not significantly correlated with survival after second surgery. In the event of tumor recurrence, patients in good clinical condition with recurrent GBM amenable to complete resection should thus not be withheld second surgery as a treatment option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastomas (GBMs) are devastating tumors, and despite aggressive multimodal treatment, recurrence is inevitable. The management of recurrent glioblastoma (rGBM) is a matter of ongoing debate [6]. Treatment options encompass different chemotherapeutic as well as radio-therapeutic approaches [6, 8]. Repeat surgery is also frequently considered for rGBM [2, 3, 5, 15, 23].
To date, however, reports regarding the benefit of resection in rGBM are inconclusive. While some groups claimed a survival advantage of patients undergoing repeat surgery compared to patients who did not have a second surgical procedure [19], this observation has so far not been confirmed in larger series. In contrast, the perception of a benefit of repeat resection has been challenged [9]. Thus, it is one of the challenges for neurosurgeons and neurooncologist to establish selection criteria to identify patients who might benefit from repeat surgery. In 2010, Park and colleagues introduced a clinical scale to predict survival after repeat resection in an attempt to facilitate patient guidance [21]. They reported that patient condition, tumor location and tumor size were predictors of outcome after repeat resection. They did not, however, address the time between first diagnosis and treatment until tumor recurrence (TTR) or the extent of tumor removal achieved after repeat resection. In the first line treatment of GBM, radical tumor resection without deliberate induction of deficits is associated with a survival benefit, but data concerning the effect of extensive removal of rGBM are sparse [2, 12, 14, 22–24, 30].
With this analysis, we therefore address whether extent of resection (EOR) likewise plays a role in rGBM.
Methods
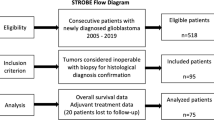
We performed a retrospective analysis of our institutional database consisting of prospectively collected data with approval from the local ethics committee (approval no. 4/09, project SNO NCH 05-11). We identified patients who underwent a second tumor resection for histologically verified GBM between October 1, 2007 and September 30, 2010. Diagnosis of GBM was established at both, first and at repeat surgery for all patients, thus ruling out pseudoprogression due to radionecrosis. All patients had undergone resection of their tumor at initial diagnosis, followed by adjuvant treatment according to Stupp et al [31]. The decision for or against repeat surgery was based on recommendations of an institutional interdisciplinary tumor board consisting of neurosurgeons, neuro-oncologists, neuropathologists, medical oncologists, and radiation therapists. Generally, criteria for repeat surgery in our institution are tumor location allowing macroscopic (near) total resection and acceptable clinical patient status (ie KPS ≥60). Patients with tumors crossing the midline or growing infiltratively into eloquent cortical or subcortical structures usually are not regarded as candidates for repeat surgery.
Every patient underwent pre- and early postoperative MRI (within 72 h) to determine the extent of tumor removal. An experienced neuroradiologist, blinded to clinical patient information independently interpreted imaging data concerning EOR. Tumor volumes were calculated using the volumetry tool of iPlan® Net 3.0 (Brainlab, Feldkirchen, Germany). If there was no evidence of residual contrast enhancement, we considered the resection to be complete, else we considered it incomplete. Patient files were also reviewed for EOR achieved in the first surgical procedure. In addition, we reviewed preoperative MRI data to classify tumor location according to the MSM score introduced by Park et al. [21]. All patients received adjuvant therapy and were followed with clinical and radiological examinations every 3 months.
We assessed overall survival (OAS) as well as survival following second surgery (SSS) and looked at factors potentially affecting patient outcome [patient age, clinical status according to preoperative Karnofsky performance scale (KPS) score, tumor size, MGMT promotor methylation status, MSM score, TTR, and EOR].
Statistical analyses were performed using commercially available software (SPSS Statistics 19, IBM, Chicago IL). Survival times were analyzed with the Kaplan–Meier method. For multivariate analyses we used a Cox proportional hazard model. P values lower than 0.05 were considered statistically significant.
Results
Forty patients met the inclusion criteria. We included 22 female (55 %) and 18 (45 %) male patients. At recurrence, median age was 58 years (range 30–76), median KPS score was 80 (range 30–100), and the median tumor volume according to volumetric analyses was 5.05 cm3 (range 0.16–48.5); for statistical analyses, we stratified between tumors < or > median volume and considered them small or large, resepectively. Median TTR was 10.2 (range 3.7–32.9 months), so it was considered early if it was less than 10 months and late if it was 10 months or longer following first surgery. Following repeat surgery, adjuvant treatment was performed according to an institutional interdisciplinary tumor board recommendation and patient preference: 31 patients received temozolomide chemotherapy (77.5 %), 3 patients (7.5 %) had re-irradiation therapy, and 3 patients (7.5 %) underwent re-irradiation and additional temozolomide chemotherapy. 2 patients (5 %) received CCNU chemotherapy, 1 patient (2.5 %) received ACNU chemotherapy. Median follow-up time after repeat surgery was 18.8 months. Histologically, a methylated MGMT promotor was found in 4 patients (10 %), while it was not methylated in 16 (40 %). In half of the patients, MGMT promotor methylation testing rendered inconclusive results.
Survival after second surgery (SSS)
Table 1 summarizes the association of potential prognostic factors with SSS. Median SSS was 13.0 months (95 % CI 10.1–17.0). EOR appeared to be the strongest predictor of survival following resection of rGBM with a median SSS advantage of 6.7 months for patients undergoing a radiologically complete tumor resection (median 15.3 months, 95 % CI 13.0–17.6) compared to patients with residual tumor (median 8.6 months, 95 % CI 4.9–12.3; Fig. 1a). This difference was statistically significant in both uni- and multivariate analyses. Removal of at least 95 % of the tumor volume showed a survival benefit of 5.5 months (p < 0.05, Log rank test), but it did not reach statistical significance in the multivariate analysis (Table 1). Similarly, age and KPS appeared to be prognostic factors according to Kaplan–Meier estimates, but for both statistical significance was missed in the multivariate analysis. There were no statistically significant differences between patients bearing tumors smaller or greater than 5 cm3 (Table 1). Likewise, we did not observe statistically significant differences concerning SSS between patients with an MSM score of ≤1 compared to ≥2. While SSS of patients with a methylated MGMT promotor was longer than of those not exhibiting this methylation, this difference was not statistically significant (Table 1). When looking at TTR as a prognostic factor, there was no difference between patients with an early vs. late recurrence (13.0 vs. 13.5 months; p = 0.54, Log rank test, Fig. 1b).
Survival after second surgery. Kaplan–Meier curves showing survival after second surgery of patients with recurrent glioblastoma stratified between those with and without complete tumor removal (a); there was a statistically significant difference in favor of complete resection regarding survival (p < 0.001). There was no statistically significant difference in survival when stratifying between patients with an early or late tumor recurrence (b, p = 0.54)
Overall survival
Median OAS was 21.7 months (95 % CI 16.5–26.1 months). In univariate analyses, both complete resection and TTR were significantly associated with longer survival (p < 0.001 for both, Log rank test). Patients with complete removal of contrast enhancing tumor at recurrence had a median OAS of 26.0 months according to Kaplan–Meier estimates (95 % CI 20.9–31.1 months), which was more than 7 months longer than that of patients with an incomplete resection (Fig. 2a). Resection of at least 95 % of the tumor volume showed a statistical trend to affect survival as did KPS (p < 0.1 for both, Log rank test). When assessing the influence of EOR achieved at first resection on OAS, we found that patients with complete resection had longer OAS than patients with incomplete resection (26.2 vs. 16.2 months), however this difference did not reach statistical significance (p = 0.15, Log rank test). Interestingly, patients with complete resection at recurrence who had had an initial incomplete resection did not have shorter OAS than patients with two complete resections (19.1 vs. 18.7 months, respectively). There were no statistically significant associations for all other potential factors examined. Multivariate analysis revealed that complete tumor removal at second surgery, KPS, and TTR were independently associated with improved OAS (EOR and TTR, p < 0.02; KPS, p < 0.05; Cox regression, Fig. 2b). Details are provided in Table 2.
Overall survival. Kaplan–Meier curves showing overall survival of patients with recurrent glioblastoma stratified between those with and without complete tumor removal at second surgery (a)—patients with complete resection had a statistically significantly longer survival (p < 0.005). There also was a statistically significant difference regarding survival between patients with an early or late tumor recurrence (b, p < 0.01)
Volumetric assessment of EOR
In 29 patients, a complete resection was achieved (72.5 %) at repeat surgery, whereas it was incomplete in 11 patients (27.5 %). Residual tumor constituted less than 5 % of the initial tumor volume in 3 patients (7.5 %), while it was more than 5 % in 8 patients (20 %). There was no statistically significant association between tumor volume and complete resection (p = 0.48, Fisher’s exact test), or tumor volume and resection of at least 95 % of the tumor (p = 1.0, Fisher’s exact test; Table 3).
Influence of the first resection on result of second surgery
At first surgery, a complete tumor resection was achieved in 23 patients (57.5 %), while it was incomplete in 17 (42.5 %). Of the latter, 10 (58.8 %) had complete resection at second surgery; there was no association between EOR achieved at first or second surgery, respectively (p = 0.15, Fisher’s exact test, Table 4).
Complications of repeat surgery
5 patients (12.5 %) showed a new or worsening of an already existing neurological deficit. 2 patients (5 %) suffered from postoperative CSF fistula leading to wound revision with resolution thereafter. 1 patient (2.4 %) had a wound infection requiring antibiotic treatment.
Discussion
The role of (extensive) tumor resection for GBM is beyond controversy [30]. In contrast, the value of a repeat resection for rGBM has not been determined yet. Without doubt, maintaining quality of life, prolonging survival and delaying new symptoms are the main goals when treating patients for tumor recurrence. Re-craniotomy in combination with adjuvant postoperative therapy might play an important role concerning quality of life and survival time [15]. Concerns have been raised, because repeat resection carries a higher risk of wound infection and neurological deficits [7, 18]. Therefore, it has been argued that only patients with severe neurological deficits due to mass effects of recurring tumor tissue should undergo second surgery [18]. Thus, it can be difficult to counsel patients whether or not to undergo repeat surgery in the event of tumor recurrence [13].
We recently reported that the risk of new diffusion weighted imaging lesions and new neurological deficits does not differ significantly between patients undergoing first or repeat resection of a glioma [10]. We did find, however, that tumor localization was of major importance, and surgery in areas such as the insula or operculum put neurological function at risk. In 2010, Park et al. [21] introduced a new scale to predict survival of patients with rGBM based on KPS, tumor volume and tumor localization (MSM score). Thereby Park et al. predicted poor, intermediate and good clinical outcomes/after re-surgery of GBM. In patients with tumors adjacent to MCA territory and eloquent regions Park et al. found a poorer outcome than for patients with other tumor localizations. In our current series, the complication rate was lower than previously reported for patients undergoing repeat surgery [7], although there appeared to be a higher risk of wound healing disturbances (CSF fistula, infection) than was reported for patients undergoing first tumor resection [25]. We suppose that patients with tumor recurrence in eloquent regions might have a poorer outcome because total tumor resection might not be possible due to the eloquent region of the tumor. Consequently, MSM score did not influence SSS or OAS on a statistically significant level.
According to our current study, EOR as determined by complete removal of contrast enhancing tumor according to early postoperative MRI was the only factor statistically significantly influencing SSS. In contrast to Stark et al. [28], who found EOR at repeat surgery to be beneficial only on univariate analysis, in our patient series EOR affected SSS resection in both, univariate and multivariate analyses. It must be kept in mind, however, that all of our patients received adjuvant treatment following repeat surgery, which is in line with other groups’ recommendations [9, 15, 32].
Several groups [3, 4, 12, 14, 16, 17, 23, 28] have previously assessed the influence of resection of rGBM, however most groups have not assessed the EOR by means of early postoperative MRI (Table 5). In contrast to our results, Filippini et al. [11] reported that re-resection did not prolong survival in case of tumor recurrence. However in their study, only 88 % of their patients underwent surgery as first line therapy, and 12 % had only biopsy. In their paper it does not become clear how many of the patients who had undergone surgery in the first place had second surgery later. In our series, all patients underwent tumor resection at initial diagnosis and recurrence. Some patients in the series of Filippini et al. only had CT scans to determine EOR, and approximately 40 % of patients did not have any form of postoperative imaging at all. It is well known that CT or surgeon’s impressions are inferior to MRI in terms of determining EOR [1].
In our current study, all patients had pre- and postoperative MRI (following both, first and second surgery), thereby providing a valid means of assessment of EOR. We demonstrate that a second neurosurgical intervention clearly impacts further patient survival, if a radiologically complete resection of enhancing tumor tissue is achieved, irrespective of TTR: we found that TTR (< or ≥10 months) was not a significant prognosticator for further survival in our series. A radiologically complete tumor resection prolonged SSS by more than 6 months compared to patients with an incomplete resection. As a conclusion, both patient groups (with early and late recurrence) may benefit from second tumor resection alike. In our opinion this is an important aspect when counselling patients.
Analysis of OAS, however, showed that patients with an early tumor recurrence had a shorter survival than those with a late recurrence; in part, this may be explained by the fact that treatment for tumor recurrence can only influence SSS and cannot make up for the time until tumor regrowth. It is also possible that differences in tumor biology can be held accountable; unfortunately, we were able to gather reliable data on MGMT status only in a subset of patients; therefore, the differences observed in SSS and OAS between patients with and without methylated MGMT promoter did not reach statistical significance. Conceivably MGMT status could be an important prognosticator, if outcomes are studied in a larger cohort. However, this does not diminish the impact of neurosurgical intervention on further survival at recurrence.
Some groups have even reported positive effects of multiple resections for tumor recurrences [5, 15]. Ko et al. [16] found better outcomes for patients receiving chemotherapy wafers and iodine-125 seeds if a gross-total resection was achieved at tumor recurrence. Just recently Chaichana et al. [5] reported statistically significantly longer survival for patients who underwent not only one, but up to three tumor resections. Additional tumor resections beyond third surgery were not found to be efficacious in terms of providing additional lifetime. In their study, OAS was 6.8 months in patients who had only one tumor resection, compared to 15.5 or 22.4 months in patients who also had a second or third resection, respectively. There may be, however, a potential selection bias in offering additional surgery to some patients while not offering it to others.
The strength of our study is, in contrast to those published earlier, that patient selection was very homogenous, i.e. we included only patients in whom a near complete resection was deemed possible, whereas those in whom only a partial removal was attempted were not included. The decision to perform repeat resection was based upon an interdisciplinary board recommendation and patient preference; repeat surgery was usually offered to patients who were in rather good clinical condition (KPS was <60 in only 5 patients) and if we thought the tumor could be resected for the largest part. Thus, large remnants >25 % occurred in only 4 patients. Certainly our group of patients represents a highly selected cohort, and this selection accounts for the fact that complete resections were achieved in >70 % of repeat surgeries, but only <60 % of first surgeries.
Also, absolute survival times of the patients in this cohort must be interpreted with caution: arguably, we cannot be certain that solely performing repeat tumor resection truly affects OAS, since we did not compare patients who had undergone second surgery to those who did not. Nonetheless, assessment of EOR clearly showed that complete removal of contrast enhancing recurrent tumor was advantageous over incomplete removal with regards to both, SSS and OAS. In contrast, removal of only 95 % of the tumor volume, or less (data not shown), did not influence patient survival. Thus, “aggressive” surgical treatment of rGBM (>95 % resection) is warranted in all patients, if a complete resection seems feasible.
Comparable to other contemporary series on GBM resection without surgical adjuncts, we unfortunately did not achieve a 100 % complete resection rate [29]. In order to achieve radiologically complete resections, we believe the use of adjunct surgical technology, e.g. intraoperative imaging or fluorescence guidance [20, 27] is a valuable option. Recently, we and other groups have stressed the influence of surgical technology on optimizing EOR in GBM [17, 20, 26]. Complete tumor resection at first surgery has been shown to affect OAS in patients with GBM [22, 24, 30]. Here, EOR at recurrence also influenced OAS, even if the first surgery resulted in an incomplete resection—we could achieve a complete resection of rGBM in almost 60 % of patients with an incomplete resection at first surgery. In this respect, our study corroborates the findings of Bloch et al. [4] who concluded that complete resection in the event of tumor recurrence may even overcome any potential shortcomings of the initial treatment. Therefore, it appears reasonable to use adjunct techniques to improve EOR for rGBM as well.
Due to the retrospective nature of our analysis, it is a limitation of our study that we were not able to incorporate quality of life-data. Future studies concerning the value of repeat resection should include this aspect of patient outcome.
Conclusion
The true value of repeat resection may not be clear, but patients without residual tumor after resection of rGBM fare better than those with residual tumor, regardless of the time between initial diagnosis and second surgery or EOR achieved at first surgery. Therefore, patients in good clinical condition should be offered a second tumor resection prior to adjuvant therapy if a radiologically complete resection is feasible.
The authors report no conflict of interests concerning materials, methods or findings in this study.
References
Albert FK, Forsting M, Sartor K, Adams HP, Kunze S (1994) Early postoperative magnetic resonance imaging after resection of malignant glioma: objective evaluation of residual tumor and its influence on regrowth and prognosis. Neurosurgery 34(1):45–60 (discussion 60–41)
Barbagallo GM, Jenkinson MD, Brodbelt AR (2008) ‘Recurrent’ glioblastoma multiforme, when should we reoperate? Br J Neurosurg 22(3):452–455. doi:10.1080/02688690802182256
Barker FG 2nd, Chang SM, Gutin PH, Malec MK, McDermott MW, Prados MD, Wilson CB (1998) Survival and functional status after resection of recurrent glioblastoma multiforme. Neurosurgery 42(4):709–720 (discussion 720-703)
Bloch O, Han SJ, Cha S, Sun MZ, Aghi MK, McDermott MW, Berger MS, Parsa AT (2012) Impact of extent of resection for recurrent glioblastoma on overall survival. J Neurosurg 117(6):1032–1038. doi:10.3171/2012.9.JNS12504
Chaichana KL, Zadnik P, Weingart JD, Olivi A, Gallia GL, Blakeley J, Lim M, Brem H, Quinones-Hinojosa A (2012) Multiple resections for patients with glioblastoma: prolonging survival. J Neurosurg. doi:10.3171/2012.9.JNS1277
Chang SM, Butowski NA, Sneed PK, Garner IV (2006) Standard treatment and experimental targeted drug therapy for recurrent glioblastoma multiforme. Neurosurg Focus 20(4):E4
Chang SM, Parney IF, McDermott M, Barker FG 2nd, Schmidt MH, Huang W, Laws ER Jr, Lillehei KO, Bernstein M, Brem H, Sloan AE, Berger M (2003) Perioperative complications and neurological outcomes of first and second craniotomies among patients enrolled in the Glioma Outcome Project. J Neurosurg 98(6):1175–1181. doi:10.3171/jns.2003.98.6.1175
Combs SE, Gutwein S, Thilmann C, Huber P, Debus J, Schulz-Ertner D (2005) Stereotactically guided fractionated re-irradiation in recurrent glioblastoma multiforme. J Neurooncol 74(2):167–171. doi:10.1007/s11060-004-2463-y
De Bonis P, Fiorentino A, Anile C, Balducci M, Pompucci A, Chiesa S, Sica G, Lama G, Maira G, Mangiola A (2013) The impact of repeated surgery and adjuvant therapy on survival for patients with recurrent glioblastoma. Clin Neurol Neurosurg 115(7):883–886. doi:10.1016/j.clineuro.2012.08.030
Dützmann S, Gessler F, Bink A, Quick J, Franz K, Seifert V, Senft C (2012) Risk of ischemia in glioma surgery: comparison of first and repeat procedures. J Neurooncol 107(3):599–607. doi:10.1007/s11060-011-0784-1
Filippini G, Falcone C, Boiardi A, Broggi G, Bruzzone MG, Caldiroli D, Farina R, Farinotti M, Fariselli L, Finocchiaro G, Giombini S, Pollo B, Savoiardo M, Solero CL, Valsecchi MG (2008) Prognostic factors for survival in 676 consecutive patients with newly diagnosed primary glioblastoma. Neuro Oncol 10(1):79–87
Gorlia T, Stupp R, Brandes AA, Rampling RR, Fumoleau P, Dittrich C, Campone MM, Twelves CC, Raymond E, Hegi ME, Lacombe D, van den Bent MJ (2012) New prognostic factors and calculators for outcome prediction in patients with recurrent glioblastoma: a pooled analysis of EORTC Brain Tumour Group phase I and II clinical trials. Eur J Cancer 48(8):1176–1184
Guyotat J, Signorelli F, Frappaz D, Madarassy G, Ricci AC, Bret P (2000) Is reoperation for recurrence of glioblastoma justified? Oncol Rep 7(4):899–904
Helseth R, Helseth E, Johannesen TB, Langberg CW, Lote K, Ronning P, Scheie D, Vik A, Meling TR (2010) Overall survival, prognostic factors, and repeated surgery in a consecutive series of 516 patients with glioblastoma multiforme. Acta Neurol Scand 122(3):159–167. doi:10.1111/j.1600-0404.2010.01350.x
Hong B, Wiese B, Bremer M, Heissler HE, Heidenreich F, Krauss JK, Nakamura M (2012) Multiple microsurgical resections for repeated recurrence of glioblastoma multiforme. Am J Clin Oncol. doi:10.1097/COC.0b013e3182467bb1
Ko AL, Fink KR, Stelzer KM, Silbergeld DL (2012) Safety and efficacy of concomitant chemotherapeutic wafers and iodine-125 seeds for recurrent glioblastoma. Surg Neurol Int 3:137
Kuhnt D, Becker A, Ganslandt O, Bauer M, Buchfelder M, Nimsky C (2011) Correlation of the extent of tumor volume resection and patient survival in surgery of glioblastoma multiforme with high-field intraoperative MRI guidance. Neuro Oncol 13(12):1339–1348
Mandl ES, Dirven CM, Buis DR, Postma TJ, Vandertop WP (2008) Repeated surgery for glioblastoma multiforme: only in combination with other salvage therapy. Surg Neurol 69(5):506. doi:10.1016/j.surneu.2007.03.043 (discussion 509)
McGirt MJ, Chaichana KL, Gathinji M, Attenello FJ, Than K, Olivi A, Weingart JD, Brem H, Quinones-Hinojosa AR (2009) Independent association of extent of resection with survival in patients with malignant brain astrocytoma. J Neurosurg 110(1):156–162. doi:10.3171/2008.4.17536
Nabavi A, Thurm H, Zountsas B, Pietsch T, Lanfermann H, Pichlmeier U, Mehdorn M (2009) Five-aminolevulinic acid for fluorescence-guided resection of recurrent malignant gliomas: a phase ii study. Neurosurgery 65(6):1070–1076 (discussion 1076–1077)
Park JK, Hodges T, Arko L, Shen M, Dello Iacono D, McNabb A, Olsen Bailey N, Kreisl TN, Iwamoto FM, Sul J, Auh S, Park GE, Fine HA, Black PM (2010) Scale to predict survival after surgery for recurrent glioblastoma multiforme. J Clin Oncol 28(24):3838–3843. doi:10.1200/JCO.2010.30.0582
Pichlmeier U, Bink A, Schackert G, Stummer W (2008) Resection and survival in glioblastoma multiforme: an RTOG recursive partitioning analysis of ALA study patients. Neuro Oncol 10(6):1025–1034. doi:10.1215/15228517-2008-052
Pinsker M, Lumenta C (2001) Experiences with reoperation on recurrent glioblastoma multiforme. Zentralbl Neurochir 62(2):43–47. doi:10.1055/s-2002-19477
Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS (2011) An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg 115(1):3–8. doi:10.3171/2011.2.JNS10998
Sawaya R, Hammoud M, Schoppa D, Hess KR, Wu SZ, Shi WM, Wildrick DM (1998) Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors. Neurosurgery 42(5):1044–1055 (discussion 1055–1046)
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V (2011) Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol 12(11):997–1003. doi:10.1016/S1470-2045(11)70196-6
Senft C, Franz K, Ulrich CT, Bink A, Szelenyi A, Gasser T, Seifert V (2010) Low field intraoperative MRI-guided surgery of gliomas: a single center experience. Clin Neurol Neurosurg 112(3):237–243
Stark AM, van de Bergh J, Hedderich J, Mehdorn HM, Nabavi A (2012) Glioblastoma: clinical characteristics, prognostic factors and survival in 492 patients. Clin Neurol Neurosurg 114(7):840–845
Stummer W, Pichlmeier U, Meinel T, Wiestler OD, Zanella F, Reulen HJ (2006) Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol 7(5):392–401
Stummer W, Reulen HJ, Meinel T, Pichlmeier U, Schumacher W, Tonn JC, Rohde V, Oppel F, Turowski B, Woiciechowsky C, Franz K, Pietsch T (2008) Extent of resection and survival in glioblastoma multiforme: identification of and adjustment for bias. Neurosurgery 62(3):564–576. doi:10.1227/01.neu.0000317304.31579.17 (discussion 564-576)
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996. doi:10.1056/NEJMoa043330
Terasaki M, Ogo E, Fukushima S, Sakata K, Miyagi N, Abe T, Shigemori M (2007) Impact of combination therapy with repeat surgery and temozolomide for recurrent or progressive glioblastoma multiforme: a prospective trial. Surg Neurol 68(3):250–254. doi:10.1016/j.surneu.2006.11.042
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Quick, J., Gessler, F., Dützmann, S. et al. Benefit of tumor resection for recurrent glioblastoma. J Neurooncol 117, 365–372 (2014). https://doi.org/10.1007/s11060-014-1397-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-014-1397-2