Abstract
Treatment of glioblastoma with platinum compounds modestly improves progression-free survival and may cause toxic effects which prevent use at higher dose that would otherwise improve the antineoplastic effect. To reduce toxicity, we propose to encapsulate the platinum drug in a liposome. We have also tested three methods of drug administration (intra-venous, intra-arterial and intra-arterial combined with blood brain barrier disruption) to determine which one optimizes the tumor cell uptake, limits the toxicity and delivers the best concomitance effect with radiotherapy. Cisplatin, oxaliplatin, their respective liposomal formulations, Lipoplatin™ and Lipoxal™, and carboplatin were assessed in F98 glioma, orthotopically implanted in Fischer rats. We found that the modest accumulation of drugs in tumor cells after intra-venous injection was significantly improved when the intra-arterial route was used and further increased after the transient opening of the blood brain barrier with mannitol. The liposomal formulations have largely reduced the toxicity and have allowed a better exploitation of the anti-cancer activity of platinum agent. Although the liposomes Lipoplatin™ and Lipoxal™ have shown a similar ability to that of carboplatin, to accumulate in brain tumors, the highest additive effect with radiotherapy was obtained with carboplatin. We conclude that the intra-arterial infusion of carboplatin or Lipoxal™ in concomitance with radiation therapy leads to the best tumor control as measured by an increase of mean survival time in Fischer rats implanted with the F98 glioma with a benefit in survival time of 13.4 and 6.5 days respectively compared to intra-venous.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma multiforme (GBM) is the most aggressive primary brain neoplasm, taking the lives of patients within a median survival time of 12–14 months after diagnosis and standard treatment, which consists of optimal surgical resection of the tumor followed by concomitant chemotherapy with temozolomide and radiotherapy [1, 2]. Optimization of concomitant effects between chemotherapy and radiotherapy requires ideally to maximize drug accumulation in tumor cells. For brain tumors, the permeability of the blood brain barrier (BBB) and the high sensitivity of healthy brain bring important challenges.
Drugs administration by intra-venous (IV) is commonly used but it results in a poor distribution in brain and a weak accumulation in tumor because of the limited permeability of the BBB, which results in low anti-cancer effects. To overcome this limited uptake of drugs in brain tumor, it has been proposed to use a cerebral intra-arterial (IA) infusion, while an even higher tumor uptake can be obtained after a temporary opening of the BBB [3, 4]. Unfortunately, adverse effects can be observed when high doses of some chemotherapeutic drugs are administrated by the IA route and some drugs that are not typically neurotoxic with a standard IV administration can become so [5–7]. Therefore, this duality leads to an important dilemma for clinicians who must look for a compromise between improved tumor accumulation of the drug and minimal adverse effects. Despite the large amount of information available on the treatment of glioblastoma, inconsistencies in the methods used, the variety of drugs tested and the disparity of research models complicate analysis of the results and make it very difficult to compare the different routes of administration of drugs and their therapeutic efficacy. Therefore, the controversy remains regarding the route of administration of drugs that would optimize the anti-cancer effect in concomitance with radiotherapy while minimizing the side effects.
The present study compares three different methods of administration [IV, IA and IA with blood brain barrier disruption (BBBD)] and five platinum drugs (cisplatin, oxaliplatin, carboplatin, Lipoplatin™ and Lipoxal™) alone and in combination with localized irradiation delivered by Gamma Knife. Drug uptake into brain tumors, toxicity and improvement of mean survival time of Fischer rats implanted in their brain with F98 glioma tumor were measured. Platinum compounds were chosen for their radiosensitizing ability [8–10]. To better exploit their radiosensitizing effect while trying to limit adverse effects, we also tested the liposomal formulations of cisplatin and oxaliplatin, which are respectively Lipoplatin™ and Lipoxal™ [11, 12].
The overall aims of this study were to use an animal model of GBM to; 1—determine and compare alternative routes of administration (IA, BBBD) to IV for each of these platinum compounds, 2—test the abilities of liposomal formulations to reduce the toxicity associate to their respective bare platinum compounds and 3—evaluate the concomitant anticancer effect of these drugs in combination with radiotherapy.
Materials and Methods
Chemicals
Carboplatin and oxaliplatin were obtained respectively from Novopharm (Anjou, QC, Canada) and Sanofi-Avantis (Laval, QC, Canada). Cisplatin was purchased from Sigma-Aldrich (Oakville, ON, Canada). Lipoplatin™ and Lipoxal™ were generously provided by Regulon Inc. (Athens, Greece).
Cell line and culture conditions
We chose the F98 cell line as it is syngeneic with the Fischer rat, eliminating any fluctuations that can be caused by the immune response generate by other cell type implanted in non-immunosuppressed animal. F98 model was also chosen because it is known to adequately reproduce the behaviour of human GBM, particularly in terms of its response/resistance to chemo- and radiotherapy [13, 14]. The F98 cell line was obtained from American type culture collection (Manassas, VA, USA) and tested negative for the MAP assay by Charles River Laboratories (Wilmington, MA, USA). The cells preparation and maintenance used in our experiments are described by Blanchard et al. [15].
Animal experiments
For all procedures (implantation, chemotherapy infusion, radiotherapy and euthanasia) male Fischer rats (Charles River Laboratories, Saint-Constant, QC, Canada) were anesthetised with an intra-peritoneal injection of ketamin/xylazine (87/13 mg/ml) at 1 ml/kg. The experimental protocols were approved by the institutional ethical committee and conformed to regulations of the Canadian Council on Animal Care. A diagram of the overview of the experimental strategies used is shown in Fig. 1.
F98 glial cells implantation in Fischer rat brain
For the implantation procedure, confluent F98 cells were suspended in non-supplemented warm MEM at a concentration of 2,000 cells/μl. The implantation (10,000 cells in 5 μl) was performed as described by Blanchard et al. [15].
Routes of drug administration
Ten days after the F98 glioma cells implantation, platinum compounds were administrated. Equivalent doses of platinum compounds to those used in humans were established in respect to the body surface area, which is determined as 0.04 m2 for rats weighting 250 g. Platinum doses used in this study were: carboplatin 5 mg, oxaliplatin 3 mg, cisplatin 3 mg, Lipoplatin™ 3 mg (of cisplatin) and Lipoxal™ 3 mg (of oxaliplatin). Free platinum drugs were diluted in 1 ml of 5 % dextrose solution (Baxter, Toronto, ON, Canada). Lipoplatin™ and Lipoxal™ were used without dilution at a concentration of 3 mg platinum/ml.
The IV injections were performed via the tail vein over 2 min. Regarding the groups of animal injected IA, the drugs were infused in the right internal carotid artery in a retrograde manner via the external carotid as described by Fortin et al. [16, 17]. A solution of 1 ml of platinum formulation was injected over 20 min. Temporary disruption of the blood brain barrier (BBBD) by mannitol was accomplished following the same surgical procedure as described for the IA procedure. In a previous study, MRI scanner for animals was used after injection of mannitol to follow the temporal opening of BBB. The permeability of the BBB was increased early after infusion of mannitol and remained open for at least 30 min [18]. Before platinum drug infusion, a warm (37 °C) solution of mannitol 25 % was administered in the right internal carotid artery in a retrograde manner via the external carotid at a rate of 7.20 ml/min for 30 s as described by Blanchette et al. [18, 19]. Beginning three minutes after the BBBD, the drugs were infused over 20 min by the same catheter used for the mannitol injection. After IA infusion, the external carotid was ligated and the neck of the animal was closed by sutures.
Treatment groups
Thirty-six treatment groups were planned as follows: five platinum compounds and one control (sham, cisplatin, oxaliplatin, carboplatin, Lipoplatin™ and Lipoxal™) multiply by 3 routes of administration (IV, IA, BBBD) multiply by 2 choices of combination (with or without radiotherapy).
Platinum drug uptake in tumor and brain tissue
Animals (n = 3–4 animals per group) were implanted with the F98 glioma cells at day zero, infused with platinum compounds at day 10 according to the different delivery approaches described previously, and euthanized 24 h later. Brains were removed by craniotomy and promptly cut in two sections with a brain matrix (WPI, RBMA-300C, Sarasota, FL) as described elsewhere [17]. Briefly, left hemisphere (contralateral section) and tumor section were isolated and a part of the tumor section was divided for the cytoplasmic and nuclear compartments analysis. The nuclear and cytoplasmic compartments were separated using a commercial Nuclear Extract Kit (Active Motif, Carlsbad, CA). These fresh tissue and cellular compartments samples were rapidly weighed and solubilised in 10 % nitric acid, 30 % hydrogen peroxide and sonicated until homogenization. Samples were then analysed for platinum concentration by inductively coupled plasma mass spectrometer (ICP-MS) (ELAN DRC-II, PerkinElmer, Woodbridge, ON, Canada).
Gamma Knife irradiation of brain tumor
Twenty-four hours after chemotherapeutic treatments (platinum compounds and sham), rats (n = 8–12 animals per group, except for cisplatin where n = 4 animals) were anesthetised and positioned in our home made stereotactic frame [20] designed for the Gamma Knife 4C and later adapted [21] for the Gamma Knife PERFEXION (Elekta Instruments AB, Norcross, GA, USA). The 8 mm collimators were used to deliver the radiation treatment at predetermined coordinates targeting the tumor which typically had a diameter of about 4 mm [15]. GBM are not routinely treated in clinic with the Gamma Knife. However, to irradiate such a small tumor implanted in a rat brain with a margin of 2 mm, the Gamma Knife is an adequate tool available to precisely treat them with a minimum radiation dose deposited to the surrounding tissues in the brain. Fractionation with a daily radiation dose of 2 Gy was deemed impractical for our experiments, since such a protocol requires repetitive animal anaesthesia, which leads cumulatively to important toxic effects. Therefore, the brain tumors were irradiated with a single dose of 15 Gy (2.8 Gy/min), which is radiobiologically approximately equivalent to a typical protocol of 25 daily fractions of 2 Gy. Control animals (sham) received 1 ml of 5 % dextrose (vehicle for platinum drugs) infused as performed for animals treated with platinum compounds.
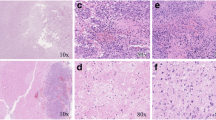
Evaluation of mean survival time
Animal monitoring, including weight measurement, mobility, coordination, loss of self-grooming (periocular secretion accumulation) and landing ability was performed on a daily basis. In agreement with the ethical committee regulations, the experimental endpoint for survival was established when the animals lost a maximum of 30 % of their initial weight or when one of the monitored function reached a score of 1/10. At this point, animals were anesthetised and 4 % paraformaldehyde (PFA) was infused by intra-cardiac route to fix the brain tissue. The brain was removed by craniotomy to corroborate the presence of tumor and to be kept in PFA for future analysis.
Statistical analyses
Data of drug accumulation were analysed by a Student’s t test to compare two treatments together and by ANOVA for more than two groups. For the survival study, data were analysed by the Quartile method before doing Kaplan–Meier survival curves which were analysed by Log-Rank test. P values under 0.05 were considered statistically significant. A complete statistic Table is available in the Electronic Supplementary Material.
Results
Drugs accumulation in nucleus and cytoplasm of tumor cells
When the IV route of administration was used, the uptake of carboplatin, Lipoplatin™ and Lipoxal™ in the nucleus of cancer cells were very low (~4 ng platinum/g tissue), whereas the accumulation of cisplatin and oxaliplatin were significantly more substantial (P < 0.03) with 67 ± 14 and 78 ± 8 ng platinum/g tissue respectively. All these drugs were also distributed preferentially in the cytoplasm (Table 1; Fig. 2).
Uptake of the studied Platinum drugs, 24 h after administration. Nucleus and cytoplasm are from the tumor sections. Tumor section was measured separately (it is not an addition of nucleus and cytoplasm). The term Contra-lat refers to the healthy contralateral hemisphere of the brain that does not contain the tumor. IV intra-veinous, IA intra-arterial, BBBD blood brain barrier disruption
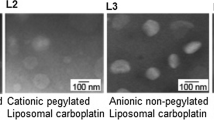
Administration via the IA route largely increased the concentration of drugs in tumor cells. Accumulations of the liposomal formulations Lipoplatin™ and Lipoxal™ in the cell’s nucleus were increased by 153 and 91 times compared to the values obtained with the IV route. It is noteworthy that although carboplatin administrated by IA reached higher levels in nucleus and cytoplasm than measured after IV injection, this drug was still accumulated at lower levels than cisplatin and oxaliplatin injected IV.
For Lipoplatin™ and Lipoxal™, BBBD did not further increase their accumulation in nucleus of tumor cells (P = 0.32 and 0.49 respectively) whereas twofold increase was observed only in the cytoplasm for these drugs. Conversely, BBBD for carboplatin led to an 18-fold increase in the nuclear concentration, while a 4.7-fold increase was measured in the cytoplasm (nucleus IA = 9 ± 7, nucleus BBBD = 160 ± 85, cytoplasm IA = 84 ± 61, cytoplasm BBBD = 398 ± 191).
Drugs accumulation in tumor and contralateral brain
We also measured the impact of the routes of administration on the distribution of platinum drugs between the tumor and the healthy contralateral brain (Table 1; Fig. 2). For all drugs, a preferential accumulation in the tumor area was measured, whatever the route of administration used. The IA route improved both the tumor uptake and specificity for cisplatin, carboplatin, LipoplatinTM and LipoxalTM, but not for oxaliplatin. Surprisingly, the tumor uptake of oxaliplatin was not modified when this drug was injected by IA. BBBD increased by two to fivefold the drug accumulation in the tumor, the highest improvement being observed with the liposomal formulations. Regarding the contralateral brain, administration through IV or IA resulted in a similar and modest drug uptake for all the drugs, except for cisplatin. However, BBBD promoted by 3.4 to tenfold the distribution of carboplatin, Lipoplatin™ and Lipoxal™ in the contralateral brain.
Cisplatin and oxaliplatin were not evaluated for BBBD, because they were already deemed too toxic for the animals when administrated IA.
Anti-cancer effect and toxicity of the platinum compounds
IV administration of carboplatin, oxaliplatin, Lipoplatin™ and Lipoxal™ did not significantly increase the mean survival time of the animals compared to the sham group (P > 0.43) (Table 1; Fig. 3). Even worse, injection of cisplatin reduced mean survival time to 18.1 ± 0.9 days (P = 0.012, compared to IV sham group), suggesting that this drug is too toxic for the animals even when injected IV.
Kaplan–Meier survival graphs for F98 Fischer rat model. a IV platinum alone (dashed lines) or combination with radiation (full lines). b IA platinum alone (dashed lines) or combination with radiation (full lines). c BBBD platinum alone (dashed lines) or combination with radiation (full lines). d Carboplatin and Lipoplatin™ by IV, IA and BBBD. e Oxaliplatin compared to its liposomal formulation, Lipoxal™, by IV, IA and BBBD. f Cisplatin compared to its liposomal formulation, Lipoplatin™, by IV and IA. GK gamma knife (15 Gy to the tumor volume plus a margin of 2 mm.)
The toxic effect of cisplatin was amplified when administrated by the IA route. Severe apathy was observed 3 days after its infusion, resulting in a mean survival time of 13.3 ± 0.1 days, which is much shorter than the sham group (22.5 ± 0.6 days, P < 0.001) (Fig 3f). Regarding oxaliplatin, administration through IA did not result in any improvement of the mean survival time (22.0 ± 4.7 days vs. 22.5 ± 0.6 days for sham group, P = 0.95).
Drug administration by IA was beneficial for the animals treated with carboplatin, Lipoplatin™ and Lipoxal™. The mean survival time using these drugs was improved by an interval of 6.7–8.5 days compared to the IA sham group (P < 0.004).
Blood brain barrier disruption was then used to further increase exposure of brain tumor cells to these drugs. Assays with cisplatin and oxaliplatin were not conducted considering their toxicity or lack of anti-cancer effect as measured in this animal model in our preliminary experiments. BBBD has depicted no benefits for the other platinum drugs. For the liposomal formulation of cisplatin, Lipoplatin™, the mean survival time were similar when infused IA, with or without opening of the BBB (IA = 29.2 ± 1.8 days; BBBD = 29.4 ± 6.1 days, P = 0.74). BBBD was detrimental for animals treated with Lipoxal™, as the mean survival time of these animals was shorter but not significant compared to the IA infused animals (IA = 30.1 ± 2.9 days; BBBD = 21.1 ± 12.9 days, P = 0.99). Interestingly, an important apathy was observed in the first 24 h after treatment for the Lipoxal™ by BBBD. However, for those animals that overcome this initial acute toxicity, the mean survival time was extended to 39 days compared to 30.1 days with IA. Only animals treated with carboplatin show a longest progression free survival with BBBD administration procedure (Fig. 3d), but the improvement of the overall surviving time was not significant (AI = 31.0 ± 3.6 days; BBBD = 33.7 ± 2.0, P = 0.35).
Concomitant treatment with radiation
Irradiation (IR) of the F98 tumor without platinum compounds increased the mean survival time of the animals from 22.9 ± 3.2 days (sham group) to 29.7 ± 1.4 days (sham group + IR) (P < 0.001) (Fig. 3a). When platinum compounds were administrated IV and combined with radiation, only the group treated with Lipoxal™ showed a modest but significant increase in the mean survival time from 29.7 ± 1.4 days to 31.4 ± 0.5 days (P = 0.0453).
Regarding the IA injection, its combination to tumor irradiation was beneficial only for the animals treated with carboplatin with a 10.7 days increase of the mean survival time (44.7 ± 6.1 days, P < 0.004), but not with Lipoplatin™ and Lipoxal™ (P = 0.91 and 0.40 respectively).
BBBD resulted in important toxicity for animals injected with Lipoxal™ (Fig. 3c). Consequently, combination with tumor irradiation was not conducted. Regarding treatment with Lipoplatin™, no improvement of the mean survival time was measured in the irradiated animals (sham group + IR = 34.5 ± 2.2 days vs. Lipoplatin™ + IR = 33.2 ± 1.8 days, P = 0.14). A small but not significant benefit was measured with carboplatin (sham group + IR = 34.5 ± 2.2 days vs. carboplatin + IR = 38.0 ± 6.4 days, P = 0.33).
When we analysed the irradiated groups of animals according to the administration route, tumor irradiation combined to the IA route increased the mean survival time for each drug tested compared to the IV route (P < 0.012). For the drugs tested (Lipoplatin™ and carboplatin), BBBD increased the mean survival time of the animals when compared to the IV injected groups (P < 0.005). Finally, BBBD did not significantly improve the anti-cancer activity of Lipoplatin™ and carboplatin, compared to the IA groups (P > 0.077).
Discussion
Instinctively, optimisation of the concomitant treatments of chemo- with radiotherapy requires that accumulation of chemotherapeutic agent in tumor cells is maximized, while minimizing the adverse effects to surrounding healthy brain tissue. For GBM treatment, the obstacle caused by the BBB for drug accumulation in tumor cells and sensitivity of healthy brain tissue represents significant challenges for clinicians. Using a pre-clinical syngeneic model of GBM implanted in the brain of Fischer rats, we have compared three routes of drug administration (IV, IA and BBBD). Drug uptake and tumor response were determined for five platinum compounds, which include the liposomal formulations of cisplatin and oxaliplatin (Lipoplatin™ and Lipoxal™ respectively). The concomitance effects were measured on F98 tumor, when combined to a single fraction of radiation.
Drug administration by the IV or oral routes is routinely used to treat GBM patients [22]. Our results show that IV administration leads to a modest accumulation of all five platinum drugs tested in the F98 tumor implanted in brain of Fischer rats. This low uptake of drugs did not result in a significant anti-tumor effect, as measured by the mean survival time of the rats. When IV administrations were combined to radiotherapy, only treatment with Lipoxal™ (the liposomal formulation of oxaliplatin) improved slightly the therapeutic efficacy (P = 0.045). Our results with Fischer rats are in line with clinical trials on GBM patients treated with IV platinum where a modest therapeutic efficiency was reported [23]. It is noteworthy that cisplatin was the only drug to accumulate significantly in the brain tumor after IV procedure. However, its high toxicity led to a reduction of the mean survival time of the animals. This result is in agreement with previous report suggesting that treatment with cisplatin is not appropriated in the management of brain tumor [23].
To overcome the toxic effect of cisplatin on brain, we have tested its liposomal formulation, Lipoplatin™. As this liposomal formulation is less toxic, preclinical and clinical studies made on NSCLC have shown that a 3–6 times higher dose than the standard dose of cisplatin resulted to a better anticancer effect with lower toxicity [24, 25]. In our studies, no toxicity was observed with Lipoplatin™ as measured by the mean survival time of the animals compared to controls, whatever the route of administration used. In the present study, we used the same dose for liposomal formulations and free platinum compounds for two reasons. First, we wanted to compare the radiosensitizing effect of the platinum with a minimum of variation in the method. Secondly, the liposomal formulations have a concentration of 3 mg/mL and it could be hazardous to inject a volume greater than one ml to a rat of 250 g, especially via IA and BBBD route of administration. However, IA injection was required to obtain a higher accumulation of Lipoplatin™ in the brain tumor, which was further amplified by BBBD method. It is noteworthy that drug concentration in healthy brain after BBBD of Lipoplatin™ was about 20-fold higher than measured after IV injection of cisplatin not encapsulated in liposome. This data suggests that the liposomal formulation protect the healthy brain tissue against the toxic effect of cisplatin. Moreover, as malignant gliomas are infiltrative tumors, this lends some credence to the use of the BBBD approach to reach distant infiltrative tumor cells. The explanations for this decrease in toxicity are not clear, but we cannot exclude that the liposomal formulation could modify the distribution of platinum drugs in healthy and cancer cells.
Drug administration via IA is clinically more demanding than IV infusion, since it requires an IA cannulation, and thereby the access to the angiography suite. The main advantage of IA, dubbed ‘the first pass effect’, is a higher concentration of the drug reaching the brain tumor tissue prior to its redistribution (and thereby dilution) in the whole body. In our animal model, carboplatin, Lipoplatin™ and Lipoxal™ required an IA or BBBD infusion to observe anti-cancer effects.
In the F98 Fischer rat model, infiltration of GBM cells in the brain parenchyma is somehow limited, when compared to the level of infiltration reaching the contralateral hemisphere observed in some patients [26]. Since an important advantage of opening the BBB is to reach these infiltrating clusters of cancer cells with the chemotherapeutic agent, our animal model of GBM might not be optimal to evaluate the therapeutic gain of platinum drugs after opening of the BBB. Nevertheless, our results support that BBBD might not be appropriated for all drugs. Using this approach, the gain of drug accumulation further improved the mean survival time of the animals only for carboplatin. No improvement was observed with Lipoplatin™, while a reduction of mean survival time for the animals treated with Lipoxal™ was observed. This suggests that the increase of Lipoxal™ accumulation in healthy brain after BBBD was deleterious for the animals. Therefore, precaution must be taken to select drugs showing minimal toxicity to the healthy brain when planning to administrate them by IA with or without BBBD. On the other hand, since the BBBD procedure can be safely done, this administration way should continue to be considered in further investigations. Also, it would be appropriated in subsequent studies to evaluate the maximum tolerated dose and the dose-limiting toxicity for each drug injected by the different routes.
The anti-tumor effect of platinum compounds is typically associated with their ability to bind covalently to DNA. The platinum–DNA complex combined to secondary electrons as produced by ionizing radiation has clearly demonstrated a radiosensitizing effect as measured by an increase of the yield of DNA single and double strand breaks [9]. When injected by IA, the accumulations of platinum in the nucleus of cancer cells were 40–68 times higher with the liposomal formulation Lipoplatin™ and Lipoxal™ than when the animals were treated with carboplatin. Nevertheless, the best therapeutic effect was measured with carboplatin. Although we cannot rule out that DNA is not an important target in tumor cells, these results suggest the other important molecules were targeted by carboplatin. For example, when cisplatin accumulated solely in the cytoplasm, apoptosis is induced. This supports that DNA damage may not be the only critical event for the initiation of cytotoxicity [27, 28].
Whatever the identity of these molecular targets, optimization of the concomitant effect with radiation still require an elevated drug accumulation in tumor. To reach these conditions, IA and BBBD routes of administration allow an increase in the platinum uptake compared to IV, while liposomal formulation considerably reduces the systemic toxicity observed with bare platinum compounds.
Other studies have already reported the therapeutic efficacy of platinum drugs. However, it is difficult to conclude which drugs and administration routes were the most efficient since different animal models of GBM, dose of radiation, dose of drugs were used.
However, if we focus only on the surviving outcome, our results are comparable with those of Biston et al. [29] that used convection enhance delivery (CED) and a common 6 MV standard irradiator to treat Fischer rats implanted with 1000 F98 cells. With this method Biston et al. obtained an MeSt for cisplatin of 41 days and 50.5 days combined with radiation. MeSt for carboplatin was 58 days and 83.5 days combined with radiation. In a similar study [30], delivery of liposome (Lipoplatin™ and empty liposome) by CED was highly neurotoxic and resulted in death immediately following or within a few days after administration.
The present study was necessary to compare administration routes and drugs used in the treatment of glioblastome since inconsistencies (cell lines, animal models, routes of administration, doses of drug, doses of radiation, types of radiation) do not allows to compare adequately each publication together.
In conclusion, concomitant effect with radiation was observed with all drugs tested in F98 tumor implanted in brain of Fisher rats since improvement of the mean survival time was measured with all of them after radiotherapy. However, the best concomitant effect was obtained when carboplatin was injected IA. While BBBD infusion route should be considered to maximize the potential of treatment when treating more invasive brain tumor.
References
Chaichana K, Parker S, Olivi A et al (2010) A proposed classification system that projects outcomes based on preoperative variables for adult patients with glioblastoma multiforme. J Neurosurg 112:997–1004. doi:10.3171/2009.9.JNS09805
Gilbert MR (2011) Recurrent glioblastoma: a fresh look at current therapies and emerging novel approaches. Semin Oncol 38(Suppl 4):S21–S33. doi:10.1053/j.seminoncol.2011.09.008
Hirano Y, Mineura K, Mizoi K et al (1998) Therapeutic results of intra-arterial chemotherapy in patients with malignant glioma. Int J Oncol 13:537–542
Doolittle ND, Miner ME, Hall WA et al (2000) Safety and efficacy of a multicenter study using intraarterial chemotherapy in conjunction with osmotic opening of the blood-brain barrier for the treatment of patients with malignant brain tumors. Cancer 88:637–647
Fortin D, McAllister LD, Nesbit G et al (1999) Unusual cervical spinal cord toxicity associated with intra-arterial carboplatin, intra-arterial or intravenous etoposide phosphate, and intravenous cyclophosphamide in conjunction with osmotic blood brain-barrier disruption in the vertebral artery. Am J Neuroradiol 20:1794–1802
Boulikas T (2007) Molecular mechanisms of cisplatin and its liposomally encapsulated form, Lipoplatin™. Lipoplatin™ as a chemotherapy and antiangiogenesis drug. Cancer ther 5:349–376
Boulikas T, Vougiouka M (2003) Cisplatin and platinum drugs at the molecular level. (Review). Oncol Rep 10:1663–1682
Yang L, Douple EB, O’Hara JA et al (1995) Enhanced radiation-induced cell killing by carboplatin in cells of repair-proficient and repair-deficient cell lines. Radiat Res 144:230–236
Zheng Y, Hunting DJ, Ayotte P et al (2008) Role of secondary low-energy electrons in the concomitant chemoradiation therapy of cancer. Phys Rev Lett 100:198101
Sanche L (2012) Nanoscale dynamics of radiosensitivity: role of low energy electrons. Radiation damage in biomolecular systems. Springer, Netherlands, pp 3–44. doi:10.1007/978-94-007-2564-5
Maeda H, Wu J, Sawa T et al (2000) Tumor vascular permeability and the EPR effect in macromolecular therapeutics: a review. J Control Release 65:271–284
Kaasgaard T, Andresen TL (2010) Liposomal cancer therapy: exploiting tumor characteristics. Expert Opin Drug Deliv 7:225–243. doi:10.1517/17425240903427940
Barth RF (1998) Rat brain tumor models in experimental neuro-oncology: the 9L, C6, T9, F98, RG2 (D74), RT-2 and CNS-1 gliomas. J Neurooncol 36:91–102
Mathieu D, Lecomte R, Tsanaclis AM et al (2007) Standardization and detailed characterization of the syngeneic Fischer/F98 glioma model. Can J Neurol Sci 34:296–306
Blanchard J, Mathieu D, Patenaude Y et al (2006) MR-pathological comparison in F98-Fischer glioma model using a human gantry. Can J Neurol Sci 33:86–91
Fortin D, Adams R, Gallez A (2004) A blood-brain barrier disruption model eliminating the hemodynamic effect of ketamine. Can J Neurol Sci 31:248–253
Charest G, Sanche L, Fortin D et al (2012) Glioblastoma treatment: bypassing the toxicity of platinum compounds by using liposomal formulation and increasing treatment efficiency with concomitant radiotherapy. Int J Radiat Oncol Biol Phys. doi:10.1016/j.ijrobp.2011.10.054
Blanchette M, Pellerin M, Tremblay L et al (2009) Real-time monitoring of gadolinium diethylenetriamine penta-acetic acid during osmotic blood-brain barrier disruption using magnetic resonance imaging in normal wistar rats. Neurosurgery 65:344–550. doi:10.1227/01.NEU.0000349762.17256.9E
Blanchette M, Fortin D (2011) Blood-brain barrier disruption in the treatment of brain tumors. Methods Mol Biol 686:447–463. doi:10.1007/978-1-60761-938-3_23
Charest G, Mathieu D, Lepage M et al (2009) Polymer gel in rat skull to assess the accuracy of a new rat stereotactic device for use with the Gamma Knife. Acta Neurochir (Wien) 151:677–683. doi:10.1007/s00701-009-0298-1
Charest G, Paquette B, Mathieu D (2011) Applications of Gamma Knife radiosurgery for experimental investigations in small animal models. Gamma Knife radiosurgery. Karger Publisher, Switzerland, pp 157–180
Henson JW (2006) Treatment of glioblastoma multiforme: a new standard. Arch Neurol 63:337–341. doi:10.1001/archneur.63.3.337
Newton HB (2005) Intra-arterial chemotherapy of primary brain tumors. Curr Treat Options Oncol 6:519–530
Stathopoulos GP, Antoniou D, Dimitroulis J et al (2011) Comparison of liposomal cisplatin versus cisplatin in non-squamous cell non-small-cell lung cancer. Cancer Chemother Pharmacol 68:945–950. doi:10.1007/s00280-011-1572-5
Stathopoulos G, Stathopoulos J, Dimitroulis J (2012) Two consecutive days of treatment with liposomal cisplatin in non-small cell lung cancer 4:1013–1016
Desmarais G, Fortin D, Bujold R et al (2012) Infiltration of glioma cells in brain parenchyma stimulated by radiation in the F98/Fischer rat model. Int J Radiat. doi:10.3109/09553002.2012.692495
Sheikh-Hamad D (2008) Cisplatin-induced cytoxicity: is the nucleus relevant? Am J Physiol Renal Physiol 295:F42–F43. doi:10.1152/ajprenal.90293.2008
Yu F, Megyesi J, Price PM (2008) Cytoplasmic initiation of cisplatin cytotoxicity. Am J Physiol Renal Physiol 295:F44–F52. doi:10.1152/ajprenal.00593.2007
Biston MC, Joubert A, Charvet AM et al (2009) In vitro and in vivo optimization of an anti-glioma modality based on synchrotron X-ray photoactivation of platinated drugs. Radiat Res 172:348–358. doi:10.1667/RR1650.1
Huo T, Barth RF, Yang W et al (2012) Preparation, biodistribution and neurotoxicity of liposomal cisplatin following convection enhanced delivery in normal and F98 glioma bearing rats. PLoS One 7:e48752. doi:10.1371/journal.pone.0048752
Acknowledgments
This work was supported by Canadian Institutes of Health Research (Grant No. MOP 81356). David Fortin, David Mathieu, Benoit Paquette and Léon Sanche are members of the Centre de recherche Clinique-Étienne Lebel supported by the Fonds de la Recherche en Santé du Québec.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Charest, G., Sanche, L., Fortin, D. et al. Optimization of the route of platinum drugs administration to optimize the concomitant treatment with radiotherapy for glioblastoma implanted in the Fischer rat brain. J Neurooncol 115, 365–373 (2013). https://doi.org/10.1007/s11060-013-1238-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-013-1238-8