Abstract
Primary intracranial germ-cell tumors are rare tumors primarily of adolescence, and literature on this disease in adults is scarce. The available evidence on intracranial germ-cell tumors is reviewed with a focus on adult patients whenever possible, and used to make suggestions for diagnosis and treatment. Diagnostic and treatment algorithms were developed to provide an evidence-based backbone to base treatment on in adult patients with a (suspected) primary intracranial germ-cell tumor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary intracranial germ-cell tumors (GCT) are rare tumors primarily of adolescence with an incidence of 0.07–0.1 per 100,000 per year [1]. The majority of patients (60–70 %) is aged under 20 and 53 % of patients is between 10 and 19 years at diagnosis [1]. Given the rarity of this disease, especially in adults, literature for this patient population is scarce. Prospective studies have not been performed in adults and even in children only non-randomized studies have been published. The current review aims to provide an evidence-based backbone for evaluation and treatment decisions in adult patients with primary intracranial GCTs.
We performed a pub-med search utilizing the following terms: “intracranial” or “CNS”, and “germ cell”, “germ-cell”, “germcell” or “germinoma”. Selection criteria were: humans, clinical trial, randomized controlled trial, article, consensus, review, meta-analysis or guideline and being written in English. Studies were included if they reported on at least 15 patients unless they concerned only a subgroup such as patients with bifocal GCT or pure teratoma. If multiple studies reported similar results a selection was made to minimize redundancy.
We found no evidence, in the limited available data on adult patients with GCTs, that treatment results in children differed from those in adults, but it is likely that toxicity of treatment differs between adults and (young) children.
Intracranial GCTs are heterogenous with respect to histology, biological profile, response to treatment and secretion of tumor markers [α-fetoprotein (AFP) and β-human chorionic gonadotropin (β-HCG)] into serum and/or cerebrospinal fluid (CSF). The majority are located in the pineal and/or supra-sellar regions [2]. The incidence ratio in men:women is 10:1 in pineal region GCTs [1]. Two main groups are distinguished: the germinomas and the non-germinomatous germ-cell tumors (NGGCT). Prognosis is highly variable and depends on histology and dissemination.
Origin, classification and molecular genetics
Germ-cell tumors of the CNS have been hypothesized to originate from primordial germ-cells that either migrated in aberrant fashion, or homed to the embryonic CNS rather than the developing genital ridges. An alternative hypothesis is that intracranial GCTs are derived from neural stem cells that have acquired pluripotent capacity. The molecular pathways leading to oncogenesis of GCTs of the CNS are not known but a pluripotent cell of origin may help to explain the histological heterogeneity within mixed GCTs [2, 3]. Up till now, classification of (intracranial) GCTs is based on their histopathological features. Germinoma is the most common subtype accounting for 70–80 % of the GCTs and is histologically identical to testicular seminoma and dysgerminoma of the ovary [2, 4]. The NGGCT subtypes are shown in Table 1. Accurate histological (sub) classification of GCTs of the CNS is critical for treatment planning and prognosis. While germinoma and teratoma are frequently encountered as pure tumor types, other intracranial GCTs are often of mixed histologic composition.
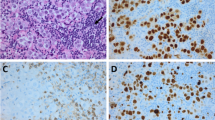
Most GCTs show immunohistochemical staining for placenta-like alkaline phophatase (PLAP). Germinomas usually express c-Kit (CD117), the receptor for stem cell factor, an important mitogen for normal germ-cells. Embryonal carcinomas are frequently CD30 positive. Teratomas by definition show components of all three germ layers which may be mature and/or immature in aspect. Examples of mature components are epidermis with skin appendages (incl. hair follicles/hair), teeth, cartilage, bone, glial and thyroid tissue. Immature neural tissue with neurotubular structures is frequently seen in immature teratomas [2, 3].
Germ-cell tumors of the CNS (beyond early childhood) show complex chromosomal anomalies including gains of chromosomes 12p, 8q, 1p and X, as well as losses of 11q, 13, and 18q. Whether 12p gain, isochromosome 12p formation, and X duplication, frequently present in testicular and mediastinal GCTs, occur at comparably high frequency in CNS tumors is debated. Klinefelter syndrome (47, XXY) is associated with an increased risk of intracranial GCT. Up till now, the contribution of molecular analysis in the diagnosis and further characterization of GCTs has been limited [2, 3].
Clinical presentation and diagnostic investigations
Clinical presentation
Symptoms and signs at presentation of GCTs are dependent on size of the tumor, site of involvement and histological tumor type. Typical locations are the pineal (40–60 %) and suprasellar regions (30–40 %), with at least 15 % of patients having tumors at multiple sites [1, 5]. Germinomas may present with bifocal location in the pineal and suprasellar region (25–30 % of cases) without metastases elsewhere in/around the CNS [6]. The vast majority of patients with tumors in the pineal region presents with symptoms and signs of intracranial hypertension and/or Parinaud’s syndrome and diplopia as a result of obstruction of the aquaduct, invasion of the tectal plate, and hydrocephalus [7]. The majority of patients with suprasellar tumors present with hypothalamo-hypophyseal insufficiency e.g. diabetes insipidus (DI) or visual disturbances caused by compression or invasion of the optic chiasm. Serum levels of cortisol, thyroid stimulating hormone (TSH), thyroxine or cortisol are abnormal in 40–60 % of patients and females older than 12 years frequently manifest with primary or secondary amenorrhea [5, 8]. Duration of symptoms before diagnosis is related to tumor location and type of symptoms. Especially DI may precede all other abnormalities and initially isolated DI may result in a prolonged interval of up to 3 years between initial symptom and diagnosis [7, 8].
Suggested evaluations in patients suspected of intracranial GCT are summarized in Fig. 1; suggested treatment is summarized in Figs. 2 and 3.
Imaging
MRI is the best imaging modality although CT can also contribute information on tumor location, cellular density, and calcification. Typical MRI abnormalities in typical locations (suprasellar, pineal, bifocal), in conjunction with clinical signs, are strongly suggestive of an intracranial GCT.
Germ-cell tumors other than teratomas usually appear as a solid mass, similar of intensity to the grey matter showing prominent enhancement after administration of contrast material. Teratomas frequently have heterogeneous signal characteristics due to fat, cysts and calcification, whereas choriocarcinoma has a high propensity for intratumoral hemorrhage [9]. Calcification of the pineal gland is a characteristic feature of GCTs but may also occur in healthy individuals. Germinoma may show more or less symmetric, ‘butterfly wing-like’ spread of the tumor from the pineal gland into the cerebral hemispheres [9]. Cases involving both the suprasellar region and the pineal gland without further dissemination are most likely to be germinomas [6]. Germinomas located in the basal ganglia may not enhance with gadolineum and a mass effect may be subtle or absent [10].
Germ-cell tumors are the most common tumor in the pineal region, accounting for 31–85 % of tumors [9]. The differential diagnosis includes pineal parenchymal tumors (pineocytoma, pineoblastoma, pineal parenchymal tumor of intermediate differentiation), a spectrum of gliomas (astrocytomas, ependymomas), meningeoma, and metastasis. In suprasellar sites the main differential diagnosis for small lesions is Langerhans Cell Histiocytosis and sarcoidosis, and for larger lesions low-grade glioma or craniopharyngeoma.
To determine the extent of macroscopic disease full craniospinal MR imaging is necessary.
Tumor markers
Germ-cell tumors may secrete the tumor markers AFP and β-HCG, which are not produced by any other primary intracranial tumor, into serum or CSF. One or both of these markers is elevated at diagnosis in the majority of patients with malignant NGGCTs, and in patients with germinoma β-HCG may be mildly elevated [11, 12]. The presence of elevated AFP in conjunction with consistent MRI appearances is considered sufficient for the diagnosis NGGCT without the need for biopsy [4, 13]. When initially elevated, tumor markers can also be used for response evaluation [12]. Therefore investigation of AFP and β-HCG in both serum and CSF is essential in patients suspected of harboring an intracranial GCT. Association of pathology with tumor markers and clinical behavior is shown in Table 2.
In pure germinomas AFP is never elevated. However, in 40–60 % of patients with germinoma mild elevation of HCG, more frequently in CSF than in serum (though generally less than 50 IU/l) is found [14]. Normal values for CSF HCG are lower in men than in women but always below 5 IU/l [15]. In a majority of subjects without GCTs CSF levels of HCG are higher than simultaneously obtained serum levels; therefore a higher CSF than serum HCG, provided it is still within normal limits, is not a sign of a CNS GCT [15].
CSF examination
Germ-cell tumors may disseminate through the CSF and, rarely, extracranially. It is essential to stage patients completely before starting treatment. If possible, CSF should be sampled before neurosurgical intervention for pathologic examination and evaluation of tumor markers.
Tissue sampling
Pathological diagnosis should be obtained in all patients except those with typical MRI findings and elevated serum and/or CSF AFP (>25 μg/l) (diagnosis NGGCT) [4, 13, 16]. In children with typical bifocal disease (pineal and suprasellar only) with normal AFP some authors also accept the diagnosis of germinoma without biopsy, but it is questionable whether this is also acceptable in adults [17].
Systemic evaluation
Presentation of a systemic GCT with an intracranial metastasis is exceedingly rare. Nevertheless, given the clinical consequences of concurrent systemic disease, CT evaluation of chest and abdomen and, in men, testicular ultrasonography is advisable.
Treatment
Neurosurgery
Given the radio- and chemo-sensitivity of most GCTs the value of extensive resection up-front is under debate. In patients with germinoma, resection carries the risk of neurological or endocrinological deterioration and has not led to survival benefit [18]. In NGGCT surgical resection does appear to improve outcome but especially after delayed, second look surgery rather than up-front resection [4, 16, 19, 20]. In our opinion, therefore, the role of initial neurosurgery in patients with a suspected GCT consists of a biopsy in order to confirm the diagnosis and treatment of hydrocephalus if present.
Tumor biopsy
Biopsy can be performed either with neuronavigation guided techniques, stereotactic procedures or via an endoscopic approach [21]. A disadvantage of biopsy is the risk of sampling error, especially in patients with a mixed GCT, but this risk is considered to be low [16, 22].
Treatment of hydrocephalus
In case of hydrocephalus, CSF shunting may be necessary. An option is to place a ventriculoperitoneal shunt, although if technically possible, an endoscopic third ventriculostomy is preferable. An additional benefit of neuro-endoscopy is the possibility to simultaneously perform tumor biopsy [21, 23]. CSF can be sampled for assessment of tumor markers and cytology during a neuroendoscopic procedure or ventriculoperitoneal shunt placement. Whenever possible CSF should be collected before biopsy or surgery of the tumor.
Extensive resection
In the following cases an extensive resection is indicated:
-
1)
Patients who suffer acute obstructive visual deteroriation from a suprasellar mass.
-
2)
Proven mature teratomas (after a previous biopsy) with normal tumor markers. In these patients gross total resection is curative and no further interventions are required.
-
3)
Patients with a NGGCT and a single residual mass after chemotherapy. The tumor recurrence rate is higher and the outcome is worse when compared with patients who do not have a residue [19]. Some NGGCTs are relatively resistant to conventional chemotherapy and radiotherapy; in these cases total resection by second look operation improves disease control [4]. Furthermore, in mixed tumors the residual tumor may be a mature teratoma, for which resection may be curative even if the residual lesion progresses [16, 24, 25].
-
4)
Patients with localized NGGCT who do not respond to chemoradiotherapy.
Radiotherapy
Germinoma
Only one study on radiotherapy for germinoma in adults has been published; it reports on 10 patients with a median age of 24 years and results were similar to those in children [26]. In general, over 90 % of patients with a germinoma can be cured with radiotherapy alone in the form of craniospinal irradiation (CSI) [27–29], whole brain irradiation [30], or whole-ventricle irradiation [31, 32]. Irradiation of the entire craniospinal axis has been abandoned for reasons of significant endocrine and neurocognitive toxicities and based on equivalent control rates with the use of limited irradiation to the intracranial ventricular system in patients with localised disease [27, 28, 33, 34]. The choice of whole-ventricle irradiation is based on the natural spread of germinoma, which is believed to be along the wall of the ventricles, and the fact that after focal irradiation the majority of relapses occur in the periventricular area [35].
For germinoma in the basal ganglia, previously thought to require whole brain irradiation, irradiation of tumor and ventricles seems also to be sufficient, as is the case for bifocal germinoma provided no other dissemination is present [6, 10, 17].
Although various radiation doses have been utilized, a dose of 24 Gy to the ventricular system with a 16 Gy boost to the tumor seems to be sufficient in patients with localized germinoma [33, 36]. In patients with spinal metastases or positive CSF suggested treatment is CSI at the same dose with the boost given both to the primary tumor and the metastases [37–39]. Incompletely staged germinoma should also receive CSI. If a component of immature teratoma exists, either incompletely or not resected, an increase of tumorbed dose boost up to 54.4 Gy has been advocated [16, 39].
Non-germinomatous germ-cell tumors
For NGGCTs, radiation therapy alone is rarely curative; 5 year survival is reported between 35 and 60 % [5, 40]. Combining radiotherapy with platinum-based chemotherapy, however, results in improved survival [15, 16]. A dose higher than 50 Gy should be given to the local tumor bed [39, 41, 42]. For non-metastasised tumors focal irradiation appears to be sufficient when combined with platinum-based chemotherapy [38]. For patients with metastatic disease CSI (30 Gy) with a boost to the tumorbed (24 Gy) is advised as increased recurrences have been reported after focal irradiation [43, 44].
Chemotherapy
Germinoma
In children, cognitive and endocrine toxicity of radiotherapy [45], led to investigation of chemotherapy treatment, either alone or in combination with reduced dose and/or field radiation [35, 37, 41, 46–48]. However, despite good response rates to chemotherapy, elimination of radiotherapy or even limiting the radiation field to the tumor bed led to higher rates of relapse, with a majority of recurrences in the ventricles [20, 35, 47]. Cognitive function seems largely preserved after reduced dose whole-ventricle irradiation [49]. In adults, tolerance of radiotherapy, especially in limited dose and field as is sufficient in germinoma, is acceptable, while chemotherapy-related toxicity is greater than in children. The rationale to replace radiotherapy with chemotherapy is therefore largely absent and in our opinion treatment with chemotherapy should be reserved for patients participating in clinical trials.
Non-germinomatous germ-cell tumors
Analogous to extracranial NGGCTs, primary intracranial NGGCTs are highly responsive to platinum-based chemotherapy, with response rates of 68–78 % in prospective studies utilizing chemotherapy only [50, 51]. However, chemotherapy alone is associated with relapse rates of 50–70 % [20, 50]. In non-randomized studies various regimens of chemotherapy in association with radiotherapy have been tested. Incorporation of cisplatin at a minimum cumulative dose of 400 mg/m2 was prognostically favourable, and platinum-based chemotherapy followed by radiotherapy has improved survival rates with overall survival (OS) 65–75 %. [20, 42, 43]
Recently two large cooperative studies have provided updated data. In the SIOP-CNS-GCT 96 trial, 197 patients with intracranial NGGCT were treated with four cycles of cisplatin, etoposide and ifosfamide (PEI). In non-metastatic disease, focal irradiation with 54 Gy was then administered, while patients with metastatic disease were treated with 30 Gy CSI and a 24 Gy boost to all sites of visible tumor on MRI. Five year progression free survival (PFS) (68 %) and OS (74 %) were similar in patients with localised and disseminated disease, with only 5 patients suffering a distant relapse after focal irradiation [38]. A Japanese cooperative study in which 67 patients with NGGCT were treated with carboplatin and etoposide followed by risk adapted radiotherapy and then PEI chemotherapy showed similar results although the risk categories used are not fully comparable to those in the SIOP study [52].
Thus the combination of radiotherapy with platinum-based chemotherapy has now become the treatment standard in intracranial NGGCTs. Whether the use of high-dose chemotherapy plus autologous haematopoietic stem cell support given as first-line therapy increases survival is not known and this is currently regarded as experimental. In patients with poor risk primary gonadal NGGCTs high-dose therapy with stem cell support has not resulted in improved survival in first-line treatment [53, 54].
Salvage therapy
Salvage therapies for relapsed GCTs include surgery, local or whole neuroaxis irradiation, and myeloablative chemotherapy with autologous blood stem cell rescue. Both in primary gonadal and in primary intracranial NGGCT limited data suggest that survival may improve with early intensification of salvage treatment using high-dose chemotherapy [55, 56]. Further studies are needed to evaluate this treatment.
Follow-up
Most relapses of CNS GCTs occur within 5 years and at the primary tumor site. However, in up to 30 % of cases distant metastases develop, mostly within the nervous system [4, 57]. Overall median time to relapse is 12 months (range 7–120), but in germinoma median time to first recurrence was 50 months after initial treatment [4, 55, 58]. Therefore surveillance should be most intensive in the first year after treatment and should continue for at least 5 years, preferably 10 years. Generally, surveillance with both MR imaging and tumor markers, if initially elevated, is advised.
Prognosis
Prognosis is determined by pathology of the tumor, extent of disease and presence or absence of elevated tumor markers. In pure germinoma OS at 5 years is >90 % after radiotherapy only; (mildly) elevated β-HCG does not seem to influence this prognosis, although one small study in 12 patients did find a poorer prognosis in patients with elevated β-HCG in CSF [11, 12, 59]. Patients with mature teratoma achieve survival rates of 100 % at 5 years. In the other NGGCTs 5-year survival rates of up to 70 % have been reported after the combination of platinum-based chemotherapy and radiotherapy [4, 38]. Since elevated AFP is a marker of the NGGCTs this coincides with a poorer prognosis, but survival was also worse in NGGCT patients with initially elevated β-HCG after platinum chemotherapy-based treatment with a hazard ratio (HR) of death of 1.9 for patients with raised markers [12].
Conclusions
Adult intracranial GCTs are rare but treatment sensitive tumors. In the absence of studies in adults, suggestions for diagnostic evaluations and treatment are made based on extrapolation from studies in children and from testicular GCT. Given the rarity of (adult) intracranial GCTs randomized studies are unlikely to be feasible. Prospective registration of all intracranial GCT patients in national or supranational databases and treatment according to consensus-based guidelines should increase the body of knowledge and lead to improved outcomes in future.
References
McCarthy BJ, Shibui S, Kayama T, Miyaoka E, Narita Y, Murakami M, Matsuda A, Matsuda T, Sobue T, Palis BE, Dolecek TA, Kruchko C, Engelhard HH, Villano JL (2012) Primary CNS germ cell tumors in Japan and the United States: an analysis of 4 tumor registries. Neuro-Oncology 14:1194–1200
Rosenblum MK (2007) Germ cell tumors. In: Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (eds) WHO classification of tumours of the centrel nervous system. International Agency for Research on Cancer, Lyon, pp 198–204
Matsutani M (2005) Germ cell tumors. In: Berger MS, Prados MD (eds) Textbook of neuro-oncology. Elsevier, Philadelphia, pp 310–320
Kamoshima Y, Sawamura Y (2010) Update on current standard treatments in central nervous system germ cell tumors. Curr Opin Neurol 23:571–575
Matsutani M, Sano K, Takakura K, Fujimaki T, Nakamura O, Funata N, Seto T (1997) Primary intracranial germ cell tumors: a clinical analysis of 153 histologically verified cases. J Neurosurg 86:446–455
Weksberg DC, Shibamoto Y, Paulino AC (2012) Bifocal intracranial germinoma: a retrospective analysis of treatment outcomes in 20 patients and review of the literature. Int J Radiat Oncol Biol Phys 82:1341–1351
Crawford JR, Santi MR, Vezina G, Myseros JS, Keating RF, LaFond DA, Rood BR, MacDonald TJ, Packer RJ (2007) CNS germ cell tumor (CNSGCT) of childhood: presentation and delayed diagnosis. Neurology 68:1668–1673
Jorsal T, Rorth M (2012) Intracranial germ cell tumours. A review with special reference to endocrine manifestations. Acta Oncol 51:3–9
Blakeley JO, Grossman SA (2006) Management of pineal region tumors. Curr Treat Options Oncol 7:505–516
Sonoda Y, Kumabe T, Sugiyama S, Kanamori M, Yamashita Y, Saito R, Ariga H, Takai Y, Tominaga T (2008) Germ cell tumors in the basal ganglia: problems of early diagnosis and treatment. J Neurosurg Pediatr 2:118–124
Ogino H, Shibamoto Y, Takanaka T, Suzuki K, Ishihara S, Yamada T, Sugie C, Nomoto Y, Mimura M (2005) CNS germinoma with elevated serum human chorionic gonadotropin level: clinical characteristics and treatment outcome. Int J Radiat Oncol Biol Phys 62:803–808
Kim A, Ji L, Balmaceda C, Diez B, Kellie SJ, Dunkel IJ, Gardner SL, Sposto R, Finlay JL (2008) The prognostic value of tumor markers in newly diagnosed patients with primary central nervous system germ cell tumors. Pediatr Blood Cancer 51:768–773
Calaminus G, Bamberg M, Harms D, Jurgens H, Kortmann RD, Sorensen N, Wiestler OD, Gobel U (2005) AFP/beta-HCG secreting CNS germ cell tumors: long-term outcome with respect to initial symptoms and primary tumor resection. Results of the cooperative trial MAKEI 89. Neuropediatrics 36:71–77
Allen J, Chacko J, Donahue B, Dhall G, Kretschmar C, Jakacki R, Holmes E, Pollack I (2012) Diagnostic sensitivity of serum and lumbar CSF bHCG in newly diagnosed CNS germinoma. Pediatr Blood Cancer 59:1180–1182
Tian C, Shi Q, Xiao G, Pu C, Huang X, Yu S, Zhang J (2011) CSF and serum hCG in patients without gestational and neoplastic hCG-secretion. Scand J Clin Lab Invest 71:264–268
Weiner HL, Finlay JL (1999) Surgery in the management of primary intracranial germ cell tumors. Childs Nerv Syst 15:770–773
Lafay-Cousin L, Millar BA, Mabbott D, Spiegler B, Drake J, Bartels U, Huang A, Bouffet E (2006) Limited-field radiation for bifocal germinoma. Int J Radiat Oncol Biol Phys 65:486–492
Sawamura Y, de Tribolet N, Ishii N, Abe H (1997) Management of primary intracranial germinomas: diagnostic surgery or radical resection? J Neurosurg 87:262–266
Czech T, Nicholson J, Frappaz D, Kortmann RD, Alapetite C, Garre ML, Ricardi U, Saran FH, Calaminus G (2012) Patients with intracranial non-germinomatous germ cell tumours (NGGCT) benefit from delayed surgery after neoadjuvant chemotherapy. Final results of SIOP CNS GCT 96. p i52
Kellie SJ, Boyce H, Dunkel IJ, Diez B, Rosenblum M, Brualdi L, Finlay JL (2004) Primary chemotherapy for intracranial nongerminomatous germ cell tumors: results of the second international CNS germ cell study group protocol. J Clin Oncol 22:846–853
Souweidane MM, Krieger MD, Weiner HL, Finlay JL (2010) Surgical management of primary central nervous system germ cell tumors: proceedings from the Second International Symposium on Central Nervous System Germ Cell Tumors. J Neurosurg Pediatr 6:125–130
Luther N, Edgar MA, Dunkel IJ, Souweidane MM (2006) Correlation of endoscopic biopsy with tumor marker status in primary intracranial germ cell tumors. J Neurooncol 79:45–50
Shono T, Natori Y, Morioka T, Torisu R, Mizoguchi M, Nagata S, Suzuki SO, Iwaki T, Inamura T, Fukui M, Oka K, Sasaki T (2007) Results of a long-term follow-up after neuroendoscopic biopsy procedure and third ventriculostomy in patients with intracranial germinomas. J Neurosurg 107:193–198
Friedman JA, Lynch JJ, Buckner JC, Scheithauer BW, Raffel C (2001) Management of malignant pineal germ cell tumors with residual mature teratoma. Neurosurgery 48:518–522
O’Callaghan AM, Katapodis O, Ellison DW, Theaker JM, Mead GM (1997) The growing teratoma syndrome in a nongerminomatous germ cell tumor of the pineal gland: a case report and review. Cancer 80:942–947
Foote M, Millar BA, Sahgal A, Menard C, Payne D, Mason W, Laperriere N (2010) Clinical outcomes of adult patients with primary intracranial germinomas treated with low-dose craniospinal radiotherapy and local boost. J Neurooncol 100:459–463
Bamberg M, Kortmann RD, Calaminus G, Becker G, Meisner C, Harms D, Gobel U (1999) Radiation therapy for intracranial germinoma: results of the German cooperative prospective trials MAKEI 83/86/89. J Clin Oncol 17:2585–2592
Maity A, Shu HK, Janss A, Belasco JB, Rorke L, Phillips PC, Sutton LN, Goldwein JW (2004) Craniospinal radiation in the treatment of biopsy-proven intracranial germinomas: twenty-five years’ experience in a single center. Int J Radiat Oncol Biol Phys 58:1165–1170
Schoenfeld GO, Amdur RJ, Schmalfuss IM, Morris CG, Keole SR, Mendenhall WM, Marcus RB Jr (2006) Low-dose prophylactic craniospinal radiotherapy for intracranial germinoma. Int J Radiat Oncol Biol Phys 65:481–485
Shikama N, Ogawa K, Tanaka S, Toita T, Nakamura K, Uno T, Ohnishi H, Itami J, Tada T, Saeki N (2005) Lack of benefit of spinal irradiation in the primary treatment of intracranial germinoma: a multiinstitutional, retrospective review of 180 patients. Cancer 104:126–134
Nguyen QN, Chang EL, Allen PK, Maor MH, Ater JL, Mahajan A, Wolff JE, Weinberg JS, Woo SY (2006) Focal and craniospinal irradiation for patients with intracranial germinoma and patterns of failure. Cancer 107:2228–2236
Haas-Kogan DA, Missett BT, Wara WM, Donaldson SS, Lamborn KR, Prados MD, Fisher PG, Huhn SL, Fisch BM, Berger MS, Le QT (2003) Radiation therapy for intracranial germ cell tumors. Int J Radiat Oncol Biol Phys 56:511–518
Ogawa K, Shikama N, Toita T, Nakamura K, Uno T, Onishi H, Itami J, Kakinohana Y, Kinjo T, Yoshii Y, Ito H, Murayama S (2004) Long-term results of radiotherapy for intracranial germinoma: a multi-institutional retrospective review of 126 patients. Int J Radiat Oncol Biol Phys 58:705–713
Wolden SL, Wara WM, Larson DA, Prados MD, Edwards MS, Sneed PK (1995) Radiation therapy for primary intracranial germ-cell tumors. Int J Radiat Oncol Biol Phys 32:943–949
Alapetite C, Brisse H, Patte C, Raquin MA, Gaboriaud G, Carrie C, Habrand JL, Thiesse P, Cuilliere JC, Bernier V, Ben-Hassel M, Frappaz D, Baranzelli MC, Bouffet E (2010) Pattern of relapse and outcome of non-metastatic germinoma patients treated with chemotherapy and limited field radiation: the SFOP experience. Neuro-Oncology 12:1318–1325
Shibamoto Y, Takahashi M, Abe M (1994) Reduction of the radiation dose for intracranial germinoma: a prospective study. Br J Cancer 70:984–989
Aoyama H, Shirato H, Ikeda J, Fujieda K, Miyasaka K, Sawamura Y (2002) Induction chemotherapy followed by low-dose involved-field radiotherapy for intracranial germ cell tumors. J Clin Oncol 20:857–865
Calaminus G, Frappaz D, Kortmann RD, Alapetite C, Garre ML, Ricardio U, Saran FH, Nicholson J (2012) Risk adapted irradiation is feasible in intracranial non-germinomatous germ cell tumours (NGGCT): final results of SIOP CNS GCT 96. p i51
Buckner JC, Peethambaram PP, Smithson WA, Groover RV, Schomberg PJ, Kimmel DW, Raffel C, O’Fallon JR, Neglia J, Shaw EG (1999) Phase II trial of primary chemotherapy followed by reduced-dose radiation for CNS germ cell tumors. J Clin Oncol 17:933–940
Jennings MT, Gelman R, Hochberg F (1985) Intracranial germ-cell tumors: natural history and pathogenesis. J Neurosurg 63:155–167
Matsutani M (2001) Combined chemotherapy and radiation therapy for CNS germ cell tumors–the Japanese experience. J Neurooncol 54:311–316
Robertson PL, DaRosso RC, Allen JC (1997) Improved prognosis of intracranial non-germinoma germ cell tumors with multimodality therapy. J Neurooncol 32:71–80
Calaminus G, Bamberg M, Jurgens H, Kortmann RD, Sorensen N, Wiestler OD, Gobel U (2004) Impact of surgery, chemotherapy and irradiation on long term outcome of intracranial malignant non-germinomatous germ cell tumors: results of the German Cooperative Trial MAKEI 89. Klin Padiatr 216:141–149
Kim JW, Kim WC, Cho JH, Kim DS, Shim KW, Lyu CJ, Won SC, Suh CO (2012) A multimodal approach including craniospinal irradiation improves the treatment outcome of high-risk intracranial nongerminomatous germ cell tumors. Int J Radiat Oncol Biol Phys 84(3):625–631
Sands SA, Kellie SJ, Davidow AL, Diez B, Villablanca J, Weiner HL, Pietanza MC, Balmaceda C, Finlay JL (2001) Long-term quality of life and neuropsychologic functioning for patients with CNS germ-cell tumors: from the First International CNS Germ-Cell Tumor Study. Neuro-Oncology 3:174–183
Bouffet E, Baranzelli MC, Patte C, Portas M, Edan C, Chastagner P, Mechinaud-Lacroix F, Kalifa C (1999) Combined treatment modality for intracranial germinomas: results of a multicentre SFOP experience. Societe Francaise d’Oncologie Pediatrique. Br J Cancer 79:1199–1204
Eom KY, Kim IH, Park CI, Kim HJ, Kim JH, Kim K, Kim SK, Wang KC, Cho BG, Jung HW, Heo DS, Kang HJ, Shin HY, Ahn HS (2008) Upfront chemotherapy and involved-field radiotherapy results in more relapses than extended radiotherapy for intracranial germinomas: modification in radiotherapy volume might be needed. Int J Radiat Oncol Biol Phys 71:667–671
Kellie SJ, Boyce H, Dunkel IJ, Diez B, Rosenblum M, Brualdi L, Finlay JL (2004) Intensive cisplatin and cyclophosphamide-based chemotherapy without radiotherapy for intracranial germinomas: failure of a primary chemotherapy approach. Pediatr Blood Cancer 43:126–133
Mabbott DJ, Monsalves E, Spiegler BJ, Bartels U, Janzen L, Guger S, Laperriere N, Andrews N, Bouffet E (2011) Longitudinal evaluation of neurocognitive function after treatment for central nervous system germ cell tumors in childhood. Cancer 117:5402–5411
Balmaceda C, Heller G, Rosenblum M, Diez B, Villablanca JG, Kellie S, Maher P, Vlamis V, Walker RW, Leibel S, Finlay JL (1996) Chemotherapy without irradiation—a novel approach for newly diagnosed CNS germ cell tumors: results of an international cooperative trial. The first International Central Nervous System Germ Cell Tumor Study. J Clin Oncol 14:2908–2915
da Silva NS, Cappellano AM, Diez B, Cavalheiro S, Gardner S, Wisoff J, Kellie S, Parker R, Garvin J, Finlay J (2010) Primary chemotherapy for intracranial germ cell tumors: results of the third international CNS germ cell tumor study. Pediatr Blood Cancer 54:377–383
Matsutani M (2012) Multi-institutional, prospective phase 2 study for primary intracranial germ cell tumors. German Medical Science GMS Publishing House, Düsseldorf, p i51
Motzer RJ, Nichols CJ, Margolin KA, Bacik J, Richardson PG, Vogelzang NJ, Bajorin DF, Lara PN Jr, Einhorn L, Mazumdar M, Bosl GJ (2007) Phase III randomized trial of conventional-dose chemotherapy with or without high-dose chemotherapy and autologous hematopoietic stem-cell rescue as first-line treatment for patients with poor-prognosis metastatic germ cell tumors. J Clin Oncol 25:247–256
Daugaard G, Skoneczna I, Aass N, De WR, De SM, Dumez H, Marreaud S, Collette L, Lluch JR, Bokemeyer C, Schmoll HJ (2011) A randomized phase III study comparing standard dose BEP with sequential high-dose cisplatin, etoposide, and ifosfamide (VIP) plus stem-cell support in males with poor-prognosis germ-cell cancer. An intergroup study of EORTC, GTCSG, and Grupo Germinal (EORTC 30974). Ann Oncol 22:1054–1061
Modak S, Gardner S, Dunkel IJ, Balmaceda C, Rosenblum MK, Miller DC, Halpern S, Finlay JL (2004) Thiotepa-based high-dose chemotherapy with autologous stem-cell rescue in patients with recurrent or progressive CNS germ cell tumors. J Clin Oncol 22:1934–1943
Simonelli M, Rosti G, Banna GL, Pedrazzoli P (2012) Intensified chemotherapy with stem-cell rescue in germ-cell tumors. Ann Oncol 23:815–822
Ogawa K, Toita T, Nakamura K, Uno T, Onishi H, Itami J, Shikama N, Saeki N, Yoshii Y, Murayama S (2003) Treatment and prognosis of patients with intracranial nongerminomatous malignant germ cell tumors: a multiinstitutional retrospective analysis of 41 patients. Cancer 98:369–376
Kamoshima Y, Sawamura Y, Ikeda J, Shirato H, Aoyama H (2008) Late recurrence and salvage therapy of CNS germinomas. J Neurooncol 90:205–211
Inamura T, Nishio S, Ikezaki K, Fukui M (1999) Human chorionic gonadotrophin in CSF, not serum, predicts outcome in germinoma. J Neurol Neurosurg Psychiatry 66:654–657
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bromberg, J.E.C., Baumert, B.G., de Vos, F. et al. Primary intracranial germ-cell tumors in adults: a practical review. J Neurooncol 113, 175–183 (2013). https://doi.org/10.1007/s11060-013-1114-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-013-1114-6