Abstract
Primary tumors and metastatic involvement of the central nervous system (CNS) lead to a multitude of symptoms and care needs. Patients and caregivers struggle with physical and psychological impairments, a shortened life expectancy and diverse palliative care needs. This study assesses the symptom burden and palliative care needs of patients with primary brain tumors and with metastatic brain tumors requiring inpatient hospital care. It is a retrospective analysis of patients with primary CNS tumors or cerebral metastases over a 6 month period. The data analysed included physical symptom burden and end of life care decisions such as health care proxy, transition to hospice and do-not-resuscitate orders. Hundred and sixty eight patients were included. The most common symptoms were gait impairment (65.5 %), cognitive/personality change (61.9 %), motor deficits (58.3 %), seizures (57.1 %) and delirium (27.4 %). Of the patients that died, 79 % had an appointed health care proxy, 79 % had hospice discussions, 70 % had a do-not-resuscitate order and 24 % received cancer directed therapy in the last month of life. There is a role for more aggressive palliative care support in patients living with primary or metastatic brain tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oncological involvement of the central nervous system (CNS) results in symptoms such as increased dependency on caregivers (physical and cognitive), personality changes, headaches, seizures and dysphagia [1–4] This occurs secondary to tumor growth and severe fatigue, cerebral radiation effects, chemotherapy induced toxicities and steroid or anticonvulsant side effects [1–4] Changes in cognitive function, behavior and personality may be especially difficult for caregivers to cope with and manage. These symptoms provide important areas for palliative intervention in the care of patients with cerebral metastases or primary CNS tumors.
The median survival for patients with cerebral metastases and maximal therapy is 7.1 months (in patients <65 years, Karnofsky performance status >70, controlled primary, no extracranial spread) [5]. Similarly, in patients living with low grade gliomas the median survival is 6 years from the time of diagnosis [6] and in patients living with grade III gliomas survival varies from 3 to 5 years [7]. High grade malignant CNS gliomas, treated with concomitant radiation therapy and temozolomide, have a median survival that remains at 14 months [8]. With the combination of rapid disease progression, a high burden of symptoms and a short life expectancy the need for expertise in palliative measures is paramount.
Recent retrospective analyses of the palliative care needs of patients with malignant gliomas or cerebral metastases at the end of life demonstrate that the most common symptoms were dysphagia, drowsiness, headache, seizures, agitation and delirium and death rattle Pace et al. [9–11] showed that emergence of symptoms such as drowsiness and dysphagia often triggered discussions regarding end of life decisions such as route of medication delivery, interruption of steroids, hydration and nutrition during the last 4 weeks of life [9]. Only 6 % of patients had established advance care directives to assist and guide substitute decision makers with care decisions [9]. However, drowsiness and dysphagia emerge most frequently within the last week of life [10]. Thus, while these symptoms may trigger important discussions regarding end-of-life care, it would appear that the discussions occur late in the disease trajectory.
While there is a growing body of literature concerning palliation of neurological patients, further evidence is required in order to determine the specific care needs, both symptomatic and with respect to advance care planning, of patients living with primary CNS tumors or cerebral metastases. The aim of the study is to assess the symptom burden and palliative care needs of a group of patients with primary brain tumors and with metastatic brain tumors requiring inpatient hospital care in order to more precisely determine the palliative care needs of this population throughout the spectrum of their illness.
Method
Standard protocol approvals, registrations, and patient consents
The Institutional Review Board at Memorial Sloan-Kettering Cancer Center approved the study. A waiver of the HIPAA authorization and informed consent for collection of existing data was obtained prior to initiation of the study. All data was de-identified prior to analysis.
The study is a retrospective descriptive assessment of all patients with primary brain tumors or metastatic brain tumors admitted to the neurology and neurosurgery inpatient services at Memorial Sloan-Kettering Cancer Center (New York, NY) between January 1, 2010 and June 30, 2010.
Data collection
Patients were identified by query of pre-existing institutional databases for the neurology and neurosurgery services. The total number of admission determined and the patients fulfilling the inclusion criteria were enumerated. Pertinent electronic records were reviewed by the authors (TG, JG). The data abstracted included: sex, primary cancer, age, age at diagnosis, duration of disease, age at time of death, location of death, cancer directed therapies including surgical resection, radiation and chemotherapy, evidence of resuscitation at the end of life, evidence of cancer directed therapy in the last month of life, health care proxy, palliative care consultation, hospice discussion and evidence of discussion regarding resuscitation wishes.
Data Analysis
Data on the following clinical symptoms were collected: falls, gait impairment, incontinence, spasticity, motor deficits, sensory disturbance, delirium, cognitive/personality change, aphasia, dysarthria, dysphagia, seizures, diplopia, visual changes, delirium, pain, headache and depression or anxiety. Cognitive/personality changes included memory impairment, altered personality and impaired activities of daily living for non-physical reasons. Gait impairment included the spectrum of patients with mild unsteadiness and inability to tandem gait to bed-bound patients. Sensory disturbances included objective physical examination findings and subjective paresthesias. Visual changes included loss of visual acuity or visual field deficits. Pain and headache were considered separately and patients with pain other than headache, either acute or chronic, were grouped together under ‘pain’. All symptoms occurred over the 6 month study period. Symptoms were included if they were either intermittent or persistent.
In the case of missing data, these data were excluded from the analysis. All data was analyzed in groups identified as World Health Organization (WHO) grade I/II tumors, WHO grade III/IV tumors, primary central nervous system lymphoma (PCNSL), metastatic brain tumors and as an entirety.
Statistical analysis
We analyzed variables associated with DNR status and time from last admission to death using PRISM version 5.0. Non-parametric data was analyzed using Mann–Whitney tests with two-tailed p-values <0.05 considered significant.
Patients
Inclusion criteria
Patients greater than 18 years admitted to the inpatient neurology or neurosurgery inpatient services between January and June of 2010. All patients had a primary brain tumor or a systemic cancer with an intracranial metastasis requiring admission.
Exclusion criteria
Patients less than 18 years of age and patients admitted to the inpatient neurology or neurosurgery services for other reasons including spinal cord tumors or peripheral nerve tumors.
Results
Patients
A total of 530 patients (770 admissions, 1.45 admissions per patient) were admitted to the inpatient neurology and neurosurgery services at Memorial Sloan-Kettering Cancer Center between January 1 and June 30 of 2010. One hundred and sixty-eight (168) patients satisfied the inclusion and exclusion criteria (Table 1). The mean age was 60.0 ± 13.8 years with the mean age at the time of diagnosis being 56.7 ± 15.2 years and the mean duration of disease being 3.6 years. There were 96 males (57.1 %) and 72 females (42.9 %). There were nine patients with grade I/II primary CNS tumors (5.4 %), 101 patients with grade III/IV primary CNS tumors (60.1 %), 34 patients with PCNSL (20.2 %) and 24 patients with cerebral metastases (14.3 %). Fifty-eight (34.5 % of 168) patients died during the study period. Please see Table 1 for details regarding patient demographics and subgroups.
Overall, 91 (54.2 %) patients were admitted for management of acute neurological symptoms, 31 (18.5 %) patients with otherwise stable disease were admitted for administration of inpatient chemotherapy and 46 (27.4 %) of patients were transitioned to hospice care during the 6 month study period (see Fig. 1).
Group observations and patterns of end of life discussions
The burden of symptoms is shown in detail in Fig. 2. The most common symptoms were gait impairment (65.5 %), cognitive/personality change (61.9 %), motor deficits (58.3 %), seizures (57.1 %) and delirium (27.4 %). The three most common symptoms in each subgroup of patients were (Table 2): (1) WHO grade I/II tumors—seizures (55.6 %), cognitive/personality change (33.3 %) and headache (33.3 %); (2) WHO grade III/IV tumors—cognitive/personality change (66.3 %), seizures (66.3 %), motor deficits (59.4 %) and gait impairment (59.4 %); (3) PCNSL—gait impairment (73.5 %), cognitive/personality change (67.6 %) and motor deficits (58.8 %); and (4) metastatic brain tumors—gait impairment (91.7 %), motor deficits (66.7 %) and seizures (50.0 %).
Within the group of patients that died, a palliative care consultation was initiated in seven (12.1 %) patients. Prior to death, 46 (79.3 %) patients had a formally appointed health care proxy. Hospice discussions were initiated in 46 (79.3 %) patients a mean of 37.5 ± 33.4 days prior to death (median = 28d; range = 1–140d). Forty (70.0 %) of deceased patients had a do-not-resuscitate established a mean of 48.8 ± 44.9 days prior to the time of death (median = 39d; range = 1–198d). Fourteen patients (24.1 %) received cancer directed treatment during the last 30 days of life. Please see Table 3 for details regarding end of life discussions.
Patients with a DNR order (mean 61.3, range 30.0–90.0, 95 % CI = 56.3–66.2) had a lower median KPS at the time of their last clinic visit prior to final admission than those without a DNR order (mean 74.3, range 50.0–100.0, 95 % CI = 71.0–77.6; p < 0.00001). There was no significant association between DNR status and age. There was no significant association between marital status, pain, headache, aphasia, cognitive dysfunction, incontinence, falls or use of opioids with time from last admission to death.
Primary brain tumors (not including PCNSL)
The largest subgroup of patients was made up of WHO grade III/IV brain tumors (101 patients, 70.1 % of 168 patients) including glioblastoma, anaplastic oligodendroglioma, anaplastic astrocytoma, anaplastic meningioma and mixed anaplastic glioma. The majority of these patients underwent surgical resection (80.2 %), chemotherapy (87.1 %) and radiation (85.1 %). Forty-three patients (42.6 %) of the patients with WHO grade III/IV tumors died during the course of the study. Twenty-one percent (20.9 %) of patients with WHO grade III/IV tumors died at home, 34.9 % died with outpatient hospice support, 32.6 % died in an inpatient hospice facility and 2.3 % died in a nursing home. Fifteen percent (15 %) of patients had no documented end-of-life discussions, 77.1 % had an appointed health care proxy, 64.6 % had a do-not-resuscitate order and 85.4 % had a hospice care discussion (see Table 3 for details).
There were only nine (8.9 % of 101) patients with WHO grade I/II tumors (ependymoma, low grade cerebellar astrocytoma, grade II astrocytoma, meningioma, recurrent ganglioglioma, pleomorphic xanthroastrocytoma, pilocytic astrocytoma). One hundred percent of this group had a surgical resection, while 55.6 % received radiation therapy and 33.3 % received chemotherapy. Two patients (22.2 % of nine patients) died during the course of the study. Both patients had an appointed health care proxy and one patient had a documented hospice discussion (Table 3).
Primary CNS lymphoma
There were 34 (23.6 % of 168) patients with PCNSL. One hundred percent of these patients were treated with chemotherapy and 23.5 % of this group had a surgical resection or radiation therapy. Three (8.8 % of 34) patients died during the study period. All three patients had a documented resuscitation order and two had both an appointed health care proxy and a hospice discussion (Table 3).
Metastatic brain tumors
Twenty-four (14.3 % of 168) patients with metastatic brain tumors were included. The range of primary cancers included B cell lymphoma, breast cancer, melanoma, non small cell lung cancer, small cell lung cancer and adenocarcinoma of unknown primary. Of these patients, 91.7 % received chemotherapy directed at the primary systemic cancer, 75.0 % received radiation therapy and 37.5 % had a surgical resection of the metastasis during the course of the illness. Ten (41.7 % of 24) patients died during the study period. Thirty percent of the patients with metastatic disease had a palliative care consultation, 90 % had an appointed health care proxy, 50.0 % had a hospice discussion and 80.0% had a resuscitation order (Table 3).
Conclusions
These data suggest that patients living with primary CNS tumors and cerebral metastases have a high degree of symptom burden. The most common symptoms in this population are gait impairment, cognitive/personality change, motor deficits, seizures and delirium. The literature in palliative care in the brain tumor population has focused upon seizures, cognitive changes, steroid side effects, thromboembolism and the management of cerebral edema [1, 2, 9, 12, 13]. While these topics are important, there is a plethora of other symptoms, including gait impairment and falls, aphasia, cognitive impairment, that cause significant distress and impair quality of life. Palliative care services are underutilized despite a high number of patients being admitted to hospital when they are approaching the end of life. We recognize that the population of patients included in this study (all patients with primary or metastatic brain tumors admitted to the inpatient neurology and neurosurgery inpatient services over a 6 month period) is diverse and represents patients along a spectrum of disease from early diagnosis to end of life. This population was chosen in order to assess the total symptom burden in this population, not simply the symptom burden in the last few weeks of life. There is little data to demonstrate the timing of end of life care discussions in this population. Including the complete spectrum of patients in this study allowed us to comment on the timing of these discussions and to highlight the variability in the timing of end of life discussions (see below for further discussion).
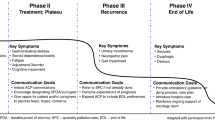
In our study, 32 % of patients with primary CNS tumors had aphasia or dysarthria (12 %). A further 61.9 % of patients live with personality changes or cognitive impairment during their time of illness. Aphasia, dysarthria, personality changes and cognitive impairment may lead to impaired communication, which presents a specific challenge in this population. At different stages of illness, communication about complex topics and end of life decision-making is required and may be impaired due to an individual’s inability to adequately express themselves or to fully understand the content of a discussion. Difficulty with speech, limited communication or aphasia affects as many as 64 % of patients in the final months of life [14]. Despite high rates of impaired communication, studies show that speech and language therapies are underutilized in patients living with brain tumors [14].
The most frequent end of life decisions made within the last 4 weeks of life in patients with brain tumors focus upon hydration, nutrition, steroid interruption, advance directives and palliative sedation [9]. By then, patients may be cognitively or psychologically unable to express what is most distressing for them or what they fear about the future. advocate for early discussions with patients when communication remains intact Watanabe and MacLeod [15].
Mental competence is very important to patients living with brain tumors and to their caregivers [11]. The evidence suggests that tumor size and grade are associated with worse neuropsychological test scores [16]. However, there is conflicting evidence regarding the effects of tumor resection on cognition: tumor resection has the potential to either improve (24 %) or to further impair (38 %) neuropsychological test results [16]. Both radiation therapy and chemotherapy also contribute to neurotoxicity and potential cognitive impairment [17]. Patients place so much importance on mental competence that they feel that it directly determines their quality of life. These same patients state that quality of life is more important for them than is prolongation of life [11]. In addition to impacting quality of life, impaired cognition impacts the decision-making capacity of patients living with malignant gliomas. Many of these patients have capacity compromise in understanding, reasoning and appreciation as measured by the capacity to consent to treatment instrument [18]. There is no impairment in the ability to express a treatment choice, however, this is a less complex aspect of medical decision-making. Cognitive predictors for understanding are short-term verbal acquisition, recall and semantic word fluency [18]. These aspects of cognition are impaired in patients with aphasia, which highlights the need for further study on impaired cognition and communication on end of life decision-making in patients living with brain tumors.
Patients and families rarely discuss end of life issues with physicians at a time when the patient retains competence [9, 19, 20]. However, patients with brain tumors and their caregivers value discussions with health care professionals about death and dying and, in fact, many find such discussions to be therapeutic [11]. The same study demonstrated that patients living with brain tumors value their quality of life very highly [11]. A qualitative study addressing quality of life in patients with brain metastases showed that patients feared being a burden on their families, that they did share decision making with their family but often felt that they had a lack of understanding of their disease [21]. It remains to be determined if increasing the exposure of this patient population to palliative care services would stimulate earlier end of life discussions enabling patients to take a more active role in the decision making process.
It is known that inpatients with primary malignant brain tumors admitted to a general hospital account for 4 % of all inpatients with palliative care needs [22]. While 4 % of patients represents a small proportion of all patients with palliative care needs, this group of patients is known to have some of the highest palliative care needs. Patients living with brain metastases also account for approximately 38 % of patients in a general hospital with palliative care needs [22]. Our study shows that almost one-third (27 %) of patients with primary brain tumors or brain metastases admitted to the neurosciences inpatient unit have acute palliative care needs and were transitioned from acute care hospital to hospice services during the course of the study. Oberndorfer et al. [23] showed that the most common reasons that patients with advanced primary brain malignancies are admitted to hospital in the last weeks of life include difficulties with ongoing care at home due to immobility, an acute change in the patient’s clinical condition, seizures and infection. A UK study of hospice utilization in patients living with primary malignant brain tumors showed that the vast majority of patients accessing community palliative care services did so after cessation of active therapy [14]. Within this group of patients, only half benefitted from inpatient hospice services while 74 % were re-admitted to local acute care hospitals for management of symptom crises [14]. Despite the high symptom burden at or near the end of life, only 12 % of patients in our study received a palliative care consultation. In our study, there is a gap between the number of patients transitioning to hospice care and the number of patients receiving a palliative care consultation.
Seventy-nine percent of patients had a designated health care proxy, but there remains a wide degree of variation in the timing of end of life discussions such as hospice planning (1–140 days prior to death) and resuscitation wishes (1–198 days prior to death). Patients with lower KPS scores at the last clinic visit prior to hospitalization were more likely to have a DNR order prior to death than patients with higher KPS scores. The gap in palliative care consultation and the range in timing of end of life discussions reflects that a standard approach to end of life care in this population has not yet been established.
Data suggests that patients with gliomas have fewer interactions with palliative care specialists than other oncological patients [24]. A survey of American neurologists suggested that substantial gaps exist in the knowledge and attitudes of practicing neurologists with respect to palliative care in neurological patients [25]. There is a need to further educate both general palliative care physicians and neurologists on the end of life needs of patients with neurological disease.
The limitations of this study include its retrospective design. This did not allow for quality of life measurements or the study of the current content of end of life discussions. Despite the disadvantages inherent to a retrospective study, it also provides some advantages. For example, a physician’s approach to and the timing of end-of-life care discussions is likely to be altered simply because the physician is aware that this aspect of care is under scrutiny. By investigating the timing of end-of-life care discussions in a retrospective manner, a realistic assessment of the current timing of these discussions is possible, which in itself is valuable information. This study also reflects patient management and referral patterns by neuro-oncology specialists at a single, tertiary care institution. The chart review included all documents regarding patient care at Memorial Sloan-Kettering Cancer Center and all of its satellite facilities. Information regarding patients who were unable to obtain care at or chose not to continue care at this institution would not be included in this data. Thus, it is possible that the data may not reflect the full range of symptoms and that it may represent a skewed population of patients and that end of life care discussions occurring outside of the institution could be missed. However, given the similarity of our results to that of other reports in the literature [1–4, 10, 14], the care studied is likely to reflect the care offered at other institutions. Patients’ symptoms were tracked based on both inpatient and outpatient records. Because only the symptoms noted as an inpatient or volunteered by the patient at outpatient visits or by telephone correspondence are recorded, this introduces a potential source of bias. However, this approach does ensure that all reported symptoms are accounted for and, in addition to the existing literature, provides a comprehensive framework for future studies in this population. Further prospective studies delving into the subjective patient-reported symptom burden, into symptom management and into the content and timing of end of life discussions as well as the reactions of patients and their families to these discussions will be invaluable. We consider the data obtained in this study, while preliminary, important and valuable in the design of a comprehensive prospective study.
Overall, it is clear that patients living with primary CNS tumors and with cerebral metastases have a high degree of symptoms burden but infrequent encounters with specialist palliative care. We have demonstrated that, end of life decision making takes places at variable stages of the disease trajectory and almost one-third of patients in the study group transition to hospice care within a 6 month period. In order to enhance this process, there is a role for specialist palliative care participation in the care of more aggressive and rapidly progressive brain tumors. Further research on symptom management and the timing and content of end of life discussions in patients living with brain tumors may help decrease distress and improve quality of life throughout the disease trajectory for both patients and caregivers.
References
Taillibert S, Laigle-Donadey F, Sanson M (2004) Palliative care in patients with primary brain tumors. Curr Opin Oncol 16:587–592
Taillibert S, Delattre JY (2005) Palliative care in patients with brain metastases. Curr Opin Oncol 17:588–592
Batchelor TT, Byrne TN (2006) Supportive care of brain tumor patients. Hematol Oncol Clin North Am 20:1337–1361
Catt S, Chalmers A, Fallowfield L (2008) Psychosocial and supportive-care needs in high-grade glioma. Lancet Oncol 9:884–891
Jenkinson MD, Haylock B, Shenoy A, Husband D, Javadpour M (2011) Management of cerebral metastasis: evidence-based approach for surgery, stereotactic radiosurgery and radiotherapy. Eur J Cancer 47:649–655
Pignatti F, van den Bent M, Curran D et al (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 20:2076–2084
Puduvalli VK, Hashmi M, McAllister LD et al (2003) Anaplastic oligodendrogliomas: prognostic factors for tumor recurrence and survival. Oncology 65:259–266
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. New Engl J Med 352:987–996
Pace A, Di Lorenzo C, Guariglia L, Jandolo B, Carapella CM, Pompili A (2009) End of life issues in brain tumor patients. J Neurooncol 91:39–43
Sizoo EM, Braam L, Postma TJ et al (2010) Symptoms and problems in the end-of-life phase of high-grade glioma patients. Neuro Oncol 12:1162–1166
Lipsman N, Skanda A, Kimmelman J, Bernstein M (2007) The attitudes of brain cancer patients and their caregivers towards death and dying: a qualitative study. BMC Palliat Care 6:7
Junck L (2004) Supportive management in neuro-oncology: opportunities for patient care, teaching, and research. Curr Opin Neurol 17:649–653
Pace A, Metro G, Fabi A (2010) Supportive care in neurooncology. Curr Opin Oncol 22:621–626
Faithfull S, Cook K, Lucas C (2005) Palliative care of patients with a primary malignant brain tumour: case review of service use and support provided. Palliat Med 19:545–550
Watanabe K, MacLeod R (2005) Care for dying patients with primary malignant brain tumor. Neurol Med Chir 45:657–659
Talacchi A, Santini B, Savazzi S, Gerosa M (2010) Cognitive effects of tumour and surgical treatment in glioma patients. J Neurooncol 103(3):541–549
Correa DD (2010) Neurocognitive function in brain tumors. Curr Neurol Neurosci Rep 10:232–239
Triebel KL, Martin RC, Nabors LB, Marson DC (2009) Medical decision-making capacity in patients with malignant glioma. Neurology 73:2086–2092
Bosshard G, Nilstun T, Bilsen J et al (2005) Forgoing treatment at the end of life in 6 European countries. Arch Intern Med 165:401–407
The SUPPORT Principal Investigators (1995) A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). JAMA 274:1591–1598
Dorman S, Hayes J, Pease N (2009) What do patients with brain metastases from non-small cell lung cancer want from their treatment? Palliat Med 23:594–600
Becker G, Hatami I, Xander C et al (2011) Palliative cancer care: an epidemiologic study. J Clin Oncol 29:646–650
Oberndorfer S, Lindeck-Pozza E, Lahrmann H, Struhal W, Hitzenberger P, Grisold W (2008) The end-of-life hospital setting in patients with glioblastoma. J Palliat Med 11:26–30
Addington-Hall J, Altmann D (2000) Which terminally ill cancer patients in the United Kingdom receive care from community specialist palliative care nurses? J Adv Nurs 32:799–806
Carver AC, Vickrey BG, Bernat JL, Keran C, Ringel SP, Foley KM (1999) End-of-life care: a survey of US neurologists’ attitudes, behavior, and knowledge. Neurology 53:284–293
Acknowledgments
Thank you to John Francavilla and Kristin Herman for their assistance with the database information. This research was not funded by any granting agency or other funding source.
Conflict of interest
Dr. Gofton and Dr. Graber both receive fellowship funding from Memorial Sloan-Kettering Cancer Center. Dr. Carver has nothing to disclose. No funding was received for this project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gofton, T.E., Graber, J. & Carver, A. Identifying the palliative care needs of patients living with cerebral tumors and metastases: a retrospective analysis. J Neurooncol 108, 527–534 (2012). https://doi.org/10.1007/s11060-012-0855-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-012-0855-y