Abstract
High-grade gliomas are highly vascularized tumors, in which the amount of new blood vessels is closely related with the degree of malignancy. The role of endothelial progenitor cells (EPCs) in the neoangiogenesis of gliomas and the effects of post-surgical therapies (i.e., radiotherapy (RT) and chemotherapy) have not yet been fully elucidated. The aim of the present study was to evaluate the effect of surgery and post-surgical treatment on the levels of circulating EPCs in glioma patients and their correlation with vascular endothelial growth factor (VEGF). In this study, we assessed by flow cytometry the number of EPCs in the peripheral blood of 78 high-grade glioma patients (both untreated and treated with RT and chemotherapy) and 34 age- and sex-matched healthy controls. EPCs were markedly decreased in all treated glioma patients as compared to untreated ones. VEGF levels were significantly higher in patients as compared to controls, and surgery, but not chemotherapy, significantly decreased VEGF concentrations. We found no relationship between VEGF plasma levels and EPCs. In conclusion, the reliability of EPCs as a biomarker for monitoring angiogenesis in glioma patients needs further studies of correlations of this parameter with other markers of tumor-related vasculature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Numerous studies have demonstrated that neovascularization associated with tumor growth occurs through several mechanisms, among which is the recruitment of endothelial progenitor cells (EPCs). Their role in tumor-associated vasculogenesis is being investigated both in in vivo models [1, 2] and in patients affected by various tumors [3–5]. Work by Peters et al. [6] on tumors arising in patients having undergone allogenic bone marrow transplantation suggests that the contribution of EPCs to tumor-associated vasculature may vary considerably, depending on the type of tumor. Moreover, it has been suggested that the time point in tumor development/growth may significantly influence the number of circulating EPCs [7].
High-grade gliomas are highly vascularized tumors characterized by rapid growth and fatal prognosis. In their most aggressive variant (WHO grade IV glioma, glioblastoma, GBM), both cooption of pre-existing vessels and alterations in vessels (endothelial proliferation, and formation of vascular glomeruli and garlands) are reported [8]. Recently, Zhang et al. [9] demonstrated in an in vivo model that human EPCs, injected into SCID mice bearing subcutaneously implanted human glioma, were incorporated in tumor neovasculature. In patients with glioma, a correlation between the percentage of circulating EPCs and tumor angiogenic activity has also been recently reported [10].
Chemotherapeutics like taxanes and anthracycline [11] have been shown to induce mobilization of EPCs from the bone marrow, a clearly undesirable effect, since they might contribute to neoangiogenesis and tumor regrowth. However, in a recently published paper, the authors demonstrated, in an in vivo model, that the administration of antiangiogenic agents may prevent the EPCs spike induced by taxanes [12]. On the other hand, chemotherapy at different doses may have opposite effects on circulating EPCs in mice bearing tumors: cyclophosphamide induced the mobilization of EPCs when administered at high doses, while a metronomic schedule decreased EPCs levels [13].
The aim of the present study was to evaluate, in patients with glioma, the effect of surgery and post-surgical treatment on the levels of circulating EPCs. For this purpose, the number of circulating EPCs was assessed by flow cytometry in 78 patients with glioma and in 34 healthy controls (HC). Since vascular endothelial growth factor (VEGF) has been shown to be produced locally in patients with high-grade glioma, and might contribute in homing and incorporation of EPCs within the tumor vasculature [14, 15], EPCs levels were related to plasma VEGF concentrations.
Patients and methods
Patients and controls features are shown in Table 1.
Seventy-eight patients affected by grade IV gliomas (60 GBM, 2 gliosarcoma, median age: 54.7 years, 37M/25F) and grade III glioma (6 anaplastic astrocytoma, 5 anaplastic oligoastrocytoma, 5 anaplastic oligodendroglioma, median age: 43.3 years, 9M/7F) followed at our Institution underwent blood sampling either before surgery (14 grade IV, 5 grade III), or after surgery and before treatment (17 grade IV and 9 grade III), or after adjuvant radiotherapy (RT) and 2 cycles of chemotherapy (37 grade IV and 7 grade III). In the following text, we will define as “treatment” the post-surgical RT and chemotherapy. A small group (11 patients of the 78: 6 grade IV, 3 anaplastic oligoastrocytoma, and 2 anaplastic oligodendroglioma) were analyzed the day before and 4 days after surgery.
A complete blood cell count was performed in order to evaluate a putative pancytopenia in treated patients, as compared to patients sampled before RT/chemotherapy and HC.
Chemotherapy delivered to patients sampled after post-surgical treatment was temozolomide in GBM and gliosarcomas (n = 37), a combination of cisplatin (CDDP) and carmustine (BCNU) in anaplastic astrocytomas (n = 4), and procarbazine, lomustine, and vincristine (PVC) in anaplastic oligoastrogliomas and anaplastic oligodendrogliomas (n = 3). Some patients (12/37 grade IV glioma and 8/12 grade III glioma patients) were concomitantly treated with steroids (dexamethasone 8 mg/die) at the time of EPCs assessment.
Thirty-four age- and sex-matched healthy individuals also underwent blood sampling and were used as controls.
FACS analysis
Evaluation of EPCs was performed as previously reported by Keeney et al. [16]: briefly, a volume of 100 μl of whole blood was incubated with monoclonal antibodies anti-CD45-Cy5 (BD Bioscience, Franklin Lakes, NJ, USA), anti-CD34-FITC (BD Bioscience) and anti CD133-PE (Miltenyi, Bergisch Gladbach, Germany) for 30 min at 4°C. Red blood cells were then lysed and leucocytes were fixed with Uti-Lyse kit (DakoCytomation, Glostrup, Denmark). Isotopic antibodies served as controls (Simultest; BD Bioscience). Samples were analyzed with a FACS Vantage SE (BD Bioscience).
We considered as EPCs, CD45dim CD34+CD133+ mononuclear cells.
Since EPCs are rare in normal peripheral blood, at least 500 CD34+ cells per sample were acquired. A complete white blood cell (WBC) count was performed by the cell counter Advia 120 (Bayer, Leverkusen, Germany) and the absolute number of EPCs per μl of blood was calculated as follows:
EPCs (cell/μl) = number of EPC/(number of WBC acquired/number of WBC per μl).
VEGF quantitation
VEGF plasma levels were assessed by commercially available ELISA kits following the manufacturer’s instructions (R&D Systems, Minneapolis, MN, USA).
Statistical analysis
Differences in the levels of investigated parameters between the patients and the control group, and between patients before and after surgery, were analyzed by t test.
Spearman’s rank correlation coefficient was used for detection of relationships between two different parameters (i.e., VEGF and EPCs).
Results
Data regarding complete blood cell count are reported in Table 2. WBC were significantly higher in both treated and untreated grade IV glioma patients as compared to HC (p < 0.0130 and p < 0.0007, respectively), while WBC were higher only in untreated grade III glioma patients as compared to HC (p < 0.0051). The absolute number of lymphocytes was significantly lower in treated grade IV glioma patients as compared to HC (p < 0.0002). Platelets were lower in treated grade III glioma patients as compared to untreated grade III glioma patients (p < 0.0200), while they were higher in untreated as compared to HC (p < 0.0309).
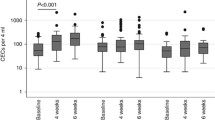
The number of EPCs and CD34+ cells in grade IV glioma patients, grade III glioma patients, and controls is reported in Table 1 and Fig. 1. A significant reduction of circulating EPCs was detected in both grade IV and grade III treated patients as compared to HC (p < 0.0002 and p < 0.0140, respectively), while CD34+ levels were similar.
Levels of EPCs and CD34+ in grade IV (a, b) and in grade III (c, d) glioma patients expressed as cells/μl of blood. Patients were subgrouped in chemotherapy/RT-treated and untreated and compared to HC. a EPCs were decreased in treated patients compared to both untreated and controls. b A statistically significant increase in CD34+ was also detected in untreated patients compared to treated or HC. Mean data (±SD) refers to 37 treated, 25 untreated patients and 34 HC. c EPCs (expressed as cell/μl) were decreased in chemotherapy/RT-treated patients as compared to HC. d CD34+ were increased in untreated patients. Mean data (±SD) refers to 7 treated and 9 untreated patients
The mean values of circulating EPCs were slightly higher in untreated grade IV patients as compared to HC, but the difference was not statistically significant. On the other hand, circulating CD34+ were significantly higher in untreated grade IV patients as compared to controls (p < 0.0411), while in grade III patients only a slight increase was detected (Table 1).
The numbers of both EPCs and CD34+ cells were similar in the two groups of untreated patients (Fig. 1). No major differences were observed in steroid-treated patients as compared to untreated ones, nor according to the different chemotherapy schedules (unshown).
EPCs, CD34+ cells, and VEGF levels of the 11 patients monitored before and after surgery are reported in Table 3. Since we did not find differences between grade IV and grade III glioma patients, we analyzed these patients as a single group. No statistically significant changes in EPCs and CD34+ numbers were detected, while there was a significant decrease of VEGF levels (166.5 ± 165.5 vs. 84.6 ± 87.9, p < 0.0348) after surgery. Post-surgical levels of VEGF in glioma patients were not different from those of HC.
Comparing all IV glioma patients sampled before surgery. and after surgery but before chemotherapy. we did not find significant differences either in EPCs or in CD34+ cells (not shown). In patients sampled after surgery but before chemotherapy, we detected only a trend to an increase in circulating EPCs, while CD34+ cells were significantly higher compared to control (9.18 vs. 5.6, p < 0.033).
Within the group of HC, no relationship between age and number of EPCs was found, nor were differences detected between male and female individuals (unshown).
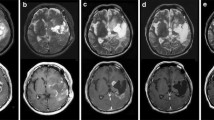
VEGF plasma levels were significantly higher in patients as compared to HC (grade IV vs. controls: p < 0.00033; grade III vs. controls: p < 0.00027; Fig. 2). No statistically significant differences were detected between grade IV and grade III patients, nor between treated and untreated patients.
Discussion
The contribution of EPCs to neoangiogenesis and tumor progression and their potential as biomarker of angiogenesis is under intensive investigation (reviewed in [17]). Despite several previous studies focused on circulating EPCs in glioma models or in untreated glioma patients, little is known about the in vivo effects of different chemotherapy schedules on EPCs levels in glioma patients.
In our study on 78 glioma patients, we did find a significant reduction in circulating EPCs in all treated patients as compared to HC. Moreover, our data showed that EPCs were decreased in treated patients as compared to untreated ones, although this difference was statistically significant only in grade IV glioma patients, possibly due to the relatively high inter-individual variations.
The reduction in EPCs in treated patients paralleled a decrease in CD34+ cells (i.e., bone marrow-derived progenitor cells) and took place in all subgroups of patients, both those treated with a “metronomic” schedule (i.e., grade IV gliomas and anaplastic oligodendrogliomas/oligoastrocytomas) and those treated with “pulsed” chemotherapy with CDDP + BCNU (i.e., anaplastic astrocytomas). This observation is in agreement with the findings of Shaked et al. [12], who demonstrated that CDDP, at variance with Paclitaxel, induced a significant decrease in circulating EPCs. Hence, CDDP per se (or in association with BCNU) might have an antiangiogenic effect by reducing circulating EPCs and CD34+ cells. However, since the group of patients treated with CDDP + BCNU was small (n = 4), this observation deserves further investigation.
The marked decrease in EPCs and CD34+ cells does not seem to be related to severe pancytopenia caused by therapies. Although a significant decrease in the absolute number of lymphocytes was detected in treated grade IV glioma patients as compared to HC (1,340 vs. 2,047), no differences were found between treated and untreated patients.
In our cohort of untreated grade IV glioma patients, circulating EPCs levels were only slightly higher as compared to controls (3.8 vs. 3.6 EPCs/μl). Our findings are in contrast with those previously reported by other authors, who observed higher circulating EPCs levels in, respectively, 39 and 10 glioma patients as compared to patients affected by other tumors [18] or to HC [10]. A possible explanation for the discrepancy is that in our study the group of untreated patients is relatively small, and high inter-individual variations of EPCs in our cohort of patients (i.e., SD) were observed. However, methodological differences in EPCs calculation should also be considered; to avoid influence of leukocyte subset fluctuations, circulating EPCs were calculated as absolute number per μl of blood [16] and not as the percentage of peripheral blood mononuclear cells as previously reported. It should also be stressed that, despite intensive investigation, different opinions persist as to the best way of identifying EPCs. Different cell surface markers have been used to identify circulating EPCs [19–21], and a consensus has not yet been reached [17]. In addition, it has been demonstrated that endothelial-like cells may originate from bone marrow-derived CD34+ cells or from monocyte-like CD14+ cells [22, 23], and that bone marrow-derived CD34+ hematopoietic progenitor cells may contribute to tumor vasculature development with different roles [24].
As a matter of fact, in untreated glioma patients (both grades III and IV), we observed a significant increase of CD34+ cells as compared to HC. As previously suggested in other tumors, circulating CD34+ cells (and not only EPCs) might also contribute to tumor-induced neoangiogenesis in glioma [24]. Our study was not primarily focused on circulating endothelial cells (CECs); however, the finding of increased levels of blood CD34+ cells deserves further investigation, in as much as it could be at least partly due to CECs released by redundant neoangiogenesis. Monitoring of CECs has also been proposed to evaluate anti-angiogenic efficacy [25, 26]. The reduction in CD34+ cells after the treatments delivered in these patients might also indicate a partial antiangiogenic effect after chronic non-metronomic chemotherapy.
In agreement with previously reported data, plasma VEGF levels were markedly higher in glioma patients than in controls [10, 14]. Surgical tumor resection significantly reduced VEGF plasma levels in the 11 patients analyzed the day before and 4 days after surgery (166.5 vs. 84.6 pg/mL, p < 0.0348) suggesting an even more pronounced decrease in cerebral microenvironment. No changes were observed in circulating EPCs or CD34+ cells after surgery, although we cannot exclude putative delayed effects. Our data suggest that chemotherapy has little effect on the production of VEGF. Indeed, treated patients displayed only a slight decrease in VEGF levels as compared to untreated ones, and no relationship was detected between VEGF plasmatic levels and circulating EPCs either in patients or in controls. Similarly, survival time was not different in treated grade IV glioma patients with higher VEGF or EPCs values compared to patients with lower levels (not shown). In agreement with our observations, a lack of correlation between VEGF and circulating EPCs has been described in patients with breast and gastric carcinoma [5]. Previously reported data showed that paclitaxel-induced mobilization of EPCs paralleled an increase in plasma stromal cell-derived factor-1 (SDF-1) levels, and that the pre-treatment with an anti SDF-1 monoclonal antibody abrogated the circulating EPCs peak [12].
The putative value of circulating EPCs as surrogate markers for tumor-related vasculature changes is still controversial [5, 10]. In fact, in addition to difficulties in evaluating this parameter in routine analysis, and to persisting uncertainties about the best way of identifying circulating EPCs, it is known that a number of physiological, pharmacological, and disease-related factors may affect the number of EPCs; among these are vascular damage [21], physical activity [27], estrogen [28], G-CSF [20], erythropoietin [29], smoking [30], and also surgical trauma [21]. Although the helpfulness of a biomarker for monitoring angiogenesis would be welcome, all these factors seem to limit the reliability of the use of circulating EPCs in glioma patients. Evaluation of other markers of tumor-related vasculature (such as perfusion MRI or histological microvessel density), and longitudinal studies focusing on fluctuations of EPCs, are needed to better investigate the putative usefulness of EPCs as a biomarker in the disease course and response to therapies in high-grade glioma patients.
References
Young MR (2004) Tumor skewing of CD34+ progenitor cell differentiation into endothelial cells. Int J Cancer 109:516–524. doi:10.1002/ijc.20003
Vajkoczy P, Blum S, Lamparter M, Mailhammer R, Erber R, Engelhardt B et al (2003) Multistep nature of microvascular recruitment of ex vivo-expanded embryonic endothelial progenitor cells during tumor angiogenesis. J Exp Med 197:1755–1765. doi:10.1084/jem.20021659
Hilbe W, Dirnhofer S, Oberwasserlechner F, Schmid T, Gunsilius E, Hilbe G et al (2004) CD133 positive endothelial progenitor cells contribute to the tumour vasculature in non-small cell lung cancer. J Clin Pathol 57:965–969. doi:10.1136/jcp.2004.016444
Mancuso P, Burlini A, Pruneri G, Goldhirsch A, Martinelli G, Bertolini F (2001) Resting and activated endothelial cells are increased in the peripheral blood of cancer patients. Blood 97:3658–3661. doi:10.1182/blood.V97.11.3658
Kim HK, Song KS, Kim HO, Chung JH, Lee KR, Lee YJ et al (2003) Circulating numbers of endothelial progenitor cells in patients with gastric and breast cancer. Cancer Lett 198:83–88. doi:10.1016/S0304-3835(03)00268-4
Peters BA, Diaz LA, Polyak K, Meszler L, Romans K, Guinan EC et al (2005) Contribution of bone marrow-derived endothelial cells to human tumor vasculature. Nat Med 11:261–262. doi:10.1038/nm1200
Komarova NL, Mironov V (2005) On the role of endothelial progenitor cells in the tumor neovascularisation. J Theor Biol 235:338–349. doi:10.1016/j.jtbi.2005.01.014
Birner P, Piribauer M, Fischer I, Gatterbauer B, Marosi C, Ambros PF et al (2003) Vascular patterns in glioblastoma influence clinical outcome and associate with variable expression of angiogenic proteins: evidence for distinct angiogenic subtypes. Brain Pathol 13:133–143. doi:10.1111/j.1750-3639.2003.tb00013.x
Zhang HR, Chen FL, Xu CP, Ping YF, Wang QL, Liang ZQ et al (2009) Incorporation of endothelial progenitor cells into the neovasculature of malignant glioma xenograft. J Neurooncol 93:165–174. doi:10.1007/s11060-008-9757-4
Rafat N, Beck GCh, Schulte J, Tuettenberg J, Vajkoczy P (2009) Circulating endothelial progenitor cells in malignant gliomas. J Neurosurg 112:43–49. doi:10.3171/2009.5.JNS081074
Fürstenberger G, von Moos R, Lucas R, Thürlimann B, Senn HJ, Hamacher J, Boneberg EM (2006) Circulating endothelial cells and angiogenic serum factors during neoadjuvant chemotherapy of primary breast cancer. Br J Cancer 94:524–531. doi:10.1038/sj.bjc.6602952
Shaked Y, Henke E, Roodhart JM, Mancuso P, Langenberg MH, Colleoni M et al (2008) Rapid chemotherapy-induced acute endothelial progenitor cell mobilization: implications for antiangiogenic drugs as chemosensitizing agents. Cancer Cell 14:263–273. doi:10.1016/j.ccr.2008.08.001
Bertolini F, Paul S, Mancuso P, Monestiroli S, Gobbi A, Shaked Y, Kerbel RS (2003) Maximum tolerable dose and low-dose metronomic chemotherapy have opposite effects on the mobilization and viability of circulating endothelial progenitor cells. Cancer Res 63:4342–4346
Salmaggi A, Eoli M, Frigerio S, Silvani A, Gelati M, Corsini E et al (2003) Intracavitary VEGF, bFGF, IL-8, IL-12 levels in primary and recurrent malignant glioma. J Neurooncol 62:297–303. doi:10.1023/A:1023367223575
Salmaggi A, Gelati M, Pollo B, Frigerio S, Eoli M, Silvani A et al (2004) CXCL12 in malignant glial tumors: a possible role in angiogenesis and cross-talk between endothelial and tumoral cells. J Neurooncol 67:305–317. doi:10.1023/B:NEON.0000024241.05346.24
Keeney M, Brown W, Gratama J, Papa S, Lanza F, Sutherland DR (2003) Immunophenotyping characterization of CD34pos cells. J Biol Regul Homeost Agents 17:254–260
Mancuso P, Bertolini F (2010) Circulating endothelial cells as biomarkers in clinical oncology. Microvasc Res 79:224–228. doi:10.1016/j.mvr.2010.02.007
Zheng PP, Hop WC, Luider TM, Sillevis Smitt PA, Kros JM (2007) Increased levels of circulating endothelial progenitor cells and circulating endothelial nitric oxide synthase in patients with gliomas. Ann Neurol 62:40–48. doi:10.1002/ana.21151
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T et al (1997) Isolation of putative progenitor endothelial cells for angiogenesis. Science 275:964–967. doi:10.1126/science.275.5302.964
Peichev M, Naiyer AJ, Pereira D, Zhu Z, Lane WJ, Williams M et al (2000) Expression of VEGFR-2 and AC133 by circulating human CD34+ cells identifies a population of functional endothelial precursors. Blood 95:952–958
Gill M, Dias S, Hattori K, Rivera ML, Hicklin D, Witte L et al (2001) Vascular trauma induces rapid but transient mobilization of VEGFR(+) AC133(+) endothelial precursor cells. Circ Res 88:167–174. doi:10.1161/01.RES.88.2.167
Fuijyama S, Amano K, Uehira K, Yoshida M, Nishiwaki Y, Nozawa Y et al (2003) Bone marrow monocyte lineage cells adhere on injured endothelium in a monocyte chemoattractant protein-1 dependent manner and accelerate reendothelization as endothelial progenitor cells. Circ Res 93:980–989. doi:10.1161/01.RES.0000099245.08637.CE
Garmy-Susini B, Varner JA (2005) Circulating endothelial progenitor cells. Br J Cancer 93:855–858. doi:10.1038/sj.bjc.6602808
Reddy K, Zhou Z, Schadler K, Jia S, Kleinerman ES (2008) Bone marrow subsets differentiate into endothelial cells and pericytes contributing to Ewing’s tumor vessels. Mol Cancer Res 6:929–936. doi:10.1158/1541-7786.MCR-07-2189
Shaked Y, Emmenegger U, Man S, Cervi D, Bertolini F, Ben-David Y et al (2005) Optimal biologic dose of metronomic chemotherapy regimens is associated with maximum antiangiogenic activity. Blood 106:3058–3061. doi:10.1182/blood-2005-04-1422
Farace F, Massard C, Borghi E, Bidart JM, Soria JC (2007) Vascular disrupting therapy-induced mobilization of circulating endothelial progenitor cells. Ann Oncol 18:1421–1422. doi:10.1093/annonc/mdm367
Adams V, Lenk K, Linke A, Lenz D, Erbs S, Sandri M et al (2004) Increase of circulating endothelial progenitor cells in patients with coronary artery disease after exercise-induced ischemia. Arterioscler Thromb Vasc Biol 24:684–690. doi:10.1161/01.ATV.0000124104.23702.a0
Strehlow K, Werner N, Berweiler J, Link A, Dirnagl U, Priller J et al (2003) Estrogen increases bone marrow-derived endothelial progenitor cell production and diminishes neointima formation. Circulation 107:3059–3065. doi:10.1161/01.CIR.0000077911.81151.30
Bahlmann FH, Song R, Boehm SM, Mengel M, von Wasielewski R, Lindschau C et al (2004) Low-dose therapy with the long-acting erythropoietin analogue darbepoetin alpha persistently activates endothelial Akt and attenuates progressive organ failure. Circulation 110:1006–1012. doi:10.1161/01.CIR.0000139335.04152.F3
Vasa M, Fichtlscherer S, Aicher A, Adler K, Urbich C, Martin H et al (2001) Number and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery disease. Circ Res 89:E1–E7. doi:10.1161/hh1301.093953
Conflict of Interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Corsini, E., Ciusani, E., Gaviani, P. et al. Decrease in circulating endothelial progenitor cells in treated glioma patients. J Neurooncol 108, 123–129 (2012). https://doi.org/10.1007/s11060-012-0805-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-012-0805-8