Abstract
Brain and spinal tumors are the second most common malignancies in childhood after leukemia, and they remain the leading cause of death from childhood cancer. Autophagy is a catabolic cellular process that is thought to regulate chemosensitivity, however its role in pediatric tumors is unknown. Here we present studies in pediatric medulloblastoma cell lines (DAOY, ONS76) and atypical teratoid/rhabdoid tumor cell lines (BT-16, BT-12) to test this role. Autophagy was inhibited using siRNA against autophagy-related genes ATG12 and ATG7 or pharmacologically induced or inhibited using rapamycin and chloroquine to test the effect of autophagy on chemosensitivity. Autophagic flux was measured using Western blot analysis of LC3-II and p62 and cell viability was determined using MTS assays and clonogenic growth. We found that when pediatric brain tumor cells under starvation stress, exposed to known autophagy inducers such as rapamycin, or treated with current chemotherapeutics (lomustine, cisplatin), all stimulate autophagy. Silencing ATG12 and ATG7 or exposure to a known autophagy inhibitor, chloroquine, could inhibit this autophagy increase; however, the effect of autophagy on tumor cell killing was small. These results may have clinical relevance in the future planning of therapeutic regimens for pediatric brain tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
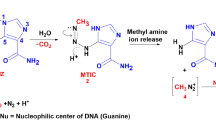
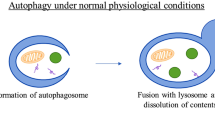
Brain and spinal tumors, the second most common malignancies in childhood after leukemia, account for 22% of all childhood cancers in children up to 14 and 10% of tumors in children 15–19. Despite advances in therapy, they remain a leading cause of death from childhood cancer. Understanding mechanisms of tumor cell death and survival are vital to developing new therapies and improving the effectiveness of currently utilized therapies. One of these mechanisms is autophagy, a catabolic process that turns over long-lived proteins and organelles and contributes to cell and organism survival during nutrient deprivation and other stresses. One form of autophagy, macroautophagy (hereafter referred to as autophagy), is a ubiquitous process in eukaryotic cells. In autophagy, double membrane vesicles called autophagosomes engulf proteins, organelles and other cytoplasmic components, fuse with lysosomes to form an autophagolysosome and allow engulfed material to be degraded [1]. Autophagy is thought to be a tumor suppression mechanism because a genetic deficiency in autophagy regulators (e.g. beclin 1 [2, 3], Atg4 [4], Bif1 [5], UVRAG [6]) leads to increased cancer. Additionally, many oncogenes inhibit autophagy and tumor suppressors increase autophagy [7]. However, autophagy may also promote tumor progression and metastasis by, for example, helping tumor cells survive in a stressful microenvironment [8, 9] and it has been suggested that autophagy may simultaneously both suppress tumor development and be required for tumor progression [10].
There is great interest in manipulating autophagy to improve cancer treatment but considerable disagreement about how to use the effects of autophagy appropriately [7, 11–13]. Many publications report autophagy as a tumor cell killing mechanism by diverse anti-cancer agents [14–16]. However, autophagy induced during treatment often inhibits tumor cell killing as shown in our lab [17] and by others [18–21]. Thus there is evidence that autophagy can prevent or promote cancer and kill or protect cancer cells. These contradictions create an important therapeutic question—should we try to inhibit autophagy or stimulate autophagy in people with cancer?
The urgency of answering these questions is underscored by the fact that clinical trials manipulating autophagy are already active. For example, a current trial (ClinicalTrials.gov NCT00728845) uses hydroxychloroquine to inhibit autophagy in combination with carboplatin, paclitaxel, and bevacizumumab in lung cancer. Other trials combining chemotherapy with hydroxychloroquine are recruiting patients with glioblastoma, breast cancer, multiple myeloma, prostate cancer, and other advanced tumors. Conversely, several trials are treating patient with mTOR inhibitors and other drugs known to induce autophagy. For example, a Phase I pharmacokinetic and pharmacodynamic study of ridaforolimus in pediatric and adolescent patients with refractory malignancies including tumors of the central nervous system (ClinicalTrials.gov NCT00704054) and a Phase II trial of everolimus in pediatric patients with refractory low-grade gliomas (ClinicalTrials.gov NCT00789828).
While autophagy’s importance in adult tumors has been extensively studied and there is a developing consensus that autophagy often leads to chemoresistance [2, 13], the same cannot be said with pediatric cancers, which are different in both their genetics and their response to standard therapies. The objective of this study was to define the role of autophagy in the treatment of pediatric brain tumors. We hypothesized that autophagy could be induced in pediatric brain tumor cell lines by starvation and treatment with current chemotherapeutics and FDA approved drugs. We further hypothesized that by altering the levels of autophagy within the cells, we could affect chemosensitivity. We found that when pediatric medulloblastoma and atypical teratoid/rhabdoid tumor (AT/RT) cell lines cells are under starvation stress or exposed to known autophagy inducers, they show increased levels of autophagy. We also showed that standard chemotherapeutics used to treat these tumors stimulates autophagy; this stimulation was inhibited by silencing autophagy genes or treating with chloroquine. However, MTS assays and clonogenic studies, looking at both short and long-term endpoints, found only small differences in cell survival in select conditions when autophagy was manipulated. Thus, the effect of the manipulation of autophagy on tumor cell kill may be small at best and does not appear to have a substantial effect on long-term tumor cell survival. These data may have significant clinical relevance in the future planning of therapeutic regimens for pediatric brain tumors.
Materials and methods
Cells and reagents
Cells obtained from ATCC include: Daoy, number HTB-186; U87 MG, number HTB-14. ONS76 cells were kindly provided by Dr. James T. Rutka (University of Toronto, Canada). Peter Houghton, St. Jude Children’s Hospital, provided the AT/RT cells (BT-16, BT-12). Lomustine (CCNU) and cisplatin were obtained from Sigma (St. Louis, MO). siRNAs and transfection reagents were obtained from Dharmacon (Lafayette, CO), and rapamycin and chloroquine from Sigma (St. Louis, MO)
siRNA transfection
Medulloblastoma and AT/RT cells were transfected with either a control scrambled siRNA or an siRNA targeting ATG12 and ATG7 (Dharmacon, Lafayette, CO) using DharmaFECT 2 transfection reagents according to the manufacturer’s recommendation (Dharmacon, Lafayette, CO). Cells were grown for 72 h and then replated for experiments and cell lysate samples were collected for immunoblot verification of protein knockdown.
Immunoblotting
Autophagy flux assays were preformed evaluating microtubule-associated light-chain 3 (LC-3) II formation and p62 in the presence or absence of lysosomal protease inhibitors as recommended by Mizushima and Yoshimori [22]. Cell lysates were collected in RIPA buffer and quantified by Bio-Rad protein assay. For siRNA transfections, cell lysates were similarly collected 72 h after transfection to demonstrate protein levels. For each lysate sample, 5 μg of protein were resolved on SDS-PAGE 15% denaturing gels and transferred to polyvinylidene difluoride (PVDF) membranes. The membranes were blocked with 5% nonfat dry milk in TBST buffer for 1 h and were incubated overnight with antibodies that recognize LC3 (Novus Biologicals, Littleton, CO), p62 (Abnova, Walnut, CA) or β-Actin (Sigma, St. Louis, MO) and then washed in TBST and incubated with the appropriate peroxidase-conjugated secondary antibody. Bands were visualized with Immobilon Western Chemiluminescent HRP substrate (Millipore, Billerica, MA) on X-ray film and densitometry measurements were preformed. All experiments were performed a three times.
Viability assays
For short-term viability assays, cells were plated in 96-well plates with 2 × 103 cells/well and incubated overnight in media. Cells were then treated with CCNU, cisplatin, or a combination of CCNU and cisplatin in decreasing doses for 24 h. Cell viability was evaluated by MTS assay according to the manufacturer’s recommendation (Promega, Madison, WI). All experiments were performed three times in triplicate and the proportion of living cells was normalized to control wells of untreated cells.
For long-term viability assays, cells were plated in 12-well plates with 1 × 104 cells/well and incubated overnight in media. Cells were then treated with CCNU or cisplatin in decreasing doses for 24 h. Drug was then removed, the cells were gently washed and fresh media was provided every 4 days until control untreated wells had grown to approximately 70% confluence. Cells were fixed and stained using 0.4% crystal violet. Because the medulloblastoma and AT/RT cell lines do not form tight colonies, stained cells were solubilized in 33% acetic acid and absorbance were read at 540 nm. All experiments were performed three times in triplicate and the proportion of cells was normalized to control wells of untreated cells.
Results
To test if medulloblastoma (Daoy) and AT/RT cell lines (BT-16) have functional autophagy programs, cells were treated with known autophagy inducers (Fig. 1). When autophagy is induced, LC3-I is converted to LC3-II and the accumulation of LC3-II in the presence of PepA/E64D (lysosomal protease inhibitors) or chloroquine (blocks fusion of lysosomes with autophagosomes) indicates increased autophagic flux. p62, a scaffolding protein that is degraded by autophagy also accumulates in the presence of PepA/E64D or chloroquine. When the cells were stressed with serum starvation using Earl’s balanced salt solution (EBSS), autophagic flux was demonstrated by LC3-II and p62 accumulation in the presence of PepA/E64D or chloroquine (Fig.1a). The average accumulation of LC3-II and p62 in the presence of chloroquine over three experiments is shown in Fig. 1b. Accumulation of LC3-II and p62 was also seen when the cells were treated with rapamycin, which induces autophagy through inhibition of the mTOR pathway (Fig. 1). ONS76 and BT-12 cells undergoing starvation stress with EBSS also demonstrated accumulation of LC3-II, indicating autophagic flux (Fig. 2a). These findings demonstrate that all four pediatric tumor cell lines have functional autophagy systems.
Starvation stress and rapamycin induce autophagy and chloroquine inhibits autophagy in pediatric brain tumor cell lines. AT/RT (BT-16) and medulloblastoma (DAOY) cells were treated with EBSS or rapamycin for 8 h in the presence or absence of either lysosomal protease inhibitors (PepA/E64D) or chloroquine added for the last 4 h of treatment. Protein lysate was collected and analyzed for LC-3 II and p62 using Western immunoblot analysis to detect autophagy flux. Representative immunoblots are shown (a). Experiments were repeated three times, and the mean levels of LC3 and p62 normalized to actin are shown with SEM (b). *Statistical significance from the control group (P < 0.05)
Current chemotherapeutics induce autophagy in pediatric brain tumor cell lines. AT/RT (BT-12, BT-16) and medulloblastoma (DAOY, ONS76) cells were treated with starvation stress, CCNU or cisplatin for 8 h at the estimated LD50 based on previous MTS assays (data not shown) in the presence or absence of lysosomal protease inhibitors (PepA/E64D) added for the last 4 h of treatment. Protein lysate was collected and analyzed for LC3-II using Western immunoblot analysis. Representative immunoblots are shown (a). The data are represented as the mean ± SEM (b)
Medulloblastoma and AT/RT are treated clinically with combination chemotherapy agents. Two currently used chemotherapeutics, CCNU and cisplatin, were used to treat all four cell lines and cell lysates were evaluated for autophagic flux. Representative immunoblots are shown alongside cells starved with EBSS as in Fig. 2a. When these cells were treated with CCNU and cisplatin, autophagy was induced in all the cell lines albeit to varying degrees. The average accumulation of LC3-II over three experiments is shown in Fig. 2b. Of note, the ONS76 cells did not have as large an increase of LC3-II before the addition of protease inhibitors. When the cells were treated with cisplatin there was an increase in LC3-II in the BT-16, BT-12, and Daoy cells. ONS76 cells demonstrated an initial drop in LC3-II levels, but had accumulation of LC3-II with PepA/E64D thus indicating that the chemotherapy drugs also induced autophagy.
Autophagy is a multi-step process that requires multiple proteins to complete the formation of autophagosomes and LC-3 II; siRNA knockdown of required autophagy-related proteins (ATG) blocks this process. ATG12 conjugation to ATG5 is required for autophagosome formation and ATG7 is an E1 enzyme essential for this conjugation. Using siRNA targeted to ATG12 and ATG7, we were able to achieve a significant decrease of ATG12 protein 72 h after transfection as shown by western blotting (Fig. 3a). When these cells were treated with either CCNU or cisplatin, there was a dramatic decrease in the accumulation of LC3-II in all cell lines compared to cells transfected with a control scrambled siRNA (Fig. 3b) indicating that autophagy was inhibited by the siRNA treatment.
siRNA ATG7 and ATG12 knockdown is effective at inhibiting autophagy after treatment with current chemotherapeutics. AT/RT (BT-16, BT-12) and medulloblastoma (Daoy, ONS76) cells were treated with non-targeted or ATG7 and ATG12 specific siRNA for 72 h and protein lysates were evaluated for the presence of ATG7 and ATG12 by Western immunoblot analysis. Representative immunoblots showing knockdown of baseline ATG12 and ATG7 protein levels are shown (a). Cells were treated with CCNU or cisplatin 72 h after transfection as described in Fig. 2. Representative immunoblots of LC3-II levels are shown for each cell line
To determine if the genetic inhibition of autophagy altered tumor cell killing, autophagy was inhibited using siRNA to ATG12 and ATG7 and cells were treated with increasing doses of CCNU, cisplatin, or a combination of both drugs. Cells were treated 72 h after transfection and knockdown of ATG12 of at least 70%, which is sufficient to inhibit autophagy in these cells was confirmed by immunoblot analysis. Cell survival was compared between cells treated with siRNA and cells treated with a control scrambled siRNA (Fig. 4). There was no significant difference seen in tumor cell survival in a short-term MTS assay between any of the treatment groups.
Genetic manipulation of autophagy has minimal effect on tumor cell survival. AT/RT (BT-16, BT-12) and medulloblastoma (Daoy, ONS76) cells with autophagy inhibited as in Fig. 3 were treated with increasing doses of CCNU, cisplatin, or a combination of CCNU and cisplatin for 24 h. Cell viability was evaluated by MTS assay. The data are represented as the mean ± SEM
Clinically, patients can be treated with chloroquine to inhibit autophagy or rapamycin to stimulate autophagy. Published reports have shown that inhibition of autophagy in adult brain tumor cell lines can improve responses to chemotherapy and radiation [23, 24]. We therefore used an adult glioma cell line (U87) to confirm that chloroquine inhibition and rapamycin induction of autophagy can influence cell survival in a setting where survival is influenced by autophagy. U87 cells were exposed to both chloroquine and rapamycin and levels of LC3-II were evaluated by immunoblotting (Fig. 5a). U87 cells were treated with either chloroquine or rapamycin and starved for 24 h. Cells were then grown in regular media in a clonogenic assay and the percent survival was evaluated (Fig. 5b). There was a significant decrease in cell survival in chloroquine treated cells with a concomitant increase in survival in the rapamycin treated cells. These findings confirm that pharmacological manipulation of autophagy is sufficient to positively or negatively affect tumor cell survival after exposure to a stress (starvation) that is known to be autophagy-dependent.
Chloroquine and rapamycin influence survival in conditions where autophagy is important. Adult glioma cells (U87) were treated with chloroquine or rapamycin for 4 h and levels of LC3-II were evaluated as in Fig. 1. A representative immunoblot is shown (a). U87 cells were then placed under starvation stress in EBSS for 24 h with either chloroquine inhibition or rapamycin induction of autophagy. Fresh media was provided and cells were allowed to grow for 10–14 days and then evaluated for long-term viability by clonogenic growth. Experiments were repeated three times in triplicate and the data are represented as the mean ± SEM. *Statistical significance from the control group (P < 0.001)
We then used these same pharmacologic autophagy manipulations in pediatric brain tumor cells where we previously showed that autophagy is induced by chemotherapy (Fig. 2) to test if pharmacological manipulation of autophagy affects chemosensitivity in this context. Cells were treated with increasing doses of CCNU or cisplatin in the presence of rapamycin or chloroquine and cell viability was assessed by MTS assay. There was a shift in the survival curve in a short-term assay when autophagy in BT-16 cells was inhibited by pre-treatment with chloroquine, with these cells showing improved survival compared to cells with baseline or up-regulated autophagy (Fig. 6). However, no significant difference was seen in tumor cell survival between any of the other treatment groups in a short-term MTS assay.
Pharmacologic manipulation of autophagy has minimal effect on tumor cell survival in a short-term growth assay. AT/RT (BT-16, BT-12) and medulloblastoma (Daoy, ONS76) cells were pre-treated for 4 h with either chloroquine to inhibit autophagy or rapamycin to induce autophagy. They were then treated with increasing doses of CCNU (a) or cisplatin (b) in the presence of chloroquine or rapamycin for 24 h and cell viability was evaluated by MTS assay. Experiments were repeated three times in triplicate and the data are represented as the mean ± SEM
Cells were then treated with increasing doses of CCNU or cisplatin in the presence of rapamycin or chloroquine and allowed to recover to show long-term clonogenic survival (Fig. 7). The small effect seen in the BT-16 cells treated with chloroquine evaluated by MTS assay was not confirmed during clonogenic growth. Since the long-term clonogenic assay more rigorously tests the effect on chemosensitivity and resistance we conclude that the effects seen in the short-term assays did not reflect altered tumor cell killing but instead may be merely due to altered kinetics of cell death. There was no significant difference on long-term clonogenic growth in any of the other cell lines treated with cisplatin (Fig. 7b), and only very small effects on response to CCNU (Fig. 7a). These data indicate that as with the autophagy gene knockdowns, pharmacological manipulations of autophagy do not lead to altered chemosensitivity.
Pharmacologic manipulation of autophagy has minimal effect on tumor cell survival in a long-term growth assay. AT/RT (BT-16, BT-12) and medulloblastoma (Daoy, ONS76) cells were pre-treated with either chloroquine or rapamycin for 4 h, then treated with increasing doses of CCNU (a) or cisplatin (b) in the presence of chloroquine or rapamycin for 24 h. Fresh media was provided and cells were allowed to grow for 10–14 days and then evaluated for long-term cell viability. Experiments were repeated three times in triplicate and the data are represented as the mean ± SEM. *Statistical significance from the control group (P < 0.001)
Discussion
Autophagy is currently being targeted clinically to improve the treatment of a number of different cancers [25]. However, while manipulation of autophagy has been reported to be important in the treatment of adult brain tumors and other cancers [13], its importance in the treatment of pediatric tumors is unclear. This question is of particular importance in pediatric patients due to an increased risk for long-term side effects of autophagy manipulation. Autophagy is required in normal brain development; impaired autophagy in the brain causes behavioral defects, loss of brain cells, and early death [26] and mice that lack a component of a multi-protein complex that is required for formation of autophagosomes called AMBRA display aberrant brain development [27]. Therefore treatments that alter autophagy may affect normal brain development and altered autophagy resulting from brain tumor treatment could contribute to subsequent neurologic morbidity for pediatric brain tumor survivors. Thus, if autophagy inhibition were to prove useful to increase chemosensitivity, the beneficial effect on chemosensitivity would need to be substantial in order to justify the risk of causing subsequent developmental problems in the brain.
We hypothesized that autophagy could be induced in pediatric brain tumor cell lines by starvation and treatment with current chemotherapeutics and FDA approved drugs, and that by altering the levels of autophagy within the cells, we could affect chemosensitivity. In contrast to findings in the study of adult brain tumors that often show an increase in tumor cell kill when autophagy is inhibited [24, 28], our results show at most a very small effect of autophagy inhibition seen only in the BT-16 cells treated with cisplatin. Moreover, even this effect was lost in long-term clonogenic assays that provide a more rigorous test of altered chemosensitivity. There was a small but significant change in long-term survival in one of the medulloblastoma cell lines treated with chloroquine and a complimentary response in cells treated with rapamycin with one of the CCNU treatment doses, but not in any of the cisplatin treatment doses. These findings suggest that any effect on chemosensitivity of altering autophagy may depend on the cell type being studied and the stimulus used to induce autophagy and even if alterations in chemosensitivity are found, the effect is small at best. Thus, rather than autophagy being a general mechanism of chemoresistance in pediatric brain tumors, we propose that its effects may be context dependent. If this idea is correct, it will be necessary to identify the tumors and the treatments where autophagy manipulation is worthwhile rather than treating all brain cancer patients the same way.
Our study has some limitations. For example, it is possible that there is a true effect of autophagy on pediatric brain tumor response to therapy, but that blocking autophagosome formation has different effects on tumor cell survival than blocking autophagic flux. There are over 115 currently known genes targeting autophagy at various steps in the process and this study was limited to affecting only two of those genes; thus a more comprehensive analysis would be worthwhile. Additionally, both chloroquine and rapamycin have other cellular effects that may influence chemosensitivity; of course, these autophagy-independent effects may also influence the results of ongoing clinical studies as well.
Conclusions
In this study, we found that AT/RT and medulloblastoma cell lines have functional autophagy, current chemotherapeutics used to treat these tumors induce autophagy and that this autophagy can be manipulated both genetically and pharmacologically. However, the effect of manipulating autophagy on tumor cell kill in these pediatric brain tumors is small at best and does not have a significant effect on long-term tumor cell survival. We do not exclude the possibility that in specific tumors or with other treatments, autophagy manipulation may be a useful way to increase chemosensitivity, however the lack of a general effect on chemosensitivity by autophagy suggests that it will be necessary to use a higher throughout system to identify specific tumors and treatments where this applies if autophagy manipulation is to be of therapeutic benefit to patients.
References
Mizushima N (2007) Autophagy process and function. Genes Dev 21(22):2861–2873
Qu X et al (2003) Promotion of tumorigenesis by heterozygous disruption of the beclin 1 autophagy gene. J Clin Invest 112(12):1809–1820
Yue Z et al (2003) Beclin 1, an autophagy gene essential for early embryonic development, is a haploinsufficient tumor suppressor. Proc Natl Acad Sci USA 100(25):15077–15082
Marino G et al (2007) Tissue-specific autophagy alterations and increased tumorigenesis in mice deficient in Atg4C/autophagin-3. J Biol Chem 282(25):18573–18583
Takahashi Y et al (2007) Bif-1 interacts with Beclin 1 through UVRAG and regulates autophagy and tumorigenesis. Nat Cell Biol 9(10):1142–1151
Liang C et al (2006) Autophagic and tumour suppressor activity of a novel Beclin1-binding protein UVRAG. Nat Cell Biol 8(7):688–699
Maiuri MC et al (2009) Control of autophagy by oncogenes and tumor suppressor genes. Cell Death Differ 16(1):87–93
Degenhardt K et al (2006) Autophagy promotes tumor cell survival and restricts necrosis, inflammation, and tumorigenesis. Cancer Cell 10(1):51–64
Kenific CM, Thorburn A, Debnath J (2010) Autophagy and metastasis: another double-edged sword. Curr Opin Cell Biol 22(2):241–245
Takamura A et al (2011) Autophagy-deficient mice develop multiple liver tumors. Genes Dev 25(8):795–800
Hippert MM, O’Toole PS, Thorburn A (2006) Autophagy in cancer: good, bad, or both? Cancer Res 66(19):9349–9351
Kondo Y et al (2005) The role of autophagy in cancer development and response to therapy. Nat Rev Cancer 5(9):726–734
Levine B, Kroemer G (2008) Autophagy in the pathogenesis of disease. Cell 132(1):27–42
Garcia-Escudero V, Gargini R (2008) Autophagy induction as an efficient strategy to eradicate tumors. Autophagy 4(7):923–925
Lin MH, Liu SY, Liu YC (2008) Autophagy induction by a natural ingredient of areca nut. Autophagy 4(7):967–968
Turcotte S, Sutphin PD, Giaccia AJ (2008) Targeted therapy for the loss of von Hippel–Lindau in renal cell carcinoma: a novel molecule that induces autophagic cell death. Autophagy 4(7):944–946
Thorburn J et al (2009) Autophagy regulates selective HMGB1 release in tumor cells that are destined to die. Cell Death Differ 16(1):175–183
Amaravadi RK et al (2007) Autophagy inhibition enhances therapy-induced apoptosis in a Myc-induced model of lymphoma. J Clin Invest 117(2):326–336
Carew JS et al (2007) Targeting autophagy augments the anticancer activity of the histone deacetylase inhibitor SAHA to overcome Bcr-Abl-mediated drug resistance. Blood 110(1):313–322
Park MA et al (2008) Regulation of autophagy by ceramide-CD95-PERK signaling. Autophagy 4(7):929–931
Wu H et al (2006) Elongation factor-2 kinase regulates autophagy in human glioblastoma cells. Cancer Res 66(6):3015–3023
Mizushima N, Yoshimori T (2007) How to interpret LC3 immunoblotting. Autophagy 3(6):542–545
Ito H et al (2005) Radiation-induced autophagy is associated with LC3 and its inhibition sensitizes malignant glioma cells. Int J Oncol 26(5):1401–1410
Wu H et al (2009) Silencing of elongation factor-2 kinase potentiates the effect of 2-deoxy-d-glucose against human glioma cells through blunting of autophagy. Cancer Res 69(6):2453–2460
Levy JM, Thorburn A (2011) Targeting autophagy during cancer therapy to improve clinical outcomes. Pharmacol Ther 131(1):130–141
Komatsu M et al (2006) Loss of autophagy in the central nervous system causes neurodegeneration in mice. Nature 441(7095):880–884
Fimia GM et al (2007) Ambra1 regulates autophagy and development of the nervous system. Nature 447(7148):1121–1125
Shingu T et al (2009) Inhibition of autophagy at a late stage enhances imatinib-induced cytotoxicity in human malignant glioma cells. Int J Cancer 124(5):1060–1071
Acknowledgments
JM Mulcahy Levy is supported by a St. Baldrick’s Foundation Fellowship. Additional support provided by The Morgan Adams Foundation and NIH grant CA150925. We thank Dr. Rajeev Vibhakar for providing the ONS76 cell line and Dr. Peter Houghton for providing the BT-16 and BT-12 cell lines.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Levy, J.M.M., Thorburn, A. Modulation of pediatric brain tumor autophagy and chemosensitivity. J Neurooncol 106, 281–290 (2012). https://doi.org/10.1007/s11060-011-0684-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-011-0684-4