Abstract
The role of prophylactic intrathecal chemotherapy in the treatment of primary central nervous system lymphoma remains controversial. We report a retrospective single center study of a cohort of 69 patients with primary central nervous system lymphoma who had been treated with a regimen that combined high intravenous doses of Methotrexate, CCNU, procarbazine and methylprednisolone. Before 2000, patients systematically received intrathecal prophylaxis including Methotrexate, cytarabine, and hydrocortisone delivered either by intraventricular or lumbar injection along with the systemic chemotherapy (group A, n = 39). After this date, the procedure was changed and intrathecal chemotherapy was withdrawn from the protocol (group B, n = 30). The median age and Karnofsky index were comparable in both groups. At the time of analysis, we found no significant difference between patients with and without intrathecal prophylaxis in terms of objective response rate, patterns of relapse, progression-free survival or overall survival. In our study, intrathecal prophylaxis withdrawal from a high dose intravenous Methotrexate-based chemotherapy regimen did not influence disease control and outcome of primary central nervous system lymphoma. Further studies prospectively investigating the role of intrathecal chemoprophylaxis are warranted for this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is a rare non-Hodgkin’s lymphoma that involves the brain, and also the eyes, spinal cord, leptomeninges or any combination of these sites. It accounts approximately for 1–3% of primary CNS tumors. The optimal treatment for PCNSL remains to be determined [1]. The addition of intravenous high dose methotrexate (HD-MTX) chemotherapy to whole brain radiotherapy (WBRT) has clearly improved the prognosis compared to WBRT alone [2]. Encouraging results using chemotherapy alone with deferment of WBRT have been reported by some authors, both in term of efficacy and reduced neurotoxicity [3–8], and the value of radiotherapy as consolidation treatment after chemotherapy is therefore currently being investigated using randomized trials [9, 10]. Because leptomeningeal relapse may occur in up to 20% of cases in the course of the disease [11, 12], another important concern is the role of intrathecal (IT) chemoprophylaxis as part of the initial treatment. Studies addressing the impact of IT prophylaxis on PCNSL outcome are scarce and have led to contradictory results [13, 14]. In the present study, we report our retrospective single center study of patients uniformly treated by a HD-MTX-based polychemotherapy (Anocef regimen), either combined with IT prophylaxis or not.
Patients and methods
Chemotherapy regimen
Until recently, immunocompetent patients with PCNSL were treated in our institution with a chemotherapy regimen alone (without radiotherapy) as initial treatment (Anocef regimen). The regimen included intravenous HD-MTX (1 g m2 for patients aged over 60 or 3 g m2 for younger patients), CCNU, procarbazine and methylprednisolone. Before 2000, patients systematically received IT prophylaxis along with systemic chemotherapy including Methotrexate (15 mg), Cytarabine (40 mg), and Metilprednisolone (40 mg) delivered as described [7] either by intraventricular or lumbar injection for up to nine injections as soon they could tolerate it (group A). After this date, the procedure was changed, IT prophylaxis was withdrawn from the protocol, and all patients received intravenous HD-MTX (3 g m2) in addition to CCNU, Procarbazine and Methylprednisolone without IT prophylaxis (group B).
Eligibility criteria
We retrospectively reviewed the patients from our database of 1996–2007 and included the patients who fulfilled the following criteria: (1) pathologically confirmed PCNSL, (2) age >16 years, (3) Karnofsky index >40, (4) absence of positive or suspicious cytology at the CSF analysis at diagnosis, (5) initial treatment according to the Anocef chemotherapy regimen, and (6) no WBRT as part of the initial treatment.
Statistics
Progression-free survival (PFS) was calculated from the date of first treatment to progression or recurrence. Overall survival (OS) was calculated from the date of first treatment to death or last follow-up. Follow-up was conducted up to December 2009.
The proportion of patients with CR or PR defined the objective response rate (ORR)
The two groups were compared using the Student’s t test and chi-square test. Kaplan–Meier survival curves were constructed and compared between the two groups using the log rank test. A p value less than 0.05 was considered statistically significant.
Results
A total of 69 patients were eligible for the study. The main clinical characteristics of the patients are summarized in Table 1. Thirty-nine patients received IT prophylaxis (Group A) and 30 did not (Group B). The median age was 55 years (range 24–74) and 60 years (range 17–82) for groups A and B, respectively. Median Karnofsky performance status (KPS) was 70 in both groups (range 40–90). In group A, all the patients but one received an IT prophylaxis and Methotrexate, Cytarabine and Metilprednisolone with a median number of five injections (range 1–9); one patient received cytarabine only. IT chemotherapy was delivered by Ommaya reservoir and lumbar puncture in 3 and 36 patients, respectively. The ORR to upfront chemotherapy of the whole population was 64.5%. No significant statistical difference in gender, age, KPS and ORR to first line chemotherapy was observed between both groups.
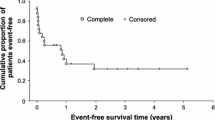
After the first treatment and with a median follow-up of 136.2 months (CI: 69.9–153.8) for group A and a median follow-up of 47 months (CI: 42–87.5) for group B, the median PFS was 28.7 months (CI: 11.1–40.1) in group A and 9.9 months (CI: 5.6–27.4) in group B (p = 0.0518). The 2-year PFS rate was 53.8% in group A and 36.6% in group B (Fig. 1). The median OS did not differ significantly between patients in groups A and B (47.9 months vs 35.4 months; p = 0.4281) (Table 2). At the time of analysis, 53 patients had relapsed (30 in group A and 23 in group B), with four meningeal relapses in group A and two in group B evaluated by CSF cytology. Delayed neurotoxicity associated with diffuse leukoencephalopathy on MRI was reported in 5 patients (7%), including 3 patients from group A and 2 patients from group B (of 67, 74, 48 years old from group A and 65 and 64 years old from group B).
Discussion
In systemic diffuse large B cell non-Hodgkin’s lymphoma, several studies have demonstrated that IT chemoprophylaxis may reduce the risk of CNS recurrence [15, 16]. However, patients of these studies did not receive systemic cytotoxic drugs known to cross the blood–brain barrier. Because intravenous HD-MTX, the key drug of the chemotherapy for PCNSL, is suspected to yield cytotoxic doses in the CSF when used at doses higher than 3 g m2, the addition of IT chemoprophylaxis is questionable. In addition, IT MTX chemotherapy delivery is not exempt from potential morbidity. It exposes the patients to an increased risk of treatment-related neurotoxicity. Moreover, it is recommended to be delivered intraventricularly through an Ommaya reservoir for an optimal diffusion within the leptomeningeal spaces and better efficacy, but Ommaya reservoir infection may occur in up to 19% of cases during chemotherapy, resulting in interruption and delay in the treatment schedule [8].
In the present study, we did not observe negative impact after IT prophylaxis withdrawal from our HD-MTX-based polychemotherapy regimen either on disease control or OS when intravenous MTX was delivered at high doses (1 or 3 g m2). However, our study had several limitations regarding its retrospective design: the fact that the patients who received an intrathecal chemoprophylaxis were almost exclusively treated by the lumbar route which could be suboptimal in comparison with the intraventricular administration efficacy [17], and the absence of systematic analysis of the CSF at relapse. Our results are in accordance with those reported in a case-controlled retrospective study from the MSKKC [13]. In this study, the authors compared patients treated with HD-MTX (intravenous dose of >3.5 g m2) without IT-MTX chemotherapy (n = 14) with a series of patients matched for age, KPS, CSF cytology and cranial radiotherapy who received IT Methotrexate (n = 28). No difference was found in survival, disease control or neurotoxicity. Interestingly, our cohort of patients differs from that of the latter study by several aspects: all patients had to be free of detectable leptomeningeal involvement on CSF analysis at diagnosis; in addition, they all received the same systemic chemotherapy regimen without WBRT as part of the initial treatment. In contrast, a recent German study reported an increased early relapse rate in a small series of 18 patients when intraventricular chemotherapy was omitted from their initial chemotherapy regimen. This latter polychemotherapy included intravenous HD-MTX at the dose of 5 g m2 combined with cytarabine, ifosfamide, vinka-alkaloids and cyclophosphamide [14]. MRI re-evaluation suggested a higher rate of leptomeningeal relapse in the patients without IT chemotherapy, but the authors acknowledged the limits of their conclusion included the fact that systematic CSF analysis was not performed in all patients at relapse.
The benefit to risk ratio of IT prophylaxis in the treatment of PCNSL warrants further clarification by a prospective study.
References
Sierra del Rio M, Rousseau A, Soussain C et al (2009) Primary CNS lymphoma in immunocompetent patients. Oncologist 14:526–539
DeAngelis LM, Yahalom J, Thaler HT et al (1992) Combined modality therapy for primary CNS lymphoma. J Clin Oncol 10:635–643
Cher L, Glass J, Harsh GR et al (1996) Therapy of primary CNS lymphoma with methotrexate-based chemotherapy and deferred radiotherapy: preliminary results. Neurology 46:1757–1759
Freilich RJ, Delattre JY, Monjour A et al (1996) Chemotherapy without radiation therapy as initial treatment for primary CNS lymphoma in older patients. Neurology 46:435–439
Ng S, Rosenthal MA, Ashley D et al (2000) High-dose methotrexate for primary CNS lymphoma in the elderly. Neuro Oncol 2:40–44
Abrey LE, Yahalom J, DeAngelis LM (2000) Treatment for primary CNS lymphoma: the next step. J Clin Oncol 18:3144–3150
Hoang-Xuan K, Taillandier L, Chinot O et al (2003) Chemotherapy alone as initial treatment for primary CNS lymphoma in patients older than 60 years: a multicenter phase II study (26952) of the European organization for research and treatment of cancer brain tumor group. J Clin Oncol 21:2726–2731
Pels H, Schmidt-Wolf IG, Glasmacher A et al (2003) Primary central nervous system lymphoma: results of a pilot and phase II study of systemic and intraventricular chemotherapy with deferred radiotherapy. J Clin Oncol 21:4489–4495
Illerhaus G, Marks R, Müller F et al (2009) High-dose methotrexate combined with procarbazine and CCNU for primary CNS lymphoma in the elderly: results of a prospective pilot and phase II study. Ann Oncol 20:319–325
Soussain C, Hoang-Xuan K (2009) Primary central nervous system lymphoma: an update. Curr Opin Oncol 21:550–558
Balmaceda C, Gaynor JJ, Sun M et al (1995) Leptomeningeal tumor in primary central nervous system lymphoma: recognition, significance, and implications. Ann Neurol 38:202–209
Chamberlain MC, Kormanik P, Glantz M (1998) Recurrent primary central nervous system lymphoma complicated by lymphomatous meningitis. Oncol Rep 5:521–525
Khan RB, Shi W, Thaler HT et al (2002) Is intrathecal methotrexate necessary in the treatment of primary CNS lymphoma? J Neurooncol 58:175–178
Pels H, Juergens A, Glasmacher A et al (2009) Early relapses in primary CNS lymphoma after response to polychemotherapy without intraventricular treatment: results of a phase II study. J Neurooncol 91:299–305
Tomita N, Kodama F, Kanamori H et al (2002) Prophylactic intrathecal methotrexate and hydrocortisone reduces central nervous system recurrence and improves survival in aggressive non-hodgkin lymphoma. Cancer 95:576–580
Arkenau HT, Chong G, Cunningham D et al (2006) The role of intrathecal chemotherapy prophylaxis in patients with diffuse large B-cell lymphoma. Ann Oncol 18:541–545
Glantz MJ, Van Horn A, Fisher R et al (2010) Route of intracerebrospinal fluid chemotherapy administration and efficacy of therapy in neoplastic meningitis. Cancer 11:1947–1952 Emotherapy
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Sierra del Rio, M., Ricard, D., Houillier, C. et al. Prophylactic intrathecal chemotherapy in primary CNS lymphoma. J Neurooncol 106, 143–146 (2012). https://doi.org/10.1007/s11060-011-0649-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-011-0649-7