Abstract
Epigenetic silencing of the MGMT gene through promoter methylation correlates with improved survival in Glioblastoma Multiforme (GBM) patients receiving concurrent chemoradiotherapy. Although the clinical benefit is primarily seen in patients with methylated MGMT promoter, some unmethylated patients also respond to Temozolomide. One possible explanation may be intratumoral heterogeneity. This study was designed to assess the methylation status of the MGMT promoter in different areas of GBM and determine if methylation status varied depending on the fixation technique (paraffin-embedding versus fresh frozen) used to store tissue. Using intraoperative navigation, biopsies were obtained from three distinct regions: the enhancing outer area, the non-enhancing inner core, and an area immediately outside the enhancing region. Only patients with GBM were included for evaluation and analysis. Samples taken from each area were divided with half stored by flash freezing and the other half stored using paraffin fixation. Methylation Specific-PCR (MS-PCR) was used for analysis of MGMT promoter methylation. Thirteen patients were included. Ten were male with a median age of 62 years. In each patient, samples were taken from the enhancing rim and the necrotic centre. However, it was not considered safe or feasible to obtain samples from the area immediately adjacent to the enhancing tumor rim in one case. All patients were homogeneous for methylation status throughout their tumor and tissue taken adjacent to it when frozen tissue was used. However, four patients had discrepancies in the MGMT promoter status between the frozen and paraffin-embedded blocks and one patient was not homogeneous within the tumor when paraffin-embedded tissue was used. MGMT promoter methylation status was homogeneous in all GBM tumors. Our observation that methylation status varied depending if the DNA was extracted from paraffin-embedded versus frozen tissue is concerning. Although the reason for this is unclear, we postulate that the timing from resection to fixation or the process of fixation itself may potentially alter methylation status in paraffin-embedded tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma multiforme (GBM) is the most common and lethal primary brain tumor. Stupp et al. demonstrated that the addition of temozolomide (TMZ) to radiotherapy (RT) significantly prolonged the survival of patients with newly diagnosed GBM [1]. This study, in addition to other in vitro studies, demonstrated synergy between TMZ and RT [1–4]. As a result, concurrent treatment with TMZ and RT has become the international standard of care for GBM patients.
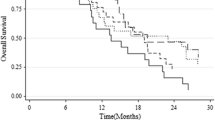
The O6-methylguanine-DNA methyltransferase (MGMT) gene encodes for a DNA-repair protein that removes alkyl groups from the O6 position of guanine. This position is an important site in the context of alkylating chemotherapy such as TMZ. If left alkylated, DNA is unable to replicate and the cell subsequently undergoes apoptosis [5–7]. It is generally accepted that high levels of MGMT activity in cancer cells create a resistant phenotype by reducing the therapeutic effect of alkylating agents such as TMZ. Several studies have shown that epigenetic silencing of the MGMT gene through promoter methylation is correlated with a median survival (MS) of nearly 2 years in patients receiving RT with TMZ for the treatment of GBM [5, 8, 9]. In contrast, patients whose tumors are unmethylated only have a MS of 12 months with the same treatment [5].
However, in these clinical trials, some patients with unmethylated tumors did demonstrate a significant survival benefit with RT and TMZ. This outlier finding is counterintuitive to the expectations derived from the overall results for patients with unmethylated tumors. The reason for this is unclear but two plausible explanations are commonly cited to explain this apparent disparity. First, there may be intratumoral heterogeneity for MGMT promoter methylation status. In the Stupp study [1] 573 patients were included and Hegi [5] was able to obtain genomic DNA from one or two paraffin sections in only 206 cases without any requirement to use tissue from a specific and common tumor location. In some cases the location of the tumor precluded extensive resection and the determination of MGMT promoter status was made using stereotactic biopsy specimens. This may not be an accurate assessment of methylation status in the tumor. Although controversial, it has therefore been postulated that intratumoral heterogeneity for MGMT promoter methylation may explain why some unmethylated patients responded to therapy (i.e. a stereotactic biopsy may have unmethylated MGMT promoter status while in actuality, the tumor is predominantly methylated but missed due to sampling error effect) [10, 11].
An alternative explanation for the unexpected significant treatment response of certain GBM patients with apparent unmethylated tumor to concurrent RT and TMZ is that it may be related to a false negative methylation result due to an adverse effect associated with the tissue fixation method used to preserve extracted tumor tissue. Paraffin embedded samples were used to determine methylation status in most of the clinical trials. While formalin fixation/paraffin embedding is most commonly used to preserve tissue, it has drawbacks in that formaldehyde can introduce deleterious changes to DNA. These include hydroxymethyl group additions (–CH2OH) especially to adenine and cytosine nucleotides, methylene bridges between adjacent bases and the generation of AP (apurinic and apyrimidinic) sites [12]. In contrast, flash freezing tissue produces relatively minimal DNA damage and is considered by many to represent the gold standard for tissue preservation [13].
This study was designed to address these two questions. First, we endeavored to determine if the methylation status of the MGMT promoter is homogeneous in different areas of GBM tumors. Second, we assessed the corroboration of promoter methylation status between paraffin-embedded and frozen tissues taken from the same location within each tumor. The need to answer these questions is extremely important. The determination of whether treatment decisions for patients with GBM can be based upon MGMT methylation status will depend upon a reliable methodology to establish this for each patient.
Methods and patients
After Institutional Ethics Review Board approval, adult patients with suspected previously untreated GBM consented to have portions of their tumor banked at the time of their initial cranial surgery at Foothills Medical Centre in Calgary, Alberta, Canada. A single neurosurgeon (MH) used preoperative and intraoperative MRI planning and performed intraoperative biopsies from the enhancing rim (x), non-enhancing inner region (y), and an area outside of the enhancing tumor rim (z) (Fig. 1). Each of the tumor samples were divided into two parts with one half being flash frozen and the other undergoing paraffin fixation. Only patients with a confirmed pathological diagnosis of GBM were included for evaluation and analysis. This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
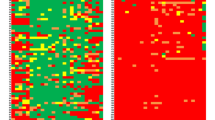
We used the methylation specific polymerase chain reaction (MS-PCR) technique outlined by Hegi et al. [5] for the purpose of identifying the MGMT promoter methylation status in GBM tumors. Briefly, MS-PCR involved isolating DNA from tumor samples followed by bisulphite conversion. Bisulphite treatment chemically converts unmethylated cytosines to uracil leaving methylated cytosines unaltered. Afterwards, sequences within the MGMT promoter which contain methylated CpG island motifs were amplified via PCR using primers specifically designed to distinguish between methylated and unmethylated DNA. MS-PCR allows for a qualitative analysis of the MGMT promoter methylation status of fresh frozen tissue and paraffin-embedded samples (Fig. 2). DNA extracted from HTB-30 cells was used as a control for the unmethylated MGMT promoter and DNA from U87MG cells served as a control for the methylated MGMT promoter (pos). Water was used as a negative control (neg).
Intratumoral sampling and corresponding results. a x: enhancing margin; y: necrotic centre; z: infiltrated white matter outside of enhancing margin (when possible). b MS-PCR result showing methylation of MGMT promoter in the three samples of one patient. DNA extracted from HTB-30 cells was used as a control for the unmethylated MGMT promoter and DNA from U87MG cells served as a control for the methylated MGMT promoter (pos). Water was used as a negative control (neg)
Descriptive statistics were used to analyze the distribution of methylation status of MGMT promoter between different samples from the same patient when frozen and paraffin-embedded samples were used.
Results
Clinical characteristics
Thirteen patients diagnosed with GBM were included in this study, twelve had primary newly diagnosed de novo GBMs and one had secondary GBM. Ten were male. Median age was 62 years (range; 49–74) and a median Karnofsky score of 80 (range; 50–90). Eight patients had a gross total resection (>95% of the tumor resected) with subtotal resection (between 50 and 95%) done in the rest. After surgery, 10 out of 13 patients were offered concurrent treatment with RT (60 Gy) and low dose temozolomide (75 mg/m2 daily) followed by monthly cycles of TMZ. Two patients were not offered concurrent therapy because of synchronous metastatic cancer (one lung adenocarcinoma and one bladder cancer); one of these patients received RT and the other medical palliative care. The remaining patient had poor performance status resulting in treatment with RT only.
Molecular data
In all patients, samples were taken from the enhancing rim (x) and the necrotic centre (y). However, it was considered safe to obtain samples from the area outside and adjacent to the enhancing rim (z) in only twelve of the thirteen patients.
Results are shown in Table 1. All patients except one had homogeneous MGMT promoter methylation status within a given tumor and tissue taken adjacent to the enhancing tumor edge demonstrated homogeneous MGMT status with the enhancing tumor. These results were consistent through three separate tests. The isolated finding of heterogeneity occurred in the paraffin-embedded tissue of patient #2, but did not occur when frozen tissue was used. Importantly, when we compared frozen versus paraffin-embedded samples taken from identical tumor regions, discrepancies in the MGMT promoter status between frozen and paraffin-embedded blocks were seen in four patients (Table 1). In order to rule out possible PCR contamination, tests were repeated and these results were also consistent through multiple tests (Supplemental Fig. 1).
Slides review
The observation of inconsistent results led us to perform additional investigations. We hypothesized that paraffin embedded blocks with discordant results may have significant necrotic tissue, low cellularity, inflammatory infiltration or be non representative of the tumor itself. Slides corresponding to the blocks of 12 of the 13 patients including the ones with discordant results were reviewed by a pathologist (TM) blinded to MGMT status results. Sample size and cellularity, percentage of tumor and inflammatory cells, blood vessels content and necrosis were reviewed.
Median size of samples was 2 cm (range; 0.5–3 cm) with most of the samples showing <30% of necrosis with a range from none to >80% necrotic tissue. Tumor cells varied from <5 to >80% and inflammatory cells ranged from 5 to 40% of the cells in the slide. Blood vessels content varied between 0 to 40%. After correlating these results with MGMT promoter status there was no correlation between any of these variables and the presence of inconsistent results. Of notice, even in patients with <5% tumor cells and >80% necrosis, MGMT promoter methylation status was consistent. Specifically, patient #2 had a 2 cm sample with 50% necrosis, 30% tumor cells, 10% inflammatory cells and 20% blood vessels in the sample with an unmethylated result that was discordant with the rest of paraffin and frozen samples (Fig. 3).
Discussion
In this study, we describe two key findings. First, MGMT promoter methylation status is homogeneous throughout the tumor if frozen tissue is used. Second, MGMT promoter methylation status can vary if the sample is paraffin fixed versus fresh frozen.
Others have recently corroborated the intratumoral MGMT promoter methylation homogeneity reported in our study. Parkinson et al. [11] evaluated 3–4 sites taken from seven GBM tumors using MGMT promoter sequencing, MS-PCR and IHC. They demonstrated that the degree of methylation and protein expression was homogeneous across each tumor. Interestingly, all samples analyzed in their study were unmethylated for the MGMT promoter which differs from our data where both methylated and unmethylated tumors were seen. Cao et al. [14] analyzed 37 samples from 12 patients with GBM. They observed no difference in the methylation status of the MGMT promoter at different locations within individual tumors. Similarly, Grasbon-Frodl reported from analysis of biopsy specimens (including stereotactic) taken from 20 high grade glioma patients (Grade III and IV) that the MGMT promoter status determined by MS-PCR (confirmed by sequencing) was homogeneous. However, the biopsy sites were not standardized as the mean of the maximum distance between the chosen biopsy sites throughout each tumor was 14 mm (range 2–32) [15].
However, intratumoral MGMT homogeneity has not been seen in all studies [10, 14, 16, 17]. Juillerat-Jeanneret et al. [10] assessed promoter methylation status using MS-PCR and methylation-sensitive dot blot assay (MS-DBA) in 14 patients. They reported differences in MGMT promoter status in samples from the same tumor taken at least 3 mm apart from each other using MS-PCR and MS-DBA in 7/14 cases. In this study, MS-PCR was used for patients 1–5 and MS-DBA for patients 6–14. These authors do not mention whether they included internal positive and negative controls in the MS-PCR and MS-DBA. Frozen and paraffin-embedded samples were from different fragments of the same tumor, at sites located at least 3 mm apart of each other. They also observed cases with discrepancy between the results of MGMT promoter status from frozen tissue and paraffin embedded tissue from the same patient. They consider this finding a result of differential expression without questioning the influence of tissue processing. Grasbon-Frodl [15] studied biopsy tissues from high grade glioma patients. All specimens were initially frozen and when a sample was taken for molecular analysis, a corresponding sample (level 1 + 1 mm) was taken for paraffin embedding. No differences in MGMT promoter methylation were detected between the different samples of each individual tumor in 24 of 25 patients. One false negative result was obtained due to the contamination of the biopsy specimen by necrotic tissue. They observed intratumoral homogeneity and suggested that misleading results may have been obtained by tissue samples involving necrotic debris and/or non-neoplastic tissue or blood. In our study, we standardized sites of tissue analysis within the tumor and we did not observe a difference in MGMT status based on location within the tumor.
The second key finding of the study was that 4 out of 14 patients demonstrated a difference in methylation status between matched frozen and paraffin-embedded samples. It is possible that this may have been due problems with MS-PCR analysis of MGMT status in formalin-fixed and paraffin-embedded tissues. Recently Preusser et al. [18] tested the reproducibility of MGMT promoter status determination by MS-PCR from formalin-fixed and paraffin-embedded samples and found that only 38.5% of the runs were successful and even when repeated 4 times, consistent results were seen in only 1 of 6 cases.
Clearly, there is controversy regarding the reliability of a single biopsy analysis to assess MGMT promoter methylation status [19]. For some, a strict interpretation of the Stupp data would suggest that unmethylated patients should only be treated with radiation and not concurrent therapy. Furthermore, new clinical trials are beginning to stratify patients on the basis of methylation status [20, 21]. The results of this study suggest that methylation status is typically homogeneous within these tumors and supports the use of single biopsy, even in an area immediately outside of the enhancing rim, to determine methylation status. However, we also observed that the evaluation of methylation status varied depending if the DNA was extracted from paraffin-embedded versus frozen tissue. Although the reason for this is unclear, we postulate that the timing from resection to fixation and the process of fixation itself may potentially alter methylation status in paraffin-embedded tumors and/or impair the faithful amplification of the MGMT promoter by methylation-specific PCR methodology.
References
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
van Rijn J, Heimans JJ, van den Berg J, van der Valk P, Slotman BJ (2000) Survival of human glioma cells treated with various combination of temozolomide and X-rays. Int J Radiat Oncol Biol Phys 47:779–784
Wedge SR, Porteous JK, Glaser MG, Marcus K, Newlands ES (1997) In vitro evaluation of temozolomide combined with X-irradiation. Anticancer Drugs 8:92–97
Wick W, Wick A, Schulz JB, Dichgans J, Rodemann HP, Weller M (2002) Prevention of irradiation-induced glioma cell invasion by temozolomide involves caspase 3 activity and cleavage of focal adhesion kinase. Cancer Res 62:1915–1919
Hegi ME, Diserens AC, Gorlia T et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003
Liu L, Markowitz S, Gerson SL (1996) Mismatch repair mutations override alkyltransferase in conferring resistance to temozolomide but not to 1,3-bis(2-chloroethyl)nitrosourea. Cancer Res 56:5375–5379
Ochs K, Kaina B (2000) Apoptosis induced by DNA damage O6-methylguanine is bcl-2 and caspase-9/3 regulated and Fas/caspase-8 independent. Cancer Res 60:5815–5824
Esteller M, Garcia-Foncillas J, Andion E et al (2000) Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med 343:1350–1354
Hegi ME, Diserens AC, Godard S et al (2004) Clinical trial substantiates the predictive value of O-6-methylguanine-DNA methyltransferase promoter methylation in glioblastoma patients treated with temozolomide. Clin Cancer Res 10:1871–1874
Juillerat-Jeanneret L, Bernasconi CC, Bricod C et al (2008) Heterogeneity of human glioblastoma: Glutathione-S-transferase and methylguanine-methyltransferase. Cancer Invest 26:597–609
Parkinson JF, Wheeler HR, Clarkson A et al (2008) Variation of O(6)-methylguanine-DNA methyltransferase (MGMT) promoter methylation in serial samples in glioblastoma. J Neurooncol 87:71–78
Srinivasan M, Sedmak D, Jewell S (2002) Effect of fixatives and tissue processing on the content and integrity of nucleic acids. Am J Pathol 161:1961–1971
Talaulikar D, Gray JX, Shadbolt B, McNiven M, Dahlstrom JE (2008) A comparative study of the quality of DNA obtained from fresh frozen and formalin-fixed decalcified paraffin-embedded bone marrow trephine biopsy specimens using two different methods. J Clin Pathol 61:119–123
Cao VT, Jung TY, Jung S et al (2009) The correlation and prognostic significance of MGMT promoter methylation and MGMT protein in glioblastomas. Neurosurgery 65:866–875
Grasbon-Frodl EM, Kreth FW, Ruiter M et al (2007) Intratumoral homogeneity of MGMT promoter hypermethylation as demonstrated in serial stereotactic specimens from anaplastic astrocytomas and glioblastomas. Int J Cancer 121:2458–2464
Nakagawa T, Ido K, Sakuma T, Takeuchi H, Sato K, Kubota T (2009) Prognostic significance of the immunohistochemical expression of O(6)-methylguanine-DNA methyltransferase, P-glycoprotein, and multidrug resistance protein-1 in glioblastomas. Neuropathology 29:379–388
Yachi K, Watanabe T, Ohta T et al (2008) Relevance of MSP assay for the detection of MGMT promoter hypermethylation in glioblastomas. Int J Oncol 33:469–475
Preusser M, Elezi L, Hainfellner JA (2008) Reliability and reproducibility of PCR-based testing of O6-methylguanine-DNA methyltransferase gene (MGMT) promoter methylation status in formalin-fixed and paraffin-embedded neurosurgical biopsy specimens. Clin Neuropathol 27:388–390
Wller M, Stupp R, Reifenberger G et al (2010) MGMT promoter methylation in malignant gliomas: ready for personalized medicine? Nat Rev Neurol 6:39–51
Cilengitide for subjects with newly diagnosed glioblastoma multiforme and methylated mgmt gene promoter—a multicenter, open-label, controlled phase III study, testing cilengitide in combination with standard treatment (temozolomide with concomitant radiation therapy, followed by temozolomide maintenance therapy) versus standard treatment alone. http://www.clinicaltrials.gov/ct2/show/NCT00689221. Accessed 16 Feb 2010
Cilengitide in subjects with newly diagnosed glioblastoma multiforme and unmethylated mgmt gene promoter—a multicenter, open-label phase ii study, investigating two cilengitide regimens in combination with standard treatment (temozolomide with concomitant radiation therapy, followed by temozolomide maintenance therapy). http://www.clinicaltrials.gov/ct2/show/NCT00813943. Accessed 16 Feb 2010
Acknowledgments
We would like to acknowledge Elizabeth Kornaga, Angela Chan, Jaclyn Vande Graaf and Annabelle Mastalic for their collaboration in this study. This study was supported in part by an Alberta Cancer Board Research Legacy Grant and the Brain Tumor Foundation of Canada.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
11060_2010_307_MOESM1_ESM.tif
Verification of patient 8 FFPE MGMT-MSP result: Figure 1a shows the original result for patient 8 FFPE tissues. Figure 1b is the result from an independent experiment using DNA re-extracted from FFPE tissues B, C and D in order to rule out possible PCR contamination. NTC = no template control, U87MG = methylation positive control, HTB30 = methylation negative control 1 (TIFF 907 kb)
Rights and permissions
About this article
Cite this article
Hamilton, M.G., Roldán, G., Magliocco, A. et al. Determination of the methylation status of MGMT in different regions within glioblastoma multiforme. J Neurooncol 102, 255–260 (2011). https://doi.org/10.1007/s11060-010-0307-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0307-5