Abstract
We conducted this study to determine whether the methylation status of the O6-methylguanine-DNA methyltransferase (MGMT) promoter was a prognostic marker for positive outcomes of gamma knife radiosurgery (GKS) for recurrent glioblastoma (GBM). We retrospectively examined 61 patients, who underwent GKS for local recurrent GBM between 2004 and 2015; in all patients, the methylation status of the MGMT promoter was identified via methylation-specific quantitative real-time polymerase chain reaction. All patients underwent surgical resection and were diagnosed histopathologically with GBM. Prognostic factors associated with progression-free survival (PFS) and overall survival (OS) were identified in univariate and multivariate analyses. Twenty-five (41%) had a methylated MGMT promoter, and 36 (59%) had an unmethylated MGMT promoter. The median age at GKS was 58 years. The median tumor volume at GKS was 7.0 cm3, and the median marginal dose was 16 Gy. The median follow-up period after GKS was 7.5 months. The median PFS time after GKS was 8.9 months (95% CI 4.3–13.5 months) in the methylated and 4.6 months (95% CI 3.7–5.5 months) in the unmethylated group (P = 0.016). The median OS time after GKS was 14.0 months (95% CI 9.3–18.7 months) in the methylated group and 9.0 months (95% CI 6.5–11.5 months) in the unmethylated group (P = 0.026). Methylation of the MGMT promoter correlated with better PFS and OS after GKS for recurrent GBM. Prospective comparative studies are required to determine whether MGMT methylation directly affects the efficiency of GKS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma (GBM) is the most common primary malignant brain tumor in adults. Its prognosis is dismal, with a median survival of 12–15 months. The standard of care for patients with newly diagnosed GBM was established in 2005 after a phase III trial by the European Organization for the Research and Treatment of Cancer/National Cancer Institute of Canada Clinical Trials Group [1]. Although there is no standard therapy for recurrence, several studies recommend gamma knife radiosurgery (GKS) for surgically inaccessible or small recurrent GBMs, despite limitations such as a narrow therapeutic window between tumor control and radiation necrosis [2,3,4,5].
Hegi et al. analyzed prognosis according to the methylation status of the O6-methylguanine-DNA methyltransferase (MGMT) promoter in patients with GBMs who received the alkylating agent temozolomide (TMZ) plus radiotherapy or radiotherapy alone [6]. Their results showed a significant association between methylated MGMT promoter and better prognosis in the radiotherapy plus TMZ group, as well as a trend toward improved overall survival and progression-free survival in the radiotherapy alone group. In the study by Rivera et al. [7], the methylation status of the MGMT promoter predicted response to radiotherapy in the absence of adjuvant alkylating agents in patients with newly diagnosed GBM. Moreover, Metellus et al. found that MGMT promoter methylation was an important predictive factor in patients with recurrent GBM who received surgery and chemotherapy [8].
Currently, no studies have reported the outcomes of GKS according to MGMT promoter methylation status. The purpose of this study was to investigate whether MGMT promoter methylation was a prognostic biomarker in patients who received GKS for recurrent GBM.
Methods
Patient population
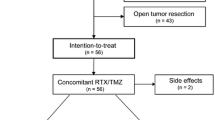
Our study consisted of 61 patients who underwent GKS for local recurrent GBM between 2004 and 2015. All GBMs showed progression on serial imaging after concurrent chemoradiotherapy (CCRT). All patients had information on the methylation status of the MGMT promoter, as determined via methylation-specific polymerase chain reaction (PCR). Institutional Review Board of our hospital approved this study.
Treatment protocols
All patients underwent maximal surgical resection within feasible limits and were histopathologically diagnosed as GBM. The extent of resection was determined via gadolinium-enhanced brain magnetic resonance imaging (MRI) performed within 48 h after surgery and was classified as gross total resection (GTR), subtotal resection (STR), partial resection (PR), or biopsy (Bx). GTR was defined as >99% removal of the initial tumor, STR as 50–99%, and PR as <50%. Patients received CCRT with TMZ within 6 weeks after pathological confirmation of GBM. CCRT consisted of continuous delivery of 75 mg/m2 TMZ per day for 6 weeks combined with a total 50–60 Gy (2 Gy 5 days per week for 6 weeks), followed by six cycles of adjuvant TMZ (150–200 mg/m2 for 5 days every 28 days).
MRI was performed before the first cycle and after every two or three cycles of adjuvant TMZ. Radiologic outcomes were defined according to the Response Assessment in Neuro-Oncology criteria. All patients received GKS as a salvage treatment at the time of first progression. Follow-up MRI after GKS for recurrent GBM was conducted every 3 months or whenever neurological changes suggested tumor progression or treatment complications.
Quantitative real-time (qRT) methylation-specific PCR for MGMT promoter methylation
We removed the largest amount of tumor possible during surgery. Formalin-fixed, paraffin-embedded (FFPE) GBM samples were stained with hematoxylin-eosin to estimate tumor cell content (at least 85%) and to exclude necrotic area and non-neoplastic tissues. For DNA extraction, 5-µm-thick tissue sections from all paraffin blocks were homogenized, deparaffinized and dehydrated.
MGMT promoter methylation was analyzed via methylation-specific PCR using the PRISM 7900HT FAST Real-time PCR system (Applied Biosystems, Foster City, CA, USA) and HotStart-IT SYBR Green qPCR Master Mix (USB, Cleveland, OH, USA). The PCR protocol was as follows: preheating at 50 °C for 2 min, 95 °C for 10 min, followed by 40 cycles at 95 °C for 15 s and 60 °C for 1 min. β-actin gene (ACTB) was used to control for methylation-independent reactions. For relative quantification, the amount of methylated DNA (percentage of methylated reference, PMR) in the MGMT promoter region was normalized to the methylation value of the calibrator, which was defined as 100%. Universal methylated DNA (Qiagen, Hilden, Germany) was used as the calibrator. The PMR was defined as 100 × 2 [sample ACTB (ct) − sample MGMT (ct)]/2[calibrator ACTB (ct) − calibrator MGMT (ct)]. A methylation level ≥3 was considered methylated and <3 was considered unmethylated.
GKS procedure
All patients were initially placed in a type G Leksell stereotactic frame under local anesthesia, followed by contrast-enhanced MRI for dose planning. Images were transferred to Leksell Gamma Knife planning stations (Elekta Instruments, Crawley, United Kingdom), and dose planning was performed using GammaPlan software, versions 5.31, 5.32, 5.34, and 9.0. A contrast-enhanced lesion was delineated as a target with no margins added.
A staff physician and a physicist were involved in treatment planning and target volume determinations for all patients. The same physician measured the tumor volume in all cases as part of the routine GKS procedure, and a second reader, who was blinded to the patients included in this study, checked the tumor volume again; differences in tumor volumes between the two readers were not significant. The treated median tumor volume was 7.0 cm3 (range 0.033–35.1 cm3). Tumor volume was determined by consensus between two observers (B.S.K. and J.-I.L), and the intraclass correlation coefficient (ICC) was used to determine interobserver agreement for the reliability of the tumor volume measurement (ICC = 0.993).
The median marginal dose delivered was 16 Gy (range 9–25 Gy). Irradiation was performed using a Leksell Gamma Knife type B, C, or Perfexion system. Each patient received a 10-mg loading dose of dexamethasone in the morning on the day of GKS followed by 5 mg after completion.
Statistical analysis
Progression-free survival (PFS) was measured from the date of the first GKS to documented disease progression or the date of the last follow-up. Overall survival (OS) was measured from the date of the first GKS to death or the date of the last follow-up. Patients alive at the time of analysis or lost to follow-up were included as censored observations. OS and PFS were the endpoints of the analysis, and prognostic and outcome variables associated with OS and PFS [age at first GKS, pre-GKS Karnofsky performance scale (KPS) score, MGMT promoter methylation status, preplanning tumor volume, marginal dose for GKS, and combination of GKS and TMZ] were examined via univariate and multivariate analyses. OS and PFS were calculated using the Kaplan–Meier method (SPSS software, version 23.0; IBM Corp., Armonk, NY). Differences between the survival curves were evaluated by using the log-rank test. A Cox proportional hazards model was used for multivariate comparisons of median OS and PFS values. Differences between groups were considered statistically significant at P < 0.05.
Results
Patients’ characteristics and overall outcomes after GKS
The patients’ characteristics are shown in Table 1. Of the 61 included patients, 34 (55.7%) were men and 27 (44.3%) were women, with a median age at first GKS of 58 years (range 27–79). The median pre-GKS KPS score was 80 (range 40–90). Fifty-three (86.9%) patients had a pre-GKS KPS score ≥70, including 24 of 25 (96%) in the methylated group and 29 of 36 (80.5%) in the unmethylated group. One (4%) patient in the methylated group and seven (19.5%) patients in the unmethylated group had KPS scores <70. One patient in the methylated group had a KPS score of 40. In the unmethylated group, one patient had a KPS score of 50, and six patients had a KPS score of 60.
All patients underwent surgery, and GBM was histopathologically confirmed. After surgery, GTR was achieved in 32 (52.5%) patients, STR in 24 (39.3%), and Bx in 5 (8.2%). Fifty-eight (95.1%) patients received CCRT with TMZ after resection or biopsy; the median dose for radiotherapy was 60 Gy (range 54–61.5 Gy), delivered in conventional fractions of 2 Gy per day. After CCRT, 54 of the 58 (93.1%) patients received one to six cycles of TMZ (median, six).
At the second recurrence after GKS, patients received repeat GKS (40 patients, 65.6%), repeat GKS plus TMZ (20 patients, 32.8%), or repeat GKS plus irinotecan/bevacizumab (1 patient, 1.6%). TMZ chemotherapy was either metronomic (13 patients, 65%) or conventional. Three (15.0%) of the 20 patients who received both GKS and TMZ underwent a second operation. The radiation doses used in GKS are shown in Table 2.
Among all patients, 25 (41.0%) had a methylated MGMT promoter and 36 (59.0%) had an unmethylated MGMT promoter. The median follow-up time after initial diagnosis was 18.5 months (range 2.3–110.6 months), and the median follow-up time after GKS was 7.5 months (range 0.1–36.0 months). The median time from initial diagnosis to GKS was 9.8 months (range 1.7–101.5 months). At the time of analysis, 15 (24.6%) patients were alive. The median OS was 22.1 months (range 18.8–25.4 months) after initial diagnosis, and 11 months (95% CI 8.4–13.6 months) after GKS. At the 6-month, 1-year, and 2-year follow-up after GKS, the OS rates were 78.5, 43.7, and 13.7%, respectively. The median PFS time after GKS was 5 months (95% CI 3.8–6.2 months), and the 6-month and 1-year PFS rates were 38.4 and 16.7%, respectively.
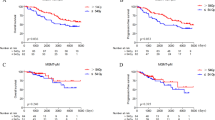
Univariate and multivariate analyses for progression and survival
The following factors were included in the univariate and multivariate analyses: age (<50 years vs. ≥50 years), KPS (<70 vs. 70–80 vs. 90–100), MGMT methylation status (methylated vs. unmethylated), preplanning tumor volume according to MGMT methylation status (<7 cm3/unmethylated vs. ≥7 cm3/unmethylated vs. <7 cm3/methylated vs. ≥7 cm3/methylated), marginal dose at GKS (≥16 Gy vs. <16 Gy), and combination of TMZ at GKS (yes or no). MGMT methylation status was the strongest predictor of PFS (P = 0.016) and OS (P = 0.026) in the univariate analysis. However, in the multivariate analysis, MGMT methylation status significantly correlated with OS only (P = 0.03). Preplanning tumor volume significantly correlated with PFS in the univariate (P = 0.008) and multivariate (P = 0.005) analyses regardless of methylation status. There was a significant association between KPS score at the time of GKS and OS in the univariate analysis (P = 0.049), and between marginal dose and PFS in the multivariate analysis. The PFS and OS values did not significantly different between GKS alone (P = 0.583) and GKS plus TMZ (P = 0.159).
Impact of MGMT promoter methylation on PFS and OS after GKS
The time to progression after GKS was longer when the MGMT promoter was methylated (Fig. 1). The median PFS time was 8.9 months (95% CI 4.3–13.5 months) for the methylated promoter and 4.6 months (95% CI 3.7–5.5 months) for the unmethylated promoter (P = 0.016). Methylated MGMT promoter was also associated with better OS (Fig. 2 ). The median OS time was 14.0 months (95% CI 9.3–18.7 months) for the methylated MGMT promoter and 9.0 months (95% CI 6.5–11.5 months) for the unmethylated promoter (P = 0.026). In the methylated group, the actuarial 6-month and 1-year OS rates were 79.4 and 51.3%, respectively; in the unmethylated group, they were 75.0 and 34.8%, respectively. The actuarial 1-year OS rate was higher when the MGMT promoter was methylated versus unmethylated (51.3 vs. 34.8%). Post-progression therapies at recurrence or progression after GKS are shown in Table 3.
Kaplan–Meier curve showing progression-free survival (PFS) after gamma knife radiosurgery according to O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation status. Patients with a methylated MGMT promoter had a longer PFS time than those with an unmethylated MGMT promoter (8.9 vs. 4.6 months)
Treatment-related complications
Adverse effects of GKS included radiation necrosis, acute radiation effect (ARE), and intracranial hemorrhage (ICH) with intraventricular hemorrhage (IVH). Radiation necrosis induced by GKS was observed in 5 (8.2%) of 61 patients. Based on the results of a follow-up MRI, 3 of 5 patients with suspected radiation-induced necrosis underwent surgical resection, after which necrosis was confirmed histologically. ARE and ICH with IVH was observed in 1 patient with a methylated MGMT promoter. Radiation necrosis was found in 1 patient with methylated MGMT promoter and 4 patients with an unmethylated MGMT promoter. Repeat follow-up MRI, magnetic resonance spectroscopy, or positron emission tomography were used to differentiate tumor recurrence and radiation necrosis. No other National Cancer Institute Common Toxicity Criteria grade 3 or 4 toxicities were observed.
Discussion
Despite advances in various treatment modalities, no current standard treatment for recurrent GBM exists. Stereotactic radiosurgery (SRS), which includes GKS, has been used as an alternative for surgery in a variety of intracranial tumors cases. However, whether SRS provides a survival benefit for patients with recurrent GBM is controversial. This study shows a strong association between MGMT promoter methylation and better PFS and OS after GKS for recurrent GBM.
Several studies report that SRS effectively treats recurrent GBM [2, 9, 10], conferring survival benefits after performance of Stupp’s protocol, either alone or in combination with chemotherapy [2, 11,12,13,14,15,16,17,18,19,20]. Based on an analysis of 187 patients with recurrent GBM who underwent SRS at a median marginal dose of 16 Gy, Imber et al. concluded that GKS benefits patients with local recurrence, especially younger patients with a tumor volume ≤5 cm3 [21]. Other studies also attest to the efficacy of GKS for recurrent GBM. Studies have also reported that GKS might be effective in selected patients with recurrent GBM [3, 5, 9, 22,23,24,25,26,27,28]. However, this conclusion is limited by selection bias owing to the retrospective design of the studies. Hence, a randomized clinical trial is needed to determine whether salvage GKS truly prolongs OS and PFS in patients with recurrent GBM. The only relevant published trial thus far is the Radiation Therapy Oncology Group 93-05 study [10], which examined the usefulness of an upfront SRS boost to conventional radiotherapy and carmustine chemotherapy for newly diagnosed GBM; it did not, however, demonstrate a survival benefit. A study performed at our institute [3] suggests that SRS is effective when used as a salvage treatment for recurrent GBM, despite the limitations of a comparison study with a historic control group. The median OS after SRS was 13 months (95% CI 10.6–16.0 months), and the median PFS was 4.6 months (95% CI 4.0–5.2 months), both of which are comparable to the outcomes in this study.
Several studies suggest that the methylation status of the MGMT promoter can predict the response to TMZ in patients with newly diagnosed GBM. However, few studies have assessed MGMT promoter methylation in patients with recurrent (compared with primary) GBM [6, 29, 30]. Felsberg et al. used methylation-specific PCR to analyze paired samples of primary and recurrent GBM in 80 patients who underwent radiotherapy and TMZ chemotherapy after their first surgery [31]. They found that the MGMT methylation status of 90% of the recurrent samples was similar to that of the primary samples. In paired analyses of 64 patients treated with radiotherapy plus TMZ, the MGMT methylation status was retained in 89.1% of recurrent tumor samples and was a prognostic factor for salvage chemotherapy with alkylating agents.
Using methylation-specific qRT PCR, Rivera et al. examined MGMT promoter methylation levels in tumor samples from 225 patients with newly diagnosed GBM prior to treatment [7]. All patients underwent external beam radiation therapy, but 172 did not undergo adjuvant chemotherapy until after the first tumor recurrence. The median PFS times were 31 and 15 weeks in the methylated and unmethylated promoter group (P = 0.009) and the median OS times were 63 and 51 weeks (P = 0.019), respectively. The authors concluded that MGMT promoter methylation was an independent prognostic factor for progression and survival and suggested that it might also predict the radiation response. In contrast, Crinière et al. found that MGMT promoter methylation did not correlate with survival in 85 patients with GBMs treated via radiotherapy without adjuvant chemotherapy: median OS times were 15.1 and 10.2 months in the methylated and unmethylated groups, respectively (P = 0.407) [32]. However, in that study, methylation was assessed by two-stage PCR.
Our results show a nearly twofold delay in tumor progression when the MGMT promoter is methylated vs. unmethylated (8.9 vs. 4.6 months, P = 0.016). MGMT promoter methylation also conferred a survival benefit: the median OS time was 14 months when the promoter methylation was methylated vs. 9 months when it was not (P = 0.026). MGMT promoter methylation was also an independent prognostic factor for progression and survival after GKS for recurrent GBM.
There are several limitations to this study. First, it was retrospective study and did not include a randomized control group; hence, selection bias is possible. Second, the sample size was insufficient for analysis of multiple prognostic factors. Third, treatment and assessment were not performed in accordance with a strictly standardized protocol. For example, the treatments after GKS were diverse, which may have confounded the analysis. Finally, we did not completely compensate for tumor heterogeneity. A recent study identified transcriptional intratumoral heterogeneity in 40% of GBMs, with variable MGMT methylation levels in 14% [33]. It is important to take multiple biopsies from a tumor in order to correctly classify the patients; however, in practical terms, this is not always feasible. Alternatively, we removed the largest amount of tumor possible for assessment of MGMT methylation status after homogenization of the sample.
Conclusion
Methylation of the MGMT promoter was associated with better PFS and OS after GKS for recurrent GBM. Because this association is correlative rather than causative, prospective comparative studies are needed to determine whether MGMT methylation directly affects the therapeutic efficiency of GKS.
References
Stupp R, Mason WP, Van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO, European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups, National Cancer Institute of Canada Clinical Trials Group (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. doi:10.1056/NEJMoa043330
Combs SE, Widmer V, Thilmann C, Hof H, Debus J, Schulz-Ertner D (2005) Stereotactic radiosurgery (SRS): treatment option for recurrent glioblastoma multiforme (GBM). Cancer 104:2168–2173. doi:10.1002/cncr.21429
Kong DS, Lee JI, Park K, Kim JH, Lim DH, Nam DH (2008) Efficacy of stereotactic radiosurgery as a salvage treatment for recurrent malignant gliomas. Cancer 112:2046–2051. doi:10.1002/cncr.23402
Mahajan A, McCutcheon IE, Suki D, Chang EL, Hassenbusch SJ, Weinberg JS, Shiu A, Maor MH, Woo SY (2005) Case-control study of stereotactic radiosurgery for recurrent glioblastoma multiforme. J Neurosurg 103:210–217. doi:10.3171/jns.2005.103.2.0210
Skeie BS, Enger PO, Brogger J, Ganz JC, Thorsen F, Heggdal Ji, Pedersen PH (2012) γ knife surgery versus reoperation for recurrent glioblastoma multiforme. World Neurosurg 78:658–669. doi:10.1016/j.wneu.2012.03.024
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JE, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003. doi:10.1056/NEJMoa043331
Rivera AL, Pelloski CE, Gilbert MR, Colman H, De La Cruz C, Sulman EP, Bekele BN, Aldape KD (2010) MGMT promoter methylation is predictive of response to radiotherapy and prognostic in the absence of adjuvant alkylating chemotherapy for glioblastoma. Neuro Oncol 12:116–121. doi:10.1093/neuonc/nop020
Metellus P, Coulibaly B, Nanni I, Fina F, Eudes N, Giorgi R, Barrie M, Chinot O, Fuentes S, Dufour H, Ouafik L, Figarella-Branger D (2009) Prognostic impact of O6-methylguanine-DNA methyltransferase silencing in patients with recurrent glioblastoma multiforme who undergo surgery and carmustine wafer implantation: a prospective patient cohort. Cancer 115:4783–4794. doi:10.1002/cncr.24546
Hsieh PC, Chandler JP, Bhangoo S, Panagiotopoulos K, Kalapurakal JA, Marymont MH, Cozzens JW, Levy RM, Salehi S (2005) Adjuvant gamma knife stereotactic radiosurgery at the time of tumor progression potentially improves survival for patients with glioblastoma multiforme. Neurosurgery 57:684–692. doi:10.1227/01.neu.0000175550.96901.a3
Souhami L, Seiferheld W, Brachman D, Podgorsak EB, Werner-Wasik M, Lustig R, Schultz CJ, Sause W, Okunieff P, Buckner J, Zamorano L, Mehta MP, Curran WJ Jr (2004) Randomized comparison of stereotactic radiosurgery followed by conventional radiotherapy with carmustine to conventional radiotherapy with carmustine for patients with glioblastoma multiforme: report of radiation therapy oncology group 93-05 protocol. Int J Radiat Oncol Biol Phys 60:853–860. doi:10.1016/j.ijrobp.2004.04.011
Shrieve DC, Alexander E 3rd, Wen PY, Fine HA, Kooy HM, Black PM, Loeffler JS (1995) Comparison of stereotactic radiosurgery and brachytherapy in the treatment of recurrent glioblastoma multiforme. Neurosurgery 36:275–282
Vordermark D, Kölbl O, Ruprecht K, Vince GH, Bratengeier K, Flentje M (2005) Hypofractionated stereotactic re-irradiation: treatment option in recurrent malignant glioma. BMC Cancer 5:55. doi:10.1186/1471-2407-5-55
Fogh SE, Andrews DW, Glass J, Curran W, Glass C, Champ C, Evans JJ, Hyslop T, Pequignot E, Downes B, Comber E, Maltenfort M, Dicker AP, Werner-Wasik M (2010) Hypofractionated stereotactic radiation therapy: an effective therapy for recurrent high-grade gliomas. J Clin Oncol 28:3048–3053. doi:10.1200/JCO.2009.25.6941
Maranzano E, Anselmo P, Casale M, Trippa F, Carletti S, Principi M, Loreti F, Italiani M, Caserta C, Giorgi C (2011) Treatment of recurrent glioblastoma with stereotactic radiotherapy: long-term results of a mono-institutional trial. Tumori 97:56–61
Greenspoon JN, Sharieff W, Hirte H, Overholt A, Devillers R, Gunnarsson T, Whitton A (2014) Fractionated stereotactic radiosurgery with concurrent temozolomide chemotherapy for locally recurrent glioblastoma multiforme: a prospective cohort study. Onco Targets Ther 7:485–490. doi:10.2147/OTT.S60358
Lederman G, Arbit E, Odaimi M, Wertheim S, Lombardi E (1997) Recurrent glioblastoma multiforme: potential benefits using fractionated stereotactic radiotherapy and concurrent taxol. Stereotact Funct Neurosurg 69:162–174
Hudes RS, Corn BW, Werner-Wasik M, Andrews D, Rosenstock J, Thoron L, Downes B, Curran WJ Jr (1999) A phase I dose escalation study of hypofractionated stereotactic radiotherapy as salvage therapy for persistent or recurrent malignant glioma. Int J Radiat Oncol Biol Phys 43:293–298
Cuneo KC, Vredenburgh JJ, Sampson JH, Reardon DA, Desjardins A, Peters KB, Friedman HS, Willett CG, Kirkpatrick JP (2012) Safety and efficacy of stereotactic radiosurgery and adjuvant bevacizumab in patients with recurrent malignant gliomas. Int J Radiat Oncol Biol Phys 82:2018–2024. doi:10.1016/j.ijrobp.2010.12.074
Minniti G, Scaringi C, De Sanctis V, Lanzetta G, Falco T, Di Stefano D, Esposito V, Enrici RM (2013) Hypofractionated stereotactic radiotherapy and continuous low-dose temozolomide in patients with recurrent or progressive malignant gliomas. J Neurooncol 111:187–194. doi:10.1007/s11060-012-0999-9
Lederman G, Wronski M, Arbit E, Odaimi M, Wertheim S, Lombardi E, Wrzolek M (2000) Treatment of recurrent glioblastoma multiforme using fractionated stereotactic radiosurgery and concurrent paclitaxel. Am J Clin Oncol 23:155–159
Imber BS, Kanungo I, Braunstein S, Barani IJ, Fogh SE, Nakamura JL, Berger MS, Chang EF, Molinaro AM, Cabrera JR, McDermott MW, Sneed PK, Aghi MK (2016) Indications and efficacy of Gamma Knife stereotactic radiosurgery for recurrent glioblastoma: 2 decades of institutional experience. Neurosurgery. doi:10.1227/neu.0000000000001344
Larson EW, Peterson HE, Lamoreaux WT, MacKay AR, Fairbanks RK, Call JA, Carlson JD, Ling BC, Demakas JJ, Cooke BS, Lee CM (2014) Clinical outcomes following salvage Gamma Knife radiosurgery for recurrent glioblastoma. World J Clin Oncol 5:142–148. doi:10.5306/wjco.v5.i2.142
Park KJ, Kano H, Iyer A, Liu X, Niranjan A, Flickinger JC, Lieberman FS, Lunsford LD, Kondziolka D (2012) Salvage gamma knife stereotactic radiosurgery followed by bevacizumab for recurrent glioblastoma multiforme: a case-control study. J Neurooncol 107:323–333. doi:10.1007/s11060-011-0744-9
Koga T, Maruyama K, Tanaka M, Ino Y, Saito N, Nakagawa K, Shibahara J, Todo T (2012) Extended field stereotactic radiosurgery for recurrent glioblastoma. Cancer 118:4193–4200. doi:10.1002/cncr.27372
Elliott RE, Parker EC, Rush SC, Kalhorn SP, Moshel YA, Narayana A, Donahue B, Golfinos JG (2011) Efficacy of gamma knife radiosurgery for small-volume recurrent malignant gliomas after initial radical resection. World Neurosurg 76:128–140. doi:10.1016/j.wneu.2010.12.053
Pouratian N, Crowley RW, Sherman JH, Jagannathan J, Sheehan JP (2009) Gamma knife radiosurgery after radiation therapy as an adjunctive treatment for glioblastoma. J Neurooncol 94:409–418. doi:10.1007/s11060-009-9873-9
Kida Y, Yoshimoto M, Hasegawa T (2009) Radiosurgery for intracranial gliomas. Prog Neurol Surg 22:122–128. doi:10.1159/000163387
Kohshi K, Yamamoto H, Nakahara A, Katoh T, Takagi M (2007) Fractionated stereotactic radiotherapy using gamma unit after hyperbaric oxygenation on recurrent high-grade gliomas. J Neurooncol 82:297–303. doi:10.1007/s11060-006-9283-1
Weller M, Stupp R, Reifenberger G, Brandes AA, van den Bent MJ, Wick W, Hegi ME (2010) MGMT promoter methylation in malignant gliomas: ready for personalized medicine? Nat Rev Neurol 6:39–51. doi:10.1038/nrneurol.2009.197
Dunn J, Baborie A, Alam F, Joyce K, Moxham M, Sibson R, Crooks D, Husband D, Shenoy A, Brodbelt A, Wong H, Liloglou T, Haylock B, Walker C (2009) Extent of MGMT promoter methylation correlates with outcome in glioblastomas given temozolomide and radiotherapy. Br J Cancer 101:124–131. doi:10.1038/sj.bjc.6605127
Felsberg J, Thon N, Eigenbrod S, Hentschel B, Sabel MC, Westphal M, Schackert G, Kreth FW, Pietsch T, Löffler M, Weller M, Reifenberger G, Tonn JC, German Glioma Network (2011) Promoter methylation and expression of MGMT and the DNA mismatch repair genes MLH1, MSH2, MSH6 and PMS2 in paired primary and recurrent glioblastomas. Int J Cancer 129:659–670. doi:10.1002/ijc.26083
Crinière E, Kaloshi G, Laigle-Donadey F, Lejeune J, Auger N, Benouaich-Amiel A, Everhard S, Mokhtari K, Polivka M, Delattre JY, Hoang-Xuan K, Thillet J, Sanson M (2007) MGMT prognostic impact on glioblastoma is dependent on therapeutic modalities. J Neurooncol 83:173–179. doi:10.1007/s11060-006-9320-0
Parker NR, Hudson AL, Khong P, Parkinson JF, Dwight T, Ikin RJ, Zhu Y, Cheng ZJ, Vafaee F, Chen J, Wheeler HR, Howell VM (2016) Intratumoral heterogeneity identified at the epigenetic, genetic and transcriptional level in glioblastoma. Sci Rep 6:22477. doi:10.1038/srep22477
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, B.S., Kong, DS., Seol, H.J. et al. MGMT promoter methylation status as a prognostic factor for the outcome of gamma knife radiosurgery for recurrent glioblastoma. J Neurooncol 133, 615–622 (2017). https://doi.org/10.1007/s11060-017-2478-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2478-9