Abstract
MicroRNAs (miRNAs) are small noncoding RNAs comprising 21–23 nucleotides that regulate gene expression by transcriptionally repressing their complementary mRNAs. In particular, let-7 miRNA has been postulated to function as a tumor suppressor in various cancer cells, but not yet in glioblastoma. In this study, we investigated the anti-tumorigenic effect of let-7 miRNA in glioblastoma cells. Human glioblastoma cells (U251 or U87 cells) were transfected with let-7 miRNA and assayed for in-vitro proliferation, migration, and in-vivo tumor formation. Transfection of let-7 miRNA reduced expression of pan-RAS, N-RAS, and K-RAS in the glioblastoma cells. Let-7 miRNA also reduced the in-vitro proliferation and migration of the cells, and reduced the sizes of the tumors produced after transplantation into nude mice. However, let-7 miRNA exerted no effect on the proliferation of normal human astrocytes. These results indicate that let-7 miRNA has an anti-tumorigenic effect on glioblastoma cells, and suggest possible use of let-7 miRNA for treating glioblastoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma is the most common primary malignant brain tumor found in adults, and patients respond poorly to chemotherapy, except for a small subgroup that benefits from administration of temozolomide or epidermal growth factor receptor (EGFR) kinase inhibitor [1]. MicroRNAs (miRNA) are small, noncoding RNAs with 21–23 nucleotides that regulate gene expression by repressing transcription or degrading target mRNA [2]. In cancer cells, miRNAs can function as tumor suppressors or oncogenes, and, thus, can regulate tumor development and prognosis [3].
In particular, let-7 miRNA has been postulated to function as a tumor suppressor by silencing RAS and high mobility group AT-hook 2 (HMGA2) [4, 5]. Let-7 was originally identified in C. elegans as a regulator of developmental timing and cellular proliferation [6], and several let-7 congeners (let-7a–k) have since been identified. Let-7 has been reported to be reduced in human lung cancer [7], colon cancer [8], and melanoma [9], and the delivery of let-7 has been found to reduce cancer cell proliferation and tumorigenicity [10, 11]. On the other hand, the oncogene Ras is a member of the small GTPase superfamily and the signaling mediator of ephrin receptors, and has been implicated in cancer cell physiology, particularly in cell proliferation, adhesion, and migration [12]. In glioblastoma, Ras signaling regulates glioblastoma cell growth, survival, and invasion [13], and Ras inhibition reduces tumorigenicity and the migration potential of glioblastoma cells [14, 15]. The above-mentioned results suggest that let-7 miRNA is likely to reduce glioblastoma growth and cellular migration via Ras inhibition. Thus, in this study, we investigated the effect of let-7 miRNA delivery on the proliferation, migration, and tumorigenicity of glioblastoma cells.
Materials and methods
Cell culture and miRNA transfection
U251 and U87 human glioblastoma cells were obtained from the American Type Culture Collection (Manassas, VA, USA), and cultured in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 2 mmol/L l-glutamine, 2 mmol/L sodium pyruvate, 100 units/mL penicillin, 100 μg/mL streptomycin, and 0.25 μg/mL amphotericin B (all from Gibco, Invitrogen, Carlsbad, CA, USA). Normal human astrocytes (Lonza, Basel, Switzerland) were cultured in Clonetics AGM Bulletkit (Lonza). Cells were maintained in a humidified 5% CO2 atmosphere at 37°C. Prepared cells were transfected in 24-well plates with pre-let-7 g (Ambion, Applied Biosystems, Foster City, CA, USA), a negative control miRNA (Ambion), or a cy3-labeled negative control miRNA (Ambion), using Lipofectamine 2000 (Invitrogen). Of the known let-7 family members, let-7 g was selected for this study on the basis of its proved action on lung cancer cells [11]; the mature sequence of let-7g is 5′-uga ggu agu agu uug uac agu u-3′.
Immunocytochemistry
Cell cultures were processed for immunocytochemistry, as previously described [16]. Cells (5 × 103) were plated on 12-mm round Aclar plastic coverslips coated with 10 μg/ml polylysine and housed in 35 mm dishes. Samples were fixed in 4% paraformaldehyde in phosphate-buffered saline (PBS, pH 7.5) for 40 min, washed with PBS, incubated for 2 h with blocking buffer (2% horse serum/1% BSA/0.1% Triton X-100 in PBS, pH 7.5), and incubated with primary antibodies overnight at 4°C. Anti-human Pan-RAS (Santa Cruz Biotechnology, Santa Cruz, CA, USA), N-RAS (Santa Cruz Biotechnology), and K-RAS antibodies (Santa Cruz Biotechnology) were used as primary antibodies. The cells were then incubated for 1 h at room temperature with secondary antibodies. Fluorescein isothiocyanate (FITC)-conjugated anti-rabbit IgG antibody (1:300; Jackson Immunoresearch, West Grove, PA, USA) was used as secondary antibody. Nuclei were counterstained with 4′,6-diamidino-2-phenylindole (DAPI; Vector Laboratories, Burlingame, CA, USA) after each experiment. The optical densities (OD) of RAS expression were analyzed quantitatively using an image-analysis system (Image Pro-Plus, Media Cybernetics, Bethesda, MD, USA). Five color images were acquired randomly per experiment group using a digital camera connected to a fluorescence microscope, and transformed to gray-scale images. Mean light transmission was measured on a scale of 0–256 relative units and averaged.
WST-1 assays
Cell proliferations were determined by WST-1 assay agent (5 mmol/l, 1:9; Roche, Basel, Switzerland), according to the manufacturer’s instructions. Higher values indicate greater cell numbers. Absorbances were measured at 450 nm (reference at 630 nm) using a Multiskan JX microplate reader (Thermo Fisher Scientific, Waltham, MA, USA). Experiments were performed in quadruplicate.
The in-vitro scratch migration assay
Glioblastoma cells were seeded into 24-well plates and cultured to subconfluence. Cell monolayers were then scratched with a 1,000-μl plastic pipette tip to create a cell-free area (a “wound”) approximately 2 mm wide [16]. Wounded monolayers were washed twice with culture medium to remove loose cell debris, and wounds were photographed under a phase-contrast microscope. Cell migration was quantified after 24 h by counting cells that had migrated into the wounded areas, and the relative cell migration (%) was calculated as [the number of let-7-treated cells that migrated into wounds/the number of control-miRNA-treated cells that migrated into wounds] × 100. Experiments were performed in triplicate.
In-vivo assays
Six-week-old male nude mice (Orient, Seoul, South Korea; n = 4) were used as hosts for glioblastoma xenografts. Briefly, let-7-transfected U251 or control U251 cells were harvested, washed twice, resuspended in cold PBS at 5 × 106/100 μL, and injected subcutaneously into flanks using a 25-gauge needle (n = 4 tumors per group). The animals were kept under pathogen-free conditions and tumors were removed 14 days after transplantation and weighed. All experiments on animals were approved by the ethics committee at our institution.
Statistical analysis
Results are presented as means ± SD. The Mann–Whitney U test was used to determine the significance of inter-group differences. SPSS ver. 15.0 (SPSS, Chicago, IL, USA) was used for the analyses, and two-tailed P values of <0.05 were considered significant.
Results
Let-7 miRNA transfection reduced RAS levels in vitro
In a preliminary study on the transfection of Cy3-labeled-negative control miRNA in U251 glioblastoma cells, cy3-immunofluorescence was maximum at 100 nM concentration, and higher concentrations of control miRNA caused cell deaths (Fig. 1a). On the basis of this result, we used 100 nM miRNA for further transfection experiments.
Transfection of let-7 and RAS levels. a Cy3-labeled-control miRNA was tested for transfection efficiency in U251 glioblastoma cells at concentrations of 0–200 nM, and 100 nM was selected for further studies. b Let-7 miRNA-transfected U251 glioblastoma cells showed lower levels of pan-RAS, N-RAS, and K-RAS than cells transfected with control miRNA (representative photographs). c Optical density analysis of their immunofluorescence confirmed these results. *P < 0.05 versus the control
Control or let-7 miRNAs were transfected into U251 cells, and RAS protein levels were evaluated at 48 h post-transfection. Let-7 miRNA transfection reduced the expressions of pan-RAS (relative optical densities versus β-actin; control = 0.62 ± 0.12, let-7 = 0.33 ± 0.10), N-RAS (control = 1.41 ± 0.25, let-7 = 0.49 ± 0.05), and K-RAS (control = 0.54 ± 0.06, let-7 = 0.19 ± 0.07) compared with the control miRNA transfection (all P < 0.05; Fig. 1b, c).
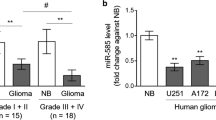
Let-7 miRNA reduced the in-vitro proliferation and migration of glioblastoma cells
We then investigated the effect of let-7 miRNA on glioblastoma cell proliferation. At 24 h post-transfection, the cellular densities of let-7-transfected U251 cells were slightly lower than those of cells transfected with control miRNA (Fig. 2a). At 48 h, WST-1 assays confirmed significantly lower cell numbers in the let-7-transfected U251 cells compared with the control miRNA-transfected U251 cells (control miRNA = 1.00 ± 0.16, let-7 = 0.80 ± 0.15, *P < 0.05, relative levels) (Fig. 2b). In experiments using U87 glioblastoma cells, let-7 transfection reduced the cell proliferation again (control miRNA = 1.00 ± 0.21, let-7 = 0.83 ± 0.11, *P < 0.05, relative levels), confirming the inhibitory effect of let-7 on glioblastoma cell proliferation in the second cell line (Fig. 2b). In contrast, human normal astrocytes transfected with let-7 showed no significant reduction of cell proliferation compared with the cells transfected with the control miRNA (control miRNA = 1.00 ± 0.14, let-7 = 1.06 ± 0.21, *P = 0.667, relative levels) (Fig. 2b), suggesting that let-7 miRNA has a different anti-proliferative effect on glioblastoma cells and normal astrocytes.
In-vitro inhibition of proliferation and migration by let-7 transfection. a The cellular densities of cultures of U251 and U87 glioblastoma cells transfected with let-7 were slightly lower than those of control transfected cells 24 h after transfection (representative photograph). However, the cellular densities of astrocytes were similar for control and let-7 transfections. b In the WST-1 assay 48 h after transfection, cell numbers were lower for let-7-transfected U251 and U87 glioblastoma cells than for control miRNA transfection, whereas cell numbers for let-7-transfected astrocytes were no different from those for control miRNA transfection. In scratch migration assays (c, representative photographs), let-7 transfection reduced the number of U251 cells that migrated over “wounds” compared with control miRNA transfection (d). *P < 0.05 and **P < 0.01 versus the control. ns, no significant difference
Migration, and invasion of normal tissue, are important hallmarks of glioblastoma cells [17]. In the scratch migration assay, let-7 transfection reduced cellular migration of U251 cells over scratch wounds compared with the control miRNA transfection (control miRNA = 100 ± 12%, let-7 = 35 ± 13%, P < 0.01) (Fig. 2c, d).
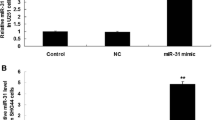
Let-7 miRNA attenuated in vivo tumor formation
U251 cells were transfected with control miRNA or let-7, and inoculated subcutaneously into nude mice. Tumors were evaluated 14 days after transplantation (Fig. 3a). Tumor weights produced by glioblastoma cells treated with let-7 were lighter that those produced by cells treated with control-miRNA (let-7 = 60 ± 44 mg, control miRNA = 233 ± 86 mg; *P < 0.05) (Fig. 3b), indicating that let-7 attenuated glioblastoma cell proliferation in vivo.
let-7 attenuated in-vivo tumor formation by glioblastoma cells. a U251 glioblastoma cells transfected with control miRNA or let-7 were inoculated subcutaneously into the flanks of nude mice, and tumors were evaluated 14 days later. b Tumors from let-7-transfected cells were lighter than those from control-miRNA transfected cells. *P < 0.05 compared with control
Discussion
In this study, we investigated the anti-tumorigenic effects of let-7 miRNA transfection in glioblastoma cells by quantifying cellular proliferation and migration. Our in-vitro and in-vivo results suggest that let-7 has anti-tumorigenic and anti-migratory effects on glioblastoma cells, and that these may be because of the reduced expressions of RAS.
Recent studies have revealed that miRNAs play key roles in the pathophysiology of glioblastoma [18]. In particular, miR-21 is aberrantly over-expressed in glioblastoma cells [19–21] and involves in migration, apoptosis, invasion, and growth of the cells [21–23]. miR-21 targets multiple components of p53, transforming growth factor-beta (TGF-beta), and mitochondrial apoptosis tumor-suppressive pathways [20], and promotes glioblastoma invasion by targeting matrix metalloproteinase regulators [23]. Thus, knockdown of miR-21 with antagomir increases glioblastoma apoptosis [19], and reduces migratory and invasion ability of the cells, suggesting therapeutic implications [23]. In addition, diagnostic and chemotherapeutic implications of miR-21 in glioblastoma have also been suggested [24, 25]. Accordingly, whether let-7 miRNA affects the expression of miR-21 is an interesting issue, and the mechanism of how let-7 miRNA inhibits glioblastoma cell proliferation should be investigated further considering the effect of other miRNAs, for example miR-21.
There have been reports of other miRNAs implicated in glioblastoma cells. miR-124 and miR-137 both induce differentiation of glioblastoma stem cells [26], and miR-128 inhibits the proliferation of glioblastoma cells by targeting Bmi-1 [27]. miR-146b inhibits migration and invasion of the cells by downregulating matrix metalloproteinases-16 [28]. miR-7 and miR-181 are downregulated in glioblastoma [29, 30], and miR-221/222 is overexpressed, which downregulates the p27(kip1) tumor suppressor [31]. Thus, various miRNA dysregulations are involved in the pathogenesis and cellular physiology of glioblastoma cells. In lung cancer, RAS is regulated by the let-7 miRNA family [4]. Therefore, our study implies that let-7 miRNA, which is known to suppress other cancer cells also, should be viewed as one of the miRNA candidates for controlling glioblastoma cell proliferation and tumorigenicity.
miRNAs regulate gene expression by translational repression and by degradation of target mRNAs, and a single miRNA can repress the production of hundreds of proteins [32]. Nevertheless, let-7 miRNA has been known to target Ras mRNA directly [4], and to repress the activation of downstream mitogen-activated protein kinase by reducing p-ERK [33]. In our study, let-7 transfection resulted in no change in hemoglobin concentration or in expression of vascular endothelial growth factor in the xenografted tumors (data not shown), suggesting that the anti-proliferative effect is more important than the anti-angiogenic effect after let-7 transfection. However, let-7 miRNA also affects multiple genes involved in the cell cycle and represses cell division directly and indirectly [34]. Accordingly, the anti-proliferative effect of let-7 is likely to be associated with multiple genes and pathways.
As shown by a previous microarray study [21, 35], let-7 expression is not downregulated in human glioblastoma tissues and cell lines. Accordingly, the transfection of let-7 miRNA does not correct a let-7 deficiency, and could result in overexpression of let-7. However, the innate down-regulation of let-7 miRNA in target tumors is not always required for let-7 delivery to achieve an anti-tumorigenic effect, as is shown by our results and those of others [36]. Low levels of let-7 or polymorphisms in 3′ untranslated region of K-RAS predict a poor outcome in various cancers [7, 37]. In addition, reduced expression of let-7 miRNA families is associated with low responsiveness to a number of chemotherapeutic agents [38]. Overexpression of let-7 miRNA creates a radiosensitive state of lung cancer cells [39]. Accordingly, variation of let-7 expression is likely to be associated with the prognosis or therapeutic responses of glioblastoma, which warrants further studies.
A small number of viral and non-viral delivery methods have been developed that may be suitable for delivery of miRNA to glioblastoma, and in particular, antagomirs have been used to target specific miRNAs in vivo [18]. As our results have shown, let-7 miRNA has different anti-proliferative effects on glioblastoma cells and astrocytes. However, the transfection of let-7 miRNA into human fibroblasts resulted in reduced cell numbers and increased G2/M cell cycle phases [40]. Thus, it is still important to deliver let-7 miRNA specifically to glioblastoma cells. We suggest that further studies should be conducted to devise a method of delivering let-7 to glioblastoma in vivo, and to design stable chemotherapeutic agents that mimic let-7 miRNA.
References
Voelzke WR, Petty WJ, Lesser GJ (2008) Targeting the epidermal growth factor receptor in high-grade astrocytomas. Curr Treat Options Oncol 9:23–31
Kim VN, Han J, Siomi MC (2009) Biogenesis of small RNAs in animals. Nat Rev Mol Cell Biol 10:126–139
Lu J, Getz G, Miska EA et al (2005) MicroRNA expression profiles classify human cancers. Nature 435:834–838
Johnson SM, Grosshans H, Shingara J et al (2005) RAS is regulated by the let-7 microRNA family. Cell 120:635–647
Mayr C, Hemann MT, Bartel DP (2007) Disrupting the pairing between let-7 and Hmga2 enhances oncogenic transformation. Science 315:1576–1579
Reinhart BJ, Slack FJ, Basson M et al (2000) The 21-nucleotide let-7 RNA regulates developmental timing in Caenorhabditis elegans. Nature 403:901–906
Takamizawa J, Konishi H, Yanagisawa K et al (2004) Reduced expression of the let-7 microRNAs in human lung cancers in association with shortened postoperative survival. Cancer Res 64:3753–3756
Akao Y, Nakagawa Y, Naoe T (2006) let-7 microRNA functions as a potential growth suppressor in human colon cancer cells. Biol Pharm Bull 29:903–906
Schultz J, Lorenz P, Gross G et al (2008) MicroRNA let-7b targets important cell cycle molecules in malignant melanoma cells and interferes with anchorage-independent growth. Cell Res 18:549–557
Yu F, Yao H, Zhu P et al (2007) let-7 regulates self renewal and tumorigenicity of breast cancer cells. Cell 131:1109–1123
Kumar MS, Erkeland SJ, Pester RE et al (2008) Suppression of non-small cell lung tumor development by the let-7 microRNA family. Proc Natl Acad Sci USA 105:3903–3908
Self AJ, Caron E, Paterson HF et al (2001) Analysis of R-Ras signalling pathways. J Cell Sci 114:1357–1366
Nakada M, Niska JA, Tran NL et al (2005) EphB2/R-Ras signaling regulates glioma cell adhesion, growth, and invasion. Am J Pathol 167:565–576
Perkins E, Calvert J, Lancon JA et al (2003) Inhibition of H-ras as a treatment for experimental brain C6 glioma. Brain Res Mol Brain Res 111:42–51
Goldberg L, Kloog Y (2006) A Ras inhibitor tilts the balance between Rac and Rho and blocks phosphatidylinositol 3-kinase-dependent glioblastoma cell migration. Cancer Res 66:11709–11717
Chu K, Jung KH, Kim SJ et al (2008) Transplantation of human neural stem cells protect against ischemia in a preventive mode via hypoxia-inducible factor-1alpha stabilization in the host brain. Brain Res 1207:182–192
Demuth T, Berens ME (2004) Molecular mechanisms of glioma cell migration and invasion. J Neurooncol 70:217–228
Lawler S, Chiocca EA (2009) Emerging functions of microRNAs in glioblastoma. J Neurooncol 92:297–306
Chan JA, Krichevsky AM, Kosik KS (2005) MicroRNA-21 is an antiapoptotic factor in human glioblastoma cells. Cancer Res 65:6029–6033
Papagiannakopoulos T, Shapiro A, Kosik KS (2008) MicroRNA-21 targets a network of key tumor-suppressive pathways in glioblastoma cells. Cancer Res 68:8164–8172
Ciafre SA, Galardi S, Mangiola A et al (2005) Extensive modulation of a set of microRNAs in primary glioblastoma. Biochem Biophys Res Commun 334:1351–1358
Krichebsky AM, Gabriely G (2009) miR-21: a small multi-faceted RNA. J Cell Mol Med 13:39–53
Gabriely G, Wurdinger T, Kesari S et al (2008) MicroRNA 21 promotes glioma invasion by targeting matrix metalloproteinase regulators. Mol Cell Biol 28:5369–5380
Conti A, Aguennouz M, La Torre D et al (2009) miR-21 and 221 upregulation and miR-181b downregulation in human grade II–IV astrocytic tumors. J Neurooncol 93:325–332
Li Y, Li W, Yang Y et al (2009) MicroRNA-21 targets LRRFIP1 and contributes to VM-26 resistance in glioblastoma multiforme. Brain Res 1286:13–18
Silber J, Lim DA, Petritsch C et al (2008) miR-124 and miR-137 inhibit proliferation of glioblastoma multiforme cells and induce differentiation of brain tumor stem cells. BMC Med 6:14
Godlewski J, Nowicki MO, Bronisz A et al (2008) Targeting of the Bmi-1 oncogene/stem cell renewal factor by microRNA-128 inhibits glioma proliferation and self-renewal. Cancer Res 68:9125–9130
Xia H, Qi Y, Ng SS et al (2009) microRNA-146b inhibits glioma cell migration and invasion by targeting MMPs. Brain Res 1269:158–165
Kefas B, Godlewski J, Comeau L et al (2008) microRNA-7 inhibits the epidermal growth factor receptor and the Akt pathway and is down-regulated in glioblastoma. Cancer Res 68:3566–3572
Shi L, Cheng Z, Zhang J et al (2008) hsa-mir-181a and hsa-mir-181b function as tumor suppressors in human glioma cells. Brain Res 1236:185–193
le Sage C, Nagel R, Egan DA et al (2007) Regulation of the p27(Kip1) tumor suppressor by miR-221 and miR-222 promotes cancer cell proliferation. EMBO J 26:3699–3708
Selbach M, Schwanhäusser B, Thierfelder N et al (2008) Widespread changes in protein synthesis induced by microRNAs. Nature 455:58–63
Ricarte-Filho JC, Fuziwara CS, Yamashita AS et al (2009) Effects of let-7 microRNA on cell growth and differentiation of papillary thyroid cancer. Transl Oncol 2:236–241
Johnson CD, Esquela-Kerscher A, Stefani G et al (2007) The let-7 microRNA represses cell proliferation pathways in human cells. Cancer Res 67:7713–7722
Zhou X, Ren Y, Moore L et al (2010) Downregulation of miR-21 inhibits EGFR pathway and suppresses the growth of human glioblastoma cells independent of PTEN status. Lab Invest 90:144–155
Sampson VB, Rong NH, Han J et al (2007) MicroRNA let-7a down-regulates MYC and reverts MYC-induced growth in Burkitt lymphoma cells. Cancer Res 67:9762–9770
Christensen BC, Moyer BJ, Avissar M et al (2009) A let-7 microRNA-binding site polymorphism in the KRAS 3′ UTR is associated with reduced survival in oral cancers. Carcinogenesis 30:1003–1007
Hummel R, Hussey DJ, Haier J et al (2010) MicroRNAs: predictors and modifiers of chemo- and radiotherapy in different tumour types. Eur J Cancer 46:298–311
Weidhaas JB, Babar I, Nallur SM et al (2007) MicroRNAs as potential agents to alter resistance to cytotoxic anticancer therapy. Cancer Res 67:11111–11116
Legesse-Miller A, Elemento O, Pfau SJ et al (2009) let-7 overexpression leads to an increased fraction of cells in G2/M, direct down-regulation of Cdc34, and stabilization of Wee1 kinase in primary fibroblasts. J Biol Chem 284:6605–6609
Acknowledgments
This work was supported by grants from the Korea Health 21 R&D Project, Ministry of Health & Welfare (A092058), WCU-Neurocytomics program (800-20080848), FPR08K1301-02210, and SNUH grant (620071079), South Korea.
Author information
Authors and Affiliations
Corresponding author
Additional information
S.-T. Lee and K. Chu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Lee, ST., Chu, K., Oh, HJ. et al. Let-7 microRNA inhibits the proliferation of human glioblastoma cells. J Neurooncol 102, 19–24 (2011). https://doi.org/10.1007/s11060-010-0286-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0286-6