Abstract
The movement to create guidelines for management of medical maladies has been gaining strength for quality, academic, financial and political purposes over the past two decades. This applies to neurological diseases, too. Evidence-based guidelines created in a multidisciplinary fashion using predetermined criteria for grading scientific data and translating this to similarly ranked recommendations is a valuable approach to meeting this goal. The following is a summary of the methods used for, and the results of, an evidence-based guideline for the management of newly diagnosed glioblastoma. In addition to outlining recommendations by discipline, it also addresses how concerns and conflicts were addressed in their development and provides comment on future directions in management of this situation that may improve outcome. It is important that clinicians directly experienced in patient management take the lead in creation of guidelines related to the diseases they deal with, as these clinicians are clearly the most suited to being able to arrive at a meaningful and useful product.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The advancement of guidelines as a manifestation of evidence-based medicine
Among the greatest satisfactions in the practice of medicine is identifying a difficult clinical question and then utilizing one’s own experience and that of colleagues to reach a successful answer. Commonly, however, personal or local experience may not provide all the answers. Fortunately, the modern practitioner of medicine has numerous other resources to turn to in such circumstances. Identifying the best methods for addressing a given clinical problem from the large number of literature resources currently available is challenging. For the most frequent problems, it is not feasible to look at all manuscripts written, and even if one could, ranking that information in terms of usefulness would be onerous. In response to this conundrum, various medical and governmental organizations have attempted to assist by creating or assisting in access to clinical practice guidelines that can facilitate the practitioner in choosing an effective therapeutic pathway [1, 2]. Ideally, this approach could lead to improvement and standardization in the quality of care for our patients.
Concerns about guidelines
Laudable as this may sound, the development of guidelines is fraught with pitfalls. Even though the authors of the documents may be well-meaning, the elaboration of guidelines can be heavily influenced by dogma, personal expertise and opinion and outright medical divas. Information from a recognized expert or consensus amongst experts in a specific field may provide interesting information and can certainly be based on scientific findings and principles, but does not necessarily yield a fair discussion of information outside of the expert’s usual pattern of practice. For example, the National Comprehensive Cancer Center Guidelines for Central Nervous System tumors have created recommendations that they define as having arisen from uniform consensus based on lower-level data including clinical experience with limited scientific foundation for the choices provided [3].
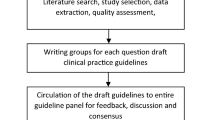
Having acknowledged the concerns regarding weaknesses of guidelines based on expert opinion and consensus conferences, one recognizes that the most systematic and valuable guidelines are those that apply the techniques referred to as “evidence-based medicine,” which Sackett has defined as “the integration of the best research evidence with clinical experience and patient values” [4]. From a practical standpoint, the elaborate development of evidence-based guidelines requires a well-recognized series of key steps. A thorough review of the scientific literature, utilizing appropriate and comprehensive search terminology, is necessary. This literature, or evidence, should then be weighted to reflect scientific validity utilizing an agreed upon system where empirical evidence takes precedence over expert judgment. In cases where evidence is weak, expert judgment is important in evaluating quality. To maximize the value of the guideline recommendations created, representative experts from each discipline to be impacted by the guidelines should participate in their formulation [5].
Guidelines are especially useful in diseases without cure, as they allow the setting of benchmarks from which research efforts can depart. Some physicians may argue that management recommendations from evidence-based guidelines are too simplistic or set the bar for too low in terms of therapy administered. The response to such criticism is that ranking of the data used to create evidence-based guidelines with uniformly predetermined eligibility and quality criteria can diminish bias in assessing the true quality of the published knowledge on the given question. As long as the managing physician questioning a particular guideline is satisfied with the clinical, scientific, or even social underpinnings of their treatment choices, then certainly their treatment choices may supersede the guidelines in a given situation.
Methods
Approach utilized for guideline development
The choice to proceed with development of this guideline was originated in the Joint Section for Tumors of the AANS and CNS. The purpose of this guideline development was to summarize a large amount of literature evidence regarding the management of newly diagnosed glioblastoma using a set of agreed upon quality parameters, as well as to set a benchmark from which improvement in this management can occur. The following is a summary of the process used to develop these guidelines.
It was deemed important that the development of this guideline be multidisciplinary. To provide proper specialty representation, five committees were designated: neuroradiology, neurosurgery, neuropathology, radiation oncology and neuro-oncology. Each committee was composed primarily of individuals with expertise in that discipline, with significant input and recommendations required from members of other committees so as to allow for a balanced assessment of the evidence. The respective committees were charged with development of one manuscript related to their area of expertise. Questions to be addressed were then formulated by each committee to cover concerns pertinent to each area when dealing with management of a newly diagnosed glioblastoma.
Literature search Strategy: The MEDLINE database of the National Library of Medicine was utilized as the primary source of the literature screened for the development of these guidelines. The Ovid interface was utilized to execute the initial searches for the time period between 1966 and the second week of May 2007. Searches were filtered to limit findings to those involving adults and newly diagnosed glioblastoma [6].
Classification of evidence related to diagnostic studies
Informative studies for the purpose of guidelines related to pathology and radiology diagnostic testing were defined as those that were prospective, were blinded between interpreters, had the interpretation of diagnosis compared to a gold standard and studied more than a handful of cases. A concerted effort was made to translate the evidence into recommendations appropriately and without bias. To accomplish this, a prospective classification scheme was used. Those cases designated as Class I data were required to have included an appropriate population of cases in terms of case number and tumor type. Additionally, they were to be blinded and provide data for calculation of sensitivity, specificity, positive and negative predictive values, accuracy, likelihood ratios for positive and negative results and κ. Once a κ value was calculated and the value was >0.6, a designation of Class I was made. For studies where the κ value was between 0.41 and 0.6, even though all other criteria were met, the data was designated as Class II. For those cases where κ was 0.4 or less, the data was designated as Class III. Studies were designated Class II if the study population was restricted, even if the work was done in blinded fashion and all parameters could be calculated. All other studies were designated Class III. Class III studies would include those that were retrospective, and where tumor grades and histologies were lumped together. Certainly studies such as these may be of value, but could not be interpreted as providing the same level of evidence as those that meet the criteria mentioned for Classes I and II [7–11].
Classification of evidence related to therapeutic studies
To assess the literature related to neurosurgery, radiation therapy and medical therapy data provided in the publications was separated into three classes. As above, a concerted effort was made to translate the evidence into recommendations appropriately and without bias. Evidence from well-designed observational comparative clinical studies, such as nonrandomized cohort studies, and case control studies was classified as Class II. Well-done prospective studies conducted in populations limited by age or other parameters, or which were very small in terms of numbers of subjects, also led to assignment of Class II to otherwise properly conducted prospective investigations. Evidence from case series and reports, comparative studies using only historical controls, expert opinion and significantly flawed randomized controlled studies was classified as Class III. Categorization as Class III information was not deemed to imply problematic or erroneous information [3]. Meta-analysis has been cited as an important method for analysis of clinical therapy data where it is difficult to reach statistically significant numbers of patients in single studies [12] and has been undertaken to provide insight into brain tumor therapies of various sorts [13, 14]. A review of this technique has brought to light the fact that individual patient data cannot be reclaimed and objectively assessed to resolve data inconsistencies and fill in data deficits such as specification of histology in relationship to treatment response [15]. The inability to separate glioblastoma from other histologies when looking at response is certainly the case in the studies collected for meta-analysis of brain tumor therapy and has resulted in the data from this work being relegated to lower impact classifications (i.e., Class III) for the purposes of these guidelines [13, 14].
Solving of reviewer conflict and evidence table construction
As would be expected, there was some disagreement amongst committee members about classification of the literature reviewed. These differences were resolved at face to face meetings or electronically with all committee members having copies of the literature in question to allow all members a chance for input. Any perceived conflict of interest or commitment was mitigated by recusing the individual(s) from input and review of whatever section was potentially problematic. Once classification of the data was agreed upon, evidence tables were created in reverse chronological order with the table headings consisting of first author’s name, journal and year, followed by a brief study description, chosen data class and conclusion. Each piece of literature cited in the table was discussed in greater detail regarding choice of classification in the scientific foundation section of each guideline.
Classification of recommendations
The recommendations created were then linked to the classification of the literature reviewed and listed in the evidence tables utilizing previously published and formalized techniques [9, 10, 16]. Class I evidence provided by the strongest clinical studies translated into Level I recommendations, indicating a high degree of clinical certainty. Class II evidence translated into Level II recommendations, indicating a moderate degree of clinical certainty. Class III evidence from less conclusive clinical study information translated into Level III recommendations, reflecting limited clinical certainty.
These guidelines were developed with an eye to the standard flow of clinical practice. Though simplistic, it was determined this method might improve readability and facilitate practitioner use of these guidelines, their ultimate purpose. Thus, as the initial step in identifying a glioblastoma is generally by imaging, a guideline was developed for this activity. Diagnosis is confirmed in almost all cases by some type of surgery, followed by pathology assessment of the tissue. Radiation and systemic chemotherapy are then provided. The following recommendations are provided in this manner with a brief comment on the literature used to support them. The comments below are extracted from the originally published guidelines and paraphrased in some cases to decrease the length of the presentation. However, substantive alterations would not be justified without reconvening each committee. The recommendations are italicized to set them apart from the subsequent scientific foundation.
Neuroradiology
Level I recommendation
Whenever possible, it is recommended that magnetic resonance imaging with the addition of gadolinium contrast enhancement be used, as it provides information that may allow differentiation of glioblastoma from other intrinsic tumors and secondary tumors.
In support of this recommendation is the Class I evidence provided by Dean et al. The authors examined the utility of MR imaging features in separating astrocytoma from anaplastic astrocytoma and glioblastoma by asking two blinded neuroradiologists to score each of the features on a 0–2 scale. They concluded that imaging review provides a valuable adjunct to clinical and neuropathology assessments. The report provides the histological diagnosis and the results of the blinded interpretation for each case. This allows calculation of standard predictive parameters and a κ value of 0.72 when looking at glioblastoma, suggesting MRI is good for differentiating this tumor from other diagnoses. It should be noted that infratentorial lesions are not addressed in this publication. The authors emphasized that even neuropathology interpretation is subject to variation due to sampling variability occurring at the time of surgery [17].
Level II recommendation
Computerized tomography with the addition of contrast material may provide data allowing differentiation of glioblastoma from other intrinsic tumors and secondary tumors.
Amundsen et al. described a prospective and blinded assessment of CT with and without contrast in the diagnosis of 46 brain tumors, 15 of which were glioblastoma. Thirteen of these were diagnosed correctly by imaging without knowledge of histology. All standard predictive parameters could be calculated, yielding a κ value of 0.80 for glioblastoma. However, the small number of glioblastoma cases diminishes the impact of this work, yielding a designation of Class II data [18].
Level III recommendations
The addition of proton magnetic resonance spectroscopy to standard anatomic magnetic resonance imaging provides details that may improve diagnostic accuracy for lesions of the brain, including brain tumors.
Proton magnetic resonance spectroscopy has been highly valued in differentiating neoplastic from non-neoplastic abnormalities of the brain. However, data from spectroscopy of tumor tissue alone has been cited by Howe et al. as not completely definitive due to tumor heterogeneity. In that study, average values for lactate and for ratios of myoinositol/choline and creatine/choline were different for gliomas, as histologic grade is elevated, but not to a statistically significant extent that would allow reliable differentiation between grades of astrocytoma. Earlier studies with the same in vitro technique specifically pointed out the inability to separate anaplastic astrocytoma from astrocytoma or glioblastoma [19]. In studies designed to assess MR imaging as a method of noninvasive grading, no differentiation between high grade gliomas could be obtained [20]. Calculations of a variety of measurable quantities and ratios have been studied using proton magnetic resonance spectroscopy. However, even quantification of choline/creatine ratios is not specific enough to reliably separate histologic grade, or even tumor types [21]. Thus, the data used in this guideline leaves proton magnetic resonance spectroscopy as a supplementary study unable to stand as a meaningful surrogate for histology [22].
In support of the supplementary nature of proton magnetic resonance spectroscopy, Moller-Hartmann et al. looked at this modality as an adjunct to standard MR imaging. A wide variety of histologies were reviewed in 176 consecutive cases, of which 164 were technically satisfactory. In this series were 23 astrocytomas, 28 anaplastic astrocytomas, and 39 glioblastomas. Choline/creatine ratios, N-acetyl aspartate/creatine ratios and the percentage of signal intensities of choline, creatine and N-acetyl aspartate were measured. These parameters were not assessed as independent predictors of histologies, but each showed some degree of correlation with tumor grade. The authors concluded that, taken together, this data assisted the interpreter of the standard images in providing a correct diagnosis. The authors calculated that the rate of correct diagnoses is raised by 15.4% and the number of incorrect diagnoses is decreased by 6.2% by the addition of MRS to MRI [23]. On the other hand, no claim was made that it in any way would replace histological evaluation of intracranial pathology.
Utilization of perfusion magnetic resonance imaging with determination of mean regional blood volume may provide data that assist in separating the histological characteristics of intrinsic tumors from one another.
Lee et al. report on the utility of the measurement of regional cerebral blood volume (rCBV). They looked at 24 patients retrospectively. Each had MR imaging initially and then histological confirmation. Regions of interest in the tumor and in normal white matter were chosen and a ratio between maximum tumor rCBV and the rCBV of contralateral normal white matter calculated. A significant difference (P < 0.05) between the values for each tumor type (astrocytomas, anaplastic gliomas and glioblastoma) was observed. These evaluations were retrospective and not blinded. There is a need for a more detailed assessment of this technique in order to validate it as a potential noninvasive diagnostic method [24]. In a later study, a smaller group of patients were analyzed, showing the potential value of the technique, but the necessary step of differentiating anaplastic gliomas from glioblastomas or astrocytomas was not taken [25].
Roberts et al. studied dynamic contrast enhanced magnetic resonance imaging prior to surgery in a series of 38 individuals. They calculated the tumor fractional blood volume and permeability in each case and then compared these to the tumor histology. There was a correlation between fractional blood volume and increasing the grade of tumor from II to IV. However, when comparing mean values per histologic subtype, differences were not significant. On the other hand, a greater degree of correlation could be identified with the permeability measurement and the differences between each histology, which were clearly statistically significant (P < 0.001 for each comparison) [26]. A prospective, blinded analysis of this technique is warranted to determine if these parameters might be able to stand alone in predicting histology.
Neurosurgery
Level I recommendation
There is insufficient evidence to support a level I recommendation
The neurosurgical literature remains unclear as to whether the extent of surgical resection statistically correlates with survival. The fact that such a fundamental question among surgeons remains unanswered for well over one-hundred years of glioma surgery is remarkable. A number of authors have attempted to identify the reasons behind the ongoing controversy [27–29]. Some of the issues described include: differing classification criteria, differing distributions of co-variants, patient selection bias and numerous methodological inconsistencies. The majority of studies available for review are retrospective and subject to design variation and bias. The prospective data available to address the benefit of cytoreductive surgery has generally been poorly designed.
No prospective randomized clinical trials specifically addressing extent of resection in the initial management of adult patients with newly diagnosed suspected malignant glioma in the general adult population were identified.
Level II recommendation
Based on the prospective data available and a general consensus in the retrospective data, it is recommended for newly diagnosed supratentorial malignant glioma in adults that the “maximal safe resection” be undertaken (i.e., the maximal cytoreductive procedure provided that postoperative neurological deficit can be minimized).
Thirty papers (ten prospective and 20 retrospective studies) ultimately qualified for inclusion in the evidence table of this portion of the guideline. These include ten prospective studies and twenty retrospective studies. Five of the prospective studies provided Class II data and one of the twenty retrospective studies provided Class II data [29–34]. All but one of the papers providing Class II data supported extent of resection as a factor in improving survival in newly diagnosed adult patients with malignant glioma. The study of Levin et al. published in 1985 failed to support extent of resection for glioblastoma, but did demonstrate a survival advantage in cases of anaplastic astrocytoma.
Vuorinen et al. reported a small randomized study specifically focusing on patients older than 65 [29]. In this study, 30 patients with radiographically suspected newly diagnosed malignant glioma were randomized to either stereotactic biopsy or resection. Only twenty-three patients were ultimately diagnosed with a malignant glioma (19 glioblastomas and four anaplastic astrocytomas). The other seven (23%) had a variety of diagnoses (three stroke, two metastasis, one lymphoma). The randomization resulted in assignment to stereotactic biopsy (n = 13) or resection (n = 10) followed by radiotherapy. Overall median survival was 4.86 months. Median survival following craniotomy was 5.7 months versus 2.83 months following biopsy alone (P = 0.035). There was no significant difference in the time of deterioration between these two treatments (P = 0.057) and radiotherapy had a significant effect on survival (P = 0.001). The authors concluded that in this population survival time was improved by craniotomy and resection of tumor. Despite the randomized design, the small sample size and inclusion of only patients over 65 limit extrapolation of the results to the general population of glioblastoma patients, thus yielding Class II data.
Stummer et al. reported a randomized study assessing the effect of fluorescence-guidance on extent of resection, progression-free survival, overall survival and morbidity [30]. Three-hundred and twenty-two adult patients with radiographically suspected malignant glioma were randomly assigned to either 5-aminolevulinic acid for fluorescence-guided resection (n = 161) or to conventional microsurgery with white light (n = 161). The primary endpoints were the number of patients without contrast-enhancing tumor on early MRI (i.e., that obtained within 72 h after surgery) and 6 month progression-free survival as assessed by MRI. Secondary endpoints were volume of residual tumor on postoperative MRI, overall survival, neurological deficit, and toxic effects.
The authors published an interim analysis of 270 patients in the full-analysis population (139 assigned 5-aminolevulinic acid, 131 assigned white light), excluding patients with ineligible histological and radiological findings as assessed by blinded central reviewers. The study was terminated following the interim analysis due to the effectiveness of the therapy. Median follow-up was 35.4 months (95% CI 1.0–56.7) and there were no significant difference in the number of adverse events between the groups.
The use of fluorescence-guidance resulted in a 65% rate of complete resection (90 of 139 patients with no contrast on early postoperative imaging). The control group had a 36% (47 of 131) chance of complete resection (P < 0.0001). The fluorescence-guidance group also had a higher 6 month progression free survival (41% vs. 21%, P = 0.0003).
The authors concluded that the use of fluorescence-guided resection using 5-aminolevulinic acid resulted in an increase in the number of complete resections of contrast-enhancing tumor, which was associated with a significant improvement in progression-free survival. Although this paper provides Level I evidence evaluating the use of the authors’ fluorescence-guided surgical technique, patients were not assigned to groups to undergo a predetermined extent of resection. Level II evidence is provided because similar cohorts are studied prospectively and the impact of extent of resection on survival is significant.
The influence of extent of surgery, tumor size and site were the subject of a study published by Simpson et al. combining the data from three large Radiation Therapy Oncology Group (RTOG) prospective randomized trials [31]. Although the data was collected in randomized prospective fashion, it was not randomized to directly assess the extent of resection but rather the role of combined radiation and chemotherapy following surgical resection or biopsy for glioblastoma and thus yielded Class II data. Six hundred and forty-five patients with a diagnosis of glioblastoma on central pathologic review were included and analyzed for survival with respect to potential prognostic factors in multivariate fashion including age, Karnofsky Performance Status (KPS), extent of resection, size of tumor and location. One-hundred and twenty-five patients had a gross total resection (19%), 413 had a subtotal resection (64%) and 107 had biopsy only (17%). Patients undergoing either total resection (11.3 months) or partial resection (10.4 months) had a significantly prolonged median survival when compared to the biopsy group (6.6 months, P < 0.0001, P < 0.001). Patients with frontal lobe tumors survived longer than temporal or parietal tumors. Multivariate analysis confirmed significant correlation with age, KPS, extent of surgery and primary site with survival. The best survival rates occurred in patients who had at least one of the following features: age less than 40 years, high KPS, frontal location and having undergone a total resection. This group had a median survival of 17 months.
Thirty-one patients operated on for supratentorial glioblastoma or anaplastic astrocytoma were prospectively studied to evaluate the extent of resection on the length and quality of survival [32]. Twenty-one patients (68%) had glioblastoma and 10 patients (32%) had anaplastic astrocytoma. Early postoperative enhanced computed tomography was used to determine the extent of tumor resection. Gross total resection was accomplished in 19 patients (61%) and subtotal resection was performed in 12 patients (39%). The gross total resection group lived longer than the subtotal resection group (median survival of 90 vs. 43 weeks, P < 0.001). Postoperatively the KPS was significantly increased in the gross total resection group (P = 0.006), but not in the subtotal resection group (P > 0.05). The gross total resection group spent significantly more time after the operation in an independent status compared to the subtotal resection group. The authors conclude that gross total resection of supratentorial glioblastomas and anaplastic astrocytomas is feasible and is directly associated with longer and better quality survival when compared to subtotal resection. Distribution of pathology appeared to be biased, with 37% of gross total resection group being anaplastic astrocytoma versus only 25% being anaplastic astrocytoma in the subtotal resection group. This may have led to outcomes being better in the gross total resection group. This flaw, along with the small number of glioblastomas in the study, resulted in categorization of this study as Class II.
A randomized study conducted to compare two chemotherapy regimens (PCV vs. BCNU) in malignant glioma patients treated with surgery and radiation was reported by Levin et al. [33]. The study group consisted of 76 patients with glioblastoma and 72 patients with anaplastic astrocytoma. The study, while designed as a Class I study for chemotherapy, provides prospective data on extent of resection, as this was studied as a co-variable. In multivariate analysis, age was determined to be the most important predictor of survival in both glioblastoma and anaplastic astrocytoma patients. Extent of resection was a significant predictor of survival in the patients with anaplastic astrocytoma, but did not achieve significance in the glioblastoma patients. This yielded Class II data because, despite the randomized data, extent of resection was not a factor for randomization.
In 1996, Kiwit et al. published their analysis of prognostic factors for survival in malignant glioma [34]. Initially, a 274 patient retrospective review was performed, including a matched pair analysis of 40 biopsy and 40 resective surgery patients. The authors demonstrated a significant effect of cytoreductive surgery over biopsy only favoring survival, comparing 42 weeks with 26 weeks (P < 0.05). The authors also found no significant improvement in KPS in the cytoreductive surgery group. Postoperative tumor volume significantly correlated with increased survival and the authors favor maximal debulking while minimizing neurological deficit. The design of the retrospective cohort study warranted Class II status.
Level III recommendation
It is recommended that biopsy, partial resection or gross total resection all be considered in the initial management of malignant glioma, depending on the condition of the patient, the size and the location of the malignant glial tumor.
Fourteen of the 19 papers meeting screening criteria for review were categorized as Class III and provided data that supported the concept of cytoreductive surgery in the initial management of malignant glioma. As a result, it follows that the majority of the reviewed data warranting inclusion in this guideline supports maximal cytoreductive surgery. The Class III data suggests that clearly room must be left for clinical judgment in this decision making as is implied by the Level III recommendation provided here.
Neuropathology
Level I recommendation
The diagnosis of malignant glioma should be based on the histopathology review of tissue
Pathologic diagnosis of malignant gliomas depends in large part upon the informed application of established histopathologic and cytopathologic criteria to sampled tissue [35–38]. It relies heavily, and in many instances exclusively, on examination of hematoxylin and eosin (H&E) stained slides from the sampled lesion. Technique and criteria for assessment are heavily dependent on tumor sampling error. An outcome-based classification scheme can be found in the St. Anne/Mayo system, which followed from an investigation of prognostic features, grading criteria and reproducibility in a set of 287 patients at the Mayo Clinic with infiltrative astrocytomas [36, 39]. This investigation studied four histologic criteria within astrocytic neoplasms as they related to patient survival, including nuclear atypia, mitoses, endothelial proliferation and necrosis. Grade 1 was defined as zero features present; grade 2 with one feature; grade 3 with two features, and grade 4 with three or four features. Based on a 15 year follow-up period, a multivariate statistical analysis found that each of the four histologic criteria, as well as the tumor grade derived from them, was strongly correlated with survival (P < 0.0001). Importantly, these methods of histologic grading showed a concordance of 94% between two double blinded observers. The recent World Health Organization classification is a multi-authored text written by international experts, which uses a grading system largely based on the St. Anne/Mayo criteria [36]. There has been no direct comparison of the most recent WHO criteria to other classification systems in terms of reliability or prognostic accuracy. However, the related St. Anne/Mayo criteria have been investigated for predictive value in a comparison to the older Kernohan criteria [40]. In a series of 273 patients with gliomas, histologic grading was performed according to the Kernohan and St. Anne/Mayo criteria and the resulting grades were compared with patient survivals. Specific pathologic features from each grading scheme were examined for their predictive value. In both classification systems, histologic grade was significantly correlated with survival (Cox analysis, P < 0.0001). This included three grades for the Kernohan classification and four grades for the St. Anne/Mayo classification. Mitosis (P < 0.0001, χ 2 = 17.9), endothelial proliferation (P < 0.0001, χ 2 = 39.4) and necrosis (P = 0.0007, χ 2 = 11.5) were all significantly correlated with survival. As noted below, these features form the basis of grading the infiltrative astrocytomas using WHO criteria. Thus, the WHO classification, which incorporates the criteria of the St.Anne/Mayo criteria, can be recommended as a recent and updated international standard for classifying and grading of malignant gliomas.
Level II recommendation
Frozen section and cytopathologic evaluation are recommended for the intra-operative diagnosis of malignant glioma.
The role of a frozen section diagnosis is to guide the neurosurgeon at the time of the operation, to ensure that diagnostic tissue has been obtained and to give the most accurate intra-operative diagnostic interpretation, acknowledging limitations of sampling and of the technique. Limitations must be recognized, as frozen sections are not an optimal technique for detecting the histologic features of an infiltrating glioma, especially those that distinguish oligodendrogliomas from astrocytomas [41]. In particular, the features of oligodendrogliomas, such as perinuclear halos, delicate chromatin pattern and nuclear regularity, are not as evident in frozen tissue. Definitive classification and grading of glial neoplasms is most accurate following examination of all tissue submitted for permanent sections, as tissue examined at frozen section may not represent the entire disease process. Nonetheless, a general degree of histologic differentiation (well-, moderately, or poorly differentiated) or histologic grade can usually be derived to a degree useful for intraoperative management by assessing the frozen sections cellular density, nuclear anaplasia, mitotic activity, microvascular hyperplasia or necrosis [42].
Cytologic preparations performed on biopsy material at the time of surgery appear to increase the diagnostic accuracy when used together with frozen sections. Martinez et al. reviewed the intra-operative materials on 100 neurosurgical biopsies and established a diagnosis based examination of 1) cytologic material alone; 2) frozen section material alone and 3) both preparations together [43]. These diagnoses were then compared with the final permanent section diagnosis. The correct intraoperative diagnosis, based on the combination of frozen section and cytopathologic exam, was given in 95% of cases, whereas the diagnosis based on frozen sections alone led to an agreement with the final diagnosis in 88%. A diagnosis based on cytologic examination alone resulted in the correct diagnosis in 76%. This study concluded that the frozen section diagnosis is superior to cytologic diagnosis at the time of operation, but that the highest diagnostic accuracy is achieved when the techniques are used together.
Reyes et al. 1991 performed a comparison of two types of cytologic preparations––imprints and smear preparations––as well as frozen sections, and compared the diagnoses established with these techniques to the diagnosis established on permanent section diagnosis. A series of 150 brain and spinal cord lesions suspected to be brain tumors were evaluated [44]. Among adequate preparations, agreement with the final permanent section diagnosis was 99% for frozen sections. Among the cytologic preparations, the correct diagnosis was achieved on 82% of imprints, and on 92% of smears. Thus, frozen section was more accurate than both cytologic preparations for intraoperative diagnosis, while smear preps were superior to imprints.
Brainard et al. addressed the issue of frozen section diagnostic yield and its improvement by increasing the number of samples obtained in the challenging circumstance of stereotactic brain biopsies. A series of 188 stereotactic brain biopsies was studied [45] and the cumulative diagnostic accuracy of each consecutive frozen section was compared to the permanent section diagnosis. The first frozen section sent to the neuropathologist was diagnostic in 73% of neoplastic cases; for non-neoplastic conditions, the first frozen section was diagnostic in 50% of cases. With the submission of one additional frozen section, diagnostic yield was 89% for neoplastic cases and 65% for neon-neoplastic cases. For all of the non-neoplastic and neoplastic cases combined, it was found that the diagnostic yield increased from 67% to 89% when the number of biopsies increased from one to four.
The accuracy of cytologic examination alone for establishing a diagnosis of central nervous system tumors has varied. In one comprehensive study, Gaudin et al. analyzed the diagnostic accuracy of a combination of cytopathologic and histopathologic techniques in a series of 74 patients undergoing stereotactic biopsy [46]. Included in this study was a comparison of the crush prep technique with the permanent section diagnosis based on evaluation of the tissue block. Diagnosis based on evaluation of crush preps during the procedure was highly correlated with the final diagnosis following evaluation of the tissue block (76% concordance). The concordance for the diagnosis of glioblastoma was 56% and for AA was 100%. In the cases of glioblastoma that could not be diagnosed at the time of the procedure on cytologic studies, there was insufficient evidence of necrosis to establish the diagnosis. For those cases diagnosed as glioblastoma, the sensitivity and specificity of the cytological technique was 0.54 and 1.0 respectively. For cases of anaplastic astrocytoma, the sensitivity was 0.81 and the specificity was 1.0. In a multivariate survival analysis, three factors correlated with decreased survival: age greater than 55 (P < 0.001, hazard ratio 3.58 (CI = 1.95, 6.57)), nuclear atypia (P = 0.004, hazard ratio 4.30 (CI = 1.61, 11.46)) and necrosis (P = 0.016, hazard ratio 2.14 (CI = 1.15, 3.97)). Thus, a high correlation between the cytologic diagnosis and final diagnosis was reported using these preparations and the presence of nuclear atypia and necrosis were found to be correlated with shorter survival.
Taken together, the evidence suggests that a frozen section diagnosis is an accurate means for establishing an intraoperative diagnosis and correlates with the final diagnosis in greater than 85% of cases. The diagnostic accuracy improves with increased numbers of biopsies and also improves with the use of cytopathologic preparations, such as crush, smear preps and imprint preps.
Consultation from a neuropathologist specialized in brain tumor diagnosis is recommended for problematic cases.
Numerous studies of inter-observer and intra-observer concordance have confirmed that histopathologic methods lack a high degree of reproducibility for distinguishing between oligodendroglial and astrocytic tumors and for grading of primary glial neoplasms. A study by Prayson et al. compared the consistency in grading astrocytomas by five neuropathologists to that of five general surgical pathologists [47]. Thirty neoplastic and non-neoplastic lesions were sent to the study participants and each was asked to place the lesion into one of three histologic grades (grading criteria were given to the participants). Agreement on the diagnoses among the neuropathologists was complete (five of five in agreement) in 12 of 30 cases (40%). Four of the five neuropathologists agreed in 26 of 30 cases (87%). In contrast, among the surgical pathologists, there were only six cases (20%) for which all five agreed and only 13 cases (43%) for which four of the five agreed. The kappa value for inter-observer concordance among the neuropathologists was higher than that for the surgical pathologists (kappa = 0.63 vs. 0.36). The kappa value for agreement on the diagnosis of glioblastoma was 0.81 for the neuropathologists versus 0.63 for the surgical pathologists. For the diagnosis of anaplastic astrocytoma, the kappa values were 0.88 versus 0.55, respectively. The authors concluded that training in neuropathology and experience in the diagnosis of grading gliomas are important for reliable diagnosis.
Level III recommendations
Incorporation of clinical and radiographic information with the final pathologic diagnosis is recommended.
The criteria of the WHO classification of brain tumors are internationally recognized and can be utilized for establishing the diagnosis of malignant gliomas.
A diagnosis should be established in a multidisciplinary setting with knowledge of clinical information, neurosurgical impression, and radiologic findings. Morphologic criteria for classifying and grading gliomas can be found in the WHO Classification of nervous system tumors.
Proliferation studies, such as those based on Ki-67/MIB-1 staining, and molecular genetic studies are recommended as adjuvant studies for classification and prognostication of malignant gliomas.
Multiple correlative laboratory studies can be obtained to assist in tumor tissue assessment. The most commonly used adjuvant analyses are studies of tumor cell proliferation. A variety of techniques have been utilized to assess cell proliferation in gliomas, including tritiated thymidine/bromodeoxyuridine, histone mRNA in situ hybridization, flow cytometry, DNA polymerase alpha, topoisomerase II-alpha, p105, PCNA and Ki-67/MIB-1 [48]. The most reliable and technically feasible method for most pathology laboratories is the Ki-67/MIB-1 antibody. This antibody identifies an antigen present in the nuclei of cells in the G1, S, G2 and M phases of the cell cycle, but is not expressed in the resting phase, G0. The results are usually expressed as a percentage of positive staining tumor cell nuclei.
Importantly, the Ki67/MIB-1 labeling index is not a component of the WHO grading scheme for glial neoplasms, nor is it considered in any other recent grading systems [35–37, 39]. However, many investigations have demonstrated a significant positive correlation between Ki-67/MIB-1 indices and histologic grade and have shown that higher Ki-67/MIB-1 proliferation indices are associated with shorter survivals. In one of the first comparative analyses of proliferation markers in astrocytic neoplasms, McKeever et al. investigated MIB-1, BrdU and PCNA, as they related to survival in 65 astrocytomas (36 grade IV, 15 grade III, and 14 grade II) [49]. The MIB-1 proliferation index was found to be more predictive of survival (log rank P = 0.06) than either Brdu or PCNA. In univariate analysis, a low MIB-1 proliferation rate (<2.5%) was associated with a longer survival (P = 0.056). On Cox multivariate analysis, histological grade, age and KPS were all associated with survival (P < 0.05), but MIB-1 proliferation was not. The authors concluded that MIB-1 is the most predictive proliferation marker and is helpful in cases where clinical or histopathology factors are ambiguous.
As part of a larger study of proliferation and prognosis, Giannini et al. studied the MIB-1 index as an independent prognostic factor in 140 diffuse astrocytomas, including 45 grade II, 50 grade III and 45 grade IV [50]. MIB-1 indices were higher in grade III than in grade II (P = 0.001) and were higher in IV than in grade III (P = 0.014). On a multivariate analysis that included tumors of all grades (grades II, III, and IV), this study found that necrosis, age and mitotic index were independent markers of survival (P < 0.05). MIB-1 proliferation was not an independent marker of prognosis when grade IV tumors were included in the analysis, mostly because the presence of necrosis was such a statistically powerful predictive marker. Among grade II and III astrocytomas, MIB-1 index was highly correlated with survival on multivariate analysis (P < 0.05). The authors concluded that MIB-1 proliferation provides clinically useful information in the categories of grade II and III astrocytomas.
The prognostic utility of MIB-1 indices among the malignant gliomas (i.e., grades III and IV) has been debated. Wakimoto et al. evaluated the MIB-1 labeling index as an independent prognostic marker in 72 supratentorial astrocytomas, including 19 grade II, 25 grade III and 28 grade IV tumors [51]. Proliferation indices in this study correlated with tumor grade: MIB-1 indices were higher in grade IV than in grade III tumors and were higher in grade III than in grade II tumors (P < 0.001). Multivariate analysis of factors associated with survival demonstrated that histologic grade, MIB-1 index and KPS before and after treatment were independent statistically significant prognostic factors (P < 0.05). When the analysis was performed only on the high grade tumors (grades III and IV), the MIB-1 index, KPS score after treatment and location (superficial vs. deep) were the only prognostically significant factors (P < 0.05). Thus, this study suggested that MIB-1 studies provide useful prognostic data for high grade gliomas.
A different conclusion was reached in a recent retrospective analysis of MIB-1 proliferation as an independent prognostic marker in a series of 116 glioblastoma patients [52]. Importantly, this study included only newly diagnosed tumors and only grade IV histology (glioblastoma). The mean MIB-1 index was 12.5% and varied from 0 to 76.4%. MIB-1 proliferation was not associated with survival on either univariate analysis or multivariate analysis. Similar to other studies, the multivariate analysis demonstrated that patient age, performance status and extent of resection were each independent markers of survival (P < 0.05). Thus, when tumor histology is restricted to GBM, the MIB-1 proliferation index does not have much utility.
The determination of a labeling index is not warranted as a routine part of the evaluation of all gliomas, due to limitations associated with tumor heterogeneity and sampling, as well as differences in staining methodology, index determination, and the degree of inter-observer variability. It may be prognostically helpful, however, in histological borderline cases, such as those that are at the grade II–III and III–IV border. A high labeling index in this setting may indicate a more aggressive neoplasm; a low index is more equivocal due to issues related to sampling and tumor heterogeneity.
In addition to studies of cell proliferation, other molecular studies are utilized, often for treatment specific reasons, though some have been reported to assist in determination of prognosis. For malignant gliomas, the specific genetic alterations that have been most thoroughly documented include PTEN and TP53 mutations, MDM2 and EGFR amplification, p14 ARF and p16(CDKN2A) deletion, and 1p/19q deletions [36, 37, 53, 54]. Some genetic alterations have been used in the diagnostic setting, either to provide assistance with pathologic classification or to provide independent prognostic information [55]. Each technique for genetic testing has its own set of advantages and disadvantages. Most often employed are loss of heterozygosity (LOH, either traditional gel-based assays or capillary electrophoresis), fluorescence in situ hybridization (FISH) and comparative genomic hybridization (CGH) [56–58]. These tests demonstrate good to excellent concordance (73–99%) and the choice depends largely on the preferences of the pathologist, department, and institution. LOH analysis and FISH have the highest concordance (>93%) and are utilized most frequently for diagnostic purposes on tissue derived from histologic sections [59]. FISH has some advantages from a pathologist’s perspective: 1) analysis is based on the morphologic identification of genetic alterations within tumor cell nuclei; 2) non-neoplastic cells (positive controls) are almost always present within the tissue sections examined (i.e. normal endothelial cells, neurons, etc.); 3) FISH does not require microdissection of normal and tumor before analysis, and 4) genetic gains and losses in infiltrative tumors with a low ratio of neoplastic/normal cells can be analyzed by FISH, whereas these alterations may not be detected by PCR-based analysis (LOH studies) due to overwhelming amounts of normal DNA. One major disadvantage of FISH is that it can be highly labor intensive and automation has not yet reached all of its applications.
One of the best studied relationships between genetic alterations and glioma histology is the strong association of allelic losses on chromosomes 1p and 19q and the oligodendroglioma phenotype [60]. Reifenberger, et al. was the first to observe that a high percentage of oligodendroglial tumors contained the specific combination of allelic losses on chromosomes 1p and 19q [61]. This group studied the genetic status at 180 polymorphic loci located throughout the human genome by restriction length polymorphism analysis on eight oligodendrogliomas, 13 anaplastic oligodendrogliomas, eight oligoastrocytomas, and eight anaplastic oligoastrocytomas. Among the pure oligodendrogliomas (not the mixed tumors), they found 19q losses in 81%, which was the most frequent genetic alteration among these neoplasms. In those tumors with 19q loss, 75% also had 1p loss. Subsequent studies by other groups have confirmed that between 60–80% of oligodendroglial neoplasms demonstrate combined 1p and 19q losses [57]. Others have suggested that the morphologically pure, or classic, forms of oligodendrogliomas have even higher frequencies of combined 1p/19q loss [62, 63]. On the other hand, gliomas with different or accompanying genetic alterations, such as 10q loss, TP53 mutation, and 9p(p16/CDKN2A) losses, have less classic oligodendroglial features [64, 65].
Enthusiasm for defining genetic subsets of oligodendrogliomas increased substantially with the demonstration of prognostically distinct groups. Cairncross et al. were the first to show that anaplastic oligodendrogliomas with losses of chromosome 1p and 19q were associated with enhanced response to chemotherapy (PCV procarbazine, CCNU vincristine) and prolonged survival. In this study, 39 anaplastic oligodendrogliomas were characterized by LOH analysis for 1p and 19q status and for CDKN2A(p16) gene deletion, and for TP53 mutations by sequence analysis. The molecular findings were compared to response to PCV therapy and survival. Sixty-five percent of anaplastic oligodendrogliomas in this study demonstrated combined loss of 1p and 19q and this genetic finding was associated with both chemoresponsiveness (P < 0.01) and longer survival (P < 0.001) on univariate analysis and with improved survival on multivariate modeling (P = 0.05). In contrast, those anaplastic oligodendrogliomas with p16(CDKN2A) homozygous deletions (21%) had shorter survivals on univariate (P = 0.0009) and multivariate (P < 0.05) analysis. These molecular subsets were not distinguishable morphologically and had little genetic overlap (i.e. tumors with 1p and 19 q losses did not contain p16(CDKN2A) deletions (P = 0.048)). Subsequent studies of therapeutic response in oligodendrogliomas have demonstrated that those tumors with 1p/19q losses are associated with improved responses to other chemotherapies, including temozolomide, and to radiation therapy [66, 67]. It remains unsettled if 1p/19q co-deletion is a marker of therapeutic response or a more general marker of favorable prognosis, independent of therapy.
From these investigations, it remained unclear if survival differences among oligodendrogliomas with 1p/19q losses were due to the genetic alterations themselves, the oligodendroglial phenotype, or their combination. Interest remained as to whether other histologic types of infiltrating gliomas with 1p and 19q losses, such as glioblastomas, could have favorable outcomes as well. Smith et al. addressed this question by assessing 1p and 19q status as it related to survival for 162 patients with diffuse gliomas, including 52 oligodendrogliomas, 79 astrocytomas and 31 mixed oligoastrocytomas [56]. 116 of these patients had malignant gliomas (72%). Combined loss of 1p and 19q was found to be predictive of prolonged overall survival for patients with oligodendrogliomas on univariate analysis (P = 0.03). After adjusting for age and tumor grade, 1p and 19q loss were associated with survival on multivariate analysis (P < 0.01). However, combined 1p and 19q losses were uncommon in tumors with astrocytic morphology (8%) and were not predictive of prolonged survival. Neither were such losses prognostically significant for mixed oligoastrocytomas of any grade. Other investigations have also provided evidence that 1p/19 losses in astrocytic neoplasms are extremely rare and not prognostically significant [57, 68].
In contrast, Schmidt et al. reached a different conclusion about the prognostic significance of 1p/19q loss in glioblastomas [69]. His investigation of 97 patients with glioblastoma assessed the prognostic significance of genetic alterations, including 1p and 19q loss. This study included 87 primary glioblastomas, six glioblastomas that had progressed from a lower grade and four giant cell glioblastomas. Similar to other studies, approximately 30% of glioblastomas demonstrated LOH at 19q and 19% at 1p. The combination of 1p and 19q loss occurred in only five of the 97 glioblastomas. However, the mean survival of these five patients was 22.2 months, much longer than patients whose tumors retained 1p, 19q, or both (9.0 months) (P = 0.053). The authors concluded that the frequency of 1p and 19q losses was much lower in glioblastomas than oligodendroglial tumors, but that these alterations could have prognostic significance. Despite the findings of this study, the cumulative evidence suggests that combined loss of 1p/19q is best viewed as a marker of oligodendroglial differentiation as well as a finding associated with a favorable prognosis in these tumors. Additional studies will be needed to demonstrate the clinical utility, if any, for 1p/19q testing in other primary brain tumors.
Amplifications of the EGFR gene occur in approximately 40% of glioblastomas and 10% of anaplastic astrocytomas and can be detected by FISH, CGH, or PCR-based tests [36, 70, 71]. Amplifications are much less frequent in low grade astrocytomas and are considered a late genetic event in the progression of tumors to glioblastoma. Either wild type or mutated forms of EGFR can be amplified, and in either case, both mRNA and cell surface protein levels are markedly increased. The most common EGFR amplification is a mutated form lacking exons 2-7, which results in a truncated cell surface protein with constitutive tyrosine kinase activity (EGFRvIII) [71–73].
The significance of EGFR gene amplification or EGFR protein over-expression as a prognostic marker in glioblastoma has been debated. Most comprehensive immunohistochemical and molecular genetic studies have concluded that EGFR status is not prognostically significant in patients with glioblastoma [69–71, 74]. Indeed, a recent meta-analysis of seven previously published investigations suggested that EGFR amplification was not associated with a statistically different prognosis [75]. In one of the most recent and most carefully performed investigations Liu et al. studied 221 astrocytic neoplasms (including 160 glioblastomas, 41 anaplastic astrocytomas, and 20 grade II) by Southern blot and quantitative PCR for EGFR amplification and EGFRvIII rearrangements and correlated the results with patient survival [71]. This investigation demonstrated that 41% of glioblastomas, 9.8% of anaplastic astrocytomas, and 0% of grade II astrocytomas had EGFR amplification and that 54% of the glioblastomas and 75% of the anaplastic astrocytomas that had EGFR amplification also had EGFRvIII rearrangements. There was a trend toward shorter survival of patient with anaplastic astrocytomas that contained EGFR abnormality (P = 0.069). However, neither EGFR amplification nor EGFRvIII rearrangement was associated with shorter survival in patients with glioblastoma. Other investigations have shown similar frequencies of EGFR amplification in glioblastomas and reached a similar conclusion that there is no association of these changes with patient outcome [69, 70]. It should be noted that the prognostic significance of EGFR expression may be more complex and that patient age may play a role in the prognostic significance of EGFR expression in glioblastoma [70, 76]. EGFR amplification and overexpression may be a marker of poor prognosis in younger patients and of good prognosis in older patients. Other studies have demonstrated that amplifications and overexpression of EGFR in anaplastic astrocytomas, although less common, might identify those that are further biologically progressed and associated with a poor prognosis [70, 71, 77]. Most analyses EGFR and EGFRvIII in glioblastoma have been performed at the genetic level using PCR-based techniques or FISH. Immunohistochemical techniques are available for the detection of EGFR and in high grade gliomas, but this application has not yet demonstrated its prognostic significance in glioblastomas or its ability to distinguish between histologic types of gliomas [77, 78].
Many of the most effective chemotherapeutic agents used to treat glioblastoma, including temozolomide and BCNU, are agents that crosslink DNA by alkylating at the O6 of guanine. DNA crosslinking is reversed by the DNA repair enzyme MGMT (O6-methylguanine-DNA methyltransferase). Thus, low levels of MGMT expression in the neoplasm would be expected to be associated with an enhanced response to alkylating agents. The expression level of MGMT is determined in large part by the methylation status of the gene’s promoter. This “epigenetic silencing” of MGMT occurs in 40–50% of glioblastomas and can be assessed by its promoter methylation status on PCR-based tests of genomic DNA. Epigenetic silencing of MGMT in tumor tissue is associated with response to BCNU therapy and improved survival in patients with GBM [79].
A recent investigation of temozolomide for the treatment of glioblastoma found that epigenetic gene silencing of MGMT was associated with a longer survival, independent of treatment [80, 81]. The study also demonstrated a survival advantage among those patients treated with temozolomide and radiotherapy whose glioblastomas had a silenced MGMT gene. Gene silencing in this study was determined by examining the methylation status of the MGMT promoter by methylation-specific polymerase-chain-reaction analysis. These tests are becoming more widely available in molecular diagnostic labs [82]. Antibodies are also available for the detection of the MGMT protein, which would make MGMT testing more technically feasible for most pathology laboratories [83, 84]. Correlations of immunohistochemical expression of MGMT with epigenetic status will be necessary as will a validation of a relationship between MGMT immunoexpression and therapeutic response. Since temozolomide has become a standard of care for the treatment of glioblastoma, testing for MGMT status will likely become an important component of a complete diagnostic workup.
Radiation oncology
Level I recommendation
Radiation therapy is recommended for the treatment of newly diagnosed malignant glioma in adults. Treatment schemes should include dosage of up to 60 Gy given in 2 Gy daily fractions that includes the enhancing area.
In 1978, the first of the Brain Tumor Study Group (BTSG) studies addressing these issues was reported by Walker et al. [85]. There were 303 patients with malignant glioma randomized to one of four study arms after surgical management. These included a control of best supportive care alone after surgery, chemotherapy alone with BCNU, radiation therapy alone with whole brain radiotherapy to a dose of 50–60 Gy and a combination of BCNU with radiotherapy (identical doses and delivery). Of the entire study group 73% were felt to have been valid for analysis (valid study group), including pathological confirmation and treatment according to the protocol. The authors also reported an “adequately treated” group that received at least the prescribed dose of radiation and at least two of the planned courses of BCNU chemotherapy. Analysis showed a significant advantage for those groups receiving radiation therapy compared to those receiving best supportive care or chemotherapy alone, with a median survival of 4.3 months for the best supportive care arm, 6.3 months in the chemotherapy alone group, 9.4 months in the radiotherapy alone group and 10.1 month in the group receiving both chemotherapy and radiation. The results of the latter three were all statistically significant when compared to the surgery alone group. This provides Class I data supporting a role for radiation therapy.
The follow-up BTSG study reported in 1980 randomized 467 patients with malignant glioma to semustine (CCNU) chemotherapy alone, radiotherapy alone, radiotherapy plus CCNU or radiotherapy plus BCNU [86]. This study again confirmed a significant advantage for the groups receiving radiotherapy. The radiotherapy in this trial was better controlled and included specification of 60 Gy in 6 to 7 weeks. The results in the “valid study” group that fulfilled protocol criteria indicated a median survival of 6 months in the CCNU alone arm, 9 months with radiotherapy alone, 12.8 months with BCNU plus radiotherapy and 10.5 months with CCNU plus radiotherapy. Statistical analysis indicated a significant survival advantage in radiotherapy containing arms over chemotherapy alone. This provided additional Class I data supporting the role for radiotherapy.
The randomized trial published by Sandberg-Wolheim et al. was conducted in Sweden and included 171 patients that were randomized to receive procarbazine, CCNU and vincristine (PCV) alone or in combination with 50 Gy to the whole brain and an additional 8 Gy to the ipsilateral hemisphere for a total of 58 Gy [87]. The analysis included 139 patients in the “valid study” group. In this group the median survival for the chemotherapy only group was 11.8 months versus 16.5 months with the addition of radiotherapy (P = 0.01). The trial showed that the addition of radiotherapy was advantageous and particularly so in those younger than 50 years of age (median survival 19.3 months vs. 30.5 months, P = 0.037).
A randomized trial of 443 patients reported by the Medical Research Council in the United Kingdom compared whole brain radiotherapy dosage of 45 Gy in 20 fractions to 60 Gy in 30 fractions for patients with newly diagnosed malignant glioma, as described by Bleehen et al. [88]. A two to one randomization scheme placed more patients in the higher dosage scheme. The one-year survival rates were 29% for the 45 Gy arm and 39% for the 60 Gy arm. The 18 month-survival rates were 11 and 18%, respectively and both comparisons were statistically significant (P = 0.04). This study provides Class I data supporting a dose of 60 Gy compared to 45 Gy.
In the combined Radiation Therapy Oncology Group (RTOG) and Eastern Cooperative Group (ECOG) trial reported by Nelson et al. 626 patients with newly diagnosed malignant glioma were randomized to four arms that included 60 Gy to the whole brain (141 patients), 60 Gy to the whole brain with a 10 Gy boost to the tumor (103 patients), 60 Gy with carmustine (156 patients) and 60 Gy with semustine and dacarbazine (138 patients) [89]. The median survival for the 60 and 70 Gy arms was reported as 9.3 and 8.2 months. No significant difference in median survival was found between any of the treatment arms. This provides Class I data that a dose above 60 Gy is not beneficial.
Hypo-fractionated radiation schemes may be used for patients with a poor prognosis and limited survival without compromising response.
A series of studies are available using various combinations of altered therapy. These include hyperfractionation, hypo-fractionation and accelerated techniques. Hyper-fractionation has perhaps received the most interest; however, the best quality data surrounds the use of hypofractionated treatment regimens. Roa et al. randomized 100 older patients with newly diagnosed glioblastoma to either conventional fractionation of 60 Gy in 30 fractions over six weeks or hypo-fractionation of 40 Gy in 15 fractions over 3 weeks [90]. The median survivals were 5.1 versus 5.6 months, respectively, and were not significantly different (P = 0.57). The authors concluded that in the population over age 60, this hypo-fractionated regimen could be considered.
Phillips et al. randomized 68 older patients (84% over 40 years of age, median age 58–59 years) with newly diagnosed glioblastoma to either conventional fractionated therapy of 60 Gy in 30 fractions over six weeks or to 35 Gy in 10 fractions of whole brain radiotherapy [91]. The study was closed prematurely due to poor accrual and was unable to demonstrate a significant difference, although the median survival for the conventional group was longer, comparing 10.3 months for conventional fractionation versus 8.7 months for the 35 Gy group (P = 0.37).
Ford et al. performed a matched-pair analysis comparing 27 poor prognosis patients treated with 36 Gy in 12 fractions to 27 matched patients treated with 60 Gy in 30 fractions [92]. Comparison of the groups indicated no difference in outcome (Hazard ratio of 1.0, 95% CI 0.57–1.74) and the authors concluded that for poor prognosis patients the shorter hypo-fractionated regimen was at least no worse than conventional fractionation.
Glinski et al. published a randomized controlled trial of 108 patients including 44 with glioblastoma and 64 with anaplastic astrocytoma with two arms: conventional fractionation (50 Gy whole brain plus 10 Gy in five fractions to the tumor) or hypo-fractionation (two courses of 20 Gy in five fractions separated by a month and followed a month later by 10 Gy in five as a boost to the tumor) [93]. The groups appeared to be well balanced. Reporting on the two-year survival there was no survival advantage for the anaplastic astrocytoma groups (22% vs. 18%, P > 0.05), However, they found a survival advantage in the subgroup of 44 glioblastoma patients treated with hypo-fractionated split regimen of 23% versus 10% (P < 0.05).
Hyper-fractionation and accelerated fractionation have not been shown to be superior to conventional fractionation and are not recommended.
Prados et al. reported a trial of 231 patients with newly diagnosed malignant glioma randomized into two radiotherapy treatments, accelerated hyper-fractionation with a total dose of 70.4 Gy at 1.6 Gy twice daily versus conventional fractionation to a total dose of 59.4 Gy at 1.8 Gy daily [94]. Comparison of the two groups demonstrated similar median survivals (10.5 vs. 10.2 months, respectively, P = 0.75).
Deutsch et al. randomized 603 patients into a trial that included randomization to groups receiving conventional fractionation with either BCNU, steptozotocin or misonidazole or hyper-fractionated radiotherapy plus BCNU [95]. No significant difference in survival was identified.
The trial by Ludgate et al. randomized 76 patients to either receive whole brain radiotherapy (40 Gy) plus local boost therapy (10 Gy) with daily treatments or hyper-fractionation to a total dose of 47.6 Gy in three times daily fractions, hence also accelerated [96]. This study is comparatively small but also demonstrated no significant differences in survival were identified.
Shin et al.’s trial published in 1985 compared two fractionation schemes: conventional fractionation of 58 Gy in 30 once-daily fractions over 6 weeks versus 61.4 Gy in three times daily fractions [97]. An additional arm included hyper-fractionation plus misonidazole and showed no advantage. The authors found an improvement in 1 year survival comparing 41% for the hyper-fractionated group versus 20% for the conventional fractionation group with a P-value of 0.07 which the authors concluded was significant. This paper updated the paper by Fulton et al. [98].
An earlier trial by Shin et al. compared conventionally fractionated whole brain radiotherapy of 34 Gy in 17 fractions plus a 16 Gy local boost with hyper-fractionated (superfractionated) treatments of 40 Gy whole brain in 45 fractions plus 10 Gy local boost [99]. The authors found no significant difference between the treatment arms and noted some imbalances between the two groups.
Payne et al. randomized 157 patients into two groups comparing hyper-fractionated radiotherapy to 36–40 Gy in four times daily fractions with conventional radiotherapy of 50 Gy in 25 fractions with both groups also receiving CCNU and hydroxyurea [100]. No significant difference in median survival was noted.
Brachytherapy or stereotactic radiosurgery as a boost to external beam radiotherapy have not been shown to be beneficial and are not recommended in the routine management of newly diagnosed malignant glioma.
Significant effort has gone into attempting to identify patients with malignant glioma who would benefit from brachytherapy techniques. Despite these thoughtful study designs and potentially promising results, two randomized trials of brachytherapy failed to demonstrate a survival advantage for brachytherapy when added to the treatment of newly diagnosed malignant glioma. The study of Laperriere et al. published in 1998 randomly assigned 140 patients to external radiotherapy of 50 Gy in 25 fractions over five weeks (69 patients) versus the same external radiotherapy plus temporary stereotactic iodine-125 implants with a minimum peripheral tumor dose of 60 Gy (71 patients) [101]. Median survival for the brachytherapy arm was 13.8 months versus 13.2 months for the non-brachytherapy arm (P = 0.49). Improved survival was associated with either chemotherapy or reoperation at progression (P = 0.004) or KPS greater than or equal to 90 (P = 0.007). The authors concluded that stereotactic radiation implants did not demonstrate a statistically significant improvement in survival in the initial management of patients with malignant glioma.
Although the initial report of the Brain Tumor Cooperative Group (BTCG Trial 87-01) randomized trial of radiotherapy plus BCNU with and without interstitial radiation for a total dose of 60 Gy at the tumor periphery suggested a significant survival advantage, the subsequent published report did not. The final report of Selker et al. described this randomized multi-center comparison of surgery, EBRT and BCNU (n = 137) versus surgery, EBRT, BCNU and I-125 brachytherapy boost (n = 133) in newly diagnosed malignant glioma (299 total patients, with 270 (90%) in the valid study group) [102]. The median survival, with all pathologies included, for surgery, EBRT and BCNU (control) was 14.7 months compared to 17.0 months for surgery, EBRT, BCNU and (125)-I brachytherapy (P = 0.101). In the GBM only group (n = 230) the median survival was 14.5 for control (n = 107) and 16.0 months for the brachytherapy group (n = 123), (P = 0.169). As in most previous studies, age, KPS and pathology were all independent predictors of mortality. Incorporating an adjustment for these variables in both stratified and Cox proportional hazard models failed to demonstrate any statistically significant differences in survival between these two treatment groups. The authors concluded that no long-term survival advantage was demonstrated with the addition of (125)-I brachytherapy to surgery, EBRT and BCNU in patients with newly diagnosed malignant glioma.
A series of encouraging reports initially described the use of radiosurgery as a focal radiation dose boost in conjunction with fractionated external beam radiotherapy in the treatment of newly diagnosed malignant gliomas. The prospective multi-center randomized trial RTOG 93-06 in newly diagnosed glioblastoma was reported by Souhami et al. and recruited 203 patients. Seventeen patients were excluded from final analysis including seven who were randomized to SRS but had tumor treatment diameters greater than 40 mm at the time of SRS. Ten additional patients were excluded based on histology (n = 3), refusal or withdrawal (n = 4), multifocal tumor (n = 1), prior chemotherapy (n = 1) and failure to record KPS (n = 1), leaving 186 patients for evaluation. Ninety-seven were randomized to EBRT alone and eighty-nine to EBRT plus SRS. Both groups received IV BCNU. Median survival was 13.6 in the EBRT group and 13.5 in EBRT plus SRS (P = 0.57) with no significant difference in two and three survival rates or quality of life measures. The authors conclude that stereotactic radiosurgery followed by EBRT and BCNU does not improve outcome in patients with newly diagnosed glioblastoma [103].
Level II recommendation
It is recommended that radiation therapy planning include a 1 to 2 cm margin around the radiographically defined T1 contrast-enhancing tumor volume or the T2 weighted abnormality on MR imaging.
Despite the propensity of early whole brain radiotherapy studies, the choice for volume of radiation delivery has evolved to a more limited field based primarily on natural history studies demonstrating a tendency for local recurrence [104–106] and Class II data suggesting a lack of benefit for whole brain radiotherapy compared to more limited fields. Randomized studies addressing the volume of radiotherapy delivery have been limited. Shapiro et al. described the BTCG 8001 study in which 571 patients were randomized into three chemotherapy regimens [107]. In the early phase of the trial, patients received 60 Gy whole brain radiotherapy. In the later phases, the protocol was modified and patients received 43 Gy whole brain radiotherapy and an additional 17 Gy focused on the enhancing volume plus a 2 cm margin. After analysis there was no difference in survival between the two different radiotherapy regimens. Although this was a randomized study, it was not specifically designed to address the issue of radiotherapy delivery. Therefore, there is only Class II data supporting the role of limited field therapy.
Kita et al. published the results of their randomized trial in which patients received either 40 Gy whole brain radiotherapy in 20 fractions followed with a local boost of 18 Gy in 9 fractions, giving a total dose of 58 Gy, or 56 Gy in 28 fractions targeted to the enhancing tumor volume [108]. The authors reported no significant difference in survival between the two groups. The two-year survival was 43% for the whole brain group versus 39% for the local field group and 17% versus 27% at four years. The study consisted of a small number of patients (23 and 26 patients respectively). This is additional Class II data supporting more limited fields.
Cytotoxic chemotherapy management
Level I recommendation
Concurrent and post-irradiation temozolomide is recommended in patients 18 to 70 years of age with adequate systemic health. This recommendation is supported on evidence from a single Class I study.
The European Organization for Research and Treatment of Cancer (EORTC) and the National Cancer Institute of Canada (NCIC) Clinical Trials Group conducted a clinical trial of concomitant radiotherapy and adjuvant temozolomide for newly diagnosed glioblastoma. This pivotal study, reported by Stupp et al. accrued a total of 573 patients (18 to 70 years old) from 2000 to 2002. The patients were randomized to standard radiotherapy (60 Gy in 30 daily fractions of 2 Gy) versus the same radiotherapy and concomitant temozolomide (75 mg/m2/d, daily up to 42 days) followed by up to six cycles of adjuvant temozolomide (150–200 mg/m2, daily × 5d, q28 d). Median follow-up was 28 months. The results showed the increase in median survival of 2.5 months for radiotherapy plus temozolomide over radiotherapy alone (14.6 months vs. 12.1 month, respectively). More importantly, the survival at two years was 26.5% for radiotherapy plus temozolomide and 10.4% for radiotherapy alone, a significant improvement compared to historical data. Progression free time was 6.9 months for radiotherapy plus temozolomide and 5.0 months for radiotherapy alone. The log-rank test for median survival, two year survival rate and progression-free survival was significant with a P-value of <0.0001. This significant survival benefit was sustained across all subsets at further analysis, except for a small subgroup of patients who underwent biopsy only and those with a poor KPS. Grade 3/4 hematologic toxicity was observed in 7% of patients during concomitant radiotherapy and temozolomide treatment and in 14% during adjuvant temozolomide treatment. The authors concluded that the addition of temozolomide to radiotherapy for newly diagnosed glioblastoma resulted in a clinically meaningful and statistically significant survival benefit with minimal additional toxicity [109]. The prospective, randomized nature of this investigation in which glioblastoma data can be separated from other histologies supports interpretation of this trial as Class I evidence. Clearly, much work still needs to be done to further enhance the survival and the quality of life of patients with glioblastoma. Although the search for supporting papers in this portion of the guidelines generated many studies that met the criteria for Class I data, many were negative, provided nonspecific recommendations or did not firmly demonstrate the benefit of one therapy over another.
Level II recommendation
BCNU-impregnated biodegradable polymers are recommended in patients for whom craniotomy is indicated. This recommendation based on the evidence from two Class II studies.
Meaningful experience utilizing interstitial chemotherapy alone in the treatment of newly diagnosed glioblastoma is not available. However, two prospective analyses of this modality in combination with radiation are available for interpretation. In the first, Valtonen et al. randomized 32 patients (27 were diagnosed as glioblastoma) in a double-blind, prospective study of BCNU delivered in biodegradable polymer (Gliadel) versus placebo wafers. All patients received standard radiotherapy. For patients with GBM, the Gliadel treated group had a median survival of 53.3 weeks compared to 39.9 weeks in the placebo group (P = 0.008). However, the study was stopped earlier than planned due to lack of Gliadel from the manufacturer, impairing the power and validity of the study [81]. Therefore, though designed to produce Class I data, the study is only able to provide Class II information for the purposes of this review.
A larger placebo-controlled, double-blinded study of biodegradable BCNU wafers compared to placebo wafers in patients with newly diagnosed malignant gliomas was subsequently performed. In this investigation, 240 patients (207 glioblastoma) were randomized based on intraoperative diagnosis. All went on to standard external fractionated radiation therapy. The median survival of the BCNU wafer-treated glioblastoma patients was 13.5 months and the median survival of the placebo treated glioblastoma group was 11.4 months (P = 0.10). When corrected for prognostic factors of gender, age and KPS, it was concluded that the BCNU wafer group had a longer survival (P = 0.04). The hazard ratio in the GBM patients treated with BCNU wafers was 0.76, indicating a 24% mortality risk reduction. This is certainly suggestive of an interesting effect in the glioblastoma subgroup. However, the study was powered to find significance in the intent to treat population which included malignant gliomas and not just glioblastoma. As there was not a specific randomization between treatment and placebo arms for the GBM subgroup, it cannot be assumed that the difference reported in the glioblastoma subgroup is truly significant, even given adjustments with the Cox proportional hazards model. Thus, this represents Class II data. The survival time to tumor progression based on imaging and clinical criteria was the same for both groups, suggesting no benefit in tumor control based on this method of analysis. The authors recognized that BCNU wafer-induced imaging changes can confound time to progression analysis. Cerebrospinal fluid leakage was more common in the BCNU wafer group than in placebo patients. Though implied as useful for newly diagnosed glioblastoma, it must be recognized that this technique is not applicable to cases with multifocal masses, inaccessible tumors or for patients who have medical limitations precluding the use of surgery [110].
Level III recommendations
The addition of temozolomide to radiation therapy is an option for patients with newly diagnosed glioblastoma who are older than 65 years with a Karnofsky performance status (KPS) above 50.
Recommendations of treatment for older patients can only arise from studies tailored to examine that specific population. Unfortunately, only a few non-controlled clinical trials have focused on examining the benefit of cytotoxic chemotherapy in the elderly population with newly diagnosed glioblastoma. Brandes et al. reported on the outcome of 79 consecutive patients, 65 years of age or older, with the diagnosis of glioblastoma and KPS of more than 50 [111]. Patients were followed prospectively and treatment varied according to the time period when diagnosed yielding Class II data. The first group enrolled 24 patients who were treated with radiotherapy alone in the period from March 1993 to August 1995. The second group included 32 patients who received the same radiotherapy regimen, plus adjuvant PCV (September 1995 to September 1997). The third group enrolled 23 patients who were treated with the same radiotherapy regimen, plus adjuvant temozolomide (September 1997 to August 2000). Adjuvant chemotherapy was started four weeks after the end of radiotherapy and temozolomide was delivered at a dosage of 150 mg/m2 daily for five days every 28 days. No drug escalation was allowed. The time to tumor progression was significantly longer for the temozolomide group, compared to the first and second groups (10.7 months vs. 5.3 months and 6.9 months, respectively, P = 0.0002). The median overall survival of 11.2 months after radiation alone improved significantly to 14.9 months when temozolomide was added.
Class III studies suggest that for patients 70 years or older with newly diagnosed glioblastoma, temozolomide alone is a well tolerated alternative to radiation therapy and its benefit might be comparable to that obtained with radiation therapy alone.
Chinot et al. published the results of a phase II clinical trial using only temozolomide as first line therapy in patients older than 70 years of age with newly diagnosed glioblastoma [112]. Only 32 of 57 eligible patients were included, with a median survival from the time of diagnosis of 6.4 months and a progression-free survival of 5.0 months. In 16 of 32 patients (50%) there was a one-level increase in KPS or a five-point increase in Mini-Mental State Examination score, accompanied by stable or decreased steroid dosage. Twenty-nine patients had measurable post-operative disease by MRI that showed partial response in nine patients (31%; 95% CI, 14–48%), stable disease in 12 patients (41%; 95% CI, 23–59%) and progressive disease in eight patients (28%; 95% CI, 12–44%). The definition of efficacy or futility for this approach was not described in this phase II clinical trial. Grade 3–4 hematologic toxicity consisted of thrombocytopenia in 6% and neutropenia in 9% of the patients. The phase II nature of the work combined with multiple reasons for limits in the number of patients enrolled that could be analyzed yields Class III data.
Glantz et al. retrospectively reviewed their experience with 86 consecutive patients with high grade glioma (98% had glioblastoma) who were older than 70 years of age [113]. As it is retrospective, this study yields Class III data. Radiation therapy alone was the treatment for 54 patients (63%), resulting in a median survival of 4.1 months and one-year survival of 9.26%. For 32 patients who received temozolomide alone as first line treatment, the median survival was six months and the one-year survival was 11.88%. No patients in the chemotherapy-only group had to discontinue treatment because of side effects, while RT was stopped due to toxicity in five of 54 patients.
Radiation therapy, followed by one of the nitrosoureas, is recommended for those patients not eligible for temozolomide.
As mentioned above in the summary of the study by Brandes et al. one portion of the investigation included a radiotherapy regimen plus adjuvant PCV. There was no statistical difference in overall survival between that group and the radiation plus temozolomide groups [111]. The choice of the PCV regimen, CCNU alone or even other nitrosoureas alone is a choice that must be made by the managing physician based upon their experience and the patient’s specific circumstances.
Summary and future directions
The information in the neuroradiology guideline does not provide direction as to which method of imaging brain tumors will prove to be superior in the future [114]. Certainly, techniques such as measuring regional cerebral blood volume as a surrogate of histology appear promising and warrant further study. Magnetic resonance spectroscopy is likely to provide very useful data for glioblastoma diagnosis, but unlikely to replace, by itself, the need for pathology classification. Once any imaging modality shows reasonable technical promise and consistency, assessment of its true value should include a prospective study of meaningful numbers of tumors whose histology is known (by direct surgical sampling) by a series of clinicians blinded to the known tumor type and who make as detailed and committed a diagnosis as is possible. Improvements in glioblastoma imaging that would allow it to act as a reliable surrogate for histology and overcome limitations due to tumor heterogeneity would be of great value in facilitating patient comfort, minimizing morbidity and assessing treatment.
It is clear from the neurosurgical guideline that properly planned prospective or case control studies designed to address the impact of extent of resection or postoperative tumor burden on clinical outcome must incorporate neuro-imaging methodology that allows accurate and consistent analysis [115]. The role of advanced neuro-imaging in evaluating resections in these patients remains an area of investigation. The role of intraoperative MRI and advanced intraoperative ultrasound imaging need to be clarified and expanded to improve the extent and safety of surgery and be balanced against technology costs. This ties in well with the needed improvements in preoperative imaging of brain tumors mentioned in the neuroradiology guidelines, as these technologies will assist both preoperative and postoperative care. The continued development of intra-operative tumor markers or enhancing agents should greatly assist in surgical decision-making and may result in improved extent of resection without creating new neurological deficit. Development of standardized methodologies for residual tumor assessment and investigation into techniques for assessing the residual “non-enhancing” tumor burden are needed. The study of malignant primary neoplasms with evolving molecular imaging techniques may be linked to molecular-based treatment paradigms.
Histologic classification and grading remains a powerful and cost-effective tool for providing prognostically meaningful diagnoses for glial neoplasms for the neuropathologist [116]. It has become clear, however, that specific histopathology entities may include several genetic subtypes, raising the possibility that molecular alterations may be important for predicting survival and responsiveness to therapy within diagnostic groups. The future of neuro-oncology will likely require an expanded role defining the genetic make-up of gliomas, including the status of 1p, 19q, EGFR, 10q (PTEN), TP53 and MGMT. New biologic concepts are emerging from the study of tumor stem cells and new diagnostic techniques have been advanced from micro-array and proteomic technologies and that could revolutionize pathology. It has recently been demonstrated that there is a small subset of tumor cells in GBMs, and presumably other malignant gliomas, that have stem-cell like properties (CD133+) that are responsible for self-renewing and radioresistant properties [117, 118]. The identification and characterization of these cell-types in glioblastoma specimens as a part of diagnosis may prove critical. Proteomic investigations of the CSF from patients with malignant gliomas are uncovering novel proteins that may serve as markers of advanced disease or tumor progression [119, 120]. Gene expression profiles have identified new molecular markers that can be exploited for classification and grading, but have also challenged our conception of tumor classification [118]. Gene expression profiles, coupled with computer modeling algorithms, are capable of reliably predicting clinical outcome for glial neoplasms [121–123]. Indeed, computer generated tumor class distinction based on their gene expression profiles may predict clinical outcome better than standard pathologic classifications.
In the radiation oncology guideline, consistent Class I data supports the conclusion that radiation therapy should be recommended as standard therapy for glioblastoma [124]. Patients with good prognosis can confidently be treated with conventional doses of 60 Gy in 30 fractions, as supported by the body of the literature. Consideration for hypofractionated regimens, especially in the setting of poor prognosis, is very reasonable and is supported by the literature in Class I data. Local fields are generally used to treat the tumor volume as identified on imaging with a 1–2 cm margin. Although there is minimal Class I support for this, the preponderance of evidence supports this approach and there is no clear benefit of larger whole brain fields. Studies addressing the most appropriate volume of solid and infiltrating tumor in a systematic fashion are needed. The role of dose escalation with brachytherapy and radiosurgery is limited and not supported as a standard approach with the data at hand.
Although there has been recent important progress in the medical treatment of newly-diagnosed GBM, the addition of temozolomide to radiation therapy results in only a modest 2.5 month improvement in median survival [125]. There is clearly a need to develop more effective therapies. Overcoming resistance to this drug due to MGMT promoter methylation will be a significant advance in glioblastoma therapy. Other strategies being explored to overcome tumor resistance to temozolomide and other alkylating agents include combinations with inhibitors of MGMT such as O6-benzylguanine (O6BG) and O6-(4-bromothenyl)-guanine (PaTrin-2), with inhibitors of poly(ADP-ribose) polymerase (PARP) which is involved in repair of N7 methylation, and with inhibitors of the NFκB pathways [126–133].
There is also significant interest in combining radiotherapy and standard chemotherapy with targeted molecular agents and inhibitors of angiogenesis [134, 135]. Trials are currently assessing combining epidermal growth factor receptor (EGFR) inhibitors such as erlotinib, vascular endothelial growth factor receptor (VEGFR) inhibitors such as vatalanib (PTK787), or dual EGFR and VEGFR inhibitors such as vandetanib (ZD6474) with radiation therapy and temozolomide [136–138]. Ultimately, the goal is to genotype each patient’s tumor and allow for the most appropriate therapeutic agents to be selected on an individual basis.
Epidemiologic studies suggest that there has been an increase in the incidence of brain tumors in the elderly, and age is probably the most important prognostic indicator of survival in patients with glioblastoma. If the prevailing nihilistic therapeutic approach for this population is to change, well-designed and controlled studies that demonstrate the effectiveness of cytotoxic chemotherapy with a tolerable toxicity profile are required. The benefit of the addition of temozolomide to radiation therapy for the treatment of patients older than 70 years of age is unknown since this cohort was excluded in the Stupp trial [80]. Therefore, future controlled trials need to be inclusive of elderly patients, keeping in mind that measurement of quality of life might be a more relevant primary endpoint in chemotherapy clinical trials than in the younger population.
Standard cytotoxic chemotherapeutic agents with a history of failing systemically may be worthy of reevaluation as interstitial treatment agents. Though biodegradable devices have a role, convection-enhanced delivery may serve the same purpose and overcome limitations in biodegradable matrix compatibility with treatment agents. In view of the promising preliminary data supporting interstitial therapy administration, it is recommended that patients be considered for enrollment in high quality investigative protocols studying this issue. Biologic methods such as viral delivery also warrant encouragement and funding.
This set of guidelines should not be a static group of documents. Rather, it warrants refreshment at regular intervals. Ideally, this would be by a separate multi-disciplinary set of experts using this guideline as a point of departure. This maximizes the chance of identifying weaknesses and guiding recommendations for future improvements. Ideally, application of evidence-based principals as were used here can be implemented proactively to point out where weaknesses in our knowledge may lie and serve as a guide to basic and clinical research. These guidelines are not meant to tell physicians how to manage patients or to take away independence of practice. Anyone who regularly manages individuals with glioblastoma recognizes the variety of presentations that are possible. Thus, their therapy needs to be individualized based on their circumstances, utilizing evidence-based guidelines such as these not as a set of limitations, but as a point of departure. Though perceived as painful by some practitioners, Brockman’s statement that, “In a culture shaped by truly critical thinking and scientific method, being proven wrong, and being constantly challenged to prove your most cherished concepts, is understood as part of intellectual evolution” is applicable to guideline development and their ongoing modification [139]. In light of this, even new avenues and pilot or preliminary clinical research can be reviewed, classified and ranked. Automated classification systems proposed for use by the National Library of Medicine and other organizations on a prospective basis may facilitate these endeavors in the future. Continued oversight by parent organizations in neurosurgery or other specialties is of value. In the case of this set of guidelines, the guidance and support of the Joint Tumor Section of the Congress of Neurological Surgeons and the American Association of Neurological Surgeons was critical to their successful completion. This oversight assists in minimizing any sense of conflict of interest and improves the likelihood of the document providing meaningful guidance for health policy makers.
References
Johnstone PA (2008) ACR appropriateness criteria. Int J Radiat Oncol Biol Phys 70:1303–1304. doi:10.1016/j.ijrobp.2007.08.075
Burstin H, Lanier D (2001) Update from funders: Center for Primary Care Research and Agency for Health Care Research and Quality. Med Care 39:309–311. doi:10.1097/00005650-200104000-00001
Brem SS, Beirman PJ, Black P, Brem H, Chamberlain MC, Chiocca EA, DeAngelis LM, Fenstermaker RA, Friedman A, Gilbert MR, Glass J, Grossman SA, Heimberger AB, Junck L, Linette GP, Loeffler JJ, Maor MH, Moots P, Mrugala M, Nabors LB, Newton HB, Olivi A, Pornow J, Prados M (2008) Central Nervous System cancers, clinical practice guidelines in oncologyTM. J Natl Compr Cancer Cent Netw 6:456–504
Sackett DL, Straus SE, Richardson WS, Rosenberg W (2000) Evidence-based medicine: how to practice and teach EBM, vol 2. Churchill Livingstone, Edinburgh
Field MJ, Lohr KN (1990) Clinical practice guidelines: directions for a new program. National Academy Press, Washington DC, pp 78–95
Olson JJ, Ryken T (2008) Guidelines for the treatment of newly diagnosed glioblastoma: introduction. J Neurooncol 89:255–258. doi:10.1007/s11060-008-9595-4
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46. doi:10.1177/001316446002000104
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174. doi:10.2307/2529310
Walters BC (1998) Clinical practice parameter development in neurosurgery. In: Bean JR (ed) Neurosurgery in transition: the socioeconomic transformation of neurological surgery. Williams and Wilkins, Baltimore, pp 99–111
Moher D, Schulz KF et al (2001) The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Lancet 357:1191–1194. doi:10.1016/S0140-6736(00)04337-3
Lai R, Chu R et al (2006) Quality of randomized controlled trials reporting in the primary treatment of brain tumors. J Clin Oncol 24(7):1136–1144. doi:10.1200/JCO.2005.03.1179
DerSimonian R, Laird N (1986) Meta-analysis of clinical trials. Control Clin Trials 7:177–188. doi:10.1016/0197-2456(86)90046-2
Fine HA, Dear KBG, Loeffler JS, Black PM, Canellos GP (1993) Meta-analysis of radiation therapy with and without adjuvant chemotherapy for malignant gliomas in adults. Cancer 71:2585–2597. doi:10.1002/1097-0142(19930415)71:8<2585::AID-CNCR2820710825>3.0.CO;2-S
Glioma Meta-analysis Trialists Group (2002) Chemotherapy in adult high-grade gliomas: a systemic review and meta-analysis of individual patient data from 12 randomized trials. Lancet 359:1011–1018. doi:10.1016/S0140-6736(02)08091-1
Piedbois P (2004) Meta-analysis based on abstracted data: a step in the right direction, but only a first step. J Clin Oncol 19:3839–3841. doi:10.1200/JCO.2004.06.924
Methodology of guideline development (2002) Guidelines for the management of acute cervical spine and spinal cord injuries. Neurosurgery 50(3):S2–S6
Dean BL, Drayer BP, Bird CR et al (1990) Gliomas: classification with MR imaging. Radiology 174:411–415
Amundsen P, Dugstad G, Syvertsen AH (1978) The reliability of computer tomography of the diagnosis and differential diagnosis of meningiomas, gliomas and brain metastases. Acta Neurochir (Wien) 41:177–190. doi:10.1007/BF01809148
Carapella CM, Carpinelli G, Knijn A et al (1997) Potential role of in vitro 1H magnetic resonance spectroscopy in the definition of malignancy grading of human neuroepithelial brain tumors. Acta Neurochir Suppl (Wien) 68:127–132
Reimann B, Papke K, Hoess N et al (2002) Noninvasive grading of untreated gliomas: a comparative study of MR imaging and 3- (iodine 123)-L-a-methyltyrosine SPECT. Radiology 225:567–574. doi:10.1148/radiol.2252011431
Tamiya T, Kinoshita K, Ono Y et al (2000) Proton magnetic resonance spectroscopy reflects cellular proliferative activity in astrocytomas. Neuroradiology 42:333–338. doi:10.1007/s002340050894
Howe FA, Barton SJ, Cudlip SA et al (2003) Metabolic profiles of human brain tumors using quantitative in vivo magnetic resonance 1H spectroscopy. Magn Reson Med 49:223–232. doi:10.1002/mrm.10367
Moller-Hartmann W, Herminghaus S, Krings T et al (2002) Clinical application of proton magnetic resonance spectroscopy in the diagnosis of intracranial mass lesions. Neuroradiology 44:371–381. doi:10.1007/s00234-001-0760-0
Lee SJ, Kim JH, Kim YM et al (2001) Perfusion MR imaging in gliomas: comparison with histologic grade. Korean J Radiol 2:1–7
Shin JH, Lee HK, Kwun BD et al (2002) Using relative cerebral blood flow and volume to evaluate the histopathologic grade of cerebral gliomas. Am J Radiol 179:783–789
Roberts HC, Roberts TPL, Bollen AW et al (2001) Correlation of microvascular permeability derived from dynamic contrast enhanced MR imaging with histologic grad and tumor labeling index: a study in human brain tumors. Acad Radiol 8:384–391. doi:10.1016/S1076-6332(03)80545-7
Lacroix M, Abi-Said D, Fourney DR et al (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95(2):190–198
Hess KR (1999) Extent of resection as a prognostic variable in the treatment of gliomas. J Neurooncol 42(3):227–231. doi:10.1023/A:1006118018770
Jackson RJ, Fuller GN, Abi-Said D et al (2001) Limitations of stereotactic biopsy in the initial management of gliomas. Neuro-oncol 3(3):193–200. doi:10.1215/15228517-3-3-193
Vuorinen V, Hinkka S, Farkkila M, Jaaskelainen J (2003) Debulking or biopsy of malignant glioma in elderly people—a randomised study. Acta Neurochir (Wien) 145(1):5–10. doi:10.1007/s00701-002-1030-6
Stummer W, Pichlmeier U, Meinel T, Wiestler OD, Zanella F, Reulen HJ (2006) Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomized controlled multicentre phase III trial. Lancet Oncol 7(5):392–401. doi:10.1016/S1470-2045(06)70665-9
Simpson JR, Horton J, Scott C et al (1993) Influence of location and extent of surgical resection on survival of patients with glioblastoma multiforme: results of three consecutive Radiation Therapy Oncology Group (RTOG) clinical trials. Int J Radiat Oncol Biol Phys 26(2):239–244
Ammirati M, Vick N, Liao YL, Ciric I, Mikhael M (1987) Effect of the extent of surgical resection on survival and quality of life in patients with supratentorial glioblastomas and anaplastic astrocytomas. Neurosurgery 21(2):201–206. doi:10.1097/00006123-198708000-00012
Levin VA, Wara WM, Davis RL et al (1985) Phase III comparison of BCNU and the combination of procarbazine, CCNU, and vincristine administered after radiotherapy with hydroxyurea for malignant gliomas. J Neurosurg 63(2):218–223
Kiwit JC, Floeth FW, Bock WJ (1996) Survival in malignant glioma: analysis of prognostic factors with special regard to cytoreductive surgery. Zentralbl Neurochir 57(2):76–88
Burger PC, Scheithauer BW, Vogel FS (2002) Surgical pathology of the nervous system and its coverings. Churchill Livingstone, New York
Kleihues P, Cavenee WK (2000) Pathology and genetics of tumours of the nervous system. IARC Press, Lyon
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (2007) WHO classification of tumours of the Central Nervous System. International Agency for Research, Lyon
Burger PC, Scheithauer BW (1994) Tumors of the Central Nervous System. Armed Forces Institute of Pathology, Washington, DC
Daumas-Duport C, Scheithauer B, O’Fallon J et al (1988) Grading of astrocytomas, A simple and reproducible method. Cancer 62:2152–2165. doi:10.1002/1097-0142(19881115)62:10<2152::AID-CNCR2820621015>3.0.CO;2-T
Revesz T, Scaravilli F, Coutinho L et al (1993) Reliability of histological diagnosis including grading in gliomas biopsied by image-guided stereotactic technique. Brain 116(Pt 4):781–793. doi:10.1093/brain/116.4.781
Gupta M, Djalilvand A, Brat DJ (2005) Clarifying the diffuse gliomas: an update on the morphologic features and markers that discriminate oligodendroglioma from astrocytoma. Am J Clin Pathol 124:755–768. doi:10.1309/6JNX4PA60TQ5U5VG
Burger PC, Nelson JS (1997) Stereotactic brain biopsies: specimen preparation and evaluation. Arch Pathol Lab Med 121:477–480
Martinez AJ, Pollack I, Hall WA et al (1988) Touch preparations in the rapid intraoperative diagnosis of Central Nervous System lesions, A comparison with frozen sections and paraffin embedded sections. Mod Pathol 1:378–384
Reyes MG, Homsi MF, McDonald LW et al (1991) Imprints, smears, and frozen sections of brain tumors. Neurosurgery 29:575–579. doi:10.1097/00006123-199110000-00015
Brainard JA, Prayson RA, Barnett GH (1997) Frozen section evaluation of stereotactic brain biopsies: diagnostic yield at the stereotactic target position in 188 cases. Arch Pathol Lab Med 121:481–484
Gaudin PB, Sherman ME, Brat DJ et al (1997) Accuracy of grading gliomas on CT-guided stereotactic biopsies: a survival analysis. Diagn Cytopathol 17:461–466. doi:10.1002/(SICI)1097-0339(199712)17:6<461::AID-DC16>3.0.CO;2-K
Prayson RA, Agamanolis DP, Cohen ML et al (2000) Interobserver reproducibility among neuropathologists and surgical pathologists in fibrillary astrocytoma grading. J Neurol Sci 175:33–39. doi:10.1016/S0022-510X(00)00274-4
Prayson RA (2002) Cell proliferation and tumors of the Central Nervous System, part II: radiolabeling, cytometric, and immunohistochemical techniques. J Neuropathol Exp Neurol 61:663–672
McKeever PE, Ross DA, Strawderman MS, Brunberg JA, Greenberg HS, Junck L (1997) A comparison of the predictive power for survival in gliomas provided by MIB-1, bromodeoxyuridine and proliferating cell nuclear antigen with histopathologic and clinical parameters. J Neuropathol Exp Neurol 56:798–805. doi:10.1097/00005072-199756070-00006
Giannini C, Scheithauer BW, Burger PC, Christensen MR, Wollan PC, Sebo TJ et al (1999) Cellular proliferation in pilocytic and diffuse astrocytomas. J Neuropathol Exp Neurol 58:46–53. doi:10.1097/00005072-199901000-00006
Wakimoto H, Aoyagi M, Nakayama T, Nagashima G, Yamamoto S, Tamaki M et al (1996) Prognostic significance of Ki-67 labeling indices obtained using MIB-1 monoclonal antibody in patients with supratentorial astrocytomas. Cancer 77:373–380. doi:10.1002/(SICI)1097-0142(19960115)77:2<373::AID-CNCR21>3.0.CO;2-Y
Moskowitz SI, Jin T, Prayson RA (2006) Role of MIB1 in predicting survival in patients with glioblastomas. J Neurooncol 76:193–200. doi:10.1007/s11060-005-5262-1
Hunter SB, Brat DJ, Olson JJ, Von Deimling A, Zhou W, Van Meir EG (2003) Alterations in molecular pathways of diffusely infiltrating glial neoplasms: application to tumor classification and anti-tumor therapy. Int J Oncol 23:857–869 Review
Ohgaki H, Kleihues P (2005) Population-based studies on incidence, survival rates, and genetic alterations in astrocytic and oligodendroglial gliomas. J Neuropathol Exp Neurol 64:479–489
Collins VP (2007) Mechanisms of disease: genetic predictors of response to treatment in brain tumors. Nat Clin Pract Oncol 4:362–374. doi:10.1038/ncponc0820
Smith JS, Perry A, Borell TJ, Lee HK, O’Fallon J, Hosek SM et al (2000) Alterations of chromosome arms 1p and 19q as predictors of survival in oligodendrogliomas, astrocytomas, and mixed oligoastrocytomas. J Clin Oncol 18:636–645
Perry A, Fuller CE, Banerjee R, Brat DJ, Scheithauer BW (2003) Ancillary FISH analysis for 1p and 19q status: preliminary observations in 287 gliomas and oligodendroglioma mimics. Front Biosci 8:a1–a9. doi:10.2741/896
Cairncross JG, Ueki K, Zlatescu MC, Lisle DK, Finkelstein DM, Hammond RR et al (1998) Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst 90:1473–1479. doi:10.1093/jnci/90.19.1473
Smith JS, Alderete B, Minn Y, Borell TJ, Perry A, Mohapatra G et al (1999) Localization of common deletion regions on 1p and 19q in human gliomas and their association with histological subtype. Oncogene 18:4144–4152. doi:10.1038/sj.onc.1202759
Aldape K, Burger PC, Perry A (2007) Clinicopathologic aspects of 1p/19q loss and the diagnosis of oligodendroglioma. Arch Pathol Lab Med 131:242–251
Reifenberger J, Reifenberger G, Liu L, James CD, Wechsler W, Collins VP (1994) Molecular genetic analysis of oligodendroglial tumors shows preferential allelic deletions on 19q and 1p. Am J Pathol 145:1175–1190
McDonald JM, See SJ, Tremont IW, Colman H, Gilbert MR, Groves M et al (2005) The prognostic impact of histology and 1p/19q status in anaplastic oligodendroglial tumors. Cancer 104:1468–1477. doi:10.1002/cncr.21338
Burger PC, Minn AY, Smith JS, Borell TJ, Jedlicka AE, Huntley BK et al (2001) Losses of chromosomal arms 1p and 19q in the diagnosis of oligodendroglioma, A study of paraffin-embedded sections. Mod Pathol 14:842–853. doi:10.1038/modpathol.3880400
Ueki K, Nishikawa R, Nakazato Y, Hirose T, Hirato J, Funada N et al (2002) Correlation of histology and molecular genetic analysis of 1p, 19q, 10q, TP53, EGFR, CDK4, and CDKN2A in 91 astrocytic and oligodendroglial tumors. Clin Cancer Res 8:196–201
Nigro JM, Takahashi MA, Ginzinger DG, Law M, Passe S, Jenkins RB et al (2001) Detection of 1p and 19q loss in oligodendroglioma by quantitative microsatellite analysis, a real-time quantitative polymerase chain reaction assay. Am J Pathol 158:1253–1262
Chahlavi A, Kanner A, Peereboom D, Staugaitis SM, Elson P, Barnett G (2003) Impact of chromosome 1p status in response of oligodendroglioma to temozolomide: preliminary results. J Neurooncol 61:267–273. doi:10.1023/A:1022580610598
Cairncross G, Berkey B, Shaw E, Jenkins R, Scheithauer B, Brachman D et al (2006) Phase III trial of chemotherapy plus radiotherapy compared with radiotherapy alone for pure and mixed anaplastic oligodendroglioma: Intergroup Radiation Therapy Oncology Group Trial 9402. J Clin Oncol 24:2707–2714. doi:10.1200/JCO.2005.04.3414
Brat DJ, Seiferheld WF, Perry A, Hammond EH, Murray KJ, Schulsinger AR et al (2004) Analysis of 1p, 19q, 9p, and 10q as prognostic markers for high-grade astrocytomas using fluorescence in situ hybridization on tissue microarrays from Radiation Therapy Oncology Group trials. Neuro-oncol 6:96–103. doi:10.1215/S1152851703000231
Schmidt MC, Antweiler S, Urban N, Mueller W, Kuklik A, Meyer-Puttlitz B et al (2002) Impact of genotype and morphology on the prognosis of glioblastoma. J Neuropathol Exp Neurol 61:321–328
Smith JS, Tachibana I, Passe SM, Huntley BK, Borell TJ, Iturria N et al (2001) PTEN mutation, EGFR amplification, and outcome in patients with anaplastic astrocytoma and glioblastoma multiforme. J Natl Cancer Inst 93:1246–1256. doi:10.1093/jnci/93.16.1246
Liu L, Backlund LM, Nilsson BR, Grander D, Ichimura K, Goike HM et al (2005) Clinical significance of EGFR amplification and the aberrant EGFRvIII transcript in conventionally treated astrocytic gliomas. J Mol Med 83:917–926. doi:10.1007/s00109-005-0700-2
Frederick L, Wang XY, Eley G, James CD (2000) Diversity and frequency of epidermal growth factor receptor mutations in human glioblastomas. Cancer Res 60:1383–1387
Wong AJ, Ruppert JM, Bigner SH, Grzeschik CH, Humphrey PA, Bigner DS et al (1992) Structural alterations of the epidermal growth factor receptor gene in human gliomas. Proc Natl Acad Sci USA 89:2965–2969. doi:10.1073/pnas.89.7.2965
Olson JJ, Barnett D, Yang J, Assietti R, Cotsonis G, James CD (1998) Gene amplification as a prognostic factor in primary brain tumors. Clin Cancer Res 4:215–222
Huncharek M, Kupelnick B (2000) Epidermal growth factor receptor gene amplification as a prognostic marker in glioblastoma multiforme: results of a meta-analysis. Oncol Res 12:107–112
Simmons ML, Lamborn KR, Takahashi M, Chen P, Israel MA, Berger MS et al (2001) Analysis of complex relationships between age, p53, epidermal growth factor receptor, and survival in glioblastoma patients. Cancer Res 61:1122–1128
Aldape KD, Ballman K, Furth A, Buckner JC, Giannini C, Burger PC et al (2004) Immunohistochemical detection of EGFRvIII in high malignancy grade astrocytomas and evaluation of prognostic significance. J Neuropathol Exp Neurol 63:700–707
Heimberger AB, Hlatky R, Suki D, Yang D, Weinberg J, Gilbert M et al (2005) Prognostic effect of epidermal growth factor receptor and EGFRvIII in glioblastoma multiforme patients. Clin Cancer Res 11:1462–1466. doi:10.1158/1078-0432.CCR-04-1737
Esteller M, Garcia-Foncillas J, Andion E, Goodman SN, Hidalgo OF, Vanaclocha V et al (2000) Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med 343:1350–1354. doi:10.1056/NEJM200011093431901
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. doi:10.1056/NEJMoa043330
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003. doi:10.1056/NEJMoa043331
Mikeska T, Bock C, El-Maarri O, Hubner A, Ehrentraut D, Schramm J et al (2007) Optimization of quantitative MGMT promoter methylation analysis using pyrosequencing and combined bisulfite restriction analysis. J Mol Diagn 9:368–381. doi:10.2353/jmoldx.2007.060167
Pollack IF, Hamilton RL, Sobol RW, Burnham J, Yates AJ, Holmes EJ et al (2006) O6-methylguanine-DNA methyltransferase expression strongly correlates with outcome in childhood malignant gliomas: results from the CCG-945 cohort. J Clin Oncol 24:3431–3437. doi:10.1200/JCO.2006.05.7265
Fruehauf JP, Brem H, Brem S, Sloan A, Barger G, Huang W et al (2006) In vitro drug response and molecular markers associated with drug resistance in malignant gliomas. Clin Cancer Res 12:4523–4532. doi:10.1158/1078-0432.CCR-05-1830
Walker MD et al (1978) Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial. J Neurosurg 49:333–343
Walker MD et al (1980) Randomized comparisons of radiotherapy and nitrosoureas for the treatment of malignant glioma after surgery. N Engl J Med 303:1323–1329
Sandberg-Wollheim M et al (1991) A randomized study of chemotherapy with procarbazine, vincristine, and lomustine with and without radiation therapy for astrocytoma grades 3 and/or 4. Cancer 68:22–29. doi:10.1002/1097-0142(19910701)68:1<22::AID-CNCR2820680105>3.0.CO;2-2
Bleehen NM, Stenning SP (1991) A Medical Research Council trial of two radiotherapy doses in the treatment of grades 3 and 4 astrocytoma, The Medical Research Council Brain Tumour Working Party. Br J Cancer 64:769–774
Nelson DF et al (1993) Hyperfractionated radiation therapy and bis-chlorethyl nitrosourea in the treatment of malignant glioma––possible advantage observed at 72.0 Gy in 1.2 Gy B.I.D. fractions: report of the Radiation Therapy Oncology Group Protocol 8302. Int J Radiat Oncol Biol Phys 25:193–207
Roa W et al (2004) Abbreviated course of radiation therapy in older patients with glioblastoma multiforme: a prospective randomized clinical trial. J Clin Oncol 22:1583–1588. doi:10.1200/JCO.2004.06.082
Phillips C et al (2003) A randomized trial comparing 35 Gy in ten fractions with 60 Gy in 30 fractions of cerebral irradiation for glioblastoma multiforme and older patients with anaplastic astrocytoma. Radiother Oncol 68:23–26. doi:10.1016/S0167-8140(03)00206-8
Ford JM et al (1997) A short fractionation radiotherapy treatment for poor prognosis patients with high grade glioma. Clin Oncol (R Coll Radiol) 9:20–24. doi:10.1016/S0936-6555(97)80053-2
Glinski B (1993) Postoperative hypofractionated radiotherapy versus conventionally fractionated radiotherapy in malignant gliomas, A preliminary report on a randomized trial. J Neurooncol 16:167–172. doi:10.1007/BF01324704
Prados MD et al (2001) Phase III trial of accelerated hyperfractionation with or without difluromethylornithine (DFMO) versus standard fractionated radiotherapy with or without DFMO for newly diagnosed patients with glioblastoma multiforme. Int J Radiat Oncol Biol Phys 49:71–77. doi:10.1016/S0360-3016(00)01458-9
Deutsch M et al (1989) Results of a randomized trial comparing BCNU plus radiotherapy, streptozotocin plus radiotherapy, BCNU plus hyperfractionated radiotherapy, and BCNU following misonidazole plus radiotherapy in the postoperative treatment of malignant glioma. Int J Radiat Oncol Biol Phys 16:1389–1396
Ludgate CM et al (1988) Superfractionated radiotherapy in grade III, IV intracranial gliomas. Int J Radiat Oncol Biol Phys 15:1091–1095
Shin KH et al (1985) Multiple daily fractionated radiation therapy and misonidazole in the management of malignant astrocytoma, A preliminary report. Cancer 56:758–760. doi:10.1002/1097-0142(19850815)56:4<758::AID-CNCR2820560410>3.0.CO;2-2
Fulton DS et al (1984) Misonidazole combined with hyperfractionation in the management of malignant glioma. Int J Radiat Oncol Biol Phys 10:1709–1712
Shin KH, Muller PJ, Geggie PH (1983) Superfractionation radiation therapy in the treatment of malignant astrocytoma. Cancer 52:2040–2043. doi:10.1002/1097-0142(19831201)52:11<2040::AID-CNCR2820521112>3.0.CO;2-K
Payne DG et al (1982) Malignant astrocytoma: hyperfractionated and standard radiotherapy with chemotherapy in a randomized prospective clinical trial. Cancer 50:2301–2306. doi:10.1002/1097-0142(19821201)50:11<2301::AID-CNCR2820501114>3.0.CO;2-J
Laperriere NJ et al (1998) Randomized study of brachytherapy in the initial management of patients with malignant astrocytoma. Int J Radiat Oncol Biol Phys 41:1005–1011. doi:10.1016/S0360-3016(98)00159-X
Selker RG et al (2002) The Brain Tumor Cooperative Group NIH Trial 87–01: a randomized comparison of surgery, external radiotherapy, and carmustine versus surgery, interstitial radiotherapy boost, external radiation therapy, and carmustine. Neurosurgery 51:343–355. doi:10.1097/00006123-200208000-00009 (discussion 355–357)
Souhami L et al (2004) Randomized comparison of stereotactic radiosurgery followed by conventional radiotherapy with carmustine to conventional radiotherapy with carmustine for patients with glioblastoma multiforme: report of Radiation Therapy Oncology Group 93–05 protocol. Int J Radiat Oncol Biol Phys 60:853–860. doi:10.1016/j.ijrobp.2004.04.011
Lee S et al (1999) Patterns of failure following high-dose 3-D conformal radiotherapy for high-grade astrocytomas: a quantitative dosimetric study. Int J Radiat Oncol Biol Phys 43:79–88. doi:10.1016/S0360-3016(98)00266-1
Massey V, Wallner K (1990) Patterns of second recurrence of malignant astrocytomas. Int J Radiat Oncol Biol Phys 18:395–398
Wallner K et al (1989) Patterns of failure following treatment for glioblastoma and anaplastic astrocytoma. Int J Radiat Oncol Biol Phys 16:1405–1409
Shapiro WR et al (1989) Randomized trial of three chemotherapy regimens and two radiotherapy regimens and two radiotherapy regimens in postoperative treatment of malignant glioma. Brain Tumor Cooperative Group Trial 8001. J Neurosurg 71:1–9
Kita M et al (1989) Radiotherapy of malignant glioma––prospective randomized clinical study of whole brain vs local irradiation. Gan no rinsho Jpn J Cancer Clin 35:1289–1294
Valtonen S, Timonen U, Toivanen P, Kalimo H, Kivipelto L, Heiskanen O, Unsgaard G, Kuurne T (1997) Interstitial chemotherapy with carmustine-loaded polymers for high grade gliomas: a randomized double-blind study. Neurosurgery 41:44–49. doi:10.1097/00006123-199707000-00011
Westphal M, Hilt DC, Bortey E, Delavault P, Olivares R, Warnke PC, Whittle IR, Jaaskelainen J, Ram Z (2003) A phase 3 trial of local chemotherapy with biodegradable carmistine (BCNU) wafers (Gliadel wafers) in patients with primary malignant gliomas. Neuro-oncol 5:79–88. doi:10.1215/15228517-5-2-79
Brandes AA, Vastola F, Basso U, Berti F, Pinna G, Rotilio A et al (2003) A prospective study on glioblastoma in the elderly. Cancer 97:657–662. doi:10.1002/cncr.11097
Chinot OL, Barrie M, Frauger E, Dufour H, Figarella-Branger D, Palmari J et al (2004) Phase II study of temozolomide without radiotherapy in newly diagnosed glioblastoma multiforme in an elderly populations. Cancer 100:2208–2214. doi:10.1002/cncr.20224
Glantz M, Chamberlain M, Liu Q, Litofsky NS, Recht LD (2003) Temozolomide as an alternative to irradiation for elderly patients with newly diagnosed malignant gliomas. Cancer 97:2262–2266. doi:10.1002/cncr.11323
Mukundan S, Holder CA, Olson JJ (2008) Neuroradiological assessment of newly diagnosed glioblastoma. J Neurooncol 89:259–269. doi:10.1007/s11060-008-9616-3
Ryken TC, Frankel B, Julien T, Olson JJ (2008) Surgical management of newly diagnosed glioblastoma in adults: role of cytoreductive surgery. J Neurooncol 89:271–286. doi:10.1007/s11060-008-9614-5
Brat DJ, Prayson RA, Ryken TC, Olson JJ (2008) Diagnosis of malignant glioma: role of neuropathology. J Neurooncol 89:287–311. doi:10.1007/s11060-008-9618-1
Bao S, Wu Q, McLendon RE, Hao Y, Shi Q, Hjelmeland AB et al (2006) Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature 444:756–760. doi:10.1038/nature05236
Singh SK, Hawkins C, Clarke ID, Squire JA, Bayani J, Hide T et al (2004) Identification of human brain tumour initiating cells. Nature 432:396–401. doi:10.1038/nature03128
Khwaja FW, Duke-Cohan JS, Brat DJ, Van Meir EG (2006) Attractin is elevated in the cerebrospinal fluid of patients with malignant astrocytoma and mediates glioma cell migration. Clin Cancer Res 12:6331–6336. doi:10.1158/1078-0432.CCR-06-1296
Khwaja FW, Nolen JD, Mendrinos SE, Lewis MM, Olson JJ, Pohl J et al (2006) Proteomic analysis of cerebrospinal fluid discriminates malignant and nonmalignant disease of the Central Nervous System and identifies specific protein markers. Proteomics 6:6277–6287. doi:10.1002/pmic.200600135
Phillips HS, Kharbanda S, Chen R, Forrest WF, Soriano RH, Wu TD et al (2006) Molecular subclasses of high-grade glioma predict prognosis, delineate a pattern of disease progression, and resemble stages in neurogenesis. Cancer Cell 9:157–173. doi:10.1016/j.ccr.2006.02.019
Nutt CL, Mani DR, Betensky RA, Tamayo P, Cairncross JG, Ladd C et al (2003) Gene expression-based classification of malignant gliomas correlates better with survival than histological classification. Cancer Res 63:1602–1607
Pomeroy SL, Tamayo P, Gaasenbeek M, Sturla LM, Angelo M, McLaughlin ME et al (2002) Prediction of Central Nervous System embryonal tumour outcome based on gene expression. Nature 415:436–442. doi:10.1038/415436a
Buatti J, Ryken R, Smith MC, Sneed P, Suh J, Mehta M, Olson JJ (2008) Radiation therapy of pathologically confirmed newly diagnosed glioblastoma in adults. J Neurooncol 89:313–337. doi:10.1007/s11060-008-9617-2
Fadul CE, Wen PY, Kim L, Olson JJ (2008) Cytotoxic chemotherapeutic management of newly diagnosed glioblastoma multiforme. J Neurooncol 89:339–357. doi:10.1007/s11060-008-9615-4
Quinn JA, Desjardins A, Weingart J et al (2005) Phase I trial of temozolomide plus O6-benzylguanine for patients with recurrent or progressive malignant glioma. J Clin Oncol 23:7178–7187. doi:10.1200/JCO.2005.06.502
Barvaux VA, Ranson M, Brown R et al (2004) Dual repair modulation reverses Temozolomide resistance in vitro. Mol Cancer Ther 3:123–127
Woolford LB, Southgate TD, Margison GP et al (2006) The P140K mutant of human O(6)-methylguanine-DNA-methyltransferase (MGMT) confers resistance in vitro and in vivo to temozolomide in combination with the novel MGMT inactivator O(6)-(4-bromothenyl)guanine. J Gene Med 8:29–34. doi:10.1002/jgm.816
Plummer R, Middleton M, Wilson R, et al. (2005) Final clinical, pharmacokinetic and pharmacodynamic results of the phase I study of the novel poly(ADP-ribose)polymerase (PARP) inhibitor, AGO14699, in combination with temozolomide AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics Abstr B268
Tentori L, Graziani G (2005) Chemopotentiation by PARP inhibitors in cancer therapy. Pharmacol Res 52(1):25–33. doi:10.1016/j.phrs.2005.02.010
Tentori L, Leonetti C, Scarsella M et al (2005) Brain distribution and efficacy as chemosensitizer of an oral formulation of PARP-1 inhibitor GPI 15427 in experimental models of CNS tumors. Int J Oncol 26:415–422
Weaver KD, Yeyeodu S, Cusack JC Jr, Baldwin AS Jr, Ewend MG (2003) Potentiation of chemotherapeutic agents following antagonism of nuclear factor kappa B in human gliomas. J Neurooncol 61:187–196. doi:10.1023/A:1022554824129
Nakanishi C, Toi M (2005) Nuclear factor-kappaB inhibitors as sensitizers to anticancer drugs. Nat Rev Cancer 5(4):297–309. doi:10.1038/nrc1588
Kesari S, Ramakrishna N, Sauvageot C, Stiles C, Wen PY (2006) Targeted molecular therapies for recurrent malignant glioma. Curr Oncol Rep 8:58–70. doi:10.1007/s11912-006-0011-y
Wen PY, Kesari S, Drappatz J (2006) Malignant gliomas: strategies to increase the effectiveness of targeted molecular treatment. Expert Rev Anticancer Ther 6:733–754. doi:10.1586/14737140.6.5.733
Goldbrunner RH, Bendszus M, Wood J, Kiderlen M, Sasaki M, Tonn JC (2004) PTK787/ZK222584, an inhibitor of vascular endothelial growth factor receptor tyrosine kinases, decreases glioma growth and vascularization. Neurosurgery 55:426–432
Herbst RS, Heymach JV, O’Reilly MS, Onn A, Ryan AJ (2007) Vandetanib (ZD6474): an orally available receptor tyrosine kinase inhibitor that selectively targets pathways critical for tumor growth and angiogenesis. Expert Opin Investig Drugs 16:239–249. doi:10.1517/13543784.16.2.239
Brockman J (1996) The third culture: beyond scientific revolution. Simon and Schuster, New York
Acknowledgements
The authors would like to acknowledge the editorial expertise of Emily Feinstein. Additionally, the authors wish to thank the individuals who directly participated in the writing of these guidelines in their original form: Chad Holder, Bruce Frankel, Terrance Julien, Richard A. Prayson, John Buatti, Mark C. Smith, Penny Sneed, John H. Suh, Minesh Mehta, Patrick Wen, and Lyndon Kim. We also wish to express appreciation to the AANS/CNS Joint Guidelines Committee for their review, comments and suggestions during the preparation of these guidelines in their original form.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Olson, J.J., Fadul, C.E., Brat, D.J. et al. Management of newly diagnosed glioblastoma: guidelines development, value and application. J Neurooncol 93, 1–23 (2009). https://doi.org/10.1007/s11060-009-9838-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-009-9838-z