Abstract
Introduction
The management of glioblastoma at the time of progression is an important facet of all physicians involved in neuro-oncology. This is an update of the evidence-based guidelines for management of progressive glioblastoma published by the Congress of Neurological Surgeons and American Association of Neurological Surgeons in 2014.
Methods
The medical literature from July 1, 2012 through March 31, 2019 was searched in MEDLINE® and Embase® and the Cochrane Database of Systematic Reviews, Cochrane Controlled Trials Registry, and Cochrane Database of Abstracts of Reviews of Effects to determine if information was available to update, modify or create new recommendations related to imaging, cytoreductive surgery, neuropathology, radiotherapy, cytotoxic chemotherapy, targeted therapy, and immunotherapy.
Results
The writing group utilized the information from the updated literature search to formulate recommendations that were exclusively evidence based and not founded on potentially biased consensus or expert opinion.
Conclusion
The series of guideline documents provides an update of the information and recommendations that could be derived in the 2014 version. It sets a benchmark as to what we really know about the management of this difficult disease. It also provides clues to key investigations that are necessary to move us toward truly effective disease control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background and rationale
The guidelines for the management of progressive glioblastomas sponsored by the Congress of Neurological Surgeons (CNS) and American Association of Neurological Surgeons (AANS) were published in 2014 [1,2,3,4,5,6,7]. As suggested by the Institute of Medicine, now the National Academy of Medicine, it is suggested that guidelines be updated in the range of every 5 years [8]. That interval allows for a reasonable time to assess new methods of diagnosis and treatment such as imaging, surgical intervention, use of targeted therapy and immunotherapy, and radiation therapy that were just coming on line at the time of the publication in 2014 [9,10,11,12].
Progression of glioblastoma after initial therapy usually occurs within months, and in nearly every case within a few years. Thus, this set of guideline documents will be of value to all medical specialties dealing with glioblastoma.
Using the same topics the initial set of guidelines published in 2014, these guidelines are presented as a set of documents separated by management area, thus addressing the role of imaging, cytoreductive surgery, neuropathology, radiation therapy, cytotoxic chemotherapy and utilization of targeted agents including immunotherapy. Rather than having a section on just targeted therapy as in 2014, the panelists chose to expand this section to targeted therapy and immunotherapy. These guidelines are produced using the evidence-based methodology supported by the Joint Guidelines Committee of the American Association of Neurological Surgeons (AANS) and Congress of Neurological Surgeons (CNS).
Objectives and guideline panel development
The overall objective of this series of guideline documents is to confirm or update the previous evidence-based recommendations for the management of patients with progressive glioblastoma centering on questions related to the most commonly used diagnostic and treatment modalities. The most important step in accomplishing this goal is a systematic update of the reviews of the literature utilized in the first set of publications. The Joint Tumor Section of the AANS/CNS recruited representatives from neurosurgery, radiation oncology, medical neuro-oncology, neuropathology, and neuroradiology to form a multi-disciplinary clinical panel of 12 experts who developed the evidence-based practice guidelines from the systematic review results (Table 1). The primary consequence of this work will ideally be to point out the current state of knowledge about the management of this disease process and serve as a point of departure for the development of diagnostic and treatment improvements for patients with this diagnosis.
Methods
Topical range of the systematic review and clinical practice guidelines
The questions to be answered about the treatment of progressive glioblastoma to be addressed by the systematic literature review were determined by the clinical panel. These questions are presented at the beginning of each guideline section of which there are six in all. This includes questions about diagnostic imaging, cytoreductive surgery, tumor tissue evaluation by neuropathology, radiation therapy, cytotoxic chemotherapy and targeted therapy and immunotherapy.
Literature examination approach
A broad literature search strategy was undertaken to identify all citations relevant to the management of progressive glioblastoma since the end of the search period used for the 2014 guideline publication, i.e., June 30, 2012. Thus, the MEDLINE® and Embase® electronic databases were searched from July 1, 2012 through March 31, 2019 with additional data being gleaned from the Cochrane Database of Systematic Reviews, Cochrane Controlled Trials Registry, and Cochrane Database of Abstracts of Reviews of Effects as appropriate. The search strategy used a combination of subheadings and text words. Reference lists from the publications that met inclusion criteria were also screened for potentially relevant studies.
Study selection, quality assessment and statistical methods
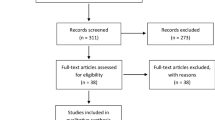
The search of the bibliographic databases identified possibly relevant citations. Two authors evaluated titles and abstracts using eligibility criteria as defined for each section’s topic. Cases of disagreement about pertinence were resolved by a third author when needed. The full text articles of the selected abstracts were collected, and the same process was applied again. Articles that met the eligibility criteria for one or more of the questions were grouped according to the questions they addressed. Reasons for exclusion were documented. The eligibility criteria for each of the questions are documented in the individual clinical practice guideline papers in this series.
Publications which met the eligibility criteria had their data extracted by one reviewer and the extracted information was checked by a second reviewer. Evidence and summary tables, reporting the extracted study information and evidence classification, were generated for the included studies for each of the questions. The literature in the evidence tables was expanded upon in the scientific foundation of each section to emphasize important points supporting its classification and contribution to recommendations.
AANS/CNS evidence classes and levels of recommendations
Both the evidence classification and the strength of the recommendations for therapeutic effectiveness were graded according to standardized AANS/CNS criteria (Table 2). The class of evidence assigned to each study was based on study design (i.e., class I, II, or III). The strength of the recommendations made (i.e., level 1, 2, or 3) was directly linked to the evidence classification and took into account aspects of study quality and whether or not the plan was accomplished, not just study design. Specifically, the class of evidence and subsequently the level of a recommendation made could be decreased, based on consensus input, if there were methodological concerns regarding the studies used as evidence. A summary of the methodology used for the development of this evidence-based update, including techniques for classification of data and its linkage to recommendations, can be found at https://www.cns.org/guidelines/guideline-development-methodology.
Guideline panel consensus and practice guideline approval process
Writing groups were created from the entire clinical guideline panel based on expertise to address each of the disciplines and areas of therapy chosen to be part of this set of clinical guidelines. Each group was involved with literature selection, creation and editing of the evidence/summary tables for their specific discipline. Evidence tables were created with most recent data first and subsequent listings in retrograde chronological order. The table headings consisted of first author name, journal and year, followed by a brief study description, chosen data class and conclusion. The authors were directed to craft the data in the tables in a succinct and fact filled manner to allow for understanding of the literature entry. Each piece of literature cited in the table is discussed in greater detail in the scientific foundation with more information regarding choice of classification to be noted in this location. Using this information, the writing groups then drafted the clinical practice guideline for their respective discipline. The draft guidelines were then circulated to the entire clinical guideline panel to allow for multidisciplinary feedback, discussion, and ultimately approval.
The completed updates of the evidence-based clinical practice guidelines on the management of progressive glioblastoma were presented to the Joint Guidelines Review Committee (JGRC) of the AANS/CNS to assess methodology, content, and conclusions. The reviewers for the JGRC were vetted by Neurosurgery for suitability and expertise to serve as reviewers for the purposes of publication in that journal also.
Development of this set of evidence-based clinical practice guidelines was editorially independent from the funding agencies. The funding agencies (AANS Board, CNS Executive Committee, and AANS/CNS Joint Tumor Section Executive Committee) review of these guideline papers, following JGRC approval but prior to submission for publication, and their role was limited to whether or not to endorse or reject this body of work. Figure 1 provides an outline of the key steps in the process of developing these clinical practice guidelines.
Conclusion
This series of guidelines was constructed primarily to update the currently existing evidence for management of progressive glioblastoma in a manner that sets a benchmark for further improvement in this task. By designing future investigations to provide high quality evidence overcoming prior weaknesses and limitations noted in these guidelines’ advancement toward a remedy of this disease will be achieved. Secondarily, the guideline recommendations provided are set forth for conscientious use by the practicing physician who must take into account all of the unique aspects of a given individuals condition and illness before applying them. The application of published guidelines information is an activity that results in strong and often polarized opinions. The guidelines presented in this current project are not meant to resolve these issues and it is unlikely that any could accomplish such a goal. Fortunately, new research is constantly underway, and these guidelines are meant to be updated in five years with earlier updates should important, practice changing new evidence be published.
Data availability
The author has ensured all data and materials as well as software applications or custom code supports their published claims and comply with field standards.
References
Olson JJ, Ryken TC, Kalkanis SN (2014) The management of progressive glioblastoma: a systematic review and evidence-based clinical practice guideline: introduction and rationale. J Neuro-oncol 118:429–434. https://doi.org/10.1007/s11060-013-1329-6
Ryken CR, Aygun N, Morris J, Schweizer M, Nair R, Spracklen C, Kalkanis SH, Olson JJ (2014) The role of imaging in the management of progressive glioblastoma. J Neuro-oncol 118:435–460. https://doi.org/10.1007/s11060-013-1330-0
Brat DJ, Ryken TC, Kalkanis SN, Olson JJ (2014) The role of neuropathology in the management of progressive glioblastoma. J Neuro-oncol 118:461–478. https://doi.org/10.1007/s11060-013-1331-z
Ryken TC, Kalkanis SN, Buatti JM, Olson JJ (2014) The role of cytoreductive surgery in the management of progressive glioblastoma. J Neuro-oncol 118:479–488. https://doi.org/10.1007/s11060-013-1336-7
Ryu S, Buatti JM, Morris A, Kalkanis SN, Ryken TC, Olson JJ (2014) The role of radiotherapy in the management of progressive glioblastoma. J Neuro-oncol 118:489–499. https://doi.org/10.1007/s11060-013-1337-6
Olson JJ, Nayak L, Ormond DR, Wen PY, Kalkanis SN (2014) The role of cytotoxic chemotherapy in the management of progressive glioblastoma. J Neuro-oncol 118:501–555. https://doi.org/10.1007/s11060-013-1338-5
Olson JJ, Nayak L, Ormond DR, Wen PY, Kalkanis SN (2014) The role of targeted therapies in the management of progressive glioblastoma. J Neuro-oncol 118:557–599. https://doi.org/10.1007/s11060-013-1339-4
The National Acadamies of Science Engineering Medicine (2011) Clinical practice guidelines we can trust. https://www.nap.edu/catalog/13058/clinical-practice-guidelines-we-can-trust. Accessed July 26, 2021. https://doi.org/10.17226/13058
Strauss SB, Meng A, Ebani EJ, Chiang GC (2019) Imaging glioblastoma posttreatment: progression, pseudoprogression, pseudoresponse. Radiation Necrosis Radiol Clin North Am 57:1199–1216. https://doi.org/10.1016/j.rcl.2019.07.003
Schipmann S, Schwake M, Suero Molina E, Stummer W (2019) Markers for identifying and targeting glioblastoma cells during surgery. J Neurol Surg 80:475–487. https://doi.org/10.1055/s-0039-1692976
Le Rhun E, Preusser M, Roth P et al (2019) Molecular targeted therapy of glioblastoma. Canc Treatment Rev Fecci PI, Sampson JH (2019) The current state of immunotherapy for gliomas: an eye toward the future. J Neurosurg 131:657–666. https://doi.org/10.1016/j.ctrv.2019.101896
Cao Y, Tseng CL, Balter JM, Teng F, Parmar HA, Sahgal A (2017) MR-guided radiation therapy: transformative technology and its role in the central nervous system. Neuro-Oncol 19(2):16–29. https://doi.org/10.1093/neuonc/nox006
Acknowledgements
The guidelines task force would like to acknowledge the Congress of Neurological Surgeons Guidelines Committee for their contributions throughout the development of the guideline, and the American Association of Neurological Surgeons/Congress of Neurological Surgeons Joint Guidelines Review Committee for their review, comments, and suggestions throughout peer review, as well as the contributions of Trish Rehring, MPH, CHES, Senior Manager of Clinical Practice Guidelines for the CNS, and Mary Bodach, MLIS, from the Congress of Neurological Surgeons Guidelines Office for organizational assistance and reference librarian services, respectively as well as Jeremy Kupsco, PhD, Informationist, Emory University, for their valuable input as Medical Research Librarians. Throughout the review process, the reviewers and authors were blinded from one another. At this time the guidelines task force would like to acknowledge the following individual peer reviewers for their contributions: John O’Toole, MD, Brian Howard, MD, Jamie Van Gompel, MD, Howard Silberstein, MD, Navid Redjal, MD and Shawn Hervey-Jumper, MD.
Funding
These guidelines were funded exclusively by the Congress of Neurological Surgery and the Joint Section on Tumors of the Congress of Neurological Surgeons and the American Association of Neurological Surgeons, which received no funding from any outside commercial sources to support the development of this document.
Author information
Authors and Affiliations
Contributions
The author listed on this publication agrees with the content included and gives explicit consent to the submission of this publication. The author obtained consent from the responsible authorities at the institute/organization where the work has been carried out, before the work was submitted. The author whose name appear on the submission: (1) made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; (2) drafted the work or revised it critically for important intellectual content; (3) approved the version to be published; and (4) agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Jeffrey J. Olson has no conflict of interest. All Guideline Task Force members were required to disclose all potential COIs prior to beginning work on the guideline, using the COI disclosure form of the AANS/CNS Joint Guidelines Review Committee. The CNS Guidelines Committee and Guideline Task Force Chair reviewed the disclosures and either approved or disapproved the nomination and participation on the task force. The CNS Guidelines Committee and Guideline Task Force Chair may approve nominations of task force members with possible conflicts and restrict the writing, reviewing, and/or voting privileges of that person to topics that are unrelated to the possible COIs. To reiterate, the authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this series of articles.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sponsors: Congress of Neurological Surgeons (CNS) and the Section on Tumors.
Endorsement: Reviewed for evidence-based integrity and endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons.
Rights and permissions
About this article
Cite this article
Olson, J.J. Congress of Neurological Surgeons systematic review and evidence-based guidelines for the treatment of adults with progressive glioblastoma update: introduction and methods. J Neurooncol 158, 133–137 (2022). https://doi.org/10.1007/s11060-021-03850-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-021-03850-3