Abstract
The prognosis of patients with primary central nervous system lymphoma (PCNSL) has improved in recent years. This has partly been achieved by remission induction protocols incorporating high-dose methotrexate (HD-MTX) and rituximab. Given the high rates of relapse, consolidation therapy is usually considered in first response. Whole brain radiotherapy may prolong PFS but appears to confer no long-term survival advantage and is associated with significant neurocognitive dysfunction. Attempts to improve efficacy and reduce neurotoxicity of consolidation therapy have included thiotepa-based high-dose chemotherapy and autologous stem cell transplant (HDC-ASCT). This multi-centre, retrospective study reports the outcome of 70 patients undergoing HDC-ASCT for PCNSL in the United Kingdom. The median age at diagnosis was 56 years and all patients received HD-MTX-containing induction regimens. All patients underwent HDC-ASCT in first response. The rate of complete response increased from 50% before HDC-ASCT to 77% following HDC-ASCT. Treatment-related mortality was 6%. At a median follow-up of 12 months from HDC-ASCT, the estimated 1- and 2-year PFS rates were 71.5% and overall survival 86.4% and 83.3%, respectively. These data are comparable to published studies of HDC-ASCT for PCNSL, supporting its feasibility and efficacy.
Similar content being viewed by others
Introduction
The prognosis of patients with primary central nervous system lymphoma (PCNSL) has continued to improve with further development of effective CNS penetrating chemotherapy regimens. Consolidation therapy has typically been employed following remission induction given the high risk of relapse and the recognition that optimal dose intensity is compromised by impeded drug delivery across the blood–brain barrier.1 Combination chemotherapy regimens that include high-dose methotrexate (HD-MTX) are the now accepted standard of care for remission induction.2, 3 The addition of rituximab and blood–brain barrier-penetrating alkylating agents including thiotepa to induction regimens has been associated with improved outcomes.3, 4, 5 Whether and how to use consolidation therapy has been more controversial.6 For patients treated with the more intensive induction protocols, three principal consolidation approaches have been described: whole brain radiotherapy (WBRT),2 non-myeloablative chemotherapy5 or high-dose chemotherapy and autologous stem cell transplant (HDC-ASCT).7 Consolidation with chemotherapy, either myeloablative or non-myeloablative, is an attractive option given the high risks of delayed neurotoxicity following WBRT after HD-MTX-containing chemotherapy.8, 9 This is particularly relevant given the median age of patients diagnosed with PCNSL is >60 years, representing a cohort of patients for whom radiation-induced neurocognitive dysfunction is a greater risk, yet many are physiologically fit enough for intensive chemotherapy approaches. The promising efficacy of thiotepa-based HDC-ASCT has been reported in several retrospective and prospective studies from Europe,7, 10 United States11 and Asia,12 whereas traditional conditioning protocols, such as ‘BEAM’ (carmustine, etoposide, cytarabine and melphalan), are considered inadequate for CNS disease.13 Accordingly, many transplant centres in the United Kingdom have undertaken thiotepa-based HDC-ASCT as consolidation treatment for patients with PCNSL. This retrospective, multicentre study describes the outcomes of patients who underwent thiotepa-based HDC-ASCT for PCNSL in the United Kingdom.
Subjects and methods
Patient selection and data collection
This study was conducted as a service evaluation, as HDT-ASCT has been used as a standard treatment in UK transplant centres; therefore, specific patient consent was not sought. UK PCNSL centres were invited to participate and 13 institutions responded to confirm that they had performed ASCT for this indication. Patients were identified from local bone marrow transplant databases. Data were collected on an electronic data sheet with pre-specified variables. Anonymised data analysis was performed centrally. Patients were eligible if they had a biopsy proven diagnosis of PCNSL of diffuse large B-cell lymphoma histology and had undergone a thiotepa-conditioned HDC-ASCT for PCNSL in first response, together with a minimum data set. We specified a minimum follow-up period of 3 months following HDC-ASCT together with the results of a post-HDC-ASCT contrast-enhanced magnetic resonance imaging scan.
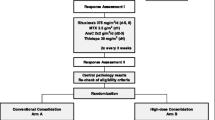
Response evaluation
Response to treatment was evaluated at individual centres by local neuroradiologists using contrast-enhanced magnetic resonance imaging. Response was assessed using the International Workshop to Standardise Baseline Evaluation and Response Criteria for PCNSL.14
Definitions and statistical analysis
The primary outcome measures were overall response rate, PFS and overall survival (OS) following HDC-ASCT. Given this was not a prospective study and adverse events were not consistently recorded or graded, we elected to evaluate other clinically important surrogates of response and tolerability, such as cytopenias, length of hospital stay and need for intensive care support. The data cutoff date was 1 July 2016. PFS was measured from the date of HDC-ASCT to the date of disease progression, relapse or death from any cause. OS was measured from the date of HDC-ASCT to the date of death from any cause. Statistical analysis was performed using GraphPad PRISM version 5 (GraphPAD Software, San Diego, CA, USA). The Kaplan–Meier method was used to construct PFS and OS curves. Neutrophil engraftment following HDC-ASCT was defined as a neutrophil count >1.0 × 109/l (either with or without granulocyte colony stimulating factor) and platelet count >20 × 109/l, unsupported by platelet transfusions.
Results
Patient characteristics
Thirteen participating centres submitted data on 76 cases for analysis. Six cases were excluded: three due to non-diffuse large B-cell lymphoma histology and three due to unavailability of a post-HDC-ASCT magnetic resonance imaging scan. Thus, 70 patients were included in the final analysis. Patient characteristics at diagnosis are shown in Table 1. Patients were diagnosed between January 2008 and February 2016. The median age at diagnosis was 56 (range 27–74) years. All had diffuse large B-cell lymphoma histology with one patient having concurrent retinovitreal involvement. Three patients had developed PCNSL in the setting of HIV infection, two had evidence of viraemia with low CD4 counts at PCNSL diagnosis (21 cells/μl and 165 cells/μl), whereas one patient had well-controlled HIV infection on anti-retroviral therapy, with an undetectable viral load and a CD4 count of 1046 cells/μl. All patients received anti-retroviral therapy during induction chemotherapy and were adherent to anti-retroviral therapy at the time of ASCT with suppressed viral loads. At PCNSL diagnosis, 49% of our cohort had an Eastern Cooperative Oncology Group (ECOG) performance score of ⩾2.15
All patients received HD-MTX-containing regimens as remission induction with 87% and 51% of patients also receiving high-dose cytarabine and rituximab, respectively, as part of the treatment regimen. One patient received concurrent intravitreal methotrexate as part of induction chemotherapy, indicated for retino-vitreal involvement. Thirteen patients included in this analysis were treated within the International Extranodal Lymphoma Study group 32 study protocol.3 Thirteen patients received HD-MTX, cytarabine, thiotepa and rituximab as induction either within, or following, the International Extranodal Lymphoma Study group 32 study.3
Response to first-line treatment
Response to treatment is outlined in Table 2. The overall response rate to induction chemotherapy was 93% with 47% of patients achieving a complete response (CR)/CR unconfirmed (CRu). Five patients with progressive disease went on to receive second-line treatment: three were treated with chemotherapy (ifosphamide, etoposide and rituximab16 n=2 and MTX, cytarabine, thiotepa and rituximab n=1) and two with WBRT. All five patients had a response to salvage treatment with two achieving a CR/CRu and three achieving a PR.
High-dose chemotherapy and autologous stem cell transplant
Patient characteristics immediately before HDC-ASCT are shown in Table 1. The median age was 56 years and, notably, 31% of patients were ⩾65 years. Characteristics of the HDC-ASCT are shown in Table 3. All patients received thiotepa as part of the conditioning regimen. For most (60%), the total dose of thiotepa was 10 mg/kg, whereas 37% received 20 mg/kg. The vast majority of patients (96%) received carmustine alongside thiotepa for ASCT conditioning.
All patients achieved haematopoietic regeneration; the median time to neutrophil and platelet engraftment were 11 and 13 days, respectively. This was not significantly different between the different conditioning regimens. The median number of days spent in hospital was 22 (range 16–265 days) with 16 patients (23%) spending 30 days or more in hospital. Five patients (7%) required admission to the intensive care unit.
Seven patients proceeded to WBRT following the HDC-ASCT (one patient in CR, two in PR and four with PD). Sixty-seven patients were evaluable for response following HDC-ASCT (three patients died before response assessment). Magnetic resonance imaging was performed at a median of 84 days post stem cell infusion. Response data are shown in Table 2. The rate of CR/CRu increased from 50% pre- to 77% post HDC-ASCT. We did not observe a significant association between the final CR/CRu rate post HDC-ASCT and the dose of thiotepa received in this cohort (CR rate of 79% vs 77% in the 10 and 20 mg groups, respectively).
Treatment-related mortality
Four (6%) patients died of treatment-related causes. This included two deaths from neutropenic sepsis at D+17 (HIV-positive patient with hepatitis C infection and cirrhosis) and D+31 post HDC-ASCT, one from acute respiratory distress syndrome at D+28 and one from neurotoxicity on a background of epilepsy and chest infection at D+124. Age ⩾65 years was not associated with risk of treatment-related death. All four who died received a total thiotepa dose of 20 mg/kg.
PFS and OS
At the time of data analysis, the median follow-up of living patients from diagnosis was 20 months (range 5–98 months) and 12 months from HDC-ASCT (range 2–90 months). Twelve (17%) patients have relapsed; 10 with lymphoma confined to the CNS and 2 with systemic lymphoma relapse (1 patient with testicular diffuse-large B-cell lymphoma, who subsequently achieved a second CR). Twelve (17%) patients have died (four from treatment). Seven patients have died of PCNSL. One patient died of bronchopneumonia 18 months post HDC-ASCT, which was neither treatment nor disease related.
The median PFS and OS from HDT-ASCT have not been reached. Representative Kaplan–Meier curves are shown in Figure 1. The estimated 1-, 2- and 5-year PFS are 71.5% (95% confidence interval (CI) 57.9–81.4), 71.5% (95% CI 57.9–81.4) and 66.4% (95% CI 49.7–78.6), respectively. The estimated 1, 2 and 5 year OS from diagnosis are 86.4% (95% CI 74.5–93), 83.3% (95% CI 69.6–91.1) and 78.4 (95% CI 61–88.7), respectively.
Discussion
A number of retrospective and prospective studies7, 11, 17 have demonstrated the feasibility and efficacy of HDC-ASCT as consolidation treatment for patients with PCNSL. The rationale for HDC-ASCT in this context is that dose intensification of CNS-penetrating drugs will result in higher concentrations in brain tissue and CSF. This is uniquely important in PCNSL given the challenges of drug delivery across the blood–brain barrier with conventional dose chemotherapy and could potentially overcome drug resistance. This large retrospective, multi-centre study is the first from the United Kingdom to report outcomes following thiotepa-based HDC-ASCT in patients with PCNSL.
This study has the limitations inherent to any retrospective analysis including heterogeneous induction chemotherapy regimens and no data on the intention to treat population; that is, patients for whom HDC-ASCT was intended but never realised. Nonetheless, these data demonstrate a high overall response rate of 87% following HDC-ASCT with a significant improvement in CR/CRu from 50% to 77% post HDC-ASCT. Follow-up is relatively short, as most patients (69%) were diagnosed from 2013 onwards. However, the 1- and 2-year PFS and OS are favourable at 71.5/71.5% and 86.4%/83.3%, respectively. Importantly, a follow-up period of 20 months from diagnosis is meaningful given that most relapses following HDC-ASCT occur in the first 18 months.7, 11 Notably, 7 patients with follow-up >5 years are alive and disease-free. These survival outcomes are comparable to published data from prospective studies.
The largest, prospective phase II study of HDC-ASCT in 79 newly diagnosed patients (aged 65 years and under) with PCNSL reported an overall response rate of 91% with the rate of CR increasing from 22.8 to 77.2% following HDC-ASCT using thiotepa (20 mg/kg) and carmustine (400 mg/m2) conditioning.7 At a median follow-up of 57 months, the median PFS was 74 months but the median OS was not reached. There does not appear to be a plateau in the survival curves, suggesting that relapse is an ongoing risk. In this study, patients with progressive disease were eligible for HDC-ASCT; seven such patients achieved PR or CR following HDC-ASCT of whom four remained alive at the time of analysis. This underscores an important and well-described principle of HDC-ASCT in PCNSL,18 that patients who fail to respond to standard chemotherapy do not necessarily have chemotherapy-resistant disease and derive meaningful benefit from dose-intensified CNS-penetrating chemotherapy. A smaller prospective study in 26 patients with newly diagnosed PCNSL reported an improved in CR rate from 69 to 81% following HDC-ASCT.11 This study used thiotepa, busulphan and cyclophosphamide, as ASCT conditioning. With a median follow-up of 45 months, the 1 and 2 year estimated PFS rates were 82% and 79%, respectively, with no progressions or deaths occurring beyond 2 years. The 1- and 2-year OS were 88% and 81%, respectively.11
The treatment-related mortality of 6% within our cohort is comparable to that reported in the literature. A notable proportion (31%) of patients were ⩾65 years and some patients ⩾70 years (n=6), who would typically be excluded from clinical trials of HDC-ASCT. The reported risk of transplant-related mortality using carmustine/thiotepa-conditioning ranges from 2 to 5%.7, 10 Published protocols have used differing total doses of thiotepa; in our UK cohort, most patients received either 10 or 20 mg/kg total dose. Interesting, all four treatment-related deaths occurred in the group that received 20 mg/mg dose of thiotepa. Other conditioning regimens have been studied, most commonly thiotepa, busulphan and cyclophosphamide. Although numbers of patients included in studies using thiotepa, busulphan and cyclophosphamide conditioning are small, the reported treatment-related mortality appears to be higher, in the region of 12–14%.11, 19, 20 Our study also included three patients with HIV infection. One patient died of complications of neutropenic sepsis, but had other comorbidities including hepatitis C-associated cirrhosis.21 The other two are alive and disease free at 50 and 18 months, respectively, post HDC-ASCT. The optimal thiotepa dose within HDC-ASCT protocols for PCNSL remains unclear; comparative data are lacking and further study is warranted.
Our study includes an older population of patients compared with published studies with the oldest patient being 75 years at the time of HDC-ASCT. Age at the time of HDC-ASCT was not significantly associated with risk of treatment-related death. The four patients who died of treatment-related complications were aged 32, 36, 65 and 66 years. The oldest patient included in the largest prospective study of HDC-ASCT was 62 years.7 However, in a retrospective study of 105 patients with PCNSL treated with carmustine/thiotepa-conditioned ASCT, patients up to the age of 70 years were included, with an overall treatment-related mortality of 2.8%.10 Together with our data, this supports the feasibility of HDC-ASCT in older patients; chronological age per se should not be regarded as a barrier.
Aside from HDC-ASCT, other strategies for consolidation include WBRT and non-myeloablative chemotherapy. WBRT at conventional doses (36–45 Gy) confers a significant risk of potentially disabling, delayed neurotoxicity.8, 22 A single randomised study attempted to address whether consolidation WBRT (45 Gy) improved OS following induction chemotherapy, as compared with chemotherapy alone. Although these data have been widely debated and criticised, the study concluded that the addition of WBRT may prolong PFS but not OS.23 Results of the second randomisation of the International Extranodal Lymphoma Study group 32 study, which compared WBRT (36±9 Gy) and HDC-ASCT as consolidation therapy following HD-MXT-based induction, have been reported in abstract form. At a median follow-up of 40 months, there is no significant difference in the primary end point of 2-year PFS between the two consolidation arms. Both treatments were equally effective at increasing the CR rate after induction from 54 to 95% after WBRT and from 53 to 93% after HDC-ASCT.24
In an attempt to mitigate the risk of delayed neurotoxicity, lower dose WBRT (23.4 Gy) has been investigated as consolidation following induction chemotherapy. In a study of 52 patients with newly diagnosed PCNSL treated with chemotherapy and low-dose radiotherapy, the median PFS and OS were 3.3 and 6.6 years, respectively, at a median follow-up of 5.6 years. In the 12 patients that underwent evaluation for neurotoxicity at a single centre, there was no decline in cognitive function.4 However, it should be noted that the most favourable outcomes with low-dose WBRT in this study were seen in younger patients who achieved CR with induction chemotherapy. An alternative approach to consolidation has been investigated by the CALGB group, employing intensive non-myeloablative chemotherapy with etoposide and cytarabine following HD-MTX-based induction. With a median follow-up of 4.9 years, the median PFS was 2.4 years and the median OS has not been reached.5 We await with interest the results of three further randomised studies that are examining the efficacy of HDC-ASCT compared with either non-myeloablative chemotherapy (NCT01511562 and NCT02531841) or WBRT (NCT00863460).
The attraction of myeloablative or non-myeloablative chemotherapy as consolidation treatment is the perceived reduction of associated long-term neurotoxicity as compared with WBRT.9 However, formal prospective neuropsychological testing following HDC-ASCT has only been reported in two studies11, 24 with results of other large randomised studies awaited. In studies that have evaluated cognitive function and quality of life following HDC-ASCT, there did not appear to be any significant neurotoxicity and quality of life after HDC-ASCT improved.7, 11 In the International Extranodal Lymphoma Study group 32 study mentioned above, neuropsychological tests showed a significant impairment of attention/executive functions and late verbal memory among patients treated with WBRT, whereas patients treated with ASCT exhibited improvement in most cognitive functions and quality of life.24
In conclusion, this study reports favourable outcomes, comparable to published data, for patients with PCNSL following HDC-ASCT. Most patients avoided WBRT and therefore may be spared from the greatest risk of treatment-related neurocognitive decline. This study describes the use of HDC-ASCT in UK transplant centres and demonstrates its feasibility and efficacy.
References
Phillips EH, Fox CP, Cwynarski K . Primary CNS lymphoma. Curr Hematol Malig Rep 2014; 9: 243–253.
Ferreri AJ, Reni M, Foppoli M, Martelli M, Pangalis GA, Frezzato M et al. High-dose cytarabine plus high-dose methotrexate versus high-dose methotrexate alone in patients with primary CNS lymphoma: a randomised phase 2 trial. Lancet 2009; 374: 1512–1520.
Ferreri AJ, Cwynarski K, Pulczynski E, Ponzoni M, Deckert M, Politi LS et al. Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and rituximab (MATRix regimen) in patients with primary CNS lymphoma: results of the first randomisation of the International Extranodal Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol 2016; 3: e217–e227.
Morris PG, Correa DD, Yahalom J, Raizer JJ, Schiff D, Grant B et al. Rituximab, methotrexate, procarbazine, and vincristine followed by consolidation reduced-dose whole-brain radiotherapy and cytarabine in newly diagnosed primary CNS lymphoma: final results and long-term outcome. J Clin Oncol 2013; 31: 3971–3979.
Rubenstein JL, Hsi ED, Johnson JL, Jung SH, Nakashima MO, Grant B et al. Intensive chemotherapy and immunotherapy in patients with newly diagnosed primary CNS lymphoma: CALGB 50202 (Alliance 50202). J Clin Oncol 2013; 31: 3061–3068.
Rubenstein JL, Gupta NK, Mannis GN, LaMarre AK, Treseler P . How I treat CNS lymphomas. Blood 2013; 122: 2318–2330.
Illerhaus G, Kasenda B, Ihorst G, Egerer G, Lamprecht M, Keller U et al. High-dose chemotherapy with autologous haemopoietic stem cell transplantation for newly diagnosed primary CNS lymphoma: a prospective, single-arm, phase 2 trial. Lancet Haematol 2016; 3: e388–e397.
Correa DD, DeAngelis LM, Shi W, Thaler H, Glass A, Abrey LE . Cognitive functions in survivors of primary central nervous system lymphoma. Neurology 2004; 62: 548–555.
Doolittle ND, Korfel A, Lubow MA, Schorb E, Schlegel U, Rogowski S et al. Long-term cognitive function, neuroimaging, and quality of life in primary CNS lymphoma. Neurology 2013; 81: 84–92.
Schorb E, Kasenda B, Atta J, Kaun S, Morgner A, Hess G et al. Prognosis of patients with primary central nervous system lymphoma after high-dose chemotherapy followed by autologous stem cell transplantation. Haematologica 2013; 98: 765–770.
Omuro A, Correa DD, DeAngelis LM, Moskowitz CH, Matasar MJ, Kaley TJ et al. R-MPV followed by high-dose chemotherapy with TBC and autologous stem-cell transplant for newly diagnosed primary CNS lymphoma. Blood 2015; 125: 1403–1410.
Cho H, Chang JH, Kim YR, Kim SJ, Chung H, Park H et al. The role of upfront autologous stem cell transplantation in high-risk younger patients with primary central nervous system lymphoma. Br J Haematol 2016; 174: 444–453.
Abrey LE, Moskowitz CH, Mason WP, Crump M, Stewart D, Forsyth P et al. Intensive methotrexate and cytarabine followed by high-dose chemotherapy with autologous stem-cell rescue in patients with newly diagnosed primary CNS lymphoma; an intent to treat analysis. J Clin Oncol 2003; 21: 4151–4156.
Abrey LE, Batchelor TT, Ferreri AJ, Gospodarowicz M, Pulczynski EJ, Zucca E et al. Report of an international workshop to standardize baseline evaluation and response criteria for primary CNS lymphoma. J Clin Oncol 2005; 23: 5034–5043.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982; 5: 649–655.
Mappa S, Marturano E, Frezzato M, Frungilo N, Llariucci F, Stelitano C et al. Salvage chemoimmunotherapy with rituximab, ifosfamide and etoposide (R-IE regimen) in patients with primary CNS lymphoma relapsed or refractory to high-dose methotrexate-based chemotherapy. Hematol Oncol 2013; 31: 143–150.
Illerhaus G, Muller F, Feuerhake F, Schafer AO, Ostertag C, Finke J . High-dose chemotherapy and autologous stem-cell transplantation without consolidating radiotherapy as first-line treatment for primary lymphoma of the central nervous system. Haematologica 2008; 93: 147–148.
Soussain C, Hoang-Xuan K, Taillandier L, Fourme E, Choquet S, Witz F et al. Intensive chemotherapy followed by hematopoietic stem-cell rescue for refractory and recurrent primary CNS and intraocular lymphoma: Société Française de Greffe de Moëlle Osseuse-Thérapie Cellulaire. J Clin Oncol 2008; 26: 2512–2518.
Cheng T, Forsyth P, Chaudhry A, Morris D, Gluck S, Russell JA et al. High-dose thiotepa, busulfan, cyclophosphamide and ASCT without whole-brain radiotherapy for poor prognosis primary CNS lymphoma. Bone Marrow Transplant 2003; 31: 679–685.
Alimohamed N, Daly A, Owen C, Duggan P, Stewart DA . Upfront thiotepa, busulfan, cyclophosphamide, and autologous stem cell transplantation for primary CNS lymphoma: a single centre experience. Leuk Lymphoma 2012; 53: 862–867.
O'Neill A, Mikesch K, Fritsch K, Kasenda B, Banerjee L, Burns F et al. Outcomes for HIV-positive patients with primary central nervous system lymphoma after high-dose chemotherapy and auto-SCT. Bone Marrow Transplant 2015; 50: 999–1000.
DeAngelis LM, Seiferheld W, Schold SC, Fisher B, Schultz CJ Radiation Therapy Oncology Group S. Combination chemotherapy and radiotherapy for primary central nervous system lymphoma: Radiation Therapy Oncology Group Study 93-10. J Clin Oncol 2002; 20: 4643–4648.
Thiel E, Korfel A, Martus P, Kanz L, Griesinger F, Rauch M et al. High-dose methotrexate with or without whole brain radiotherapy for primary CNS lymphoma (G-PCNSL-SG-1): a phase 3, randomised, non-inferiority trial. Lancet Oncol 2010; 11: 1036–1047.
Ferreri AJ, Cwynarski K, Pulczynski E, Fox CP, Schorb E, Rosee PL et al. Effects on survival and neurocognitive functions of whole-brain radiotherapy (WBRT) and autologous stem cell transplantation (ASCT) as consolidation options after high-dose methotrexate-based chemoimmunotherapy in patients with newly diagnosed primary CNS lymphoma (PCNSL): results of the second randomization of the IELSG32 Trial. Blood 2016; 128: 511.
Acknowledgements
We thank the patients and the staff that looked after them. We also acknowledge members of the UK PCNSL working party and the support of the NCRI lymphoma CSG.
Author contributions
SK, KC and CPF provided patients, collected and analysed the data, performed statistical analysis and wrote the paper. EC, AO’N, CH, TC, AD, SM, AL, GA, KM, PM, DD, CR, SE, TAE and RM provided patients and collected data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
SK has received travel support from Gilead and a research grant from Celgene. CPF has received speaker honoraria and advisory board remuneration from Adienne Pharma/Biotech and Roche. KC has received speaker honoraria and advisory board remuneration from Adienne and Roche. SM received speaker honoraria from Roche and travel support from Gilead. All other authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Kassam, S., Chernucha, E., O’Neill, A. et al. High-dose chemotherapy and autologous stem cell transplantation for primary central nervous system lymphoma: a multi-centre retrospective analysis from the United Kingdom. Bone Marrow Transplant 52, 1268–1272 (2017). https://doi.org/10.1038/bmt.2017.101
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2017.101
- Springer Nature Limited