Abstract
The over-expression of several receptor tyrosine kinases in adult high grade astrocytomas (HGA) led to trials of tyrosine kinase inhibitors in these patients. Similar molecular genetic analysis of pediatric HGA is only beginning to be published. Thus it is unclear to what degree these pathways are also involved in the pediatric age group and whether they may also serve as useful therapeutic targets for children with HGAs. Here we investigated the protein expression profile of a series of pediatric HGAs. Following institutional ethical approval, clinical information and tumor samples were obtained for 42 HGA patients. Mean age at presentation was 10.1 years (range 0.13–19.3 years). OS was 12% and PFS was 3.7%. Extent of resection was associated with improved PFS (P = 0.0015) with a trend towards improved OS (P = 0.08). There was no significant effect of age or adjuvant therapy use on PFS or OS. Immunopositivity for each of the markers was as follows: p53 35%; PDGFR-α 45%; PDGFR-β 31%; PTEN 67%; EGFR wild type 58%; EGFRvIII 2%. No significant effect on OS or PFS was found for any of the markers by log rank analysis. However, all long-term survivors expressed PTEN and were EGFRvIII negative. Further, there were distinct differences in protein expression between pediatric and adult HGAs suggesting that EGFR kinase inhibitors may not be beneficial for treatment of HGA in the pediatric age group and pointing to the need to study pediatric astrocytomas as distinct entities from adult astrocytomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain tumors are the leading cause of cancer-related mortality in the pediatric age group. Of these, tumors phenotypically resembling astrocytes, or astrocytomas, make up the largest proportion. While in adults, high grade astrocytomas are the most common, in children they account for ∼10% of brain tumors. Treatment of these tumors remains a challenge and despite aggressive multi-modal therapy comprised of surgical resection, radiation and chemotherapy, 2-year survival rates remain at ∼10 to 30% for supratentorial tumors [1]. In adults, the poor outcome for this group of tumors has led to considerable effort to understand the molecular events underlying their pathogenesis and to develop novel therapies to target these pathways. Included among the plethora of genetic abnormalities discovered in adult high grade astrocytomas are amplification of the epidermal growth factor receptor (EGFR) gene, multiple types of EGFR mutations, the most common being EGFR variant III (EGFRvIII), loss of the tumor suppressor protein PTEN, over-expression of platelet-derived growth factor receptor α and mutations in the p53 gene. The over-expression of several receptor tyrosine kinases in adult high grade astrocytomas led to trials of the EGFR inhibitor erlotinib or the tyrosine kinase inhibitor imatinib mesylate in these patients. Similar molecular genetic analysis of pediatric high grade astrocytoma is only beginning to be published. Thus it is unclear to what degree these pathways are also involved in the pediatric age group and whether they may also serve as useful therapeutic targets for children with high grade astrocytomas. Here we studied expression of p53, PDGFR-α, PDGFR-β, PTEN, EGFR wild type and EGFR variant III in a large series of pediatric high grade astrocytomas and correlated this with survival. Our results suggest a significant distinction in protein expression of pediatric high grade astrocytomas compared to their adult counterparts, and also provide information about potential therapeutic targets in the pediatric age group.
Patients and methods
Following institutional ethical approval, patients less than 18 years old operated on at the Hospital for Sick Children (HSC; Toronto, Canada) between 1985 and 2005 with a pathologic diagnosis of supratentorial high grade astrocytoma were identified through the oncology and pathology databases. Forty-two patients who had undergone a first-time surgical resection at HSC were identified including 26 WHO grade III anaplastic astrocytomas and 16 WHO grade IV glioblastoma multiformes. After pathological review, 41 patients with sufficient material and correct pathological diagnosis were included.
Clinical data
Clinical data were retrieved from patient charts and the oncology electronic database and included age at presentation, gender, tumor location, pathological diagnosis, date of first surgery, extent of resection, adjuvant chemotherapy use, radiotherapy use, date of recurrence, supplementary therapy and date of last follow-up or date of death. Only patients with a diagnosis of high grade astrocytoma and supratentorial location were included. Extent of surgical resection was recorded as Gross total resection (GTR) if no gross tumor remaining was reported in the operative note or postoperative magnetic resonance imaging. Subtotal resection was defined as more than 50% resection and partial resection as less than 50% resection. Tumors deeply seated that could only be biopsied were recorded as such. Overall survival (OS) and Progression free survival (PFS) were calculated from the date of initial surgery to the date of death or first recurrence identified by imaging follow-up, respectively.
Tissue microarray construction
All pathological blocks and corresponding slides from the 42 patients were reviewed by a neuropathologist (C.H.) for diagnostic accuracy and tissue adequacy. Astrocytomas were graded based on WHO criteria [2]. Representative tumor areas were identified and three 1-mm tumor cores were chosen for construction of tissue microarray blocks [3]. A variety of tissues including, liver, cerebral white matter, ependyma and germinal matrix were included around the periphery of each array to serve as internal controls.
Immunohistochemistry
Five-micrometer-thick sections cut from the tissue microarray were subjected to immunohistochemistry using the following monoclonal antibodies: p53 (1:30, DO-7, Dako, Denmark), PDGFR-α (1:50, sc-338, Santa Cruz Biotechnology Inc, Santa Cruz, CA), PDGFR-β (1:200, clone 28, BD Biosciences, San Jose, CA), PTEN (1:100, c-6H2.1, Cascade Bioscience Inc., Winchester, MA), EGFR-wild type (1:200, Upstate/ Millipore, Billerica, MA), EGFR-variant III (1:10, Vision Biosystems/ Novocastra, Norwell, MA), MIB-1 (1:50, Dako, Glostrup, Denmark). Briefly, tissue sections were mounted on positively charged microscope slides and then baked overnight at 60°C, dewaxed in xylene, and rehydrated through decreasing concentrations of alcohol. Immunohistochemical procedures for antibodies against p53, PDGFR-α and Ki-67 were performed on the Ventana NEXES autoimmunostainer (Ventana Medical Systems, Tucson, AZ). The other antibodies were performed manually. All sections were further treated with heat-induced epitope retrieval and blocked for endogenous peroxidase and biotin by using Vector Elite avidin-biotin complex method detection system (Vector Laboratories, Burlington, Canada). 3,3′-diaminobenzidine (DAB, Sigma-Aldrich, Oakville, Canada) was used as the chromogenic substrate and the counterstain of preference was hemotoxylin. Appropriate positive and negative controls were also stained in parallel.
Immunohistochemical grading
Staining of tissue microarray slides was reviewed and graded for both intensity (0, none; 1, weak; 2, strong) and distribution (<25%, 25–50%, 50–75%, >75% of tumor cells) by two reviewers (M.L.L. and C.E.H.) who were blinded to clinical patient data at the time of grading. Only tumors with strong staining were considered to be positive. Based on the literature, the following percentage cut-offs were then used to determine marker positivity: p53—75% (nuclear) [4], PDGFR-α and -β—25% (cytoplasmic) [5], PTEN—75% and EGFR wild type—50% [6]. For EGFRvIII tumors demonstrating even focal moderate immunostaining were considered positive [7].
Control tissues used for antibody standardization were as follows: P53—retinoblastoma, PDGFR-α & -β—breast carcinoma, PTEN—breast ductular epithelium. Xenografts from implanted transfected glioma cells with known positivity were used as positive controls for EGFR wild-type and EGFRvIII antibodies.
Statistical analysis
For each biological marker progression-free survival (PFS) and overall survival (OS) were estimated using the Kaplan Meier method, and significance testing (α = 5%) done on the basis of the log-rank test.
Results
Clinical and demographic features
Forty-two patients were included in the study (27 boys and 15 girls). The mean age of presentation was 10.1 years (range, 4 months to 18 years). Nine patients did not receive radiotherapy because of young age (<3 years at presentation) and 7 patients did not receive chemotherapy owing to compromise of immunity or the choice of the parents. Extent of surgical resection was as follows: gross total resection, 14 of 42 patients (33%); subtotal resection, 19 of 42 patients (45%); partial resection, 7 of 42 patients (17%); and biopsy, only 2 of 42 patients (5%).
The mean follow-up time was 1.8 years (2.7 years in survivors). The OS was 12% at 5 years (mean ± SD = 30 ± 6.6 months/median ± SD = 16.2 ± 1.6 months). PFS was 3.7% at 5 years (mean ± SD = 13.3 ± 3.2 months/median ± SD = 7.6 ± 3 months). Of the clinical factors only extent of resection was associated with outcome; those patients who received a gross total resection had a significantly better PFS on both univariate (Log Rank, P = 0.007) and multivariate (Wald, P = 0.01) analysis and approached significance for an improved OS (P = 0.08) (Table 1).
Immunohistochemical features
Two tissue microarrays comprising 41 tumors were analyzed for immunopositivity to p53, PDGFR-α, PDGFR-β, PTEN, EGFR wild type, and EGFRvIII (see Fig. 1). During the dewaxing stage, one tumor sample for p53, PDGFR-α and EGFR wild type and 2 tumor samples for PDGFR-β and PTEN were lost. The number of tumors positive for each of the markers is shown in Table 2.
The effect on survival of each biological marker is summarized in Table 2. None of markers significantly influenced survival on univariate analysis, likely given the generally poor survival in our cohort. We then did multivariate analysis, stratifying for extent of resection which was the only clinical factor to influence PFS in our cohort. This suggested a poorer PFS in those patients whose tumors were strongly positive for PDGFR-β (HR 2.97, 95%CI 1.00–8.85). Further, it is noteworthy that all the long term survivors are PTEN positive and EGFRvIII negative and only one is PDGFR-β positive (Table 3).
Discussion
In contrast to those in adults, pediatric high-grade astrocytomas (HGA) are significantly less common than low-grade lesions, comprising 20% of all hemispheric gliomas [8]. However, the prognosis in children with supratentorial HGAs has been dismal despite aggressive multimodality therapies involving aggressive resection, radiotherapy and chemotherapy [9, 10].
Here we describe the protein expression profile for a group of pediatric supratentorial HGAs who were treated in a single institute (HSC; Toronto, Canada) and followed up by the cooperative neuro-oncology group. The overall survival (OS) was 12% at 5 years and progression-free survival (PFS) was 3.7% at 5 years in our cohort. This outcome is worse than others that have been reported in the literature but likely reflects the purity of the high grade astrocytoma cohort and points to the worse prognosis of malignant astrocytomas compared to other mixed or low grade gliomas.
Attempt at gross-total resection has been standard in the management of pediatric malignant gliomas with improved outcome shown for well-circumscribed lesions. In two recent series, one from a single-institute and the other from the Children’s Cancer Group (CCG), extent of resection was the strongest predictor of outcome compared with other clinico-pathological factors [11, 12]. Our results are in agreement with this. In our series gross-total resection was the only clinical factor to significantly improve PFS (P = 0.007).
Over-expression of p53 is reported to be associated with adverse outcome in two series of pediatric malignant gliomas. One series included all grade III and IV gliomas together and identified p53 as a independent factor for poor progression-free survival [4]; the other series analyzed outcome of 18 pediatric glioblastomas of different anatomical locations and indicated p53 expression was significantly higher in those patients with recurrence and poorer prognosis [13]. In our analysis of supratentorial high grade astrocytomas, p53 over-expression was present in 14 of 40 (35%) cases and no association between p53 reactivity and outcome was detected.
PDGFR-α over-expression has been detected in between 20 and 50% of malignant astrocytomas. In a report of 40 patients with grade 2 astrocytomas and oligoastrocytomas, there was an association between high PDGFR-α expression and long survival time [14]. In our pediatric series, 18 out of 40 (45%) cases were immunopositive. Although there was no significant survival difference based on univariate or multivariate analysis in our cohort, the majority of long term survival cases (4/5) had PDGFR-α over-expression.
The prognostic role of PDGFR-β expression in pediatric HGA has not been well studied. In a recent series it was reported to be expressed in a subset of adult glioblastomas but was not associated with outcome [15]. Functionally, it is thought to be important in glioma angiogenesis [16]. In our series, PDGFR-β was expressed in 12 of 39 (31%) tumors and showed an association with decreased PFS on multivariate analysis after controlling for extent of resection by stratification.
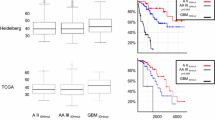
For the biological markers, while none were predictive of survival, some interesting differences from adult high grade astrocytomas emerged and are summarized in Fig. 2 [15, 17–19]. Loss of PTEN expression, which has been reported to correlate with PTEN deletion, mutation or loss of chromosome 10 [18], was much less common in the pediatric tumors (33%) than has been reported for adult high grade astrocytomas (mean 66%) [20, 21]. While loss of PTEN did not reach significance as a predictive marker in our study, the presence of PTEN mutations have been reported as a negative prognostic indicator in other pediatric and adult HGA series [9, 22]. In keeping with this, none of our long-term survivors had loss of PTEN in their tumors.
Earlier studies have reported over-expression of EGFR protein in from 11% to 81% of pediatric high grade gliomas [13, 23, 24]. Some of this variability is accounted for by differences in location, with a greater percentage of positive tumors being found in studies which excluded brain stem gliomas [24]. Consistent with this, in our series, we found strong cytoplasmic staining in more than 50% of cells in 23 out of 40 (58%) cases. EGFR expression was not of prognostic relevance in terms of either progression-free survival or overall survival in ours or other studies [24].
The most common EGFR mutant in adults, EGFR variant III is a constitutively active form of EGFR and is expressed in 24–67% adult glioblastoma cases [25]. We only found EGFRvIII expression in one case (2%) of the 41 pediatric high grade astrocytomas tested. Given the recent report of a strong association between the co-expression of EGFRvIII and PTEN in glioblastomas and responsiveness to EGFR kinase inhibitors [6], it seems less likely, given our results, that this approach will work in pediatric astrocytomas.
Conclusion
Our study offers a comprehensive expression profile in a large cohort of pediatric high-grade astrocytomas. We demonstrate the distinct protein expression between pediatric and adult high-grade astrocytomas, especially for PTEN and EGFRvIII expression. These findings suggest that EGFR kinase inhibitors may not be beneficial for treatment of high grade astrocytomas in the pediatric age group and points to the need to study pediatric astrocytomas as distinct entities from adult astrocytomas.
References
Broniscer A, Gajjar A (2004) Supratentorial high-grade astrocytoma and diffuse brainstem glioma: two challenges for the pediatric oncologist. Oncologist 9:197–206
Kleihues P, Sobin LH (2000) World Health Organization classification of tumors. Cancer 88:2887
Camp RL, Charette LA, Rimm DL (2000) Validation of tissue microarray technology in breast carcinoma. Lab Invest 80:1943–1949
Pollack IF, Finkelstein SD, Woods J, Burnham J, Holmes EJ, Hamilton RL, Yates AJ, Boyett JM, Finlay JL, Sposto R (2002) Expression of p53 and prognosis in children with malignant gliomas. N Engl J Med 346:420–427
Wilczynski SP, Chen YY, Chen W, Howell SB, Shively JE, Alberts DS (2005) Expression and mutational analysis of tyrosine kinase receptors c-kit, PDGFRalpha, and PDGFRbeta in ovarian cancers. Hum Pathol 36:242–249
Mellinghoff IK, Wang MY, Vivanco I, Haas-Kogan DA, Zhu S, Dia EQ, Lu KV, Yoshimoto K, Huang JH, Chute DJ, Riggs BL, Horvath S, Liau LM, Cavenee WK, Rao PN, Beroukhim R, Peck TC, Lee JC, Sellers WR, Stokoe D, Prados M, Cloughesy TF, Sawyers CL, Mischel PS (2005) Molecular determinants of the response of glioblastomas to EGFR kinase inhibitors. N Engl J Med 353:2012–2024
Choe G, Horvath S, Cloughesy TF, Crosby K, Seligson D, Palotie A, Inge L, Smith BL, Sawyers CL, Mischel PS (2003) Analysis of the phosphatidylinositol 3’-kinase signaling pathway in glioblastoma patients in vivo. Cancer Res 63:2742–2746
Pollack IF (1994) Brain tumors in children. N Engl J Med 331:1500–1507
Raffel C, Frederick L, O’Fallon JR, Atherton-Skaff P, Perry A, Jenkins RB, James CD (1999) Analysis of oncogene and tumor suppressor gene alterations in pediatric malignant astrocytomas reveals reduced survival for patients with PTEN mutations. Clin Cancer Res 5:4085–4090
Nicholson HS, Krailo M, Ames MM, Seibel NL, Reid JM, Liu-Mares W, Vezina LG, Ettinger AG, Reaman GH (1998) Phase I study of temozolomide in children and adolescents with recurrent solid tumors: a report from the Children’s Cancer Group. J Clin Oncol 16:3037–3043
Wisoff JH, Boyett JM, Berger MS, Brant C, Li H, Yates AJ, McGuire-Cullen P, Turski PA, Sutton LN, Allen JC, Packer RJ, Finlay JL (1998) Current neurosurgical management and the impact of the extent of resection in the treatment of malignant gliomas of childhood: a report of the Children’s Cancer Group trial no. CCG-945. J Neurosurg 89:52–59
Bucci MK, Maity A, Janss AJ, Belasco JB, Fisher MJ, Tochner ZA, Rorke L, Sutton LN, Phillips PC, Shu HK (2004) Near complete surgical resection predicts a favorable outcome in pediatric patients with nonbrainstem, malignant gliomas: results from a single center in the magnetic resonance imaging era. Cancer 101:817–824
Ganigi PM, Santosh V, Anandh B, Chandramouli BA, Sastry Kolluri VR (2005) Expression of p53, EGFR, pRb and bcl-2 proteins in pediatric glioblastoma multiforme: a study of 54 patients. Pediatr Neurosurg 41:292–299
Ribom D, Andrae J, Frielingsdorf M, Hartman M, Nister M, Smits A (2002) Prognostic value of platelet derived growth factor alpha receptor expression in grade 2 astrocytomas and oligoastrocytomas. J Neurol Neurosurg Psychiatry 72:782–787
Haberler C, Gelpi E, Marosi C, Rossler K, Birner P, Budka H, Hainfellner JA (2006) Immunohistochemical analysis of platelet-derived growth factor receptor-alpha, -beta, c-kit, c-abl, and arg proteins in glioblastoma: possible implications for patient selection for imatinib mesylate therapy. J Neurooncol 76:105–109
Guo P, Hu B, Gu W, Xu L, Wang D, Huang HJ, Cavenee WK, Cheng SY (2003) Platelet-derived growth factor-B enhances glioma angiogenesis by stimulating vascular endothelial growth factor expression in tumor endothelia and by promoting pericyte recruitment. Am J Pathol 162:1083–1093
Korshunov A, Golanov A, Sycheva R, Pronin I (1999) Prognostic value of tumour associated antigen immunoreactivity and apoptosis in cerebral glioblastomas: an analysis of 168 cases. J Clin Pathol 52:574–580
Idoate MA, Soria E, Lozano MD, Sola JJ, Panizo A, de Alava E, Manrique M, Pardo-Mindan FJ (2003) PTEN protein expression correlates with PTEN gene molecular changes but not with VEGF expression in astrocytomas. Diagn Mol Pathol 12:160–165
Heimberger AB, Hlatky R, Suki D, Yang D, Weinberg J, Gilbert M, Sawaya R, Aldape K (2005) Prognostic effect of epidermal growth factor receptor and EGFRvIII in glioblastoma multiforme patients. Clin Cancer Res 11:1462–1466
Sano T, Lin H, Chen X, Langford LA, Koul D, Bondy ML, Hess KR, Myers JN, Hong YK, Yung WK, Steck PA (1999) Differential expression of MMAC/PTEN in glioblastoma multiforme: relationship to localization and prognosis. Cancer Res 59:1820–1824
Chakravarti A, Delaney MA, Noll E, Black PM, Loeffler JS, Muzikansky A, Dyson NJ (2001) Prognostic and pathologic significance of quantitative protein expression profiling in human gliomas. Clin Cancer Res 7:2387–2395
Lin H, Bondy ML, Langford LA, Hess KR, Delclos GL, Wu X, Chan W, Pershouse MA, Yung WK, Steck PA (1998) Allelic deletion analyses of MMAC/PTEN and DMBT1 loci in gliomas: relationship to prognostic significance. Clin Cancer Res 4:2447–2454
Sure U, Ruedi D, Tachibana O, Yonekawa Y, Ohgaki H, Kleihues P, Hegi ME (1997) Determination of p53 mutations, EGFR overexpression, and loss of p16 expression in pediatric glioblastomas. J Neuropathol Exp Neurol 56:782–789
Bredel M, Pollack IF, Hamilton RL, James CD (1999) Epidermal growth factor receptor expression and gene amplification in high-grade non-brainstem gliomas of childhood. Clin Cancer Res 5:1786–1792
Heimberger AB, Suki D, Yang D, Shi W, Aldape K (2005) The natural history of EGFR and EGFRvIII in glioblastoma patients. J Transl Med 3:38
Acknowledgements
This work is supported by a grant from B.r.a.i.n.c.h.i.l.d. Canada. CH is supported by a clinician-scientist award from CIHR/Eli Lilly/CCO.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liang, ML., Ma, J., Ho, M. et al. Tyrosine kinase expression in pediatric high grade astrocytoma. J Neurooncol 87, 247–253 (2008). https://doi.org/10.1007/s11060-007-9513-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-007-9513-1