Abstract
Patients with cystic fibrosis (CF) suffer from chronic lung infections, caused by bacterial, viral or fungal pathogens, which determine morbidity and mortality. The contribution of individual pathogens to chronic disease and acute lung exacerbations is often difficult to determine due to the complex composition of the lung microbiome in CF. In particular, the relevance of fungal pathogens in CF airways remains poorly understood due to limitations of current diagnostics to identify the presence of fungal pathogens and to resolve the individual host–pathogen interaction status. T-lymphocytes play an essential role in host defense against pathogens, but also in inappropriate immune reactions such as allergies. They have the capacity to specifically recognize and discriminate the different pathogens and orchestrate a diverse array of effector functions. Thus, the analysis of the fungus-specific T cell status of an individual can in principle provide detailed information about the identity of the fungal pathogen(s) encountered and the actual fungus–host interaction status. This may allow to classify patients, according to appropriate (protective) or inappropriate (pathology-associated) immune reactions against individual fungal pathogens. However, T cell-based diagnostics are currently not part of the clinical routine. The identification and characterization of fungus-specific T cells in health and disease for diagnostic purposes are associated with significant challenges. Recent technological developments in the field of fungus-specific T helper cell detection provide new insights in the host T cell–fungus interaction. In this review, we will discuss basic principles and the potential of T cell-based diagnostics, as well as the perspectives and further needs for use of T cells for improved clinical diagnostics of fungal diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with CF suffer from broncho-pulmonary disease exacerbations due to multiple recurrent and chronic infections of the lung [1, 2]. A contribution of bacterial and viral species in this process is well established, but also filamentous fungi or yeasts, such as Aspergillus spp., Scedosporium spp., Exophiala spp., Rasamsonia spp., Trichosporon spp., and Candida spp., and their mutual interactions are becoming increasingly important [3,4,5,6,7]. In addition, also several other fungal pathogens can be detected in respiratory samples in patients with CF as epidemiological studies show [4, 8,9,10], but their contribution to disease pathogenesis is largely unknown. In terms of fungal pathogens, most of the research has been done on allergic broncho-pulmonary aspergillosis (ABPA) [5, 11,12,13,14,15,16,17,18,19,20], but increasing interest exists also in other entities than allergic reactions due to fungal species. Fungal bronchitis and fungal infections [8, 18, 21,22,23,24,25,26,27,28,29,30,31] are two important manifestations in this context. In addition, colonization with Candida spp. might have a significant impact on the clinical course of the patient with an impairment of lung function [24,25,26, 32,33,34,35]. Fungal pathogens also gain clinical importance in end-stage CF disease as several of the aforementioned fungal species can induce severe infections post-transplantation [36,37,38,39,40,41,42]. Fungal pathogens such as Scedosporium species and Lomentospora prolificans are very difficult to treat because of their resistance to many antifungal drugs [43,44,45,46,47,48,49,50,51,52]. These different clinical situations demonstrate the broad impact of fungal pathogens during the disease course of CF patients. On a microbiological and immunological level, the complex microbial community of bacteria and fungal species in CF patients might result in a very diverse pattern of pathogen–host interactions, probably unique for each individual patient [18, 41, 53, 54].
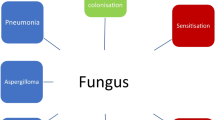
To determine the contribution of fungal pathogens to the current disease status of CF patients represents a particular challenge due to the limited possibilities for timely and specific diagnostics, which also results in delayed and rather empiric than targeted and species-specific therapeutic intervention [55,56,57]. Classical microbiological diagnostics based on direct detection of the fungus or its metabolites have limited sensitivity and specificity and often fail to resolve the complex host–pathogen interaction status, ranging from transient exposition and colonization to sensitization, hypersensitivity reactions or even invasive infections [58]. These different types of host–pathogen interaction are caused or influenced by the host immune response. Therefore, a detailed analysis of the patient’s immune status may allow resolving these different types of host–pathogen interaction. In particular, the adaptive immune response mediated by B- and T-lymphocytes provides unique and pathogen-specific information. Lymphocytes possess antigen-specific receptors allowing them to sense and react specifically to a given pathogen. This specificity in principle provides an ideal basis for pathogen-specific diagnostics. In addition, information about the qualitative immune response pattern in individual patients would improve our understanding of the basic mechanisms of immune protection versus infection-related immune pathology.
Antibody-Based Diagnostics Versus T Cells-Based Diagnostics
Antibody-Based Diagnostics
B- and T-lymphocytes form the adaptive arm of the immune response. They possess antigen-specific receptors allowing to sense and to react specifically to a given pathogen. Serum antibodies, the soluble form of the B cell antigen receptor, are commonly used to determine antigen sensitization, especially for allergic sensitization [59]. This may also be helpful to reveal different types of fungal sensitization, such as an allergic broncho-pulmonary or chronic pulmonary mycosis [60, 61]. For example, Baxter et al. [22] introduced a classification of patients with CF into allergic broncho-pulmonary aspergillosis, sensitization and Aspergillus bronchitis, based on differences in Aspergillus-specific IgE and IgG titers, revealing different types of host immune responses. However, serum antibody levels are often maintained for prolonged time following antigen contact, due to constant antibody production by long-lived plasma cells. This can provide long-lived immune reactivity against pathogens even years after pathogen clearance, but at the same time may limit the diagnostic value of antibody titers to monitor acute and transient changes of the host–pathogen interaction status. Furthermore, antibody responses against fungi often target surface structures, such as polysaccharides, which are shared between fungal species and thus lack diagnostic specificity.
Antigen-Specific CD4 T Helper Cells as Faithful Reporters of the Host–Pathogen Interaction Status
CD4 T helper (Th) cells are the central organizers of adaptive immune responses against extracellular pathogens, such as fungi (CD8 T cells and more innate γ/δ T cells or NKT cells are not part of this review). They express T cell receptors (TCRs) with a single specificity that enable the selective recognition of small pathogen-derived peptides (antigenic epitopes) presented by antigen-presenting cells in association with human leukocyte antigen (HLA) molecules on the cell surface. Antigen recognition leads to transient activation of the T cell, characterized by production of effector molecules and proliferation, i.e., clonal expansion of the antigen-specific T cells. Additional co-stimulatory signals induce further differentiation and stable adaption of the T cells effector functions, allowing optimized responses against a particular pathogen. Following clearance of the antigen, the expanded T cell population contracts and the cells return to the resting stage, i.e., they lose signs of acute activation, but they maintain the capacity to react with optimized effector functions upon re-exposure to the antigen (“T cell memory”). Taken together, antigen contact in vivo leads to characteristic, both persistent and short-lived, alterations of T cell numbers, phenotype and function. Thus, the antigen-specific T cell status may provide detailed information about the past, acute and future interaction status of the host with a certain pathogen.
Th Cell Subset Diversity in Tolerance, Pathogen Protection and Immune Pathology: Diagnostic Need for a “Global View”
Th cell phenotypes and functions display considerable heterogeneity, reflecting different types of immune reactions against the different types of antigens or pathogens, ranging from tolerogenic, to protective, non-protective or even pathogenic responses, such as hypersensitivity reactions. Therefore, the question if and how the immune system is in contact with a particular pathogen may be answered by resolving the complexity of the immune reaction on the level of the pathogen-specific T cells.
Th cells differentiate within the thymus into two distinct lineages: The conventional Th cells (Tcons) are essential to generate protective immune reactions against pathogens, whereas inadequate or dysregulated Tcon responses may result in immune pathologies, such as allergy, autoimmunity or inflammatory diseases. The second major Th cell lineage comprises the “regulatory” T cells (Tregs). Their main function is to control or to suppress inappropriate immune reactions against self and harmless antigens or to control immune reactions against pathogens in order to limit immune pathology. Tregs are characterized by expression of the lineage specifying transcription factor forkhead box protein P3 (Foxp3) and a specific epigenetic and transcriptional gene expression profile. Tregs and Tcons can be classified according to their phenotype into naive cells that have not been in contact with their antigen in vivo and antigen-experienced “memory” T cells.
Memory Tcons can be further divided into several Th subsets according to their functional profile, e.g., their capacity to produce certain effector cytokines, such as IFN-γ (Th1), IL-4, IL-5, IL-13 (Th2), IL-17, IL-22 (Th17, Th22), IL-21 (T follicular helper cells, TFH). These effector programs, which also comprise differential migratory and homing capacity, are centrally regulated by so-called master transcription factors, which determine the overall effector program of the Th subset, such as T-bet for Th1, GATA-3 (Th2), ROR-γt (Th17) or BCL-6 (TFH) [62]. Similar functional adaptations have been claimed for Tregs, suggesting that Tregs also need to undergo similar differentiation steps to be able to control the corresponding Tcon responses [63,64,65,66,67]. However, due to limited information about the antigen specificity of Tregs in particular in humans it is currently not clear to what extent Tregs undergo or require similar subset differentiation in the course of the diverse immune response types.
As outlined above, the host response against a given pathogen will be stored in terms of differential functional capacity of the T cells, and this T cell memory determines the protective or pathological outcome of future interactions with the same pathogen. Thus, the phenotypic and functional analysis of human fungus-specific T cells can provide both a detailed picture of how a particular individual can react to a future encounter with a specific pathogen and in addition provides information on the acute host–pathogen interaction status.
Host–fungus interaction status is reflected by fungus-specific CD4+ T cells responses. a In healthy donors, the main function of the adaptive immune response seems to be protection from allergy development rather than protection from infection. The A. fumigatus-reactive CD4+ T cells are dominated by clonally expanded, high-affinity regulatory T cells (Tregs). Tregs recognize particle-associated antigens of the fungus, whereas secreted soluble antigens mainly seem to be ignored by T cells within the healthy immune system. How the secreted and particle-associated antigens can cross the epithelial barrier to be taken up by antigen-presenting cells (APCs) is currently unknown. b Colonization and sensitization with A. fumigatus, as it occurs in patients with CF, is associated with increased and prolonged presence of fungal antigens due to fungal growth leading over time to the development of a conventional memory T cell response (Tmem). However, due to the intact epithelial barrier this does not necessarily lead to constant antigen activation, since Tmem do not necessarily show signs of acute T cell activation (see d). If the induced Tmem recognize the same antigens as the Tregs, or whether they are directed against other proteins, which are not “counterregulated” by Tregs, such as the secreted antigen pool is currently not understood, but may have strong impact on their protective potential. Furthermore, it is currently not clear which effector functions the Tmem possess, e.g., Th1, Th2, Th17, and whether patients differ in their qualitative response against fungal pathogens, which may provide a prognostic parameter for individual susceptibility to a certain “host–pathogen interaction status.” c Allergic patients and patients with ABPA have a completely normal A. fumigatus-specific Treg compartment. However, Th2 cells develop against secreted proteins, which are not protected by a specific Treg response. Thus, Th2 cells can escape the Treg control by targeting proteins that are not evoking Treg response. Why and how the secreted proteins are presented to prime naive T cells into Th2 cells is currently unknown. It is conceivable that soluble antigens are presented by a different APC than fungus-associated proteins, which do not present Treg target antigens at the same time, which allows escape from bystander suppression. d During acute infection, fungal growth is strongly increased and A. fumigatus hyphae may invade the epithelia barrier in invasive infection generating strong confrontation with the immune system. Under these conditions, effector T cells (Teff) are largely expanded, as shown by data from hematologic patients with invasive mycosis, and most likely possess signs of recent activation, typically not observed in peripheral blood (e.g., Ki-67, CD38, ICOS, HLA-DR expression). Similar to colonization/sensitization (b) it is important to understand which antigens are targeted by Teffs during an acute infection. Teffs may be directed against secreted proteins, i.e., non-Treg targets like in allergy (c), which may be less capable to direct cellular immune defense to the fungal particles. Alternatively, Teffs are directed against the same proteins that are recognized by Tregs and thus Tregs may negatively affect the protective effect of the Teffs
Technological Challenges to Analyze Fungus-Specific Th Cells
The analysis of antigen-specific T cells is technically challenging in particular in humans. A comprehensive overview on technical aspects of antigen-specific T cell analysis has recently been published [68, 69]. Here, we only refer to the specific aspects relevant for analysis of fungus-specific Th cells in humans. Briefly, two principally different approaches are available. Peptide–MHC (pMHC) multimers are frequently used to directly stain T cells, which express the specific TCR [70]. However, this approach is so far mainly restricted to MHC class I restricted CD8 T cells, where antigenic pMHC complexes have been defined with high precision. In contrast, MHC class II multimers are still rarely used for the analysis of human CD4 T cells. Their main restriction is that they require prior knowledge of HLA class II molecules and defined antigen-derived epitopes. However, the complexity of the fungal proteome most likely precludes dominant responses against a single protein or even peptides [71]. Thus, even successfully generated pMHC multimers would cover only a tiny fraction of the overall Th cell response against a fungal pathogen.
Therefore, the majority of studies about fungus-specific Th cells in humans rely on indirect approaches based on antigen-specific in vitro activation of T cells, with whole fungal lysates or recombinant proteins [71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88]. Functional T cell parameters are utilized as a read-out, such as activation marker expression, cytokine production, proliferation, cytotoxicity or suppressive activity for Tregs [68, 69]. Crucial for antigen-specific T cell analysis is the choice of the read-out to provide comprehensive, sensitive and specific results. As mentioned above, T cell responses against pathogens may display substantial heterogeneity with respect to the functional Th cell types involved. Therefore, restricting the analysis for example to a single functional parameter such as a certain cytokine will only give a very restricted view on the antigen-specific T cell response, as it does not fully assess the functional complexity of the pathogen-specific T cell response. Prerequisite for a global view on antigen-specific T cells is that the functional read-out allows the identification of the total repertoire of specific T cells, including naive, antigen-experienced Tcons as well as Tregs to generate a comprehensive picture of the patient’s immune status. Furthermore, the time of in vitro stimulation should be kept at a minimum to prevent major in vitro-induced manipulations of the T cells, such as expansion, outgrowth of single clones or modulations of their phenotype and function, obscuring the original in vivo frequencies, phenotype and subset composition. However, without in vitro expansion the frequency of Th cells specific for a certain antigen is usually very low (< 0.1%), except during acute infections [68]. Therefore, pre-enrichment strategies have been used to collect sufficient antigen-specific T cells directly ex vivo for detailed analysis, without in vitro changes of phenotype and function of the cells [72, 73, 89, 90].
As an alternative to direct enrichment of the few antigen-specific T cells, the in vitro expansion in response to antigen is widely used to allow their detection and characterization. In fact, the majority of studies on fungus-specific T cell responses in humans still utilize this approach [75, 77,78,79,80,81,82, 85, 91]. However, this approach has significant limitations: (i) the determination of precursor frequencies in the original samples is inaccurate (ii) the in vitro culture also modulates the T cell phenotype and (iii) the various subsets have different in vitro expansion potential and (iv) in vitro culture may also expand T cells from unprimed donors. Such “neo”-antigen-specific T cells have recently been demonstrated even in the memory T cell pool of healthy donors [73, 90, 92]. Due to these limitations of many currently used assays, the interpretation of available data about human fungus-specific Th cells is difficult and hence the role of Th cells for antifungal immunity for the different types of host–pathogen interaction is only poorly understood.
Direct Detection of Fungus-Specific Treg and Tcon via Divergent Expression of CD154 and CD137
To overcome the current challenges with regard to fungus-specific Th cell detection, we have recently introduced antigen-specific T cell enrichment (ARTE), which allows comprehensive analysis of all relevant Th cell subsets specific for fungal antigens [72, 73]. ARTE is based on a brief in vitro stimulation with antigen, which can be defined peptides, proteins or whole fungal lysates. Following 5–7 h of stimulation, all antigen-specific Tcon subsets express CD154 on the cell surface, whereas Tregs express CD137, but lack CD154 [93]. Magnetic enrichment of the few CD154 or CD137 expressing cells from large cell samples (106–108 T cells) provides the possibility to collect sufficient numbers of antigen-specific T cells for detailed downstream analysis. This technology allows detection of 1 cell out of 105–106 and provides even access to Th cells from the naive repertoire [73]. Indeed, the parallel assessment of naive, as well as all memory Treg and Tcon subsets, provides an integrated view on the immune response in contrast to analyses of only one subset, e.g., producers of certain phenotypic markers or cytokines. This integration of all facets of the Th cell response allows a much better estimation: i, to what extent the adaptive immune system has already been in contact with the antigen as indicated by a change of the naive/memory T cell ratio; and ii, to what type of immune response has been generated or will be mounted upon a future encounter with the pathogen, e.g., Tregs versus the various functional Tcon subsets.
The Role of T Cells for Human Antifungal Immunity
The immune system has to cope with the fact that most fungi are part of our daily environment. For example, many fungi or fungal spores are constantly inhaled with our breathing air [94, 95]. Other fungi, such as Candida spp. and Malassezia spp., colonize human body surfaces [96]. These various types of chronically encountered fungi have to be eliminated or controlled without generating chronic inflammation. Failure of this balanced system results in fungus-associated diseases. These comprise true invasive infections, resulting from impaired immune protection, as well as hypersensitivity reactions, due to exaggerated or inappropriate reactions against fungal antigens. If and how Th cells contribute to maintenance and failure of these diverse host–pathogen interaction types, such as tolerance, protection from invasive infection and hypersensitivity reactions, is currently largely unknown. But the variable lifestyle of the various environmental, commensal and pathogenic fungi, their different sites of exposure within the human body and their diverse interactions with the human host in health and disease demand specific analysis of the Th cell response against individual species in healthy donors and particular diseases.
That the immune system protects from fungal infections is documented by the fact that the incidence of fungal infections is rising along with the strongly increasing numbers of immunocompromised patients, due to advanced cancer treatment, transplantation or HIV [97]. Although the primary risk factors in immunocompromised patients are defects of innate immune components, in particular of neutrophilic granulocytes, there is evidence that impaired T cell responses also contribute to decreased protection against invasive fungal infections [98, 99]. However, to what extent Th cells contribute to the protection against fungal infections in immunologically competent humans is currently not very well understood. For more detailed information about immunity in fungal diseases with an emphasis on the human immune system has only recently been comprehensively reviewed [100]. Here, we highlight only a few reports, which provide in our view the best evidence for T cells being involved in antifungal immunity in healthy subjects.
The strongest evidence for a protective role for Th cells against fungal infections exists for Candida albicans. Th17 cells reacting against C. albicans antigens can readily be detected in the blood of virtually all healthy humans [72, 73, 101, 102]. With mean frequencies of about 0.2% of total CD4 T cells, Candida-specific T helper cells are among the most frequent pathogen-specific T cells detectable in healthy donors [73]. Candida-specific T cells display typical memory-like features, such as clonally expansion and high avidity for antigen [103]. Specific T cell responses against many other clinically relevant fungi have also been reported in humans (reviewed in [100, 104, 105]. In summary, the role of T cell immunity for the various fungal diseases as well as the contribution of the distinct T helper cell subsets, such as Th1, Th2, Th17 or Treg, is still highly controversial. Several fungi induce only very low T cell responses, which are more difficult to analyze. For example, the direct analysis of A. fumigatus-specific responses in healthy donors revealed much lower frequencies and even more important the reactive T cells showed a less pronounced memory phenotype as compared to C. albicans [71,72,73, 103]. This seems to be similar for many other fungi tested in healthy donors, including several species from Aspergillus spp., Scedosporium spp., Fusarium spp., Rhizopus spp., Rhizomucor spp., Cunninghamella spp. Cryptococcus spp., Alternaria spp., Penicillium spp. (Bacher & Scheffold, unpublished observations). In contrast, most published studies about fungus-reactive T cells rely on prolonged in vitro cultivation for T cell detection and the introduced bias, i.e., the inability to correctly determine the frequency and the phenotype of T cells directly ex vivo as discussed in this review may severely impact on the interpretation of the results.
Therefore, the results from studies of human gene defects with regard to susceptibility to fungal diseases are important to validate the results from in vitro analyses. Indeed, various genetic defects affecting components of Th17 cytokines or their induction pathway directly correlates with increased susceptibility to Candida infections [106,107,108,109,110], providing compelling evidence for a critical role of Th17 cells in anti-Candida defense. Interestingly, Th17-associated immunodeficiencies do not result in increased infections by other common environmental fungi, such as Aspergillus fumigatus [100, 111]. This argues against a general role of Th17 cells in protective antifungal immunity, but rather supports the view that Candida spp. have the unique capability to induce Th17 cells in humans, which are in turn critical for host protection. In contrast, patients with genetic mutations and defects affecting the IL-12/IFN-γ/GM-CSF axis have been reported with dimorphic fungal infection, such as coccidioidomycosis, paracoccidioidomycosis or histoplasmosis [112,113,114,115,116], as well as predisposition to Cryptococcus infections [117,118,119], suggesting rather an important role for Th1 cells in defense against these fungal species.
Treg-Mediated Tolerance Against Aspergillus spp. as the Dominant Immune Reaction in Healthy Donors
Evidence for protective Th cell response in healthy humans against Aspergillus spp. is scarce. Even patients with severe immunodeficiencies completely lacking T cells have no increased incidence of pulmonary infections with A. fumigatus, suggesting that innate defense mechanisms are of major importance [111]. However, several groups have investigated and identified A. fumigatus-reactive Th cells in healthy donors [71, 75,76,77,78, 82, 87]. These studies indicated that low frequencies of CD4+ T cells specific for various A. fumigatus antigens can be detected. The strongest immunoreactivity was found against membrane proteins of metabolically active A. fumigatus morphotypes (germlings and hyphae) [71]. Importantly, by using magnetic enrichment of all A. fumigatus-reactive Th cells we recently showed that actually the majority of A. fumigatus-specific Th cells in healthy donors are still in a naive state. This indicates that despite chronic exposure to A. fumigatus antigens, Th cells that have the potential to react have not been activated in vivo. In contrast, the A. fumigatus-specific memory response was dominated by high-affinity, clonally expanded Tregs, which may actively prevent the activation of the conventional naive Th cell compartment [72, 103]. The importance of a balanced immune reaction of effector and regulatory T cell for control of fungi, such as A. fumigatus, has also been proposed in other studies with animal models as well as in humans, involving IL-10 producing Tr1 cells [120] and Treg/CTLA4-mediated modulation of tryptophan catabolism [121]. Such imbalanced regulation may contribute to susceptibility to invasive infection [78] or to exaggerated inflammation compromising antifungal immunity [122]. Our data surprisingly suggest that in healthy donors A. fumigatus is actually a major tolerogen rather than an immunogen, similar to harmless plant pollen or house dust mite. Similar Treg-dominated Th responses can also be identified against other airborne fungi in healthy donors (Bacher & Scheffold, unpublished). This is in accordance with the clinical data discussed before, suggesting that T cells are not ultimately required for protection against invasive pulmonary mycoses in immunocompetent hosts. Our data rather suggest that T cells are required to maintain tolerance against constant exposure to fungal antigens. Indeed, in patients with compromised lung functions such as chronic obstructive pulmonary disease (COPD) or CF, the most frequent clinical complications are in fact hypersensitivity reactions and ABPA, but much less invasive mycoses (although the frequency of invasive mycoses might be underestimated due to diagnostic limitations, see below). This is in accordance with the known role of Treg to prevent Th2 formation and allergy development. Importantly, in CF patients allergic to A. fumigatus, Treg responses are not impaired. However, in allergic CF patients, Th2 cells only develop against proteins not protected by specific Tregs, indicating that antigen escape of Th2 effector cells from Treg-mediated tolerance is an important mechanism for allergy development [103].
T Cell Cross-Reactivity a Technological Challenge for Fungus-Specific T Cell Analyses in Human Donors
For many years, the effector function of T cells has been used as a read-out for antigen-specific T cells. In particular, the production of cytokines, which are only produced by antigen-experienced “memory” T cells, such as IFN-γ, was taken as an indicator for a previous in vivo antigen encounter. However, this strict correlation has significantly been challenged by the recent identification of “memory” T cells specific for neo-antigens using either tetramers or ARTE in healthy donors [73, 90, 92]. It is well known that each TCR can recognize many different peptides. Thus, the presence of neo-antigen-specific T cells with a memory phenotype can be explained by the large TCR repertoire within the memory T cell pool of individuals exposed to a large number of infections during lifetime. The likelihood to detect a neo-antigen-specific T cell within a cell population mainly depends on its TCR repertoire size. Thus, neo-antigen-specific T cells are more or less statistically distributed between the naive and the memory pool. Indeed, we found that the few memory cells specific for harmless aeroantigens, such as plant pollen [103] or A. fumigatus (Bacher & Scheffold, unpublished observation) which can be detected in healthy donors together with a large naive pool, are neither clonally expanded nor of high avidity, suggesting that these cells are originally not primed by these antigens in vivo. Furthermore, the frequency of memory T cells against these antigens linearly correlated with the frequency of memory T cells in the total CD4+ T cell pool, as would be expected for a statistical rather than for an antigen-driven distribution.
Although this observation sounds in the first instance rather like an immunological peculiarity, cross-reactivity has significant impact on human immunity [123, 124] and in particular on the interpretation of results of antigen-specific T cell detection. In fact, this may generate false positive results, since the detection of antigen-specific memory T cells is not a reliable indicator for an in vivo immune reaction. For example, the frequency of neo-antigen-specific memory T cells may be susceptible to aging, which is accompanied by an increase in the memory repertoire. Thus, experimental systems restricting the analysis to certain effector cytokines or involving in vitro expansion, leading to a phenotype loss may not allow distinguishing between in vivo-primed antigen-specific responses and mere cross-reactivity. Thus, the integration of all T cell subsets, naive, memory, Treg into the analysis of specific T cell responses against an individual pathogen, as well as investigation of further parameters such as clonal composition of the T cell repertoire and functional avidity/affinity of the antigen-specific T cells, provides a more reliable basis to identify antigens which have generated immune responses in a certain individual and what type of immune response has been induced.
T Cell-Based Diagnostics for Fungus-Associated Diseases
As outlined above, there is evidence that Th cells are involved in protective immune responses against fungi in healthy individuals, encompassing both invasive infections as well as hypersensitivities. Thus, alterations of these response patterns may be highly relevant to diagnose fungus-associated diseases. Although fungal colonization, sensitization or infections are common in patients with CF, the fungus-specific T cells have not yet been systematically evaluated for diagnostic purposes. For invasive mold infections in immunocompromised patients and for mold-induced allergies, these alterations can be rather obvious and actually represent valuable diagnostic tools. We highlight these results as a proof of principle for fungus-specific T cells as diagnostic sensors, which may represent a potential strategy to resolve the complexity of the host–fungus interaction in CF patients even beyond invasive infections or allergy (Fig. 1).
Invasive Mycoses
The changes in the fungus-specific Th cell reaction have been used for analysis of invasive mold infections in immunocompromised hematologic patients. Increased IFN-γ production was correlated with protection [78, 81, 85, 86, 88, 125], whereas increased IL-10 levels have been suggested to be associated with progression of invasive infection [78]. However, as outlined above for example, Aspergillus spp.-specific T cells are already present in healthy donors and ex vivo analyses revealed that only a small subset produced IFN-γ [71, 73]. Furthermore, CD4+ T cell number in the blood of this patient group is highly variable. Thus, the restricted assessment of IFN-γ or other cytokine-producing T cells is not optimal for diagnostic purposes. In contrast, we could show that assessment of the total fungus-reactive conventional T cell compartment based on reactive expression of CD154 faithfully identified patients with proven invasive mycoses only based on increased fungus-specific T cell frequencies relative to the total CD4 T cells [74]. Importantly, this also allows discrimination between individual fungal species, e.g., Aspergilllus spp. or Mucorales spp. The fungus-specific T cells in this patient group displayed a memory phenotype clearly indicating an in vivo antigen encounter (Bacher & Scheffold, unpublished observation). This proves the potency of T cell-based diagnostics for diagnosing invasive mycoses. Further exploring whether T cell frequencies and phenotypic changes may also be helpful to diagnose fungal infections in immunocompetent persons, such as patients with CF, is currently ongoing.
Fungal Allergies
Fungus-specific Th2 cell development is an example for an obvious qualitative alteration in T cell reactivity, which may be used as an early diagnostic marker for allergic sensitization. Antigen-specific Th2 cells precede allergy development since they are required for specific IgE production by B cells, which is currently used as a diagnostic parameter for ABPA [60, 126,127,128,129,130]. Since Th2 cells only represent a few percent within the total T cell memory pool even in allergic donors, the frequency of potentially cross-reactive, i.e., false positive, Th2 cells can be neglected. Indeed, in healthy donors, fungus-specific Th2 cell patients are virtually absent, whereas in patients with compromised lung function, such as CF or COPD, a high proportion of donors display strong production of Th2 cytokines against fungal antigens [80, 83, 84, 131, 132] (and own unpublished observation). In this clinical setting, T cell analyses may be applied for early detection of fungal sensitization, including sensitization with other fungi than Aspergillus spp., or for predicting the risk for ABPA or ABPM (allergic broncho-pulmonary mycoses) development, e.g., in combination with other immunological markers, such as production of non-Th2 cytokines or antibody responses.
Further Directions for T Cell-Based Diagnosis of Fungal Colonization, (Non-Th2) Sensitization and Infection or Immune Response-Associated Risk Factors
The classical IgE-mediated allergy is the most prominent and diagnostically best defined form of hypersensitivity reaction. However, immunocompetent patients with compromised lung function, such as CF, non-CF bronchiectasis, COPD or asthma, frequently suffer from even less defined fungus-associated lung pathologies, which also have to be discriminated from other types of microbial infections [133]. Hypersensitivity also includes non-Th2 reaction types, which might contribute to lung inflammation. For example, Th17 cells, which are protective in the intestinal defense against C. albicans, might have deleterious effects if directed against molds within the lung mucosa [134,135,136].
However, as outlined above the detailed characterization of fungal T cell responses are still missing and thus the functional and clinical importance of most of the various immune reaction types are poorly understood. Here, T cell specific analysis provides significant potential to resolve the fungus–host interaction at different levels and to identify further diagnostically relevant parameters: The first question is actually which fungal pathogens cause an immunological response. Although it is assumed that many fungal pathogens are frequently encountered within our daily environment, it remains to be shown, whether this encounter is sufficient to initiate an adaptive immune response, which can already be a technical challenge in human donors as discussed above. The second step is to define: (i) what type of adaptive immune response has been induced by encounter with a given fungus and potential heterogeneity within donors; (ii) whether the adaptive immune system is actually required for the control of the host–fungus interactions; and (iii) what is its main role in this interaction: protection from infection or maintenance of tolerance, i.e., prevention of immune pathology such as allergy or chronic inflammation. For infectious situations, it is in addition important to understand what type of effector T cell response, e.g., Th1, Th2, Th17 response, or combination thereof is actually protective. Only when the physiological host–fungus interaction has been defined, it can be determined what types of alterations of the adaptive immune response occur in fungus-associated diseases or which type of immune reactions may even be causative, e.g., provide a risk factor for development of hypersensitivity reactions or failing immunity in invasive mycosis. Thus, it will be important to further decipher the cellular and molecular mechanisms of antifungal immunity against individual species in healthy donors and various clinical situations to develop new and targeted tools for diagnosis and treatment of fungal infections. New technologies like ARTE now enable to obtain the whole picture of the antifungal Th cell response against a certain fungal species in the steady state and relevant disease. We propose that by detailed characterization of Th cells reacting against specific pathogens relevant for patients, the contribution of these pathogens to the disease status in each individual patient can most accurately be determined.
References
Emerson J, Rosenfeld M, McNamara S, et al. Pseudomonas aeruginosa and other predictors of mortality and morbidity in young children with cystic fibrosis. Pediatr Pulmonol. 2002;34:91–100.
Rosenfeld M, Gibson RL, McNamara S, et al. Early pulmonary infection, inflammation, and clinical outcomes in infants with cystic fibrosis. Pediatr Pulmonol. 2001;32:356–66.
Delhaes L, Monchy S, Frealle E, et al. The airway microbiota in cystic fibrosis: a complex fungal and bacterial community–implications for therapeutic management. PLoS ONE. 2012;7:e36313.
Pihet M, Carrere J, Cimon B, et al. Occurrence and relevance of filamentous fungi in respiratory secretions of patients with cystic fibrosis–a review. Med Mycol. 2009;47:387–97.
Schwarz C, Brandt C, Antweiler E, et al. Prospective multicenter German study on pulmonary colonization with Scedosporium/Lomentospora species in cystic fibrosis: epidemiology and new association factors. PLoS ONE. 2017;12:e0171485.
Sudfeld CR, Dasenbrook EC, Merz WG, et al. Prevalence and risk factors for recovery of filamentous fungi in individuals with cystic fibrosis. J Cyst Fibros. 2010;9:110–6.
Whittaker LA, Teneback C. Atypical mycobacterial and fungal infections in cystic fibrosis. Semin Respir Crit Care Med. 2009;30:539–46.
Giraud S, Pihet M, Razafimandimby B, et al. Geosmithia argillacea: an emerging pathogen in patients with cystic fibrosis. J Clin Microbiol. 2010;48:2381–6.
Matos T, Cerar T, Praprotnik M, et al. First recovery of Rasamsonia argillacea species complex isolated in adolescent patient with cystic fibrosis in Slovenia–case report and review of literature. Mycoses. 2015;58:506–10.
Ziesing S, Suerbaum S, Sedlacek L. Fungal epidemiology and diversity in cystic fibrosis patients over a 5-year period in a national reference center. Med Mycol. 2016;54:781–6.
What is allergic bronchopulmonary aspergillosis. (ABPA)? Am J Respir Crit Care Med. 2014;190:P3–4.
Antunes J, Fernandes A, Borrego LM, et al. Cystic fibrosis, atopy, asthma and ABPA. Allergol Immunopathol (Madr). 2010;38:278–84.
Hartl D. Immunological mechanisms behind the cystic fibrosis-ABPA link. Med Mycol. 2009;47(Suppl 1):S183–91.
Jubin V, Ranque S, Stremler Le Bel N, et al. Risk factors for Aspergillus colonization and allergic bronchopulmonary aspergillosis in children with cystic fibrosis. Pediatr Pulmonol. 2010;45:764–71.
Mastella G, Rainisio M, Harms HK, et al. Allergic bronchopulmonary aspergillosis in cystic fibrosis. A European epidemiological study. Eur Respir J. 2000;16:464–71.
Maturu VN, Agarwal R. Prevalence of Aspergillus sensitization and allergic bronchopulmonary aspergillosis in cystic fibrosis: systematic review and meta-analysis. Clin Exp Allergy. 2015;45:1765–78.
Milla CE. Allergic bronchopulmonary aspergillosis and cystic fibrosis. Pediatr Pulmonol. 1999;27:71–3.
Schwarz CTA, Staab D, Tintelnot K. Scedosporium apiospermum: a fungal pathogen causing pneumonia in a patient with cystic fibrosis. JMM Case Rep. 2015;. https://doi.org/10.1099/jmmcr.0.000061.
Skov M, Koch C, Reimert CM, et al. Diagnosis of allergic bronchopulmonary aspergillosis (ABPA) in cystic fibrosis. Allergy. 2000;55:50–8.
Thronicke A, Heger N, Antweiler E, et al. Allergic bronchopulmonary aspergillosis is associated with pet ownership in cystic fibrosis. Pediatr Allergy Immunol. 2016;27:597–603.
Agatha D, Krishnan KU, Dillirani VA, et al. Invasive lung infection by Scedosporium apiospermum in an immunocompetent individual. Indian J Pathol Microbiol. 2014;57:635–7.
Baxter CG, Dunn G, Jones AM, et al. Novel immunologic classification of aspergillosis in adult cystic fibrosis. J Allergy Clin Immunol. 2013;132(560–6):e10.
Caston JJ, Linares MJ, Rivero A, et al. Clinical differences between invasive pulmonary infection by Scedosporium apiospermum and invasive pulmonary aspergillosis. Mycoses. 2011;54:e468–73.
Chotirmall SH. Candida albicans in cystic fibrosis: “Opening statements presented, let the trial begin”. Pediatr Pulmonol. 2016;51:445–6.
Chotirmall SH, Greene CM, McElvaney NG. Candida species in cystic fibrosis: a road less travelled. Med Mycol. 2010;48(Suppl 1):S114–24.
Gileles-Hillel A, Shoseyov D, Polacheck I, et al. Association of chronic Candida albicans respiratory infection with a more severe lung disease in patients with cystic fibrosis. Pediatr Pulmonol. 2015;50:1082–9.
Haase G, Skopnik H, Kusenbach G. Exophiala dermatitidis infection in cystic fibrosis. Lancet. 1990;336:188–9.
Holle J, Leichsenring M, Meissner PE. Nebulized voriconazole in infections with Scedosporium apiospermum–case report and review of the literature. J Cyst Fibros. 2014;13:400–2.
Kosmidis C, Denning DW. The clinical spectrum of pulmonary aspergillosis. Thorax. 2015;70:270–7.
Kusenbach G, Skopnik H, Haase G, et al. Exophiala dermatitidis pneumonia in cystic fibrosis. Eur J Pediatr. 1992;151:344–6.
Shoseyov D, Brownlee KG, Conway SP, et al. Aspergillus bronchitis in cystic fibrosis. Chest. 2006;130:222–6.
Chotirmall SH, O’Donoghue E, Bennett K, et al. Sputum Candida albicans presages FEV(1) decline and hospital-treated exacerbations in cystic fibrosis. Chest. 2010;138:1186–95.
Hector A, Kirn T, Ralhan A, et al. Microbial colonization and lung function in adolescents with cystic fibrosis. J Cyst Fibros. 2016;15:340–9.
Muthig M, Hebestreit A, Ziegler U, et al. Persistence of Candida species in the respiratory tract of cystic fibrosis patients. Med Mycol. 2010;48:56–63.
Reihill JA, Moore JE, Elborn JS, et al. Effect of Aspergillus fumigatus and Candida albicans on pro-inflammatory response in cystic fibrosis epithelium. J Cyst Fibros. 2011;10:401–6.
Bonvillain RW, Valentine VG, Lombard G, et al. Post-operative infections in cystic fibrosis and non-cystic fibrosis patients after lung transplantation. J Heart Lung Transplant. 2007;26:890–7.
Hong G, White M, Lechtzin N, et al. Fatal disseminated Rasamsonia infection in cystic fibrosis post-lung transplantation. J Cyst Fibros. 2017;16:e3–7.
Iversen M, Burton CM, Vand S, et al. Aspergillus infection in lung transplant patients: incidence and prognosis. Eur J Clin Microbiol Infect Dis. 2007;26:879–86.
Johnson LS, Shields RK, Clancy CJ. Epidemiology, clinical manifestations, and outcomes of Scedosporium infections among solid organ transplant recipients. Transpl Infect Dis. 2014;16:578–87.
Luong ML, Chaparro C, Stephenson A, et al. Pretransplant Aspergillus colonization of cystic fibrosis patients and the incidence of post-lung transplant invasive aspergillosis. Transplantation. 2014;97:351–7.
Rolfe NE, Haddad TJ, Wills TS. Management of Scedosporium apiospermum in a pre- and post-lung transplant patient with cystic fibrosis. Med Mycol Case Rep. 2013;2:37–9.
Sole A, Morant P, Salavert M, et al. Aspergillus infections in lung transplant recipients: risk factors and outcome. Clin Microbiol Infect. 2005;11:359–65.
Cuenca-Estrella M, Alastruey-Izquierdo A, Alcazar-Fuoli L, et al. In vitro activities of 35 double combinations of antifungal agents against Scedosporium apiospermum and Scedosporium prolificans. Antimicrob Agents Chemother. 2008;52:1136–9.
Gilgado F, Serena C, Cano J, et al. Antifungal susceptibilities of the species of the Pseudallescheria boydii complex. Antimicrob Agents Chemother. 2006;50:4211–3.
Houbraken J, Giraud S, Meijer M, et al. Taxonomy and antifungal susceptibility of clinically important Rasamsonia species. J Clin Microbiol. 2013;51:22–30.
Kirchhoff L, Olsowski M, Zilmans K, et al. Biofilm formation of the black yeast-like fungus Exophiala dermatitidis and its susceptibility to antiinfective agents. Sci Rep. 2017;7:42886.
Lackner M, de Hoog GS, Verweij PE, et al. Species-specific antifungal susceptibility patterns of Scedosporium and Pseudallescheria species. Antimicrob Agents Chemother. 2012;56:2635–42.
Mortensen KL, Johansen HK, Fuursted K, et al. A prospective survey of Aspergillus spp. in respiratory tract samples: prevalence, clinical impact and antifungal susceptibility. Eur J Clin Microbiol Infect Dis. 2011;30:1355–63.
Packeu A, Lebecque P, Rodriguez-Villalobos H, et al. Molecular typing and antifungal susceptibility of Exophiala isolates from patients with cystic fibrosis. J Med Microbiol. 2012;61:1226–33.
Rodriguez MM, Calvo E, Serena C, et al. Effects of double and triple combinations of antifungal drugs in a murine model of disseminated infection by Scedosporium prolificans. Antimicrob Agents Chemother. 2009;53:2153–5.
Sedlacek L, Graf B, Schwarz C, et al. Prevalence of Scedosporium species and Lomentospora prolificans in patients with cystic fibrosis in a multicenter trial by use of a selective medium. J Cyst Fibros. 2015;14:237–41.
Valenza G, Tappe D, Turnwald D, et al. Prevalence and antimicrobial susceptibility of microorganisms isolated from sputa of patients with cystic fibrosis. J Cyst Fibros. 2008;7:123–7.
Padoan R, Poli P, Colombrita D, et al. Acute Scedosporium apiospermum Endobronchial Infection in Cystic Fibrosis. Pediatr Infect Dis J. 2016;35:701–2.
Roehmel JF, Tintelnot K, Bernhardt A, et al. Arxula adeninivorans causing invasive pulmonary mycosis and fungaemia in cystic fibrosis. Lancet. 2015;385:1476.
Liu JC, Modha DE, Gaillard EA. What is the clinical significance of filamentous fungi positive sputum cultures in patients with cystic fibrosis? J Cyst Fibros. 2013;12:187–93.
Middleton PG, Chen SC, Meyer W. Fungal infections and treatment in cystic fibrosis. Curr Opin Pulm Med. 2013;19:670–5.
Muller FM, Seidler M. Characteristics of pathogenic fungi and antifungal therapy in cystic fibrosis. Expert Rev Anti Infect Ther. 2010;8:957–64.
Chotirmall SH, McElvaney NG. Fungi in the cystic fibrosis lung: bystanders or pathogens? Int J Biochem Cell Biol. 2014;52:161–73.
Platts-Mills TA, Schuyler AJ, Erwin EA, et al. IgE in the diagnosis and treatment of allergic disease. J Allergy Clin Immunol. 2016;137:1662–70.
Fukutomi Y, Tanimoto H, Yasueda H, et al. Serological diagnosis of allergic bronchopulmonary mycosis: progress and challenges. Allergol Int. 2016;65:30–6.
Richardson MD, Page ID. Aspergillus serology: have we arrived yet? Med Mycol. 2017;55:48–55.
Zhu J, Yamane H, Paul WE. Differentiation of effector CD4 T cell populations (*). Annu Rev Immunol. 2010;28:445–89.
Chaudhry A, Rudra D, Treuting P, et al. CD4+ regulatory T cells control TH17 responses in a Stat3-dependent manner. Science. 2009;326:986–91.
Koch MA, Tucker-Heard G, Perdue NR, et al. The transcription factor T-bet controls regulatory T cell homeostasis and function during type 1 inflammation. Nat Immunol. 2009;10:595–602.
Levine AG, Medoza A, Hemmers S, et al. Stability and function of regulatory T cells expressing the transcription factor T-bet. Nature. 2017;546:421–5.
Sefik E, Geva-Zatorsky N, Oh S, et al. MUCOSAL IMMUNOLOGY. Individual intestinal symbionts induce a distinct population of RORgamma(+) regulatory T cells. Science. 2015;349:993–7.
Zheng Y, Chaudhry A, Kas A, et al. Regulatory T-cell suppressor program co-opts transcription factor IRF4 to control T(H)2 responses. Nature. 2009;458:351–6.
Bacher P, Scheffold A. Flow-cytometric analysis of rare antigen-specific T cells. Cytometry A. 2013;83:692–701.
Bacher P, Scheffold A. New technologies for monitoring human antigen-specific T cells and regulatory T cells by flow-cytometry. Curr Opin Pharmacol. 2015;23:17–24.
Davis MM, Altman JD, Newell EW. Interrogating the repertoire: broadening the scope of peptide-MHC multimer analysis. Nat Rev Immunol. 2011;11:551–8.
Bacher P, Kniemeyer O, Teutschbein J, et al. Identification of immunogenic antigens from Aspergillus fumigatus by direct multiparameter characterization of specific conventional and regulatory CD4+ T cells. J Immunol. 2014;193:3332–43.
Bacher P, Kniemeyer O, Schonbrunn A, et al. Antigen-specific expansion of human regulatory T cells as a major tolerance mechanism against mucosal fungi. Mucosal Immunol. 2014;7:916–28.
Bacher P, Schink C, Teutschbein J, et al. Antigen-reactive T cell enrichment for direct, high-resolution analysis of the human naive and memory Th cell repertoire. J Immunol. 2013;190:3967–76.
Bacher P, Steinbach A, Kniemeyer O, et al. Fungus-specific CD4(+) T cells for rapid identification of invasive pulmonary mold infection. Am J Respir Crit Care Med. 2015;191:348–52.
Bozza S, Clavaud C, Giovannini G, et al. Immune sensing of Aspergillus fumigatus proteins, glycolipids, and polysaccharides and the impact on Th immunity and vaccination. J Immunol. 2009;183:2407–14.
Chai LY, van de Veerdonk F, Marijnissen RJ, et al. Anti-Aspergillus human host defence relies on type 1 T helper (Th1), rather than type 17 T helper (Th17), cellular immunity. Immunology. 2010;130:46–54.
Chaudhary N, Staab JF, Marr KA. Healthy human T-cell responses to Aspergillus fumigatus antigens. PLoS ONE. 2010;5:e9036.
Hebart H, Bollinger C, Fisch P, et al. Analysis of T-cell responses to Aspergillus fumigatus antigens in healthy individuals and patients with hematologic malignancies. Blood. 2002;100:4521–8.
Jolink H, de Boer R, Hombrink P, et al. Pulmonary immune responses against Aspergillus fumigatus are characterized by high frequencies of IL-17 producing T-cells. J Infect. 2017;74:81–8.
Jolink H, de Boer R, Willems LN, et al. T helper 2 response in allergic bronchopulmonary aspergillosis is not driven by specific Aspergillus antigens. Allergy. 2015;70:1336–9.
Jolink H, Hagedoorn RS, Lagendijk EL, et al. Induction of A. fumigatus-specific CD4-positive T cells in patients recovering from invasive aspergillosis. Haematologica. 2014;99:1255–63.
Jolink H, Meijssen IC, Hagedoorn RS, et al. Characterization of the T-cell-mediated immune response against the Aspergillus fumigatus proteins Crf1 and catalase 1 in healthy individuals. J Infect Dis. 2013;208:847–56.
Knutsen AP, Mueller KR, Levine AD, et al. Asp f I CD4+ TH2-like T-cell lines in allergic bronchopulmonary aspergillosis. J Allergy Clin Immunol. 1994;94:215–21.
Kreindler JL, Steele C, Nguyen N, et al. Vitamin D3 attenuates Th2 responses to Aspergillus fumigatus mounted by CD4+ T cells from cystic fibrosis patients with allergic bronchopulmonary aspergillosis. J Clin Invest. 2010;120:3242–54.
Potenza L, Vallerini D, Barozzi P, et al. Characterization of specific immune responses to different Aspergillus antigens during the course of invasive Aspergillosis in hematologic patients. PLoS ONE. 2013;8:e74326.
Potenza L, Vallerini D, Barozzi P, et al. Mucorales-specific T cells emerge in the course of invasive mucormycosis and may be used as a surrogate diagnostic marker in high-risk patients. Blood. 2011;118:5416–9.
Stuehler C, Nowakowska J, Bernardini C, et al. Multispecific Aspergillus T cells selected by CD137 or CD154 induce protective immune responses against the most relevant mold infections. J Infect Dis. 2015;211:1251–61.
Vallerini D, Forghieri F, Lagreca I, et al. Detection of Fusarium-specific T cells in hematologic patients with invasive fusariosis. J Infect. 2017;74:314–8.
Day CL, Seth NP, Lucas M, et al. Ex vivo analysis of human memory CD4 T cells specific for hepatitis C virus using MHC class II tetramers. J Clin Invest. 2003;112:831–42.
Su LF, Kidd BA, Han A, et al. Virus-specific CD4(+) memory-phenotype T cells are abundant in unexposed adults. Immunity. 2013;38:373–83.
Stuehler C, Khanna N, Bozza S, et al. Cross-protective TH1 immunity against Aspergillus fumigatus and Candida albicans. Blood. 2011;117:5881–91.
Kwok WW, Tan V, Gillette L, et al. Frequency of epitope-specific naive CD4(+) T cells correlates with immunodominance in the human memory repertoire. J Immunol. 2012;188:2537–44.
Schoenbrunn A, Frentsch M, Kohler S, et al. A converse 4-1BB and CD40 ligand expression pattern delineates activated regulatory T cells (Treg) and conventional T cells enabling direct isolation of alloantigen-reactive natural Foxp3 + Treg. J Immunol. 2012;189:5985–94.
Green BJ, Sercombe JK, Tovey ER. Fungal fragments and undocumented conidia function as new aeroallergen sources. J Allergy Clin Immunol. 2005;115:1043–8.
Tovey ER, Green BJ. Measuring environmental fungal exposure. Med Mycol. 2005;43(Suppl 1):S67–70.
Huffnagle GB, Noverr MC. The emerging world of the fungal microbiome. Trends Microbiol. 2013;21:334–41.
Cutler JE, Deepe GS Jr, Klein BS. Advances in combating fungal diseases: vaccines on the threshold. Nat Rev Microbiol. 2007;5:13–28.
Brown GD, Denning DW, Gow NA, et al. Hidden killers: human fungal infections. Sci Transl Med. 2012;4:165rv13.
Marr KA. Fungal infections in hematopoietic stem cell transplant recipients. Med Mycol. 2008;46:293–302.
Lionakis MS, Iliev ID, Hohl TM. Immunity against fungi. JCI Insight. 2017;2.
Acosta-Rodriguez EV, Rivino L, Geginat J, et al. Surface phenotype and antigenic specificity of human interleukin 17-producing T helper memory cells. Nat Immunol. 2007;8:639–46.
Becattini S, Latorre D, Mele F, et al. T cell immunity. Functional heterogeneity of human memory CD4(+) T cell clones primed by pathogens or vaccines. Science. 2015;347:400–6.
Bacher P, Heinrich F, Stervbo U, et al. Regulatory T cell specificity directs tolerance versus allergy against aeroantigens in humans. Cell. 2016;167(1067–78):e16.
Borghi M, Renga G, Puccetti M, et al. Antifungal Th Immunity: growing up in Family. Front Immunol. 2014;5:506.
Chen K, Kolls JK. T cell-mediated host immune defenses in the lung. Annu Rev Immunol. 2013;31:605–33.
Eyerich K, Foerster S, Rombold S, et al. Patients with chronic mucocutaneous candidiasis exhibit reduced production of Th17-associated cytokines IL-17 and IL-22. J Invest Dermatol. 2008;128:2640–5.
Ma CS, Chew GY, Simpson N, et al. Deficiency of Th17 cells in hyper IgE syndrome due to mutations in STAT3. J Exp Med. 2008;205:1551–7.
Milner JD, Brenchley JM, Laurence A, et al. Impaired T(H)17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature. 2008;452:773–6.
Okada S, Markle JG, Deenick EK, et al. IMMUNODEFICIENCIES. Impairment of immunity to Candida and Mycobacterium in humans with bi-allelic RORC mutations. Science. 2015;349:606–13.
Puel A, Cypowyj S, Bustamante J, et al. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 2011;332:65–8.
Vinh DC. Insights into human antifungal immunity from primary immunodeficiencies. Lancet Infect Dis. 2011;11:780–92.
de Beaucoudrey L, Samarina A, Bustamante J, et al. Revisiting human IL-12Rbeta1 deficiency: a survey of 141 patients from 30 countries. Medicine (Baltimore). 2010;89:381–402.
Moraes-Vasconcelos D, Grumach AS, Yamaguti A, et al. Paracoccidioides brasiliensis disseminated disease in a patient with inherited deficiency in the beta1 subunit of the interleukin (IL)-12/IL-23 receptor. Clin Infect Dis. 2005;41:e31–7.
Vinh DC, Masannat F, Dzioba RB, et al. Refractory disseminated coccidioidomycosis and mycobacteriosis in interferon-gamma receptor 1 deficiency. Clin Infect Dis. 2009;49:e62–5.
Vinh DC, Schwartz B, Hsu AP, et al. Interleukin-12 receptor beta1 deficiency predisposing to disseminated Coccidioidomycosis. Clin Infect Dis. 2011;52:e99–102.
Zerbe CS, Holland SM. Disseminated histoplasmosis in persons with interferon-gamma receptor 1 deficiency. Clin Infect Dis. 2005;41:e38–41.
Browne SK, Burbelo PD, Chetchotisakd P, et al. Adult-onset immunodeficiency in Thailand and Taiwan. N Engl J Med. 2012;367:725–34.
Lanternier F, Cypowyj S, Picard C, et al. Primary immunodeficiencies underlying fungal infections. Curr Opin Pediatr. 2013;25:736–47.
Rosen LB, Freeman AF, Yang LM, et al. Anti-GM-CSF autoantibodies in patients with cryptococcal meningitis. J Immunol. 2013;190:3959–66.
Bedke T, Iannitti RG, De Luca A, et al. Distinct and complementary roles for Aspergillus fumigatus-specific Tr1 and Foxp3 + regulatory T cells in humans and mice. Immunol Cell Biol. 2014;92:659–70.
Montagnoli C, Fallarino F, Gaziano R, et al. Immunity and tolerance to Aspergillus involve functionally distinct regulatory T cells and tryptophan catabolism. J Immunol. 2006;176:1712–23.
Iannitti RG, Carvalho A, Cunha C, et al. Th17/Treg imbalance in murine cystic fibrosis is linked to indoleamine 2,3-dioxygenase deficiency but corrected by kynurenines. Am J Respir Crit Care Med. 2013;187:609–20.
Sewell AK. Why must T cells be cross-reactive? Nat Rev Immunol. 2012;12:669–77.
Su LF, Han A, McGuire HM, et al. The promised land of human immunology. Cold Spring Harb Symp Quant Biol. 2013;78:203–13.
Potenza L, Vallerini D, Barozzi P, et al. Mucorales-specific T cells in patients with hematologic malignancies. PLoS ONE. 2016;11:e0149108.
el-Dahr JM, Fink R, Selden R, et al. Development of immune responses to Aspergillus at an early age in children with cystic fibrosis. Am J Respir Crit Care Med. 1994;150:1513–8.
Hutcheson PS, Rejent AJ, Slavin RG. Variability in parameters of allergic bronchopulmonary aspergillosis in patients with cystic fibrosis. J Allergy Clin Immunol. 1991;88:390–4.
Nicolai T, Arleth S, Spaeth A, et al. Correlation of IgE antibody titer to Aspergillus fumigatus with decreased lung function in cystic fibrosis. Pediatr Pulmonol. 1990;8:12–5.
Stevens DA, Moss RB, Kurup VP, et al. Allergic bronchopulmonary aspergillosis in cystic fibrosis–state of the art: cystic fibrosis foundation consensus conference. Clin Infect Dis. 2003;37(Suppl 3):S225–64.
Zeaske R, Bruns WT, Fink JN, et al. Immune responses to Aspergillus in cystic fibrosis. J Allergy Clin Immunol. 1988;82:73–7.
Becker KL, Gresnigt MS, Smeekens SP, et al. Pattern recognition pathways leading to a Th2 cytokine bias in allergic bronchopulmonary aspergillosis patients. Clin Exp Allergy. 2015;45:423–37.
Knutsen AP, Slavin RG. Allergic bronchopulmonary aspergillosis in asthma and cystic fibrosis. Clin Dev Immunol. 2011;2011:843763.
King J, Brunel SF, Warris A. Aspergillus infections in cystic fibrosis. J Infect. 2016;72(Suppl):S50–5.
Allen JE, Sutherland TE, Ruckerl D. IL-17 and neutrophils: unexpected players in the type 2 immune response. Curr Opin Immunol. 2015;34:99–106.
Weaver CT, Elson CO, Fouser LA, et al. The Th17 pathway and inflammatory diseases of the intestines, lungs, and skin. Annu Rev Pathol. 2013;8:477–512.
Zelante T, Bozza S, De Luca A, et al. Th17 cells in the setting of Aspergillus infection and pathology. Med Mycol. 2009;47(Suppl 1):S162–9.
Acknowledgements
This work was supported by financial grants from the Cystic Fibrosis Foundation (SCHEFF15G0), the German Federal Ministry of Education and Science (BMBF)–Project InfectControl 2020 (ART4Fun Fkz 03ZZ0813A), the Christiane Herzog Stiftung, Stuttgart, Germany and the Mukoviszidose e.V., Bonn, the German Cystic Fibrosis Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Alexander Scheffold works as a consultant for Miltenyi Biotec who owns IP rights concerning parts of the ARTE technology. Carsten Schwarz and Petra Bacher have no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Scheffold, A., Schwarz, C. & Bacher, P. Fungus-Specific CD4 T Cells as Specific Sensors for Identification of Pulmonary Fungal Infections. Mycopathologia 183, 213–226 (2018). https://doi.org/10.1007/s11046-017-0229-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-017-0229-2