Abstract
Purpose of Review
In this article, we provide a summary of recent findings in the field of host responses to fungal infections caused by the environmental fungi Aspergillus fumigatus and Cryptococcus species. Key myeloid and lymphoid cells that are important in antifungal responses are discussed. The primary leukocytes discussed are macrophages, monocytes, dendritic cells, neutrophils, natural killer cells, and T cells, all of which play roles in conferring protective immunity to these opportunistic pathogens.
Recent Findings
An immunocompromised status is the primary risk factor for Aspergillus- and Cryptococcus-induced morbidities and mortalities, despite the use of current antifungal therapeutics. Research in the past several years has revealed that a variety of immune cell types play critical roles in mounting protection in healthy individuals. The essential effector responses involved in anti-Aspergillus and anti-Cryptococcus immunities differ in several aspects, despite the fact that both are fungi that in humans primarily colonize the pulmonary tissue. Alveolar macrophages and neutrophils comprise the first line of defense that engulfs and eliminates fungi, primarily through the release of free radicals. Monocytes and dendritic cells are the immune sentinels that not only directly eliminate fungi, but also modulate the functions of other immune cells and activate fungus-specific T cells.
Summary
Increased prevalence of immunosuppressive drugs and incidence of diseases such as HIV/AIDS have led to greater numbers of immune-incompetent hosts who are at risk for fatally invasive Aspergillus or Cyrptococcus infections. Elucidating the mechanisms and key immune effectors that combat these infections is crucial for the development of future therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of fungal infections has increased over several decades due to the development of new clinical interventions (therapies or drugs) or diseases (such as HIV) that lead to suppressed host immunity. Patients with impaired immune function can develop life-threatening infections with fungal pathogens that would otherwise be controlled (Fig. 1) [1, 2]. Hence, advances in modern medicine have unintentionally created a niche for fungal pathogens. An additional complicating factor is the rise of drug-resistant fungal strains [2,3,4,5]. In aggregate, fungal infections affect billions of people per year, worldwide, and lead to the death of at least as many people as does tuberculosis or malaria [6,7,8,9,10,11,12]. Despite the detrimental impact of fungal infections to human health, there are no approved vaccines for any fungal pathogen [1, 13]. The successful development of antifungal vaccines could help prevent the high numbers of life-threatening infections as well as potentially benefit the millions of people that contract superficial infections or fungal-related allergies.
Fungal pathogens have the potential to cause disease in a multitude of tissues. Commensal or environmental fungi can become disseminated infections in immunocompromised individuals. Aspergillus fumigatus and Cryptococcus species are two of the most common and clinically relevant environmental fungi capable of causing severe pulmonary disease.
Research efforts to gain new knowledge on the mechanisms utilized by the host to combat fungal infections and the mechanisms that fungi utilize to subvert them will likely facilitate the future development of much needed new therapies. A better understanding of how the host responds to control fungal pathogens is likely to identify host factors that can be exploited in the development of immune-based therapies. The use of combinatorial therapies where immune-based therapies and novel antifungal drugs work alongside to fight fungal infections will be critical to help improve patient outcomes in the future [13].
Given the importance of host immune status to the susceptibility to fungal infections, in this review, we summarize our current understanding of relevant mechanisms of host immunity against fungi. We will focus our discussion to the main cell types involved in the pulmonary immune responses to two major fungal pathogens: Aspergillus fumigatus and the Cryptococcus species. These two pathogens account for the vast majority of the fungal infections worldwide, particularly in immunocompromised hosts [1, 13,14,15,16]. The environmental fungi A. fumigatus and Cryptococcus neoformans are widely distributed around the world. Given the high prevalence of these fungi, it has been estimated that humans are constantly exposed to these fungal pathogens [17, 18]. In the context of normal immune status, this exposure has no detrimental consequences, but if host integrity is compromised, these otherwise minor threats can lead to major life-threatening infections. In this review, we will summarize recent advances in our understanding of the role of specific immune cells in the control of infection with these two clinically important fungal species, with a primary focus on innate immunity. For more in-depth discussions on other relevant aspects of host immunity to fungi, please see recent reviews [19, 20].
Myeloid Responses
Macrophages
Tissue-resident macrophages are a group of heterogeneous immune cells with a range of utilities including homeostatic functions, immune surveillance, and resolution of infection and inflammation. In the lung, alveolar macrophages are specialized tissue macrophages that reside between the airway epithelium and pulmonary vasculature [21, 22]. The functional requirements of macrophages vary from clearance of cellular debris [23] to phagocytosis and elimination of pathogens [24,25,26]. As a result, the plasticity of tissue-resident macrophages is important to maintain a balance of the inflammatory environment and prevent responses to non-pathogenic antigens. At the steady state, alveolar macrophages are poor antigen presenters and can induce T cell tolerance to harmless stimuli [27, 28]. They normally exist in a non-inflammatory state with poor phagocytic capability [29,30,31]. However, the engagement of multiple pattern recognition receptors (PRRs) and the disruption of the structural environment can initiate a more inflammatory state. In this activated inflammatory form, macrophages have greater phagocytic ability and more efficient oxidative burst and secrete pro-inflammatory cytokines to override the inhibited T cell responses [30, 32, 33]. In addition to alveolar macrophages, monocyte-derived “classically” and “alternatively” activated macrophages are also key mediators of host defense and clearance of fungal infection in the lung [34].
Alveolar macrophages are the main phagocytic cells encountered early in Aspergillus infection [35, 36]. Past studies have shown that Aspergillus conidia are engulfed by alveolar macrophages and killed by maturation and acidification of the phagolysosome [36, 37]. The importance of monocyte-derived classically versus alternatively activated macrophages in progressing the pathology of Aspergillus infections is somewhat debatable. One study has shown that alternatively activated macrophages, characterized by fungus-induced expression of arginase-1 and surface expression of CD206, protected against Aspergillus infection [35]. However, PU.1, a transcriptional regulator of alternative polarization of macrophages, has been implicated in the pathological outcome of Aspergillus-induced asthmatic airway inflammation [38, 39]. Moreover, classical macrophages are a potent source of reactive oxygen species and can promote Th1 response [40, 41], both of which have been shown by our studies and others to be helpful in the control of Aspergillus infection [42,43,44,45,46,47,48]. However, as it is becoming more apparent that the distinctions between “classical” and “alternative” are fluid characterizations, it is likely that both macrophage activation states are functionally required for mounting a robust defense against Aspergillus.
Similarly, the subtype diversification of macrophages appears to be highly plastic and adaptable to external signals during cryptococcal infection [49]. A recent study demonstrated that macrophage-dependent STAT1 signaling was critical for limiting uncontrolled inflammation in the lung, regulating an optimal Th1/Th2 response, and NO-dependent protection against H99, a virulent strain of C. neoformans [50]. In contrast to Aspergillus, CD4+ T cells are thought to be the most critical component of intact immunity against Cryptococcus [51]. However, a recent study found that even in the presence of sufficient T cell recruitment, a skewed M2 macrophage polarization led to failure to appropriately phagocytose and eliminate fungal cells, resulting in cryptococcal meningitis in otherwise immunocompetent individuals [52].
Recently, a study also reported the importance of a macrophage-scavenging receptor, MARCO (macrophage receptor with collagenous structure), in modulating the immune response to pulmonary Cryptococcal infection. Expression of MARCO was required for sufficient production of protective cytokines including IFN-γ and IL-12 [53]. In addition, the upregulation of CCR2 chemokine ligands was dependent on MARCO expression; mice lacking MARCO had dampened recruitment and classical activation of monocyte-derived dendritic cells (moDCs) [53]. Finally, interactions between fungal cells and pulmonary macrophages and moDCs were significantly reduced in MARCO−/− cells, resulting in diminished phagocytosis [53]. Altogether, these findings indicate the crucial role of MARCO-expressing macrophages in shaping the early immune response to C. neoformans.
The activation of macrophages by A. fumigatus occurs through the engagement of TLRs 2 and 4 [54], and C-type lectin receptors (CLRs) [55, 56]. The stimulation of TLRs as well as Fc receptors in macrophages triggers a non-canonical autophagy pathway driven by LC3, known as LC3-associated phagocytosis (LAP) [57, 58]. The engulfment of Aspergillus induces formation of a LAPosome which requires the class III PI3(K)-associated protein Rubicon [59]. Mice that either lacked Rubicon or had macrophages with defective LAP machinery were unable to properly clear Aspergillus spores and had greater pulmonary inflammation [59]. Impaired autophagy is exhibited in patients and murine models of chronic granulomatous disease (CGD), a disorder characterized by a lack of intact NADPH-oxidase activity [60, 61]. Patients with CGD are at greater risk of various infections, including invasive pulmonary aspergillosis (IPA) [62, 63]. Both monocytes from CGD patients and lung macrophages from p47 phox−/− mice displayed impaired expression of death-associated protein kinase 1 (DAPK1), a component of LAP [64]. The expression of DAPK1 in wild-type mice was upregulated 4 hours after Aspergillus infection and was dependent on IFN-γ expression. The treatment of Aspergillus-infected p47 phox−/− mice with recombinant IFN-γ restored DAPK1 expression in lung macrophages and controlled fungal growth [64]. LC3-independent autophagy appears to be more important during cryptococcal infection. The disruption of autophagy-related 5 (ATG5) protein in J774.16 cells in vitro inhibited the phagocytosis and restriction of C. neoformans cells. Bone marrow macrophages from atg5 −/− mice pre-activated with IFN-γ and LPS were more permissible to C. neoformans growth. On the other hand, unactivated atg5 −/− macrophages exhibited greater fungicidal activity. These observations suggest a complex role for autophagy in defense against cryptococcal infection, dependent on macrophage type and activation state [65]. Together, these findings demonstrate the importance of the linked macrophage phagocytosis and autophagy pathways in immunity to fungal infections.
Recently, a fucose-binding lectin (FleA) on the surface of Aspergillus has been shown to strongly bind to surface receptors on macrophages [66]. This lectin is one of many pathogen-associated molecular patterns (PAMPs) that become accessible to macrophage CLRs and mannose receptors during the germination of A. fumigatus conidia [55, 66, 67]. One of the most prevalent surface PAMPs on swollen A. fumigatus conidia is β-glucan [55, 67, 68]. Its cognate receptor, dectin-1, is capable of triggering calcineurin- nuclear factor of activated T cell (NFAT) binding in macrophages [69]. Additionally, a dectin-1- and MyD88-independent pathway has recently been found to mediate phagocytosis-dependent immune responses in macrophages. The engagement of TLR9 by Aspergillus spores leads to signaling via Bruton’s tyrosine kinase (BTK) [70]. Signaling through either pathway in turn drives downstream calcineurin-NFAT transcription responses in macrophages, which, in collaboration with NFκB, induces increased expression of TNF-α and IL-2 [70, 71]. Organ transplant patients are often treated with calcineurin inhibitors, which impair this signaling pathway and innate pulmonary responses [72, 73]. Patients treated with calcineurin inhibitors such as cyclosporine A and tacrolimus also displayed impairment in pentraxin-3 function, which was linked with increased susceptibility to aspergillosis and severe invasive aspergillosis (IA)-induced morbidity [71]. Furthermore, a recent report demonstrated that DAP12, an adaptor protein for multiple PRRs, acts as limits pulmonary inflammation during C. neoformans infection. Bone marrow-derived macrophages from DAP12−/− mice displayed improved antifungal function, including improved phagocytosis and increased production of pro-inflammatory cytokines such as TNF [74]. Although DAP12−/− mice eventually succumb to infection [74], this protein may be one potential target of combinatorial therapeutics.
Monocytes and Dendritic Cells
CCR2+, inflammatory monocytes, is also an essential innate cell in the defense against pulmonary infection with A. fumigatus [75,76,77]. The contributions of inflammatory monocytes to antifungal immunity are multifactorial and involve the direct eradication of fungal conidia and the production of protective cytokines. Inflammatory CCR2+ monocytes also assist in the clearance of cryptococcal infection [78, 79]. However, there is some debate whether monocytes may actually propagate C. neoformans infections. Studies have shown that Cryptococcus yeast phagocytosed by macrophages and monocytes may employ a “Trojan horse” mechanism to pass the blood brain barrier, leading to meningoencephalitis [80, 81].
In addition to direct killing of fungi, an intact CCR2+ monocyte compartment is required for a robust antifungal repsonse by neutrophils. It is likely that monocyte-derived factors are required for the activation of optimal neutrophil responses [75]. Indeed, CCR2+ cell ablation leads to diminished expression of IL-1α and CXCL1 24 hours after challenge with Aspergillus conidia and subsequent reduction in early neutrophil recruitment [82]. Recent studies from our lab have further identified CCR2+ monocyte-derived type I interferon (IFN) as an important mechanism of monocyte-dependent regulation of antifungal neutrophil activation [83]. We uncovered an essential role for type I and III IFNs as regulators of neutrophil antifungal activity where both IFNs were required for the efficient production of reactive oxygen species (ROS) [83]. Optimal production of type III IFN required early production of type I IFN by CCR2+ monocytes [83]. Thus, CCR2+ monocytes orchestrate antifungal defense against IA by initiating a coordinated IFN response that further promotes antifungal neutrophil activation [83]. Future studies are likely to further identify monocyte-dependent mechanisms that shape antifungal immunity.
Dendritic cells (DCs) are specialized innate cells originating from hematopoietic progenitors. These highly phagocytic cells are exceptionally proficient in antigen processing and presentation [84]. Subsets of DCs include plasmacytoid dendritic cells (pDCs), classical dendritic cells (cDCs), and moDCs. An in-depth discussion of dendritic cell lineage and diversification can be found in several reviews [84,85,86,87].
moDCs, also known as inflammatory DCs, arise from bone marrow-derived CCR2+ monocytes. During infection, CCR2+ monocytes migrate to the site of inflammation and differentiate into inflammatory DCs [88, 89]. Upon A. fumigatus infection, CCR2+ monocytes are rapidly recruited to the lung and give rise to moDCs that are critical for the activation of fungus-specific CD4 T cells [90]. Upon C. neoformans infection, the lack of CCR2+ cells resulted in diminished recruitment of cDCs to the lung and subsequently impaired Th1 response [91]. Bone marrow-derived DCs primed with a vaccine strain of Cryptococcus gatii were able to confer protective immunity in mice challenged intratracheally with the strain R265 in an IFN-γ-dependent manner [92]. Together, these studies demonstrate the importance of DCs during Cryptococcus infection. Future investigations will need to dissect whether dendritic cells, similar to monocytes, may also play a pathogenic role in the dissemination of Cryptococcus and the potential mechanisms involved in maintaining a sufficiently protective innate response.
In response to Aspergillus, CCR2+ moDCs have been shown to directly engulf and kill conidia. In their absence, mice succumbed to IPA [75]. Furthermore, pDCs were found to display anti-Aspergillus response in a dectin-2-dependent manner. Upon hyphal stimulation, pDCs secrete IFN-α and TNF-α and appear to form pDC extracellular traps [93] that likely confer protection against germinating Aspergillus spores.
Despite in vitro findings that suggest that C. neoformans is a poor activator of pDCs [94], a recent report demonstrated that pDCs can phagocytose C. neoformans cells and inhibit fungal growth. This function was dependent on dectin-3 expression [95]. However, dectin-3 is not required for immunity to C. neoformans, suggesting that pDCs might employ other innate receptors in the defense against C.neoformans or that other DC subsets can compensate for pDC function in protection against pulmonary cryptococcal infection in vivo [96].
Current findings also suggest that monocytes and dendritic cells are critical not only for the direct elimination of A. fumigatus spores, but also in coordinating the response of other effector cells [97]. Notably, in the absence of CCR2+ inflammatory monocytes and moDCs, the conidiacidal activity of neutrophils was diminished [75, 83]. Dendritic cells are also implicated in the control of the balance between protective and pathogenic inflammations. Aspergillus-induced IL-2 and IL-23 secreted by classical CD103+ DCs maintain an optimal Th17 response. In the absence of IL-2, there is unrestricted IL-23-induced Th17 polarization, leading to fatal hyper-inflammation [98].
Dendritic cells recognize A. fumigatus spores via the C-type lectin, dectin-1. When dectin-1 was blocked on human cDCs, there was diminished expression of the T cell co-stimulatory molecules CD40, CD80, and HLA-DR, as well as impaired production of TNF-α and IL-1β [99]. The formation of a phagocytic synapse enables the CLR dectin-1 to recognize of β-glucan on the surface of Aspergillus [100]. Phagocytosis leads to lysosomal processing of the fungi and expression of CD86 and CD83 co-stimulatory markers. Subsequently, mature DCs become efficient antigen-presenting cells and activators of T cell responses. In aggregate, these findings indicate that β-glucan-dependent recognition of Aspergillus is critical for efficient dendritic cell function.
Neutrophils
Neutrophils are the early responders to a variety of pathogens, including bacteria [101, 102], viruses [103, 104], and fungi [75, 105, 106]. Early in their discovery, neutrophils were thought to be simple, short-lived white blood cells that destroyed foreign intruders by “suicide” methods [107]. However, in the last couple of decades, it has become apparent that neutrophils possess several sophisticated mechanisms for detecting and eliminating pathogens. Detailed discussions on the functions of neutrophils during steady state and in inflammatory environments can be found in the following reviews [108,109,110,111].
Neutrophils have long been characterized as important effectors in defense against A. fumigatus. Neutropenia following hematopoietic stem cell transplantation, as well as immuno-therapies that suppress neutrophil function, is a major risk factor for IPA [112]. Neutrophils inhibit invasive fungal disease through the production of ROS and release of proteases via degranulation [113, 114]. In addition, neutrophils extrude nuclear extracellular traps (NETs) that contain peptides including elastases and calprotectin that exert antimicrobial functions in a process known as NETosis [115,116,117]. Signals transduced by both the MyD88 and CARD9 adaptors were shown to be essential for neutrophil-mediated antifungal responses. Defects in either molecule caused delayed or interrupted the expression of neutrophil chemokines CXCL1 and CXCL5, leading to insufficient neutrophil recruitment to the lung, resulting in fatality [56].
During Aspergillus infection, neutrophils are early recruits to the lung. In immunocompetent hosts, neutrophils form complexes with conidia that possess NADPH oxidase activity, thereby inhibiting germination [118]. Using in silico modeling, a recent report demonstrated that 6–17 hours after initial exposure, neutrophil- rather than macrophage-mediated killing of Aspergillus is the dominant conidiacidal response [119]. In addition, iron sequestration by lactoferrin secreted in neutrophilic granules is involved in restricting the initial germination of conidia [120, 121]. Recognition of conidia by neutrophils was found to depend on the integrin CR3. In contrast, detection of hyphae relies on FcγR stimulation by opsonized fungi [121].
Murine models have demonstrated that neutrophils are also essential in limiting hyphal growth in both pulmonary [75, 122, 123] and corneal [124] models of IPA. Neutrophils employ a variety of extracellular mechanisms in order to regulate unrestricted germination. The primary mechanism for destruction of hyphae is mediated by toxic superoxides produced by NADPH oxidase and myeloperoxidase [121]. It has been suggested that ROS derived from longer lived (> 10 hours) neutrophils can act as a sensor of microbe size to induce cytokine production, driving further recruitment of neutrophils and subsequent clustering at the site of hyphal formations [125]. This model challenges the classic paradigm that neutrophils are only short-lived cells that primarily function through apoptotic mechanisms. Non-oxidative mechanisms also play a role in clearing Aspergillus hyphae. The zinc- and manganese-chelating protein, calprotectin, has been shown to inhibit hyphae in a murine model of fungal keratitis [126].
Neutrophils also employ phagocytic mechanisms for killing earlier morphotypes of Aspergillus. Complement-driven phagocytosis and killing of swollen conidia and germ tubes by neutrophils are dependent on opsonization by the serum components C3b and IgG [127]. Leukocyte-intrinsic granulocyte macrophage colony-stimulating factor (GM-CSF) is also required to kill phagocytosed spores by enhancing NADPH oxidase-dependent conidiacidal activity [128]. Not only do neutrophils eradicate Aspergillus through direct mechanisms, but they also interact and synergize with other leukocytes. Importantly, this includes inflammatory monocytes and their derivative cells [75].
As one of the first responders in the lung, neutrophils also have a role in pulmonary Cryptococcal infection. Using live cell imaging, recent studies demonstrated that neutrophils actively migrate towards and rapidly phagocytose C. neoformans cells [129]. The complement factors C5a-C5aR enhance phagocytosis of C. neoformans by stimulating neutrophil upregulation of CD11b. In addition, C5a-C5aR signaling mediates chemotaxis of neutrophils towards Cryptococci via the p38 MAPK pathway [129]. Neutrophils were also shown to be critical in the clearance of disseminated C. neoformans in brain vasculature [130]. However, other studies have suggested the potential deleterious role of neutrophils during Cryptococcal infection. Depletion of neutrophils with anti-GR1 led to extended survival and reduced inflammatory lung damage without reduction in early fungal burden [131]. Moreover, mice with genetically induced neutrophilia seem to have increased susceptibility to pulmonary cryptococcal disease [132]. Further studies are needed to elucidate the implication of enhanced neutrophil recruitment during cryptococcal meningoencephalitis.
Lymphoid Responses
Natural Killer Cells
Natural killer (NK) cells are innate effector cells of lymphoid origin. They were originally found to be important in surveilling and exhibiting cytotoxic activity against tumor cells. They possess specialized receptors that allow them to distinguish healthy cells from those missing or expressing aberrant “self” molecules [133,134,135,136,137]. However, NK cells also have critical roles in immunity against external pathogens. There is strong evidence for activity of NK cells in control of viral and bacterial infections [138,139,140,141]. NK cells are one of the resident cells in the lung. Under steady state, NK cells in the lung are quiescent, tightly regulated by TGF-β and prostaglandins released by alveolar macrophages, and have severely diminished cytotoxic capability [142,143,144]. Upon stimulation with pro-inflammatory cytokines such as type I IFNs, IL-12, and IL-8, NK cells regain their function [142, 145,146,147]. NK cells enact their defensive function through the expression of IFN-γ as well as the degranulation of perforin and other cytotoxic peptides such as serine proteases [142, 145, 147, 148]. The various functions and roles of NK cells are addressed in detail in several reviews [133, 138, 149,150,151]. Here, we briefly discuss a few functions relevant to Aspergillus and Cryptococcus.
There is some evidence for the importance of NK cells in defense against IPA. One study has shown activity of human NK cells against A. fumigatus hyphae, but not conidia [152]. Another group’s findings suggest that human NK cells can kill Aspergillus upon activation by germlings and that this appears to occur through a perforin-independent manner [153]. In a model of neutropenia, NK cells were found to mediate protection from IA suggesting that in the absence of an essential antifungal cell (neutrophils), NK cells can help protect the host against IA [154]. Whether NK cells play essential roles in defense in the presence of neutrophils is unclear. We find that RγC−/− mice, which lack the entire lymphoid lineage (including NK cells), retain protective immunity to A. fumigatus [75, 83]. Thus, in the context of intact myeloid cell responses, the role of NK cells and other lymphoid lineage-derived cells appears to be secondary.
However, several studies have shown corroborating evidence for direct binding and cytotoxic function of NK cells against Cryptococcus [155,156,157,158]. The NKp30 receptor is responsible for anticryptococcal activity by mediating direct fungal binding and perforin release. Interestingly, NK cells from HIV patients had defective polarization of perforin granules and diminished NKp30 expression [159]; treatment with IL-12 restored microbiocidal activity [160]. This is likely caused by augmented NK cell cytotoxicity due to increased expression of activation receptors, including NKp30, and enhanced the release of granule-derived proteases [159, 160].
Primary human NK cells were found to have greater anticryptococcal activity in acidic, rather than physiological, pH [161]. This is unsurprising as NK cells are commonly associated with surveilling in tumor microenvironments [151]. Furthermore, NK cells were also found to be closely associated with C. gattii cells within a cryptococcoma [161]. Altogether, these findings suggest that NK cells provide protective functions against Cryptococcus cells within hypoxic milieus where other immune cells may not be present or as persistently active.
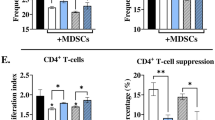
T Cells
The diversity and plasticity of CD4+ T helper cell subsets are critical for mounting robust immune responses to pathogenic challenge. The roles of the various subtypes are described in detail in other reviews [162, 163]; we discuss some functions relevant to Aspergillus and Cryptococcus.
Following the innate response phase, Aspergillus-specific T cells are rapidly primed by antigen-presenting cells in the draining lymph node [164, 165]. The resulting CD4+ T cell response is diverse and consists predominantly of Th1 and a smaller population of Th17 effectors [43, 164]. Dectin-1-mediated signals suppress Th1 and IFN-γ responses and enables Th17 differentiation [43]. Th1 cells are associated with the pro-inflammatory cytokines IFN-γ, IL-12, and TNF-α that not only further shape the CD4+ T cell response, but also enhance the phagocytic and direct antifungal functions of macrophages and monocytes [166]. Immunotherapy with recombinant IFN-γ in patients with invasive fungal infections partially restored cell-mediated antifungal responses [167]. Th17-derived IL-17 has also been found to play a significant role in conferring protective immunity in Aspergillus-driven fungal keratitis [124].
Exaggerated Th2 responses induced by Aspergillus have been associated with pathogenic lung inflammation and allergic disease [168, 169]. Increased chitin-to-β-glucan ratio due to prophylactic caspofungin, an inhibitor of β-glucan synthesis, has been associated with a type 2 cytokine profile and increased eosinophil-induced airway inflammation in mice [170,171,172,173]. Airway eosinophilia in response to a chitin-overexpressing environmental isolate was considerably diminished in mice lacking γδ+ T cells [174]. Furthermore, TCRγδ−/− mice exhibited greater protective response to Aspergillus, resulting in decreased fungal burden and pulmonary eosinophilia [173]. These observations indicate the importance of cell wall components in shaping the immune response to A. fumigatus and identify γδ+ T cells as potential regulators of pathogenic lung inflammation. During acute cryptococcal infection, γδ+ T cells accumulate in the lung [175]; however, their exact role remains unclear. One study reported a protective function of IL-17-producing γδ+ T cells in a neutropenic model of cryptococcal infection [176], while another observed enhanced fungal clearance and beneficial Th1 response in TCRγδ−/− mice [175].
CD4+ T cells are fundamental in immunity against Cryptococcus. This is illustrated by the high incidence of cryptococcosis in patients suffering from HIV/AIDS [177,178,179]. Impaired clearance of Cryptococcus is associated with significantly reduced CD4+ and CD8+ T cell numbers [51, 180]. Both CD4+ and CD8+ T cells contribute to response to pulmonary Cryptococcus; their respective roles are discussed in detail in previous reviews [180, 181]. CD4+ T cells play a dominant role in chemotaxis and activation of macrophages and granulocytes to the lung [182, 183]. Cryptococcus-specific CD4+ T cells are important sources of macrophage inflammatory proteins 1α, IFN-γ, and TNF-α [180, 184,185,186]. In a recent clinical study of patients with HIV-associated cryptococcal meningitis, 25% of individuals with low IFN-γ and TNF-α- responses succumbed to the infection, while those with intact signaling survived [184]. Another report found that in HIV/AIDS patients, a protective immune response was associated with the presence of IL-17 and IFN-γ. Patients with even a minimal Cryptococcus-specific Th1 profile had faster fungal clearance from the CNS [187]. While C. neoformans primarily affects immunocompromised individuals, C. gatii is more commonly reported in immunocompetent hosts [188]. This species is suspected to be capable of dampening the Th1/Th17 response, thereby increasing the susceptibility of an otherwise healthy host to systemic cryptococcosis [189]. In aggregate, these studies highlight the relevance of CD4+ T cells, especially Th1-derived IFN-γ, as essential contributors to protective immunity against Cryptococcus.
Concluding Remarks
Fungal pathogens are major causes of morbidity and mortality in immunocompromised patients despite the use of current antifungal chemotherapeutics. Cryptococcus species and A. fumigatus comprise some of the most common fungal pathogens that humans can be exposed to. Over the last several years, research efforts have begun unraveling the cellular mechanisms that mediate protective immunity against these species. Understanding these mechanisms is key for the development of more effective therapeutics in the future. Ongoing research in this area continues to provide exciting new knowledge on relevant mechanisms of antifungal defense that could be developed into effective immunotherapies.
References
Brown GD, Denning DW, Levitz SM. Tackling human fungal infections. Science. 2012;336(6082):647.
Mortensen KL, et al. Environmental study of azole-resistant Aspergillus fumigatus and other Aspergilli in Austria, Denmark, and Spain. Antimicrob Agents Chemother. 2010;54(11):4545–9.
Bader O, et al. cyp51A-based mechanisms of Aspergillus fumigatus azole drug resistance present in clinical samples from Germany. Antimicrob Agents Chemother. 2013;57(8):3513–7.
Orni-Wasserlauf R, et al. Fluconazole-resistant Cryptococcus neoformans isolated from an immunocompetent patient without prior exposure to fluconazole. Clin Infect Dis. 1999;29(6):1592–3.
Ashu EE, et al., Global population genetic analysis of Aspergillus fumigatus. mSphere, 2017. 2(1).
Park BJ, et al. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23(4):525–30.
Pegues CF, Daar ES, Murthy AR. The epidemiology of invasive pulmonary aspergillosis at a large teaching hospital. Infect Control Hosp Epidemiol. 2001;22(6):370–4.
Cryptococcal meningitis. 2015 [cited 2017; Available from: http://www.life-worldwide.org/cryptococcal-meningitis1/.
Chronic pulmonary aspergillosis. 2015 [cited 2017; Available from: http://www.life-worldwide.org/chronic-pulmonary-aspergillosis1/.
Wald A, et al. Epidemiology of Aspergillus infections in a large cohort of patients undergoing bone marrow transplantation. J Infect Dis. 1997;175(6):1459–66.
WHO: malaria fact sheet. 2017 [cited 2017; Available from: http://www.who.int/mediacentre/factsheets/fs094/en/.
WHO: tuberculosis fact sheet. 2017.
Brown GD, et al. Hidden killers: human fungal infections. Sci Transl Med. 2012;4(165):165rv13.
Pfaller MA, Pappas PG, Wingard JR. Invasive fungal pathogens: current epidemiological trends. Clin Infect Dis. 2006;43(Supplement_1):S3–S14.
Mirza SA, et al. The changing epidemiology of cryptococcosis: an update from population-based active surveillance in 2 large metropolitan areas, 1992-2000. Clin Infect Dis. 2003;36(6):789–94.
Rajasingham R, et al. Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis. Lancet Infect Dis. 2017;17(8):873–81.
Latgé J-P. Aspergillus fumigatus and aspergillosis. Clin Microbiol Rev. 1999;12(2):310–50.
Nosanchuk JD, et al. Evidence that Cryptococcus neoformans is melanized in pigeon excreta: implications for pathogenesis. Infect Immun. 1999;67(10):5477–9.
Espinosa V, Rivera A. First line of defense: innate cell-mediated control of pulmonary aspergillosis. Front Microbiol. 2016;7:272.
Marcos CM, et al. Anti-immune strategies of pathogenic fungi. Front Cell Infect Microbiol. 2016;6:142.
Holt PG, et al. Downregulation of the antigen presenting cell function(s) of pulmonary dendritic cells in vivo by resident alveolar macrophages. J Exp Med. 1993;177(2):397.
Landsman L, Jung S. Lung macrophages serve as obligatory intermediate between blood monocytes and alveolar macrophages. J Immunol. 2007;179(6):3488.
Dubuisson L, et al. Removal of cellular debris formed in the Disse space in patients with cholestasis. Virchows Archiv A. 1987;410(6):501–7.
Liang Z, et al. Impaired macrophage phagocytosis of bacteria in severe asthma. Respir Res. 2014;15(1):72.
Koziel J, et al. Phagocytosis of Staphylococcus aureus by macrophages exerts cytoprotective effects manifested by the upregulation of antiapoptotic factors. PLoS One. 2009;4(4):e5210.
Nicola AM, Casadevall A, Goldman DL. Fungal killing by mammalian phagocytic cells. Curr Opin Microbiol. 2008;11(4):313–7.
Blumenthal RL, et al. Human alveolar macrophages induce functional inactivation in antigen-specific CD4 T cells. J Allergy Clin Immunol. 2001;107(2):258–64.
Mathie SA, et al. Alveolar macrophages are sentinels of murine pulmonary homeostasis following inhaled antigen challenge. Allergy. 2015;70(1):80–9.
Hussell T, Bell TJ. Alveolar macrophages: plasticity in a tissue-specific context. Nat Rev Immunol. 2014;14(2):81–93.
Kopf M, Schneider C, Nobs SP. The development and function of lung-resident macrophages and dendritic cells. Nat Immunol. 2015;16(1):36–44.
Gardai SJ, et al. By binding SIRPα or calreticulin/CD91, lung collectins act as dual function surveillance molecules to suppress or enhance inflammation. Cell. 2003;115(1):13–23.
Westphalen K, et al. Sessile alveolar macrophages communicate with alveolar epithelium to modulate immunity. Nature. 2014;506(7489):503–6.
Saas P, et al. Mediators involved in the immunomodulatory effects of apoptotic cells. Transplantation. 2007;84(1 Suppl):S31–4.
Leopold Wager CM, Wormley FL Jr. Classical versus alternative macrophage activation: the ying and the yang in host defense against pulmonary fungal infections. Mucosal Immunol. 2014;7(5):1023–35.
Bhatia S, et al. Rapid host defense against Aspergillus fumigatus involves alveolar macrophages with a predominance of alternatively activated phenotype. PLoS One. 2011;6(1):e15943.
Philippe B, et al. Killing of Aspergillus fumigatus by alveolar macrophages is mediated by reactive oxidant intermediates. Infect Immun. 2003;71(6):3034–42.
Ibrahim-Granet O, et al. Phagocytosis and intracellular fate of Aspergillus fumigatus conidia in alveolar macrophages. Infect Immun. 2003;71(2):891–903.
Qian F, et al. The transcription factor PU.1 promotes alternative macrophage polarization and asthmatic airway inflammation. J Mol Cell Biol. 2015;7(6):557–67.
Hoppenot D, et al. p-STAT6, PU.1, and NF-kappaB are involved in allergen-induced late-phase airway inflammation in asthma patients. BMC Pulm Med. 2015;15:122.
Mills CD, et al. M-1/M-2 macrophages and the Th1/Th2 Paradigm. J Immunol. 2000;164(12):6166.
Covarrubias A, Byles V, Horng T. ROS sets the stage for macrophage differentiation. Cell Res. 2013;23(8):984–5.
Rivera A, et al. Distinct CD4(+)-T-cell responses to live and heat-inactivated Aspergillus fumigatus conidia. Infect Immun. 2005;73(11):7170–9.
Rivera A, et al. Dectin-1 diversifies Aspergillus fumigatus–specific T cell responses by inhibiting T helper type 1 CD4 T cell differentiation. J Exp Med. 2011;208(2):369.
Chai LY, et al. Anti-Aspergillus human host defence relies on type 1 T helper (Th1), rather than type 17 T helper (Th17), cellular immunity. Immunology. 2010;130(1):46–54.
Fukahori S, et al. Clearance of Aspergillus fumigatus is impaired in the airway in allergic inflammation. Ann Allergy Asthma Immunol. 2014;113(2):180–6.
Stuehler C, et al. Cross-protective TH1 immunity against Aspergillus fumigatus and Candida albicans. Blood. 2011;117(22):5881–91.
Tramsen L, et al. Immunosuppressive compounds exhibit particular effects on functional properties of human anti-Aspergillus Th1 cells. Infect Immun. 2014;82(6):2649–56.
Porter PC, et al. Necessary and sufficient role for T helper cells to prevent fungal dissemination in allergic lung disease. Infect Immun. 2011;79(11):4459–71.
Davis MJ, et al. Macrophage M1/M2 polarization dynamically adapts to changes in cytokine microenvironments in Cryptococcus neoformans infection. MBio. 2013;4(3):e00264–13.
Leopold Wager CM, et al. STAT1 signaling within macrophages is required for antifungal activity against Cryptococcus neoformans. Infect Immun. 2015;83(12):4513–27.
Akakpo KP, Quayson SE, Lartey M. Disseminated cryptococcosis in a patient with HIV/AIDS at a teaching hospital in Ghana. SAGE Open Med Case Reports. 2015;3:2050313X14565421.
Panackal AA, et al. Paradoxical immune responses in non-HIV cryptococcal meningitis. PLoS Pathog. 2015;11(5):e1004884.
Xu J, et al. Scavenger receptor MARCO orchestrates early defenses and contributes to fungal containment during cryptococcal infection. J Immunol. 2017;198(9):3548.
Meier A, et al. Toll-like receptor (TLR) 2 and TLR4 are essential for Aspergillus-induced activation of murine macrophages. Cell Microbiol. 2003;5(8):561–70.
Hohl TM, et al. Aspergillus fumigatus triggers inflammatory responses by stage-specific β-glucan display. PLoS Pathog. 2005;1(3):e30.
Jhingran A, et al. Compartment-specific and sequential role of MyD88 and CARD9 in chemokine induction and innate defense during respiratory fungal infection. PLoS Pathog. 2015;11(1):e1004589.
Sanjuan MA, et al. Toll-like receptor signalling in macrophages links the autophagy pathway to phagocytosis. Nature. 2007;450(7173):1253–7.
Kim J-Y, et al. Noncanonical autophagy promotes the visual cycle. Cell. 2013;154(2):365–76.
Martinez J, et al. Molecular characterization of LC3-associated phagocytosis reveals distinct roles for Rubicon, NOX2 and autophagy proteins. Nat Cell Biol. 2015;17(7):893–906.
de Luca A, et al. IL-1 receptor blockade restores autophagy and reduces inflammation in chronic granulomatous disease in mice and in humans. Proc Natl Acad Sci U S A. 2014;111(9):3526–31.
van de Veerdonk FL, Dinarello CA. Deficient autophagy unravels the ROS paradox in chronic granulomatous disease. Autophagy. 2014;10(6):1141–2.
Liese J, et al. Long-term follow-up and outcome of 39 patients with chronic granulomatous disease. J Pediatr. 2000;137(5):687–93.
Winkelstein JA, et al. Chronic granulomatous disease. Report on a national registry of 368 patients. Medicine (Baltimore). 2000;79(3):155–69.
Oikonomou V, et al. Noncanonical fungal autophagy inhibits inflammation in response to IFN-γ via DAPK1. Cell Host Microbe. 2016;20(6):744–57.
Nicola AM, et al. Macrophage autophagy in immunity to Cryptococcus neoformans and Candida albicans. Infect Immun. 2012;80(9):3065–76.
Kerr SC, et al. FleA expression in Aspergillus fumigatus is recognized by fucosylated structures on mucins and macrophages to prevent lung infection. PLoS Pathog. 2016;12(4):e1005555.
Steele C, et al. The beta-glucan receptor dectin-1 recognizes specific morphologies of aspergillus fumigatus. PLoS Pathog. 2005;1(4):e42.
Erwig LP, Gow NAR. Interactions of fungal pathogens with phagocytes. Nat Rev Micro. 2016;14(3):163–76.
Goodridge HS, Simmons RM, Underhill DM. Dectin-1 stimulation by Candida albicans yeast or zymosan triggers NFAT activation in macrophages and dendritic cells. J Immunol. 2007;178(5):3107.
Herbst S, et al. Phagocytosis-dependent activation of a TLR9–BTK–calcineurin–NFAT pathway co-ordinates innate immunity to Aspergillus fumigatus. EMBO Mol Med. 2015;7(3):240.
Zelante T, et al. Impaired calcineurin signaling in myeloid cells results in downregulation of pentraxin-3 and increased susceptibility to aspergillosis. Mucosal Immunol. 2017;10(2):470–80.
Flechner SM, Kobashigawa J, Klintmalm G. Calcineurin inhibitor-sparing regimens in solid organ transplantation: focus on improving renal function and nephrotoxicity. Clin Transpl. 2008;22(1):1–15.
Scheffert JL, Raza K. Immunosuppression in lung transplantation. J Thoracic Dis. 2014;6(8):1039–53.
Heung LJ, Hohl TM. DAP12 inhibits pulmonary immune responses to Cryptococcus neoformans. Infect Immun. 2016;84(6):1879–86.
Espinosa V, et al. Inflammatory monocytes orchestrate innate antifungal immunity in the lung. PLoS Pathog. 2014;10(2):e1003940.
Blease K, et al. Enhanced pulmonary allergic responses to Aspergillus in CCR2−/− mice. J Immunol. 2000;165(5):2603–11.
Serbina NV, et al. Distinct responses of human monocyte subsets to Aspergillus fumigatus conidia. J Immunol (Baltimore, Md : 1950). 2009;183(4):2678–87.
Osterholzer JJ, et al. Accumulation of CD11b+ lung dendritic cells in response to fungal infection results from the CCR2-mediated recruitment and differentiation of Ly-6Chigh monocytes. J Immunol. 2009;183(12):8044–53.
Osterholzer JJ, et al. Chemokine receptor 2-mediated accumulation of fungicidal exudate macrophages in mice that clear cryptococcal lung infection. Am J Pathol. 2011;178(1):198–211.
He X, et al. CD44-mediated monocyte transmigration across Cryptococcus neoformans-infected brain microvascular endothelial cells is enhanced by HIV-1 gp41-I90 ectodomain. J Biomed Sci. 2016;23:28.
Santiago-Tirado FH, et al. Trojan horse transit contributes to blood-brain barrier crossing of a eukaryotic pathogen. MBio. 2017;8(1):e02183.
Caffrey AK, et al. IL-1α signaling is critical for leukocyte recruitment after pulmonary Aspergillus fumigatus challenge. PLoS Pathog. 2015;11(1):e1004625.
Espinosa, V., et al., Type III interferon is a critical regulator of innate antifungal immunity Science Immunology 2017. In press Oct 7 2017.
Mildner A, Jung S. Development and function of dendritic cell subsets. Immunity. 40(5):642–56.
Merad M, et al. The dendritic cell lineage: ontogeny and function of dendritic cells and their subsets in the steady state and the inflamed setting. Annu Rev Immunol. 2013;31(1):563–604.
Guilliams M, et al. Dendritic cells, monocytes and macrophages: a unified nomenclature based on ontogeny. Nat Rev Immunol. 2014;14(8):571–8.
Audiger C, et al. The importance of dendritic cells in maintaining immune tolerance. J Immunol. 2017;198(6):2223.
Hespel C, Moser M. Role of inflammatory dendritic cells in innate and adaptive immunity. Eur J Immunol. 2012;42(10):2535–43.
Naik SH, et al. Intrasplenic steady-state dendritic cell precursors that are distinct from monocytes. Nat Immunol. 2006;7(6):663–71.
Hohl TM, et al. Inflammatory monocytes facilitate adaptive CD4 T cell responses during respiratory fungal infection. Cell Host Microbe. 2009;6(5):470–81.
Osterholzer JJ, et al. CCR2 mediates conventional dendritic cell recruitment and the formation of bronchovascular mononuclear cell infiltrates in the lungs of mice infected with Cryptococcus neoformans. J Immunol. 2008;181(1):610–20.
Ueno K, et al. Dendritic cell-based immunization ameliorates pulmonary infection with highly virulent Cryptococcus gattii. Infect Immun. 2015;83(4):1577–86.
Loures FV, et al. Recognition of Aspergillus fumigatus hyphae by human plasmacytoid dendritic cells is mediated by dectin-2 and results in formation of extracellular traps. PLoS Pathog. 2015;11(2):e1004643.
Siegemund S, Alber G. Cryptococcus neoformans activates bone marrow-derived conventional dendritic cells rather than plasmacytoid dendritic cells and down-regulates macrophages. FEMS Immunol Med Microbiol. 2008;52(3):417–27.
Hole CR, et al. Antifungal activity of plasmacytoid dendritic cells against Cryptococcus neoformans in vitro requires expression of dectin-3 (CLEC4D) and reactive oxygen species. Infect Immun. 2016;84(9):2493–504.
Campuzano A, et al. Dectin-3 is not required for protection against Cryptococcus neoformans infection. PLoS One. 2017;12(1):e0169347.
Rivera A, et al. Innate cell communication kick-starts pathogen-specific immunity. Nat Immunol. 2016;17(4):356–63.
Zelante T, et al. CD103(+) dendritic cells control Th17 cell function in the lung. Cell Rep. 2015;12(11):1789–801.
Hefter M, et al. Human primary myeloid dendritic cells interact with the opportunistic fungal pathogen Aspergillus fumigatus via the C-type lectin receptor Dectin-1. Med Mycol. 2017;55(5):573–8.
Goodridge HS, et al. Activation of the innate immune receptor Dectin-1 upon formation of a “phagocytic synapse”. Nature. 2011;472(7344):471–5.
Tateda K, et al. Chemokine-dependent neutrophil recruitment in a murine model of Legionella pneumonia: potential role of neutrophils as immunoregulatory cells. Infect Immun. 2001;69(4):2017–24.
Hajishengallis G, et al. Importance of TLR2 in early innate immune response to acute pulmonary infection with Porphyromonas gingivalis in mice. J Immunol. 2008;181(6):4141.
Galani IE, Andreakos E. Neutrophils in viral infections: current concepts and caveats. J Leukoc Biol. 2015;98(4):557–64.
Tate MD, et al. Neutrophils ameliorate lung injury and the development of severe disease during influenza infection. J Immunol. 2009;183(11):7441.
Bruns S, et al. Production of extracellular traps against Aspergillus fumigatus in vitro and in infected lung tissue is dependent on invading neutrophils and influenced by hydrophobin RodA. PLoS Pathog. 2010;6(4):e1000873.
Todeschini G, et al. Invasive aspergillosis in neutropenic patients: rapid neutrophil recovery is a risk factor for severe pulmonary complications. Eur J Clin Investig. 1999;29(5):453–7.
Janeway CA Jr, Travers P, Walport M, et al. The front line of host defense, in Immunobiology: the immune system in health and disease. New York: Garland Science; 2001.
Amulic B, et al. Neutrophil function: from mechanisms to disease. Annu Rev Immunol. 2012;30(1):459–89.
Mócsai A. Diverse novel functions of neutrophils in immunity, inflammation, and beyond. J Exp Med. 2013;210(7):1283.
Nauseef WM, Borregaard N. Neutrophils at work. Nat Immunol. 2014;15(7):602–11.
Witter AR, Okunnu BM, Berg RE. The essential role of neutrophils during infection with the intracellular bacterial pathogen Listeria monocytogenes. J Immunol. 2016;197(5):1557.
Imbert S, et al. Calcineurin inhibitors impair neutrophil activity against Aspergillus fumigatus in allogeneic hematopoietic stem cell transplant recipients. J Allergy Clin Immunol. 2016;138(3):860–8.
Bonfim-Mendonça PDS, et al. β-Glucan induces reactive oxygen species production in human neutrophils to improve the killing of Candida albicans and Candida glabrata isolates from vulvovaginal candidiasis. PLoS One. 2014;9(9):e107805.
Reeves EP, et al. Killing activity of neutrophils is mediated through activation of proteases by K+ flux. Nature. 2002;416(6878):291–7.
Tkalcevic J, et al. Impaired immunity and enhanced resistance to endotoxin in the absence of neutrophil elastase and cathepsin G. Immunity. 2000;12(2):201–10.
Branzk N, et al. Neutrophils sense microbe size and selectively release neutrophil extracellular traps in response to large pathogens. Nat Immunol. 2014;15(11):1017–25.
Urban CF, et al. Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog. 2009;5(10):e1000639.
Bonnett CR, et al. Early neutrophil recruitment and aggregation in the murine lung inhibit germination of Aspergillus fumigatus Conidia. Infect Immun. 2006;74(12):6528–39.
Tanaka RJ, et al. In silico modeling of spore inhalation reveals fungal persistence following low dose exposure. Sci Rep. 2015;5:13958.
Zarember KA, et al. Human polymorphonuclear leukocytes inhibit Aspergillus fumigatus conidial growth by lactoferrin-mediated iron depletion. J Immunol. 2007;178(10):6367.
Gazendam RP, et al. Human neutrophils use different mechanisms to kill Aspergillus fumigatus conidia and hyphae: evidence from phagocyte defects. J Immunol. 2016;196(3):1272.
Stephens-Romero SD, Mednick AJ, Feldmesser M. The pathogenesis of fatal outcome in murine pulmonary aspergillosis depends on the neutrophil depletion strategy. Infect Immun. 2005;73(1):114–25.
Mircescu MM, et al. Essential role for neutrophils but not alveolar macrophages at early time points following Aspergillus fumigatus infection. J Infect Dis. 2009;200(4):647–56.
Taylor PR, et al. Aspergillus and Fusarium corneal infections are regulated by Th17 cells and IL-17-producing neutrophils. J Immunol. 2014;192(7):3319–27.
Warnatsch A, et al. Reactive oxygen species localization programs inflammation to clear microbes of different size. Immunity. 46(3):421–32.
Clark HL, et al. Zinc and manganese chelation by neutrophil S100A8/A9 (calprotectin) limits extracellular Aspergillus fumigatus; hyphal growth and corneal infection. J Immunol. 2015;196(1):336.
Braem SGE, et al. Effective neutrophil phagocytosis of Aspergillus fumigatus is mediated by classical pathway complement activation. J Innate Immun. 2015;7(4):364–74.
Kasahara S, et al. Role of granulocyte-macrophage colony-stimulating factor signaling in regulating neutrophil antifungal activity and the oxidative burst during respiratory fungal challenge. J Infect Dis. 2016;213(8):1289–98.
Sun D, et al. Real-time imaging of interactions of neutrophils with Cryptococcus neoformans demonstrates a crucial role of complement C5a-C5aR signaling. Infect Immun. 2015;84(1):216–29.
Sun D, et al. Intravascular clearance of disseminating Cryptococcus neoformans in the brain can be improved by enhancing neutrophil recruitment in mice. Eur J Immunol. 2016;46(7):1704–14.
Mednick AJ, et al. Neutropenia alters lung cytokine production in mice and reduces their susceptibility to pulmonary cryptococcosis. Eur J Immunol. 2003;33(6):1744–53.
Wiesner DL, et al. Different lymphocyte populations direct dichotomous eosinophil or neutrophil responses to pulmonary Cryptococcus infection. J Immunol. 2017;198(4):1627–37.
Vivier E, et al. Functions of natural killer cells. Nat Immunol. 2008;9(5):503–10.
Jamieson AM, et al. The role of the NKG2D immunoreceptor in immune cell activation and natural killing. Immunity. 2002;17(1):19–29.
Öberg L, et al. Loss or mismatch of MHC class I is sufficient to trigger NK cell-mediated rejection of resting lymphocytes in vivo—role of KARAP/DAP12-dependent and -independent pathways. Eur J Immunol. 2004;34(6):1646–53.
Ohlen C, et al. Prevention of allogeneic bone marrow graft rejection by H-2 transgene in donor mice. Science. 1989;246(4930):666.
Bauer S, et al. Activation of NK cells and T cells by NKG2D, a receptor for stress-inducible MICA. Science. 1999;285(5428):727–9.
Scully E, Alter G. NK cells in HIV disease. Curr HIV/AIDS Rep. 2016;13:85–94.
Hall LJ, et al. Natural killer cells protect against mucosal and systemic infection with the enteric pathogen Citrobacter rodentium. Infect Immun. 2013;81(2):460–9.
Junqueira-Kipnis AP, et al. NK cells respond to pulmonary infection with Mycobacterium tuberculosis, but play a minimal role in protection. J Immunol. 2003;171(11):6039–45.
Lam VC, Lanier LL. NK cells in host responses to viral infections. Curr Opin Immunol. 2017;44:43–51.
Robinson BW, Pinkston P, Crystal RG. Natural killer cells are present in the normal human lung but are functionally impotent. J Clin Invest. 1984;74(3):942–50.
Bordignon C, et al. Inhibition of natural killer activity by human bronchoalveolar macrophages. J Immunol. 1982;129(2):587–91.
Wang J, et al. Lung natural killer cells in mice: phenotype and response to respiratory infection. Immunology. 2012;137(1):37–47.
Hwang I, et al. Activation mechanisms of natural killer cells during influenza virus infection. PLoS One. 2013;7(12):e51858.
Reading PC, et al. IL-18, but not IL-12, regulates NK cell activity following intranasal herpes simplex virus type 1 infection. J Immunol. 2007;179(5):3214.
Nguyen QT, et al. Role of interleukin-12 in protection against pulmonary infection with methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2015;59(10):6308–16.
Trapani JA, et al. Granule serine proteases are normal nuclear constituents of natural killer cells. J Biol Chem. 1994;269(28):18359–65.
Cerwenka A, Lanier LL. Natural killer cell memory in infection, inflammation and cancer. Nat Rev Immunol. 2016;16(2):112–23.
Culley FJ. Natural killer cells in infection and inflammation of the lung. Immunology. 2009;128(2):151–63.
Waldhauer I, Steinle A. NK cells and cancer immunosurveillance. Oncogene. 2008;27(45):5932–43.
Schmidt S, et al. Human natural killer cells exhibit direct activity against Aspergillus fumigatus hyphae, but not against resting conidia. J Infect Dis. 2011;203(3):430–5.
Bouzani M, et al. Human natural killer cells are able to kill Aspergillus fumigatus; but not via the perforin-granzyme pathway. Blood. 2015;114(22):1640.
Morrison BE, et al. Chemokine-mediated recruitment of NK cells is a critical host defense mechanism in invasive aspergillosis. J Clin Invest. 2003;112(12):1862–70.
Hidore MR, et al. Murine natural killer cells are fungicidal to Cryptococcus neoformans. Infect Immun. 1991;59(5):1747–54.
Levitz SM, et al. Mechanisms of inhibition of Cryptococcus neoformans by human lymphocytes. Infect Immun. 1995;63(9):3550–4.
Jones GJ, et al. In contrast to anti-tumor activity, YT cell and primary NK cell cytotoxicity for Cryptococcus neoformans bypasses LFA-1. Int Immunol. 2009;21(4):423–32.
Marr KJ, et al. Cryptococcus neoformans directly stimulates perforin production and rearms NK cells for enhanced anticryptococcal microbicidal activity. Infect Immun. 2009;77(6):2436–46.
Li SS, et al. The NK receptor NKp30 mediates direct fungal recognition and killing and is diminished in NK cells from HIV-infected patients. Cell Host Microbe. 2013;14(4):387–97.
Kyei SK, et al. Mechanisms by which interleukin-12 corrects defective nk cell anticryptococcal activity in HIV-infected patients. MBio. 2016;7(4):e00878–16.
Islam A, et al. An acidic microenvironment increases nk cell killing of Cryptococcus neoformans and Cryptococcus gattii by enhancing perforin degranulation. PLoS Pathog. 2013;9(7):e1003439.
Caza T, Landas S. Functional and phenotypic plasticity of CD4+ T cell subsets. Biomed Res Int. 2015;2015:13.
van de Veerdonk FL, Netea MG. T-cell subsets and antifungal host defenses. Curr Fungal Infect Rep. 2010;4(4):238–43.
Rivera A, et al. Innate immune activation and CD4+ T cell priming during respiratory fungal infection. Immunity. 2006;25(4):665–75.
Rivera A, et al. Distinct CD4+−T-cell responses to live and heat-inactivated Aspergillus fumigatus conidia. Infect Immun. 2005;73(11):7170–9.
Thakur R, et al. Cytokines induce effector T-helper cells during invasive aspergillosis; what we have learned about T-helper cells? Front Microbiol. 2015;6:429.
Delsing CE, et al. Interferon-gamma as adjunctive immunotherapy for invasive fungal infections: a case series. BMC Infect Dis. 2014;14(1):166.
Becker KL, et al. Pattern recognition pathways leading to a Th2 cytokine bias in allergic bronchopulmonary aspergillosis patients. Clin Exp Allergy. 2015;45(2):423–37.
Allard JB, et al. Aspergillus fumigatus generates an enhanced Th2-biased immune response in mice with defective cystic fibrosis transmembrane conductance regulator. J Immunol. 2006;177(8):5186–94.
Da Silva CA, et al. Chitin is a size-dependent regulator of macrophage TNF and IL-10 production. J Immunol. 2009;182(6):3573–82.
Walker LA, et al. Caspofungin treatment of Aspergillus fumigatus results in ChsG-dependent upregulation of chitin synthesis and the formation of chitin-rich microcolonies. Antimicrob Agents Chemother. 2015;59(10):5932–41.
Kim LK, et al. AMCase is a crucial regulator of type 2 immune responses to inhaled house dust mites. Proc Natl Acad Sci U S A. 2015;112(22):E2891–9.
Amarsaikhan N, et al. Caspofungin increases fungal chitin and eosinophil and γδ T cell–dependent pathology in invasive Aspergillosis. J Immunol. 2017;199:624–32.
Amarsaikhan N, et al. Lung eosinophil recruitment in response to Aspergillus fumigatus is correlated with fungal cell wall composition and requires gammadelta T cells. Microbes Infect. 2017;19(7–8):422–31.
Uezu K, et al. Accumulation of γδ T cells in the lungs and their regulatory roles in th1 response and host defense against pulmonary infection with Cryptococcus neoformans. J Immunol. 2004;172(12):7629.
Wozniak KL, Kolls JK, Wormley FL. Depletion of neutrophils in a protective model of pulmonary cryptococcosis results in increased IL-17A production by gamma/delta T cells. BMC Immunol. 2012;13(1):65.
Mwaba P, et al. Clinical presentation, natural history, and cumulative death rates of 230 adults with primary cryptococcal meningitis in Zambian AIDS patients treated under local conditions. Postgrad Med J. 2001;77(914):769–73.
Baldassarre R, et al. Mortality after clinical management of aids-associated cryptococcal meningitis in Kenya. East Afr Med J. 2014;91(5):145–51.
Williamson PR. The relentless march of cryptococcal meningitis. Lancet Infect Dis. 2017;17(8):790–1.
Huffnagle GB, et al. The role of CD4+ and CD8+ T cells in the protective inflammatory response to a pulmonary cryptococcal infection. J Leukoc Biol. 1994;55(1):35–42.
Chen K, Kolls JK. T cell-mediated host immune defenses in the lung. Annu Rev Immunol. 2013;31:605–33.
Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8(12):958–69.
Kalyan S, Kabelitz D. When neutrophils meet T cells: beginnings of a tumultuous relationship with underappreciated potential. Eur J Immunol. 2014;44(3):627–33.
Jarvis JN, et al. The phenotype of the Cryptococcus-specific CD4(+) memory T-cell response is associated with disease severity and outcome in hiv-associated cryptococcal meningitis. J Infect Dis. 2013;207(12):1817–28.
Hoag KA, et al. IL-12 and IFN-gamma are required for initiating the protective Th1 response to pulmonary cryptococcosis in resistant C.B-17 mice. Am J Respir Cell Mol Biol. 1997;17(6):733–9.
Wozniak KL, et al. Induction of protective immunity against cryptococcosis. Mycopathologia. 2012;173(5–6):387–94.
Jarvis JN, et al. Cerebrospinal fluid cytokine profiles predict risk of early mortality and immune reconstitution inflammatory syndrome in HIV-associated cryptococcal meningitis. PLoS Pathog. 2015;11(4):e1004754.
Kwon-Chung KJ, et al. Cryptococcus neoformans and Cryptococcus gattii, the etiologic agents of cryptococcosis. Cold Spring Harb Perspect Med. 2014;4(7):a019760.
Angkasekwinai P, et al. Cryptococcus gattii infection dampens Th1 and Th17 responses by attenuating dendritic cell function and pulmonary chemokine expression in the immunocompetent hosts. Infect Immun. 2014;82(9):3880–90.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Immunology and Inflammation
Rights and permissions
About this article
Cite this article
Dutta, O., Masso-Silva, J.A., Wang, K. et al. Host Response to Pulmonary Fungal Infections: a Highlight on Cell-Driven Immunity to Cryptococcus Species and Aspergillus fumigatus . Curr Pharmacol Rep 3, 335–345 (2017). https://doi.org/10.1007/s40495-017-0111-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40495-017-0111-4