Abstract
Fungal respiratory colonization of cystic fibrosis (CF) patients emerges as a new concern; however, the heterogeneity of mycological protocols limits investigations. We first aimed at setting up an efficient standardized protocol for mycological analysis of CF sputa that was assessed during a prospective, multicenter study: “MucoFong” program (PHRC-06/1902). Sputa from 243 CF patients from seven centers in France were collected over a 15-month period and submitted to a standardized protocol based on 6 semi-selective media. After mucolytic pretreatment, sputa were plated in parallel on cycloheximide-enriched (ACT37), erythritol-enriched (ERY37), benomyl dichloran–rose bengal (BENO37) and chromogenic (CAN37) media incubated at 37 °C and on Sabouraud–chloramphenicol (SAB27) and erythritol-enriched (ERY27) media incubated at 20–27 °C. Each plate was checked twice a week during 3 weeks. Fungi were conventionally identified; time for detection of fungal growth was noted for each species. Fungal prevalences and media performances were assessed; an optimal combination of media was determined using the Chi-squared automatic interaction detector method. At least one fungal species was isolated from 81% of sputa. Candida albicans was the most prevalent species (58.8%), followed by Aspergillus fumigatus (35.4%). Cultivation on CAN37, SAB27, ACT37 and ERY27 during 16 days provided an optimal combination, detecting C. albicans, A. fumigatus, Scedosporium apiospermum complex and Exophiala spp. with sensitivities of 96.5, 98.8, 100 and 100%. Combination of these four culture media is recommended to ensure the growth of key fungal pathogens in CF respiratory specimens. The use of such consensual protocol is of major interest for merging results from future epidemiological studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cystic fibrosis (CF) is a major genetic disease affecting more than 28,000 and 35,000 people in the USA and Europe, respectively [1,2,3]. In France, 6,369 people were suffering from this orphan disease in 2014 [2]. Autosomal recessive mutations affecting the cystic fibrosis transmembrane conductance regulator (CFTR) gene which encodes a chloride channel characterize the disease. This leads to dysfunction of this membrane transporter involved in the maintaining of the electrochemical balance of epithelial cells, especially in bronchi [4], and therefore to thick secretions and impaired mucociliary clearance in the respiratory tract. The mucus impaction leads to a chronic bacterial and fungal colonization of the airways, resulting in subsequent epithelial inflammation and damages that finally end to progressive lung function decline [3, 4].
Since several years now, the management of CF patients has favorably evolved, with a marked increase in life expectancy (51.6% of adults in the CF population in 2015 according to the US Cystic Fibrosis Foundation Patient Registry) [1]. This trend is also punctuated with a concomitant increase in the median predicted survival age (+12.6 years within a 29-year period) and an overall upward trend in the annual number of lung transplant procedures [1].
However, along with the increase in life expectancy, fungal colonization and/or infection emerged as a new concern in CF, as evidenced by the sharp increase in the incidence of filamentous fungi from respiratory secretions over a 10-year period [6]. Indeed, a significant number of data places several fungi as key elements in the natural course of the disease as well as real threats in case of lung transplantation [5, 7, 8]. Thus, assessing the real occurrence of fungal species in the CF airways, as well as deciphering their clinical relevance, is more than ever of high medical importance [3, 4]. Several epidemiological studies, mostly observational and retrospective, have been designed to clarify the contribution of fungi to lung deterioration in CF [9,10,11,12,13,14,15]. However, the heterogeneity in study design and the lack of standardization of mycological protocols hinder exhaustive epidemiological investigations and hold back from making a thorough picture of the current fungal situation in CF [3, 6, 16, 17]. As recently proposed, optimization of routine laboratory culture methods and implementation of consensual approaches to ensure an efficient and robust recovery of fungi from sputa from CF patients are required [16, 18].
In this context, we first aimed at setting up an effective standardized and consensual protocol for routine mycological analysis of CF sputa, ensuring growth of the key fungal species involved in airway colonization/respiratory infections. To meet this purpose, a multicenter prospective study was conducted within a large cohort of CF patients in France (“MucoFong”; PHRC-06/1902) that allowed us to propose an optimal protocol for CF sputum mycological analysis and to gather epidemiological data regarding fungal prevalence rates.
Patients and Methods
Study Design and Data Source
This 3-year multicenter prospective observational study was supported by our national clinical research program “PHRC” (protocol number 06/1902, acronym: MucoFong). Its overall aim was to make a thorough and reliable mycological assessment of CF respiratory tract. For each patient, clinical data including spirometry, therapeutic, radiological and biological data along with ABPA criteria were prospectively collected by clinical staff of the CF Resource and Competence Centers (CRCM) of Angers, Bordeaux, Dijon, Dunkerque, Grenoble, Lille and Rouen (France). One sputum sample was collected per patient into a sterile cup after a water rinse to prevent excessive salivary contamination as previously described [16, 19], and the same protocol was used in all centers for mycological analysis (see mycological analysis section). This study was approved by the Institutional Ethics Committees of Lille University Hospital (Reference Number CPP 06/84), and a written informed consent was provided by all participants.
Study Population
In each center, patients were included according to the following criteria: (1) patient with a well-documented diagnosis of CF with either the two known mutations in the CFTR gene or an abnormally high sweat chloride test as required [20]; (2) patient belonging to one of the participating centers (CRCM of Angers, Bordeaux, Dijon, Dunkerque, Grenoble, Lille and Rouen); (3) patient older than 6 years; (4) patient undergoing a mycological analysis as part of either the annual microbiological checkup or the clinical management of an acute pulmonary exacerbation; and (5) written informed consent form endorsed. Pulmonary transplant recipients were excluded at baseline.
Mycological Analysis
In all centers, the following standardized protocol was used.
Sample pre-treatment Sputa were homogenized for 30 min at 37 °C with Digest-EUR® (Eurobio, France) in a 1:1 (v:v) ratio, and mycological cultures were performed after direct examination, as previously described [14, 16, 19, 21] (Fig. 1).
Mycological analysis After incubation, digested sputa (50–100 µL) underwent direct examination and were plated onto six semi-selective culture media (10 µL of digested sample per plate). Remaining sputa were stored at −20 °C for further analysis if needed. Cultures were incubated aerobically for 3 weeks at various temperatures according to the medium (Fig. 1; Table 1).
Briefly, all sputum samples were inoculated in parallel onto 6 agar media (CAN37, SAB27, ACT37, BENO37, ERY27 and ERY37—see details in Table 1) to allow growth and identification of the highest number of fungal species. Characteristics of each medium and incubation temperature are summarized in Table 1. Volume-limited samples (especially from pediatric patients) were preferentially cultured on three media (CAN37, ACT37 and SAB27).
The chromogenic medium (CAN37) enables the growth of both yeasts and molds but is specifically designed to identify and quantify yeasts from the Candida genus through the hydrolysis of chromogenic substrates, when incubated at 37 °C.
Sabouraud medium with chloramphenicol and gentamicin (SAB27) represents the usual mycological culture medium, enabling growth of most yeasts and filamentous fungi, and was routinely used mainly to detect Aspergillus species when incubated at 20–27 °C.
The Sabouraud or YPDA medium with chloramphenicol and cycloheximide (ACT37) is a semi-selective medium allowing the isolation of slow-growing molds that are cycloheximide resistant (Table 1) and therefore facilitating the recovery of filamentous fungi associated with the more rapidly growing A. fumigatus.
Dichloran–rose bengal–chloramphenicol (DRBC)–benomyl medium (BENO37) is based on microtubule inhibitory properties of benomyl that inhibits growth or significantly reduces the hyphal elongation, especially for A. fumigatus. Benomyl and DRBC compounds facilitate the development of slow-growing filamentous fungi such as Scedosporium species [22]. Plates were incubated at 37 °C.
Erythritol-enriched medium (ERY27 and ERY 37) is designed to allow the selective growth of the dimorphic fungus Exophiala dermatitidis, through the presence of a specific carbon source, erythritol. Plates were incubated both at 20–27 °C (ERY27) and at 37 °C (ERY37).
Media were checked twice a week. For each semi-selective medium, the first day of positive culture was reported, as well as species number and colony counts for each species isolated. Molds were identified by their macroscopic and microscopic morphology. For isolates with atypical morphology, identification was confirmed by ITS1-ITS2 and β-tubulin locus sequencing. Yeasts were identified according to colony color on chromogenic medium, latex tests and biochemical patterns (API®/ID 32C, bioMérieux, Marcy-l’Etoile, France) when necessary. Subcultures of micromycetes were performed on Sabouraud or YPDA medium in order to assess precise identification, to determine their antifungal susceptibility and to preserve them for any further analysis.
Statistical Analysis
Means of ages or species number were compared using the Student’s t test. Prevalences were estimated for each fungal species, and performances of each growth medium were individually assessed. Prevalences were compared through Fisher’s exact test. The optimal combination of growth media allowing the best detection of a given fungus was established using decision trees obtained by the CHAID (Chi-squared automatic interaction detector) method [23, 24]. Significance was set at p value < 0.05. The statistical software SAS© (version 9.2) was used for data acquisition and analysis.
Prevalences of each species were calculated among the entire population and, then, separately among adult and pediatric populations as follow: For a given species and a given sputum sample, culture was considered positive when the species growth was evidenced on at least one of the six media.
The assessment of growth medium performances was based on sensitivities (Se) and negative predictive values (NPV) that were established for each medium, focusing on fungal species isolated at least in five sputum samples over the whole sample panel.
To define the optimal combination of growth media able to detect 99.99% of the opportunistic fungal pathogens, including A. fumigatus, species of the Scedosporium apiospermum complex and Exophiala spp., that were recovered from the “MucoFong” population, we used decision trees obtained by the CHAID method. This statistical detection tree technique is based upon adjusted significance testing, providing highly predictive algorithms of optimal fungal detection. Using CHAID method with the chromogenic medium as reference growth medium (due to its best sensitivity and negative predictive values for all species combined), we determined which other medium was the best choice to isolate opportunistic fungi not found on the reference medium.
Results
General Data of “MucoFong” Population
A total of 300 CF patients were included in “MucoFong” study between July 2007 and October 2008. Half of our subjects came from Lille and Grenoble (25 and 21%, respectively), while 12, 10, 7, 12 and 14% of our patients were recruited in Dunkerque, Bordeaux, Angers, Dijon and Rouen, respectively.
Fifty-seven patients did not expectorate and were not included in the statistical analysis of mycological data; then, 243 sputa (one sputum per patient) underwent mycological analysis. Mean age of the “MucoFong” population was of 21.2 ± 8.7 years (median and Q1–Q3 interquartile ranges of 21.5, 15.1–24,7 y.o.). No significant difference was observed between mean and median ages of CF patients who expectorate and those who did not (24.04 ± 10.3 y.o. vs. 21.2 ± 7.3 y.o., and 22.5, Q1: 16.6–Q3: 30.5 y.o. vs. 21.5, Q1: 15.1–Q3: 24.7 y.o.).
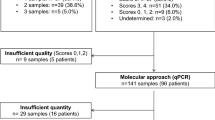
Regarding patients who expectorated, from 0 to 5 fungal species were recovered for each patient with a median number of one species isolated per sputum (Fig. 2), and 81% of patients had a positive culture for at least one fungal species (including yeasts). The mean age of culture-positive patients was significantly higher than that of culture-negative patients (24.9 ± 9.2 vs. 20.4 ± 11.2 y.o., p = 0.03). One hundred and seventy-four sputa were provided by adult patients (71.6%) and sixty-nine from pediatric patients (28.4%). Direct examination of sputa remained negative in 76.3% of cases, while hyphae and/or yeast forms were observed in 16 and 11.6% of the cases, respectively.
Species Prevalence Estimation
Species identification was mainly assessed through conventional methods, ITS and/or β-tubulin locus sequencing being performed on 5% of fungal isolates.
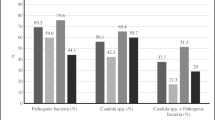
Considering our global CF population (n = 243), Candida albicans was the most prevalent species (58.8%), followed by A. fumigatus (35.4%), Penicillium spp. (10.4%) and species of the S. apiospermum complex (5.3%), while Exophiala dermatitidis accounted for only 1.7% of positive cultures (Table 2). Those prevalences followed the same trend in both the adult and the pediatric populations (Table 3).
Candida albicans showed the highest prevalences among adults (63.3%) and pediatric patients (47.8%). Non-albicans Candida species accounted for 5.3% of the 243 sputa, mostly made of C. parapsilosis, C. glabrata and C. tropicalis.
Prevalence of A. fumigatus was not significantly different between our adult and pediatric populations, this mold being recovered as frequently among adults (35.6%) and children (34.8%) (p = 0.58). Mean age of pediatric patients with A. fumigatus-positive cultures was of 13.5 ± 4.0 y.o. Regarding non-fumigatus Aspergillus species, A. flavus and A. terreus were the most frequently isolated species (prevalence of 3.7 and 2%, respectively), mainly recovered from adults.
Five percent of our patients exhibited the S. apiospermum complex in their respiratory secretions. Prevalence was higher in adults (6.9%) than in children (1.4%), although this difference was not statistically significant (p = 0.20). In 75% of the case, S. apiospermum was associated with A. fumigatus in cultures. Lomentospora prolificans (previously named Scedosporium prolificans) was recovered from only two children.
Exophiala dermatitidis was evidenced from 4 patients (global prevalence of 1.7%), all cases originating from Northern France. In most cases, this fungus was associated with A. fumigatus. Exophiala jeanselmei was isolated from one sputum sample. The two Exophiala species were considered together for sensitivity, NPV and CHAID analysis.
Penicillium species ranked the third in our population. They preferentially grew at 20–27 °C and were often recovered on a unique agar plate, with a low number of colonies.
Individual Performances of Growth Media for Fungal Species Detection
Individual sensitivities and negative predictive values of each culture medium regarding fungal species detection are presented in Tables 4 and 5. CAN37, ACT37 and BENO37 showed high similar sensitivities (79.3%) and negative predictive values (76.6%) for C. albicans. Additionally, the chromogenic medium (CAN37) exhibited the best performances for detection of non-albicans Candida species (Se = 61.5%, NPV = 97.9%), establishing it as the best medium for yeast detection from CF sputa. CAN37 also showed the best performances for detection of A. fumigatus (Se = 72.1%, NPV = 86.7%), followed by SAB27 (Se = 65.1%, NPV = 84%). The latter, along with ERY37, also showed high sensitivity (66.7%) and NPV (98.7%) for detection of A. flavus.
SAB27 and ACT37 were the most suitable media for detection of the S. apiospermum complex with sensitivities of 69.2 and 53.9% and NPVs of 98.3 and 97.5%, respectively. It is noteworthy that 3 of the isolates were exclusively detected through ACT37. The benomyl-enriched medium (BENO37) showed lower performances than the two aforementioned media (Se = 46.2%, NPV = 97.1%).
Three out of the four Exophiala spp. isolates were recovered exclusively through the erythritol-enriched growth medium incubated at 27 °C (ERY27).
Establishing the Optimal Combinations of Growth Media
Decisional trees providing optimal combinations and allowing to define the best performance to detect a given micromycete were designed for three fungi or species complexes, i.e., A. fumigatus, S. apiospermum complex and Exophiala spp., which were selected on the basis of their pathogenicity in CF. For each of these fungi, algorithms were built according to the CHAID method, based on: (1) our categorical variable, namely the presence of a given fungus in a given medium; (2) our reference medium (chromogenic medium (CAN37)) given its sensitivity and negative predictive values; and (3) the individual performances of each medium previously established. According to CHAID analysis, each of the five culture media was categorized as the best choice for isolating a given species not detected with the reference medium.
The use of the four CAN37, SAB27, ERY37 and ACT37 culture media allowed the recovery of almost all A. fumigatus isolates, with a sensitivity of about 99% (85 isolates evidenced over 86). Regarding detection of the S. apiospermum complex, the combination of CAN37, SAB27 and ACT37 exhibited an excellent sensitivity, nearly 100%, the cycloheximide-enriched medium (ACT37) allowing to detect three missed strains. Erythritol-enriched medium (ERY27) was the most suitable medium for isolating Exophiala spp., in combination with SAB27, although the number of isolates (n = 5) was low.
Finally, the combination of CAN37, SAB27, ACT37 and ERY27 provided the best sensitivities for C. albicans (96.5%), A. fumigatus (98.8%), the S. apiospermum complex (100%) and Exophiala spp. (100%), as well as higher detection sensitivities for non-albicans Candida species (77%) and non-fumigatus Aspergillus species (77.7% for A. flavus, 80% for A terreus). Besides, the addition of an erythritol-enriched medium at 37 °C (ERY37) allowed us to reach 100% sensitivity for detection of A. fumigatus, A. flavus and A. terreus.
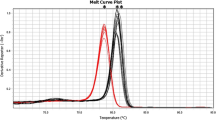
Estimating Optimal Incubation Period
Regarding the incubation time (in days) necessary for culture positivity (Fig. 3), the shortest median times were observed for C. albicans and A. fumigatus (2 and 3 days, respectively), with a range of 2–6 days required regardless of the culture medium. Scedosporium and Exophiala species required a longer incubation time (median of 6 and 8 days, respectively). The longest incubation time required for culture positivity was seen for the S. apiospermum complex (16 days for 67% of the isolates). Therefore, a incubation time of 16 days should be recommended in clinical practice, especially when Scedosporium or Exophiala species are suspected.
Discussion
The “MucoFong” French multicentric project was designed to establish an optimal culture protocol efficient for the detection of all fungal species present in CF sputa and to measure prevalence rates of these fungi in our CF patients’ cohort. Over the 243 patients able to expectorate, 81% exhibited positive mycological cultures. Half of those patients presented with only one species, while 37% were co-colonized with two species, in agreement with previous data [18, 25, 26]. It appears difficult to compare our results with previous published data because of the large heterogeneity of study design, with significant variations between absolute detection rates of fungi ranging from 32.4 to more than 80% of positive patients or from 15.2 to 92.4% of positive samples [3, 6, 14, 16, 18, 25,26,27,28,29,30]. Such dispersion can be explained by several variables: (1) study duration which greatly varied (between 6 months [27] to 10 years [6]), entailing large variations of sampling size from less than 100 [25] to more than 600 patients [6]; (2) study design which exhibited numerous discrepancies, especially regarding populations’ recruitment and characteristics, or the nature of respiratory samples (nasal swabs, sputa or bronchoalveolar lavage fluids); (3) the definition of positive fungal cultures which was highly flexible as some authors considered all micromycetes including yeasts [6, 25, 26, 30], while others focused on filamentous fungi [18, 27, 28, 31]; (4) the repeated sampling of chronically colonized patients in some studies which may have contributed to an overestimation of some prevalence rates when each biological sample was considered individually; and (5) finally, the lack of standardization of culture protocols, particularly regarding the use and type of sample pre-treatment [21, 31], the number and type of culture media (selective vs. non-selective agar), the incubation temperature and time (from 7 [31] to 28 days [18]) or the fungal identification methods used [25]. However, our high recovery rates are in agreement with the actual upward trend highlighted by the US Cystic Fibrosis Foundation Registry [1] and several studies among which an 11-year American prospective cohort analysis [6]. Although a true rise in the rate of fungal colonization among the CF population over time has to be considered, this may also be explained by the increase in life expectancy and/or the recent improvement of routine laboratories practices including the use of selective media and of a prolonged incubation time [16, 18, 25, 26, 30].
In the “MucoFong” project, patients experiencing fungal colonization were on average significantly 4.5 years older than patients exhibiting negative cultures, as already highlighted by several authors [5, 6, 11, 14, 27]. De Vrankrijker et al. [11] demonstrated in a cross-sectional analysis involving 259 patients that the airway colonization by A. fumigatus was independently associated with increased age (OR 4.80, 95% CI 2.2–10.4; p < 0.001), while Saunders et al. [14] demonstrated that A. fumigatus isolation was rare under 9 years old through a retrospective study of bronchoalveolar fluids obtained from 51 patients in the UK. This association between age and fungal colonization may be explained by additional variables (confounders) linked directly to the natural course of CF disease, such as the use of long-term antibiotic courses [6, 11] and inhaled corticosteroids [32]. Both Sudfeld et al. [6] and de Vrankrijker et al. [11] demonstrated that the fungal colonization was independently associated with the chronic use of antibiotics on multivariate analysis (OR 1.66, 95% CI 1.20–2.31; p = 0.002 and OR 5.79, 95% CI 3.1–10.8; p < 0.001, respectively). This may also explain the high number of fungal species recovered from oldest patients. However, difficulties to obtain sputum from children may have resulted in an underestimated prevalence of filamentous fungi in younger patients and created biases in studies based on sputum samples [33], as illustrated by the higher mean age of sputum-producing patients in our study (24 vs. 21.2 years old), although the difference was not statistically significant.
Taking into account the lack of standardization of CF sputum processing methods [16, 34] and the need for a consensual approach allowing better comparability of the data between CF centers worldwide, we built a standardized culturing protocol using six semi-selective growth media. To warrant reliability of our protocol, we assessed the performance of each culture medium regarding each clinically relevant species and deduced an optimal medium combination using CHAID method.
MucoFong protocol was designed, based on the expertise of the different participating laboratories and on literature data. Firstly, as sampling techniques may affect the rate of fungal recovery [17], sputa appeared to be the best noninvasive option for routine examination of the CF lung fungal biota [14, 19, 35] under practices that avoid salivary contamination [19, 21]. Secondly, we applied a mucolytic chemical pre-treatment in agreement with published studies [16, 17, 21, 25] and as recently recommended by the UK Health Protection Agency [17]. Homogenization of CF sputum does increase sensitivity of the detection procedures, especially for C. albicans and A. fumigatus [30]. Serial dilutions to prevent the overgrowth of some microorganisms [30] were not realized because we used in turn a high number of semi-selective media to overcome this issue. Finally, incubation temperature and time (3 weeks at 20–27 or 37 °C, depending on the medium, Table 1) were selected to ensure optimal conditions for isolating clinically relevant fungal species in CF, especially slow-growing fungi that are difficult to cultivate at body temperature [25].
Our medium choice was intended to be as effective and relevant as possible for detecting the most common fungal species colonizing the CF airways. Chromogenic media best suit for the isolation and identification of Candida species, as already highlighted by Borman et al. [16]. In addition, chromogenic substrates do not seem to interfere with the growth of Aspergillus spp., CAN37 being also the most suitable medium for the detection of most of Aspergillus species (including A. fumigatus), with the exception of A. flavus.
Sabouraud agar with chloramphenicol and gentamicin incubated at 20–27 °C (SAB27) was the most suitable medium for isolating clinically relevant molds including A. fumigatus, A. flavus and species of the S. apiospermum complex, but also environmental species such as Penicillium spp., the low incubation temperature (under 30 °C) likely playing a role in the isolation of these environmental molds. Antibiotics play a crucial role in mycological media as demonstrated by Nagano et al. [25, 36] with a large increase in recovery rate of fungi when using antibiotic combinations. Particularly, the concomitant use of cotrimoxazole, chloramphenicol, ceftazidime and colistin was the most effective at suppressing bacterial growth including Pseudomonas aeruginosa [36] which is known to inhibit growth of some fungal species [37]. These data support the use of agar-based media with selective antibiotic combinations (usually gentamicin and chloramphenicol) as standard culture media for routine mycological analysis of CF sputa [25, 30].
Culture medium supplemented with cycloheximide (ACT37) showed high performances for the detection of the S. apiospermum complex. ACT37 allowed the growth of three isolates that had not been detected by conventional media such as SAB27 or CAN37. As expected, ACT37 exhibited the lowest sensitivities for detecting rapidly and extensively growing molds like Aspergillus or Penicillium species, thus facilitating the selective isolation of slow-growing cycloheximide-resistant molds. Combination of ACT37 with SAB27 therefore appears to be the best option for detection of the S. apiospermum complex from CF sputa.
Surprisingly, the benomyl-containing medium (BENO37) displayed mild sensitivity values for the detection of S. apiospermum, lower than those of ACT37 and SAB27 media. Benomyl limitates the growth of Aspergillus spp. by acting on microtubules [18] and has recently been included, together with dichloran, in a culture medium called SceSel+ intended for the semi-selective isolation of the S. apiospermum complex from highly contaminated environmental sources [22]. The usefulness of this medium as a diagnostic tool for the S. apiospermum complex in CF patients has been highlighted in several studies [18, 38]. Here, we did not evidence higher detection rates when using our BENO37 medium compared with our cycloheximide-supplemented medium (ACT37), although it remained by far the most efficient to inhibit growth of the aspergilli. This discrepancy may be explained by the low prevalence of the S. apiospermum complex in our cohort compared to the other studies [18, 38]. Nevertheless, there is now accumulated evidence that the use of a selective medium able to inhibit the growth of rapidly growing fungi from CF sputa is highly recommended for isolating species of the S. apiospermum complex during routine mycological examination, especially given its pathogenicity in transplant recipients [16, 18, 30, 38, 39].
Finally, the erythritol-enriched medium revealed to be suitable for recovery of Exophiala species when incubated at 20–27 °C (ERY27), assimilation of erythritol being a particularity of these black yeasts. However, it is noteworthy that the selective advantage of this medium was lost with a higher incubation temperature (ERY37), with a sensitivity divided by three. The low number of isolates cannot allow us to draw relevant conclusions regarding its use for mycological analysis of CF sputa. Although some authors highlighted its usefulness for E. dermatitidis detection [40], its superiority compared with conventional media such as Sabouraud gentamicin–chloramphenicol agar has not been evidenced yet, even when incubated at ambient temperature [41].
Delay of culture positivity for the most frequent species, namely C. albicans and A. fumigatus, was short, 2–6 days, as previously reported [18, 21]. Pathogenic fungi known as slow-growing species required a longer incubation time, 1 week on average and up to 9 and 16 days for some isolates of S. apiospermum complex species and Exophiala, spp., respectively. Blyth et al. [18] reported similar delays, with 96.9% of Scedosporium species-positive cultures within 10 days of incubation (range 3–14 days). Regarding Exophiala spp., a 15-day incubation period is required for growth of most of the isolates (between 4 and 16 days, median time of 8 days), although some isolates require from 4 [41] to 6 weeks [17, 34]. These results led the authors to extend the incubation time of routine mycological cultures of CF sputa to at least 2 weeks, as already implemented within several centers [16, 17]. In light of our results, we recommend a similar incubation time of 16 days.
Taking into account individual performances of each medium and processing our results with an algorithm based on the CHAID method, we were in fine able to propose a standardized protocol for mycological analysis of CF sputa allowing an accurate detection of all clinically relevant fungal species (Fig. 4). This protocol is quite easy to implement in routine laboratories both in terms of technical means and of financial resources, and provides a clear benefit by ensuring a relevant fungal diagnosis in peculiar clinical situations (chronic fungal colonization, allergic diseases or lung transplantation). This procedure enhances the detection of all established pathogenic species, especially those currently under-diagnosed such as Scedosporium and Exophiala species, with excellent sensitivity rates ranging from 98.8% (A. fumigatus) to 100% (S. apiospermum complex and Exophiala spp.). It also allows to detect fungal species able to chronically colonize the airways even if their pathogenicity is still debated such as C. albicans (sensitivity of 96.5%), non-albicans Candida species (sensitivity of 77%), A. flavus (sensitivity of 77.7%) and A. terreus (sensitivity of 80%). The potential addition of a fifth medium, namely an erythritol-enriched medium, incubated at 37 °C finally leverages all Aspergillus species’ detection rates up to 100%.
By using this protocol, A. fumigatus was isolated from 35.4% of the patients, appearing to be the most frequent fungus after C. albicans, regardless of patient age. This result is in agreement with data from previous prospective studies (median isolation rate of 36.5%, with rates ranging from 5.2 to 88.9% of positive patients) [3, 6, 14, 18, 25,26,27,28,29,30,31, 33, 42,43,44]. Regarding our pediatric cohort, the mean age of patients with A. fumigatus-positive cultures (13.5 ± 4.0 y.o.) is in line with published data, arguing that the A. fumigatus colonization is uncommon among young children [5, 14, 42]. Particularly, Cimon et al. [42] reported a mean age of 12.3 years at the date of the first isolation of A. fumigatus, while other authors evidenced the increased age (around 23 years old) as a risk factor for chronic colonization by A. fumigatus [6, 27]. In contrast, we did not evidence any statistical difference between our adult and pediatric prevalence rates, maybe because of the limited size of our pediatric population. Aspergillus fumigatus stands out as the major lung colonizer among CF patients [5], all increased age, chronic bacterial lung colonization/infection and antibiotic use being risk factors for colonization [6, 11, 17, 27]. However, the clinical significance of A. fumigatus colonization within non-ABPA patients remains poorly understood yet. Since establishing this fungus as either a bystander or a pathogen is still a matter of debate [34], criteria to differentiate A. fumigatus colonization from infection have been proposed [17, 25, 45]. Our present work was not focused on studying clinical relevance of A. fumigatus isolation; the “MucoFong” database including the entire longitudinal data (2-year follow-up of the patients) is currently being analyzed. To date, some authors evidenced an association between persistent A. fumigatus colonization and lower predicted FEV1% or severe pulmonary exacerbation requiring hospitalization [6, 10, 15], while other did not [11]. Additionally, the administration of itraconazole to non-ABPA colonized patients found no benefit with respect to exacerbations or lung function parameters in a recent double-blinded placebo study, although 43% of patients did not achieve therapeutic levels [13].
Non-fumigatus Aspergillus species were isolated to a lower extent, A. flavus and A. terreus accounting for the most frequent ones (prevalences of 3.7 and 2%, respectively), as reported in previous literature data [3, 16, 27, 28, 30, 31, 42, 44], while A. versicolor, A. glaucus and A. ustus were exceptionally recovered in CF sputa. Like A. fumigatus, A. terreus has been reported to chronically colonize the CF airways and may be involved in ABPA [46].
The S. apiospermum complex ranks the second among the clinically relevant filamentous fungi isolated in our CF cohort, after A. fumigatus, displaying a 5.3% prevalence rate in line with previous published data [3, 6, 18, 22, 25, 26, 28, 30, 31, 42, 47]. Interestingly, our result tends to the prevalence rates reported in studies using selective media for detection of the species complex [18, 22, 30]. The emergence of these fungi could be partly explained by the improvement of detection techniques as well as by the increase in life expectancy and the subsequent use of antibiotics [18, 48]. Chronic colonization of the airways by these saprophytic fungi occurs almost exclusively in CF patients, CFTR mutations therefore being considered as a risk factor for the airway colonization by Scedosporium species [5]. Patterns of lung colonization by these fungi resemble those of A. fumigatus. Scedosporium species seem to better settle down in older patients, as highlighted in our study by the higher prevalence among adults, and as supported by the median age of first isolation of the S. apiospermum complex (14.5 y.o.) reported in a prospective study [47]. The clinical significance of a persistent colonization still remains unclear. Nagano et al. [25] considered Scedosporium species as clinically significant fungi (class I). Sensitization [42] and allergic bronchopulmonary (ABPA-like) manifestations have already been described and may contribute to the progression of the CF lung disease [5, 39, 47, 49]. Similarly, a mere fungal airway habitation may hasten progressive deterioration of lung function [48] by causing direct mucosal damages through the production of metallopeptidases and serine proteases and by participating in inflammatory reaction [39]. However, although some authors have described this phenomenon [48], colonization by Scedosporium species has not been found to be associated with any clinical parameters yet [34]. Three-quarters of our patients presented with co-colonization by Scedosporium species and A. fumigatus, an association frequently reported [5, 18, 26, 47] that underlines the need of selective media designed to limit the growth of A. fumigatus. The marked mortality of disseminated Scedosporium infections after lung transplantation in CF [8] places its systematic research in sputa as a prerequisite for lung transplantation [5, 49]. Out of the S. apiospermum complex, we rarely evidenced L. prolificans. Unlike the S. apiospermum complex, L. prolificans is not closely tied to CF disease but preferentially affects individuals suffering from hematological malignancies [50]. However, its high resistance level combined with a high mortality rate should alert us in case of positive culture.
Candida albicans was the most common fungus encountered within our cohort, accounting for almost 60% of the patients, with a higher prevalence rate among adults (Table 3). This result is consistent with published data showing prevalence rates ranging from 32.4 to 94.6% in CF [9, 16, 25, 26, 29, 30, 42, 43, 51, 52]. A long-term colonization has been demonstrated in some studies [9, 26, 51], but its clinical relevance is still controversial [25, 51, 53]. By participating in the maintenance of an inflammatory environment, C. albicans could be considered as a real contributor extending mucosal damages, especially since several authors evidenced specific serum IgE responses [16, 42]. However, its significant association with clinical features such as pancreatic insufficiency, osteopenia or P. aeruginosa colonization raises the question of a simple marker of advanced disease [9, 53].
Prevalence of non-albicans Candida species was low (5.3% of positive patients), slightly lower than those of published data (from 10 to 20%) [16, 25, 26, 29, 30, 51]. Candida parapsilosis, C. glabrata and C. tropicalis were the main species encountered within our CF cohort; Candida dubliniensis usually recovered in CF prospective cohorts with a high occurrence was not evidenced here.
Similarly, E. dermatitidis exhibited a lower prevalence rate (1.7%) than usually published (around 4% and up to 17%) [3, 5, 12, 25, 41, 52, 54]. This black yeast can be considered as a marker of CFTR-related disease [5, 41] and is often isolated among older patients presenting with exocrine pancreatic insufficiency [12, 34, 41], in association with other fungi [30]. We do not have any explanation regarding our low prevalence rate despite the use of a selective media, especially since most of our patients were more than 12 years old. Such as yeasts from the Candida genus, a persistent colonization has been described [30, 54] but its clinical relevance is not well established yet, although pulmonary infections [30], sensitization and a significant association with lung function impairment have been evidenced [55].
Penicillium spp. exhibited a 10.7% prevalence rate, ranking the third after C. albicans and A. fumigatus. Their isolation rates vary from 0.6 to more than 20% depending on the studies [6, 16, 18, 25, 27, 29,30,31]; their isolation is currently considered as contamination of the cultures [5] or transient carriage without a real clinical significance [5, 25].
To conclude, the “MucoFong Project” was set up in response to the urgent need of developing an optimal and standardized protocol for the detection of key fungal pathogens currently involved in colonization of the CF airways. This project was based on a prospective data collection from seven French CF Resource and Competence Centers and involved 243 patients. Our results enable us to put forward a well-defined standardized protocol for mycological analysis of CF sputa ensuring the detection of most of clinically relevant fungi. This protocol is based on: (1) a mucolytic chemical pre-treatment of sputum samples; (2) plating two usual media providing the growth of most of Aspergillus species and yeasts plus two semi-selective media facilitating the detection of slow-growing molds closely related to CF disease, namely the S. apiospermum complex and E. dermatitidis; and (3) a prolonged cultivation period of 16 days (Fig. 4).
The exhaustive analysis of data allowed us to update epidemiological data of the fungal respiratory biota recovered among CF patients in France. Our high fungal recovery rate corroborates the actual rising trend of fungi in CF. However, the significance of a positive culture requires to be interpreted with regards to the clinical context. As reported in the literature, C. albicans stands out as the most frequent isolated species—although its pathogenic power remains controversial—followed by A. fumigatus and the S. apiospermum complex which clearly emerge as central key species. Exophiala dermatitidis remains relatively uncommon despite the use of selective media.
By overcoming the major bias associated with the wide heterogeneity of mycological procedures, the implementation of such consensual standardized protocol appears to be of major interest for a better global comprehension of the fungal airway colonization determinants and for an exhaustive mapping of the CF mycobiome at the international scale.
References
Cystic Fibrosis Foundation Patient Registry Annual Report 2015. [cited 2016 Nov 18]. https://www.cff.org/Our-Research/CF-Patient-Registry/2015-Patient-Registry-Annual-Data-Report.pdf.
European Cystic Fibrosis Society Patient Registry Annual Report 2014. [cited 2017 Jan 22]. https://www.ecfs.eu/sites/default/files/images/ECFSPR_Annual%20Report%202014_Nov2016.pdf.
Touati K, Nguyen DNL, Delhaes L. The airway colonization by opportunistic filamentous fungi in patients with cystic fibrosis: recent updates. Curr Fungal Infect Rep. 2014;8:302–11.
Rowe SM, Miller S, Sorscher EJ. Cystic fibrosis. N Engl J Med. 2005;352:1992–2001.
Pihet M, Carrère J, Cimon B, et al. Occurrence and relevance of filamentous fungi in respiratory secretions of patients with cystic fibrosis—a review. Med Mycol. 2009;47:387–97.
Sudfeld CR, Dasenbrook EC, Merz WG, Carroll KC, Boyle MP. Prevalence and risk factors for recovery of filamentous fungi in individuals with cystic fibrosis. J Cyst Fibros. 2010;9:110–6.
Luong ML, Chaparro C, Stephenson A, et al. Pretransplant Aspergillus colonization of cystic fibrosis patients and the incidence of post-lung transplant invasive aspergillosis. Transplantation. 2014;97:351–7.
Symoens F, Knoop C, Schrooyen M, et al. Disseminated Scedosporium apiospermum infection in a cystic fibrosis patient after double-lung transplantation. J Heart Lung Transplant. 2006;25:603–7.
Chotirmall SH, O’Donoghue E, Bennett K, et al. Sputum Candida albicans presages FEV1 decline and hospital-treated exacerbations in cystic fibrosis. Chest. 2010;138:1186–95.
Amin R, Dupuis A, Aaron SD, Ratjen F. The effect of chronic infection with Aspergillus fumigatus on lung function and hospitalization in patients with cystic fibrosis. Chest. 2010;137:171–6.
de Vrankrijker AMM, van der Ent CK, van Berkhout FT, et al. Aspergillus fumigatus colonization in cystic fibrosis: implications for lung function? Clin Microbiol Infect. 2011;17:1381–6.
Kondori N, Gilljam M, Lindblad A, et al. High rate of Exophiala dermatitidis recovery in the airways of patients with cystic fibrosis is associated with pancreatic insufficiency. J Clin Microbiol. 2011;49:1004–9.
Aaron SD, Vandemheen KL, Freitag A, et al. Treatment of Aspergillus fumigatus in patients with cystic fibrosis: a randomized, placebo-controlled pilot study. PLoS ONE. 2012;7:e36077.
Saunders RV, Modha DE, Claydon A, Gaillard EA. Chronic Aspergillus fumigatus colonization of the pediatric cystic fibrosis airway is common and may be associated with a more rapid decline in lung function. Med Mycol. 2016;54:537–43.
Fillaux J, Brémont F, Murris M, et al. Assessment of Aspergillus sensitization or persistent carriage as a factor in lung function impairment in cystic fibrosis patients. Scand J Infect Dis. 2012;44:842–7.
Borman AM, Palmer MD, Delhaes L, et al. Lack of standardization in the procedures for mycological examination of sputum samples from CF patients: a possible cause for variations in the prevalence of filamentous fungi. Med Mycol. 2010;48(Suppl 1):S88–97.
Liu JC, Modha DE, Gaillard EA. What is the clinical significance of filamentous fungi positive sputum cultures in patients with cystic fibrosis? J Cyst Fibros. 2013;12:187–93.
Blyth CC, Harun A, Middleton PG, et al. Detection of occult Scedosporium species in respiratory tract specimens from patients with cystic fibrosis by use of selective media. J Clin Microbiol. 2010;48:314–6.
Delhaes L, Monchy S, Fréalle E, et al. The airway microbiota in cystic fibrosis: a complex fungal and bacterial community—implications for therapeutic management. PLoS ONE. 2012;7:e36313.
Rosenstein BJ, Cutting GR. The diagnosis of cystic fibrosis: a consensus statement. Cystic Fibrosis Foundation Consensus Panel. J Pediatr. 1998;132:589–95.
Pashley CH, Fairs A, Morley JP, et al. Routine processing procedures for isolating filamentous fungi from respiratory sputum samples may underestimate fungal prevalence. Med Mycol. 2012;50:433–8.
Rainer J, Kaltseis J, de Hoog SG, Summerbell RC. Efficacy of a selective isolation procedure for members of the Pseudallescheria boydii complex. Antonie Van Leeuwenhoek. 2007;93:315–22.
Moles DR, Bedi R. A simple technique for data management in general dental practice audit. Prim Dent Care. 1997;4:61–5.
Song Y, Lu Y. Decision tree methods: applications for classification and prediction. Shanghai Arch Psychiatry. 2015;27:130–5.
Nagano Y, Elborn JS, Millar BC, et al. Comparison of techniques to examine the diversity of fungi in adult patients with cystic fibrosis. Med Mycol. 2010;48:166–76.
Güngör O, Tamay Z, Güler N, Erturan Z. Frequency of fungi in respiratory samples from Turkish cystic fibrosis patients. Mycoses. 2013;56:123–9.
Mortensen KL, Jensen RH, Johansen HK, et al. Aspergillus species and other molds in respiratory samples from patients with cystic fibrosis: a laboratory-based study with focus on Aspergillus fumigatus azole resistance. J Clin Microbiol. 2011;49:2243–51.
Paugam A, Baixench MT, Demazes-Dufeu N, et al. Characteristics and consequences of airway colonization by filamentous fungi in 201 adult patients with cystic fibrosis in France. Med Mycol. 2010;48(Suppl 1):S32–6.
Valenza G, Tappe D, Turnwald D, et al. Prevalence and antimicrobial susceptibility of microorganisms isolated from sputa of patients with cystic fibrosis. J Cyst Fibros. 2008;7:123–7.
Masoud-Landgraf L, Badura A, Eber E, et al. Modified culture method detects a high diversity of fungal species in cystic fibrosis patients. Med Mycol. 2014;52:179–86.
Nielsen SM, Kristensen L, Søndergaard A, et al. Increased prevalence and altered species composition of filamentous fungi in respiratory specimens from cystic fibrosis patients. APMIS. 2014;122:1007–12.
Ren CL, Pasta DJ, Rasouliyan L, et al. Relationship between inhaled corticosteroid therapy and rate of lung function decline in children with cystic fibrosis. J Pediatr. 2008;153:746–51.
Burgel PR, Paugam A, Hubert D, Martin C. Aspergillus fumigatus in the cystic fibrosis lung: pros and cons of azole therapy. Infect Drug Resist. 2016;9:229–38.
Chotirmall SH, McElvaney NG. Fungi in the cystic fibrosis lung: bystanders or pathogens? Int J Biochem Cell Biol. 2014;52:161–73.
Whiteson KL, Bailey B, Bergkessel M, et al. The upper respiratory tract as a microbial source for pulmonary infections in cystic fibrosis. Parallels from island biogeography. Am J Respir Crit Care Med. 2014;189:1309–15.
Nagano Y, Millar BC, Goldsmith CE, et al. Development of selective media for the isolation of yeasts and filamentous fungi from the sputum of adult patients with cystic fibrosis (CF). J Cyst Fibros. 2008;7:566–72.
Kerr J. Inhibition of fungal growth by Pseudomonas aeruginosa and Pseudomonas cepacia isolated from patients with cystic fibrosis. J Infect. 1994;28:305–10.
Horré R, Marklein G, Siekmeier R, Nidermajer S, Reiffert SM. Selective isolation of Pseudallescheria and Scedosporium species from respiratory tract specimens of cystic fibrosis patients. Respiration. 2009;77:320–4.
Cortez KJ, Roilides E, Quiroz-Telles F, et al. Infections caused by Scedosporium spp. Clin Microbiol Rev. 2008;21:157–97.
Horré R, Marklein G, Siekmeier R, Reiffert S-M. Detection of hyphomycetes in the upper respiratory tract of patients with cystic fibrosis. Mycoses. 2011;54:514–22.
Lebecque P, Leonard A, Huang D, et al. Exophiala (Wangiella) dermatitidis and cystic fibrosis—prevalence and risk factors. Med Mycol. 2010;48(Suppl 1):S4–9.
Cimon B, Carrère J, Chazalette JP, et al. Fungal colonization and immune response to fungi in cystic fibrosis. J Mycol Méd. 1995;5:211–6.
Bakare N, Rickerts V, Bargon J, Just-Nübling G. Prevalence of Aspergillus fumigatus and other fungal species in the sputum of adult patients with cystic fibrosis. Mycoses. 2003;46:19–23.
Fischer J, van Koningsbruggen-Rietschel S, Rietschel E, et al. Prevalence and molecular characterization of azole resistance in Aspergillus spp. isolates from German cystic fibrosis patients. J Antimicrob Chemother. 2014;69:1533–6.
Baxter CG, Dunn G, Jones AM, et al. Novel immunologic classification of aspergillosis in adult cystic fibrosis. J Allergy Clin Immunol. 2013;132(560–566):e10.
Rougeron A, Giraud S, Razafimandimby B, et al. Different colonization patterns of Aspergillus terreus in patients with cystic fibrosis. Clin Microbiol Infect. 2014;20:327–33.
Cimon B, Carrère J, Vinatier JF, et al. Clinical significance of Scedosporium apiospermum in patients with cystic fibrosis. Eur J Clin Microbiol Infect Dis. 2000;19:53–6.
Russell GK, Gadhok R, Simmonds NJ. The destructive combination of Scedosporium apiospermum lung disease and exuberant inflammation in cystic fibrosis. Paediatr Respir Rev. 2013;14(Suppl 1):22–5.
Guarro J, Kantarcioglu AS, Horré R, et al. Scedosporium apiospermum: changing clinical spectrum of a therapy-refractory opportunist. Med Mycol. 2006;44:295–327.
Rodriguez-Tudela JL, Berenguer J, Guarro J, et al. Epidemiology and outcome of Scedosporium prolificans infection, a review of 162 cases. Med Mycol. 2009;47:359–70.
Muthig M, Hebestreit A, Ziegler U, Seidler M. Müller F-MC. Persistence of Candida species in the respiratory tract of cystic fibrosis patients. Med Mycol. 2010;48:56–63.
LiPuma JJ. The changing microbial epidemiology in cystic fibrosis. Clin Microbiol Rev. 2010;23:299–323.
Chotirmall SH, Greene CM, McElvaney NG. Candida species in cystic fibrosis: a road less travelled. Med Mycol. 2010;48(Suppl 1):S114–24.
Packeu A, Lebecque P, Rodriguez-Villalobos H, et al. Molecular typing and antifungal susceptibility of Exophiala isolates from patients with cystic fibrosis. J Med Microbiol. 2012;61:1226–33.
Kondori N, Lindblad A, Welinder-Olsson C, Wennerås C, Gilljam M. Development of IgG antibodies to Exophiala dermatitidis is associated with inflammatory responses in patients with cystic fibrosis. J Cyst Fibros. 2014;13:391–9.
Acknowledgements
L. Delhaes has received research grants from the French Ministry of Health and Research (PHRC N°2006/1902), Lille Hospital, the association “Vaincre la Mucoviscidose” (Defeat Cystic Fibrosis) (MucoFong and Mucofong-ATF N8 2006/351) and the Pharmaceutical Division of Pfizer France (Nu 2006/158). The authors would like to thank Arnaud Hautecoeur for his assistance in organizing the data set.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Coron, N., Pihet, M., Fréalle, E. et al. Toward the Standardization of Mycological Examination of Sputum Samples in Cystic Fibrosis: Results from a French Multicenter Prospective Study. Mycopathologia 183, 101–117 (2018). https://doi.org/10.1007/s11046-017-0173-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-017-0173-1