Abstract
To evaluate the in vitro efficacy of common antifungal drugs, as well as the interactions of caspofungin with voriconazole, amphotericin B, or itraconazole against the pathogenic black yeast Exophiala dermatitidis from China, the minimal inhibitory concentrations (MICs) of terbinafine, voriconazole, itraconazole, amphotericin B, fluconazole, and caspofungin against 16 strains of E. dermatitidis were determined by using CLSI broth microdilution method (M38-A2). The minimal fungicidal concentrations (MFCs) were also determined. Additionally, the interactions of caspofungin with voriconazole, amphotericin B, itraconazole or fluconazole, that of terbinafine with itraconazole, or that of fluconazole with amphotericin B were assessed by using the checkerboard technique. The fractional inhibitory concentration index (FICI) was used to categorize drug interactions as following, synergy, FICI ≤ 0.5; indifference, FICI > 0.5 and ≤4.0; or antagonism, FICI > 4.0. The MIC ranges of terbinafine, voriconazole, itraconazole, amphotericin B, fluconazole, and caspofungin against E. dermatitidis were 0.06–0.125 mg/l, 0.25–1.0 mg/l, 1.0–2.0 mg/l, 1.0–2.0 mg/l, 16–64 mg/l, and 32–64 mg/l, respectively. The in vitro interactions of caspofungin with voriconazole, amphotericin B, and itraconazole showed synergic effect against 10/16(62.5%), 15/16(93.75%), and 16/16(100%) isolates, while that of caspofungin with fluconazole showed indifference. Besides, the interaction of terbinafine with itraconazole as well as that of fluconazole with amphotericin B showed indifference. Terbinafine, voriconazole, itraconazole, and amphotericin B have good activity against E. dermatitidis. The combinations of caspofungin with voriconazole, amphotericin B or itraconazole present synergic activity against E. dermatitidis. These results provide the basis for novel options in treating various E. dermatitidis infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The black yeast E. dermatitidis, which can be isolated from various materials, is able to cause both superficial and deep-seated infections in human beings [1]. In recent years, infections caused by E. dermatitidis with various clinical presentations are increasing, including fatal fungemia [2–4] and central nervous system infections [5, 6]. Although a few papers have presented antifungal susceptibility patterns of E. dermatitidis against currently available antifungal drugs that are being used to treat phaeohyphomycosis [7–9], little was known about the combination regimens with synergistic drugs that could provide novel options for treating various phaeohyphomycosis. In this study, by using the standard microdilution method CLSI (formerly NCCLS) M38-A2 [10], we evaluated the antifungal activity of terbinafine, fluconazole, itraconazole, voriconazole, amphotericin B, and the echinocandin caspofungin [11] against E. dermatitidis from China. Since the combinations of different antifungal drugs with different mechanisms might improve clinical results, reduce doses and dose-related toxicity, we further investigated the interactions of caspofungin with itraconazole, voriconazole, amphotericin B or fluconazole, that of terbinafine with itraconazole, or that of fluconazole with amphotericin B, against E. dermatitidis strains.
Materials and Methods
Organisms
All of the 16 E. dermatitidis strains, isolated from different patients or nature, were stored in the Research Center for Medical Mycology of Peking University, China. Each strain was grown for 7 days on potato dextrose agar (PDA) at 35°C to ensure the viability and purity. Candida parapsilosis ATCC 22019 was used as quality control for antifungal susceptibility testing.
Molecular Reconfirmation
Since the species of Exophiala are morphologically very similar, we identified these 16 E. dermatitidis strains by using the molecular methods as described elsewhere [12]. After the genomic DNA was extracted, PCR of the rDNA internal transcribed spacer region with primers ITS1 (5′-TCC GTA GGT GAA CCT GCGG-3′) and ITS4 (5′-TCCTCC GCT TAT TGA TAT GC-3′) was performed as described previously [12]. Amplicons were verified by electrophoresis on agarose gels staining with ethidium bromide and were then sequenced. Similarity matrices for identification were calculated after multiple sequence alignment with strains in a research database maintained at CBS that contains lots of chaetothyrialean sequences as well as ex-type strains of all species in genus Exophiala [13]. These procedures were duplicated for each strain.
Antifungal Drugs
Antifungal agents were provided by the manufacturers or were purchased as pure powder. Itraconazole (Janssen Phamaceutica, Xian, China), voriconazole (Shouguang Fukang Pharmaceutical Co. Ltd, China), terbinafine (Shouguang Fukang Pharmaceutical Co. Ltd, China), and amphotericin B (Sigma–Aldrich Co. St. Louis, USA) were diluted in 100% dimethyl sulphoxide as the stock solution with concentration of 1600 mg/l. Fluconazole (Fuyang Genebest Chemical Industry Co. Ltd, China) and caspofungin (Merck, NJ, USA) were diluted in sterile distilled water as the stock solution with concentration of 1280 mg/l. The stock solutions were diluted in RPMI-1640 medium (Invitrogen Corporation, Grand Island, USA) and were further serially diluted twofold, yielding 2 times the final strength required for the test.
Broth Microdilution Method
The broth microdilution assay was performed according to the Clinical and Laboratory Standards Institute (CLSI) M38-A2 reference method [10]. The standard liquid RPMI-1640 medium buffered with 0.165 M MOPS (morpholinepropanesulfonic acid) to adjust the pH 7.0 ± 0.1 was used as tested medium. Each antifungal drug was serially twofold diluted in RPMI-1640 broth medium to obtain two times of the final concentrations. The final concentrations of amphotericin B, itraconazole, and voriconazole ranged 16–0.03 mg/l, that of terbinafine ranged 4–0.008 mg/l, that of fluconazole ranged 256–0.5 mg/l, and that of caspofungin ranged 128–0.25 mg/l. Spores of the tested E. dermatitidis strains were collected from PDA cultures with sterile saline containing 0.01% tween20 and were further diluted with RPMI-1640 broth medium to a final concentration of 2–5 × 104 CFU/ml as twofold of the desired inoculums, from which 100 μl was further inoculated into the each microdilution well. The MIC was determined by visual assessment and was defined as lowest concentration to inhibit 100% of fungal growth compared with the growth control for all drugs after incubation at 35°C for 72 h.
MFC Determination
The in vitro minimal fungicidal concentrations (MFCs) were determined as described previously [14]. Briefly, after the MIC for each strain was determined, the microtiter plates were shaken and 20 μl suspensions from each well showing complete inhibition (100% or an optically clear well) and from the growth control (drug-free medium) was subcultured onto Sabouraud dextrose agar plates. The MFC was defined as the lowest drug concentration at which fewer than three colonies were observed after 48 h of incubation at 35°C. The MFC value represents the concentration at which approximately 99.9% of the original inoculum is killed.
Interactions of Drugs In Vitro
Drug interactions were assessed by a checkerboard microdilution method that also included the determination of the MIC of each drug alone in the same plate using the guidelines presented in CLSI document M38-A2. Antifungal agents were placed in the rows or in the columns of the trays to perform possible combinations, with concentrations from 2 to 0.03 mg/l for terbinafine, 8–0.015 mg/l for itraconazole, voriconazole and amphotericin B, 64–1 mg/l for fluconazole and caspofungin. For all the drugs and their combinations, MIC was determined after 72 h of incubation at 35°C with the endpoint criterion that was defined as the lowest concentration resulting in 100% inhibition of visible fungal growth. Duplicate testing was performed.
The fractional inhibitory concentration index (FICI) was used to classify drug interaction. The FICI is the sum of the FIC of each of the drugs, which in turn is defined as the MIC of each drug when used in combinations divided by the MIC of the drug when used alone. The FICI was defined as the following [15]: synergic if the FICI was ≤0.5; neither synergistic nor antagonistic if the FICI was >0.5 and ≤4.0; and antagonistic if FICI was >4.0.
Results
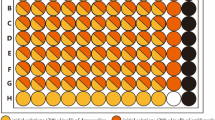
Based on the ITS DNA sequence alignment results, all the 16 strains were identical with the type strains of E. dermatitidis, e.g., CBS 686.92, CBS 207.35, CBS 581.76, and CBS 109154. MIC ranges, MIC50, MIC90, and MFC data are presented in Table 1. In brief, the MIC ranges of terbinafine, voriconazole, itraconazole, amphotericin B, fluconazole, and caspofungin against E. dermatitidis were 0.06–0.125 mg/l, 0.25–1.0 mg/l, 1.0–2.0 mg/l, 1.0–2.0 mg/l, 16–64 mg/l, and 32–64 mg/l, respectively. The MFC ranges of terbinafine, voriconazole, itraconazole, amphotericin B, and fluconazole were 0.06–0.25 mg/l, 0.25–1.0 mg/l, 1.0–2.0 mg/l, 1.0–2.0 mg/l, and 32–128 mg/l, respectively. With the high MIC values of caspofungin against E. dermatitidis, its MFCs were not assayed. In addition, the MEC (minimal effective concentration) of caspofungin against E. dermatitidis could not be determined, because most of strains showed mainly yeast cells in the growth control wells and drug-contained wells. The combinations of caspofungin with voriconazole, amphotericin B, and itraconazole had synergic effect against 10/16(62.5%), 15/16 (93.75%), and 16/16(100%) strains of E. dermatitidis, respectively (Table 2). However, no interaction of caspofungin with fluconazole was observed. Those of terbinafine with itraconazole and amphotericin B with fluconazole showed neither synergistic nor antagonistic effect against E. dermatitidis (data not show).
Discussion
In the present study, since MFCs were not higher than MICs above twofold dilution in these drugs as shown in Table 1, terbinafine, voriconazole, itraconazole, and amphotericin B presented good in vitro antifungal activity against E. dermatitidis with fungicidal activity that was consistent with previous work conducted by Fothergill et al. [8, 16]. However, the high MIC values of caspofungin and fluconazole might suggest their inadequate antifungal ability against E. dermatitidis.
Terbinafine is an allylamine antifungal drug with superior antifungal activity against various dermatophytes and other pathogenic fungi [17]. With the highly lipophilic property and wide distribution in cutaneous tissue, terbinafine is now being used in treating various dermatophytosis [18, 19]. Since E. dermatitidis can cause both superficial and subcutaneous infections, from this study and other report [15] that terbinafine has in vitro fungicidal activity against E. dermatitidis, we suggest that terbinafine would be a useful choice in the treatment of refractory cutaneous infections caused by E. dermatitidis. Although terbinafine has been proven to have synergistic activity with itraconazole against other pathogenic fungi, such as Scedosporium prolificans [20], it showed in this study no interaction with itraconazole against E. dermatitidis.
Amphotericin B is widely used for the treatment of serious systemic fungal infections [21]. From this in vitro and previous study [22], amphotericin B is effective for the treatment of patients who have phaeohyphomycosis. Systemic toxicity of amphotericin B provided the impetus to develop novel therapeutic regimen such as antifungal combinations that enable less drug dosage but better clinical outcome. According to the present study, the combination of caspofungin with amphotericin B, which is used in clinical practice for managing refractory invasive aspergillosis infections [23, 24], had synergic effect against E. dermatitidis. The role of E. dermatitidis in the lung infection has become increasingly apparent, especially in patients with cystic fibrosis [22, 25–27]. With limited therapeutic options, the present combination could be a valuable regimen to cure obstinate pulmonary phaeohyphomycosis caused by E. dermatitidis, as well as to cure systemic infections.
The triazoles, including fluconazole, itraconazole, and voriconazole, show antifungal effect by inhibiting C14-α lanosterol demethylase that contributes to the ergosterol synthesis of fungal cell membrane[28]. Although fluconazole is used widely in the treatment of various fungal infections caused by Candida spp., dermatophytes, and some dematiaceous fungi [29], poor antifungal activity against E. dermatitidis was observed in this study. And there was no interaction when fluconazole combined with either amphotericin B or caspofungin against E. dermatitidis. However, itraconazole and voriconazole, which are now being widely used in treating various invasive fungal infections including candidemia [30], invasive aspergillosis, and even the fungal infections in CNS [29, 31, 32], showed good in vitro antifungal activity against E. dermatitidis. In addition, as shown in Table 2, itraconazole and voriconazole also presented synergic effect when combined with caspofungin. These observations indicated that each of them could be used alone or in combination with caspofungin in treatment of fungemia or invasive infections caused by E. dermatitidis.
Caspofungin is an echinocandin antifungal drug and is approved to treat invasive candidiasis and invasive aspergillosis [10]. Previous studies have demonstrated that echinocandins including caspofungin and micafungin, which act by inhibiting the fungal beta-(1, 3)-glucan synthesis to cause the damages of fungal cell walls [10], can enhance the efficacy of itraconazole or amphotericin B in vitro against several fungal pathogens, such as Penicillium marnefeii[33], Aspergillus spp.[34], Candida spp.[35]. As shown in Table 2, caspofungin could enhance the activity of both voriconazole and itraconazole against 10/16 and 16/16 isolates of E. dermatitidis, with the MICs of both itraconazole and voriconazole reducing two- to fourfold dilution and that of caspofungin in the two combinations reducing two- to sixfold dilution, although caspofungin had high MIC value (Table 1) when being used alone against the E. dermatitidis. Despite there was no accurate pharmacokinetic data on the bioavailability of caspofungin in the CSF, systemic therapy with caspofungin in a few patients with cerebral fungal infection achieved more favorable outcome than other drugs [36, 37]. In addition, the combination of caspofungin with voriconazole, which is the first-line agent for the treatment of invasive aspergillosis [38], had effectively cured fatal cerebral aspergillosis that might attribute to their good brain penetration and their possible synergic antifungal activity [38–40]. Furthermore, the synergic effects presented here provide novel clinical regimens to get better clinical results in treatment for systematic E. dermatitidis infections and lethal cerebral phaeohyphomycosis. Despite these observations, indifference was seen in the combination of caspofungin with fluconazole against E. dermatitidis in vitro.
In summary, the common antifungal drugs terbinafine, voriconazole, itraconazole, and amphotericin B showed good in vitro activity against E. dermatitidis, indicating that these drugs could be used alone to treat infections caused by E. dermatitidis, although the correlation between good in vitro activity and good patient response need to be further investigated. The combinations of caspofungin with voriconazole, amphotericin B, and itraconazole presented encouraging in vitro synergic activity against E. dermatitidis, suggesting that the combinations of caspofungin with these drugs would potentially enable more effective treatment of patients with E. dermatitidis infections. Further studies in animal model and in clinical practice are anticipated to elucidate the clinical potentials of these combinations.
References
McGinnis MR. Chromoblastomycosis and phaeohyphomycosis: new concepts, diagnosis, and mycology. J Am Acad Dermatol. 1983;8:1–16.
Oztas E, Odemis B, Kekilli M, Kurt M, Dinc BM, Parlak E, et al. Systemic phaeohyphomycosis caused by Exophiala Dermatitidis resembling primary sclerosing cholangitis. J Med Microbiol. 2009;58:1243–6.
Alabaz D, Kibar F, Arikan S, Sancak B, Celik U, Aksaray N, et al. Systemic phaeohyphomycosis due to Exophiala (Wangiella) in an immunocompetent child. Med Mycol. 2009;31:1–5.
Hiruma M, Kawada A, Ohata H, Ohnishi Y, Takahashi H, Yamazaki M, et al. Systemic phaeohyphomycosis caused by Exophiala dermatitidis. Mycoses. 1993;36:1–7.
Li DM, de Hoog GS. Cerebral phaeohyphomycosis—a cure at what lengths? Lancet Infect Dis. 2009;9:376–83.
Chang X, Li R, Yu J, Bao X, Qin J. Phaeohyphomycosis of the central nervous system caused by Exophiala dermatitidis in a 3-year-old immunocompetent host. J Child Neurol. 2009;24:342–5.
Espinel-Ingroff A, Chaturvedi V, Fothergill A, Rinaldi MG. Optimal testing conditions for determining MICs and minimum fungicidal concentrations of new and established antifungal agents for uncommon molds: NCCLS collaborative study. J Clin Microbiol. 2002;40:3776–81.
Fothergill AW, Rinaldi MG, Sutton DA. Antifungal susceptibility testing of Exophiala spp.: a head-to-head comparison of amphotericin B, itraconazole, posaconazole and voriconazole. Med Mycol. 2009;47:41–3.
Okeke CN, Gugnani HC. In vitro sensitivity of environmental isolates of pathogenic dematiaceous fungi to azole compounds and a phenylpropyl-morpholine derivative. Mycopathologia. 1987;99:175–81.
Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of filamentous fungi; Approved standard—M38-A2. CLSI, Wayne, PA, USA, 2008.
Denning DW. Echinocandin antifungal drugs. Lancet. 2003;362:1142–51.
Sudhadham M, de Hoog GS, Menken SB, Gerrits VDEA, Sihanonth P. Rapid screening for genotypes as possible markers of virulence in the neurotropic black yeast Exophiala dermatitidis using PCR-RFLP. J Microbiol Methods. 2010;80:138–42.
Li DM, Li RY, de Hoog GS, Wang DL. Exophiala asiatica, a new species from patient with phaeohyphomycosis. Med Mycol. 2009;47:101–9.
Espinel-Ingroff A. In vitro fungicidal activities of voriconazole, itraconazole, and amphotericin B against opportunistic moniliaceous and dematiaceous fungi. J Clin Microbiol. 2001;39:954–8.
Odds FC. Synergy, antagonism, what the chequerboard puts between them. J Antimicrob Chemother. 2003;52:1.
Meletiadis J, Meis J, de Hoog GS, Verweij PE. In vitro susceptibilities of 11 clinical isolates of Exophiala species to six antifungal drugs. Mycoses. 2000;43:309–12.
Krishnan-Natesan S. Terbinafine: a pharmacological and clinical review. Expert Opin Pharmacother. 2009;10:2723–33.
Neoh CY, Tan SH, Perera P. Cutaneous phaeohyphomycosis due to Cladophialophora bantiana in an immunocompetent patient. Clin Exp Dermatol. 2007;32:539–40.
Revankar SG. Therapy of infections caused by dematiaceous fungi. Expert Rev Anti Infect Ther. 2005;3:601–12.
Meletiadis J, Mouton JW, Rodriguez-Tudela JL, Meis JF, Verweij PE. In vitro interaction of terbinafine with itraconazole against clinical isolates of Scedosporium prolificans. Antimicrob Agents Chemother. 2000;44:470–2.
Laniado-Laborin R, Cabrales-Vargas MN. Amphotericin B: side effects and toxicity. Rev Iberoam Micol. 2009;26:223–7.
Mukaino T, Koga T, Oshita Y, Narita Y, Obata S, Aizawa H. Exophiala dermatitidis infection in non-cystic fibrosis bronchiectasis. Respir Med. 2006;100:2069–71.
Petraitis V, Petraitiene R, Sarafandi AA, Kelaher AM, Lyman CA, Casler HE, et al. Combination therapy in treatment of experimental pulmonary aspergillosis: synergistic interaction between an antifungal triazole and an echinocandin. J Infect Dis. 2003;187:1834–43.
Aliff TB, Maslak PG, Jurcic JG, Heaney ML, Cathcart KN, Sepkowitz KA, et al. Refractory Aspergillus pneumonia in patients with acute leukemia: successful therapy with combination caspofungin and liposomal amphotericin. Cancer. 2003;97:1025–32.
Horre R, Schaal KP, Siekmeier R, Sterzik B, de Hoog GS, Schnitzler N. Isolation of fungi, especially Exophiala dermatitidis, in patients suffering from cystic fibrosis. A prospective study. Respiration. 2004;71:360–6.
Kusenbach G, Skopnik H, Haase G, Friedrichs F, Dohmen H. Exophiala dermatitidis pneumonia in cystic fibrosis. Eur J Pediatr. 1992;151:344–6.
Diemert D, Kunimoto D, Sand C, Rennie R. Sputum isolation of Wangiella dermatitidis in patients with cystic fibrosis. Scand J Infect Dis. 2001;33:777–9.
Espinel-Ingroff A. Mechanisms of resistance to antifungal agents: yeasts and filamentous fungi. Rev Iberoam Micol. 2008;25:101–6.
Hope WW, Billaud EM, Lestner J, Denning DW. Therapeutic drug monitoring for triazoles. Curr Opin Infect Dis. 2008;21:580–6.
St-Germain G, Laverdiere M, Pelletier R, Rene P, Bourgault AM, Lemieux C, et al. Epidemiology and antifungal susceptibility of bloodstream Candida isolates in Quebec: report on 453 cases between 2003 and 2005. Can J Infect Dis Med Microbiol. 2008;19:55–62.
Jain LR, Denning DW. The efficacy and tolerability of voriconazole in the treatment of chronic cavitary pulmonary aspergillosis. J Infect. 2006;52:133–7.
Schwartz S, Ruhnke M, Ribaud P, Corey L, Driscoll T, Cornely OA, et al. Improved outcome in central nervous system aspergillosis, using voriconazole treatment. Blood. 2005;106:2641–5.
Cao C, Liu W, Li R, Wan Z, Qiao J. In vitro interactions of micafungin with amphotericin B, itraconazole or fluconazole against the pathogenic phase of Penicillium marneffei. J Antimicrob Chemother. 2009;63:340–2.
O’Shaughnessy EM, Meletiadis J, Stergiopoulou T, et al. Antifungal interactions within the triple combination of amphotericin B, caspofungin and voriconazole against Aspergillus species. J Antimicrob Chemother. 2006;58:1168–76.
Kiraz N, Dag I, Yamac M, Demchok JP, Walsh TJ. Antifungal activity of caspofungin in combination with amphotericin B against Candida glabrata: comparison of disk diffusion, Etest, and time-kill methods. Antimicrob Agents Chemother. 2009;53:788–90.
Colombo AL, Rosas RC. Successful treatment of an Aspergillus brain abscess with caspofungin: case report of a diabetic patient intolerant of amphotericin B. Eur J Clin Microbiol Infect Dis. 2003;22:575–6.
Liu KH, Wu CJ, Chou CH, Lee HC, Lee NY, Hung ST, et al. Refractory candidal meningitis in an immunocompromised patient cured by caspofungin. J Clin Microbiol. 2004;42:5950–3.
Gubler C, Wildi SM, Imhof A, Schneemann M, Mullhaupt B. Disseminated invasive aspergillosis with cerebral involvement successfully treated with caspofungin and voriconazole. Infection. 2007;35:364–6.
Damaj G, Ivanov V, Le BB, D’incan E, Doglio MF, Bilger K, et al. Rapid improvement of disseminated aspergillosis with caspofungin/voriconazole combination in an adult leukemic patient. Ann Hematol. 2004;83:390–3.
Gea-Banacloche JC, Peter J, Bishop M, Kasten-Sportes C, Fowler D, et al. Successful treatment of invasive aspergillosis with the combination of voriconazole and caspofungin: correlation with in vitro interactions. Program and abstracts the 43rd Annual ICAAC; September 14–17, 2003; Chicago, IL. Abstract M-1759.
Acknowledgments
This work was supported by National Natural Science Foundation of China (30970131) and the Key Project of Chinese Ministry of Education (107002) to Wei Liu.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, Y., Liu, W., Wan, Z. et al. Antifungal Activity of Antifungal Drugs, as Well as Drug Combinations Against Exophiala dermatitidis . Mycopathologia 171, 111–117 (2011). https://doi.org/10.1007/s11046-010-9358-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-010-9358-6