Abstract
We performed a meta-analysis of the transcription profiles of type 1, type 2 and gestational diabetes to evaluate similarities and dissimilarities among these diabetes types. cRNA samples obtained from peripheral blood lymphomononuclear cells (PBMC) of 56 diabetes mellitus patients (type 1 = 19; type 2 = 20; gestational = 17) were hybridized to the same whole human genome oligomicroarray platform, encompassing 44,000 transcripts. The GeneSpring software was used to perform analysis and hierarchical clustering, and the DAVID database was used for gene ontology. The gene expression profiles showed more similarity between gestational and type 1 diabetes rather than between type 2 and gestational diabetes, a finding that was not influenced by patient gender and age. The meta-analysis of the three types of diabetes disclosed 3,747 differentially and significantly expressed genes. A total of 486 genes were characteristic of gestational diabetes, 202 genes of type 1, and 651 genes of type 2 diabetes. 19 known genes were shared by type 1, type 2 and gestational diabetes, highlighting EGF, FAM46C, HBEGF, ID1, SH3BGRL2, VEPH1, and TMEM158 genes. The meta-analysis of PBMC transcription profiles characterized each type of diabetes revealing that gestational and type 1 diabetes were transcriptionally related.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Four major groups of diabetes mellitus have been recognized, type 1, type 2, gestational and other types. Type 1 diabetes accounts for ~10 % of all cases, affecting individuals under the age of 30 years. Several genes and gene regions distributed throughout the genome have been associated with susceptibility to type 1 diabetes, including the regions designated as insulin dependent diabetes mellitus—IDDM1 to IDDM18 [1]; however, the strongest genetic contribution comes from the HLA (IDDM1) and insulin gene (IDDM2) regions [2].
Type 2 diabetes accounts for ~90 % of all cases, developing after the age of 30 years and exhibiting no important autoimmune component; however, multi-genetic and metabolic factors, and family history have been reported. Although insulin resistance and progressive pancreatic β-cell dysfunction have been recognized as fundamental factors in the pathogenesis of type 2 diabetes [3], the specific molecular mechanisms that affect insulin sensitivity and β cell function remain unknown. The genomic scanning of susceptibility regions for type 2 diabetes included genes of cellular metabolism (PPARG, KCNJ11 and CAPN10) and transcription factors (HNF4A and TCF7L2) [4].
Gestational diabetes has been defined as any degree of impaired glucose tolerance with onset during pregnancy, affecting ~7 % of pregnant women. The genetic risk for gestational diabetes has been reported to be heterogeneous [5] and no genomic scanning has been reported for this type of diabetes. Gestational diabetes shares with type 2 diabetes clinical features, life-style risk factors and genetic susceptibility genes, including KCNJ11, TCF7L2, CDKAL1, CDKN2A/CDKN2B, HHEX/IDE, IGFBP2, SLC30A8, and FTO [6]. On the other hand, 10 % of gestational diabetes patients show high frequency of HLA-DRB1*03 and HLA-DRB1*04 allele groups, which is similar to type 1 diabetes patients, and may produce autoantibodies against pancreas antigens during and after pregnancy [7].
Peripheral blood lymphomononuclear cells (PBMCs) have been widely used in microarray experiments evaluating patients with distinct disorders, including diabetes [8] and pre-diabetes [9], as reporters of the underlying pathogenic processes. Considering the intermingled gene susceptibility and transcription profiles among the major types of diabetes mellitus, in the present study we performed a meta-analysis of the transcription profiles observed in PBMCs of these three types of diabetes, using the same microarray platform.
Materials and methods
Subjects
Peripheral blood lymphomononuclear cells were obtained from 56 patients, i.e., 19 type 1 diabetes patients (7 women) aged 18–36 years, 20 type 2 diabetes patients (13 women) aged 41–72 years, and 17 patients with gestational diabetes aged 23–40 years, followed-up at the Outpatient Clinics of the Division of Endocrinology, Faculty of Medicine of Ribeirao Preto, University of Sao Paulo, Brazil. Major demographic, laboratory and treatment features of type 1, type 2, and gestational diabetes patients are shown in Table 1. The local Ethics Committee approved the protocol of the study (# 9153/2008) and informed written consent was obtained from all patients.
Total RNA extraction
Cells were isolated using Ficoll-Hypaque (Sigma, St. Louis, MO). Total RNA was extracted using Trizol reagent (Invitrogen, Carlsbad, CA), confirmed to be free of proteins or phenol using UV spectrophotometry, and RNA integrity was assessed by microfluidic electrophoresis (Bioanalyzer Model 2100 and RNA 6000 nanochips, both from Agilent Technologies, Palo Alto, CA).
Microarray hybridization
Hybridizations to whole human genome 4 × 44K oligo microarrays (G4112F, Agilent) were performed using the one color (Cy3) Quick Amp labeling kit (Agilent). Samples of complementary RNA were hybridized for 17 h at 65 °C. Images were acquired using a DNA Microarray Scanner with Surescan High-Resolution Technology (Agilent). Hybridization quantitative numerical data and microarray quality control were performed using the Feature Extraction software (Agilent). All microarray data are available online at the MIAME database (type 1 diabetes: E-MEXP-3348; type 2 diabetes: E-MEXP-3287; gestational diabetes: E-MEXP-3349).
Microarray analysis
The GeneSpring GX version 11.0 software (Agilent) was used for background adjustment, quantile normalization data, log-transformation, and gene clustering. Gene ontology was performed using the GeneSpring or DAVID database (http://david.abcc.ncifcrf.gov/). Meta-analyses were performed using one-way analysis of variance (ANOVA) (three types of diabetes) or the unpaired T test (two types of diabetes), with p values set at p < 0.05. In both situations, the Benjamini–Hochberg false discovery rate multiple testing corrections were performed to minimize selection of false-positive values. Overall, in the present study were considered differentially and significantly expressed genes exhibiting expression values greater than two-folds (fold change ≥ 2.0). Hierarchical clustering of differentially expressed genes was performed using average linkage and the Pearson uncentered distance metrics. In this kind of clustering, the relationship among genes is represented by a tree, whose branch lengths reflect the degree of similarity between genes.
Results
Hierarchical clustering analysis of the transcription profiles displayed by PBMCs of type 1, type 2 and gestational diabetic patients individualized each patient group. Overall, the transcription profile exhibited by the group of gestational diabetes was closer to type 1 diabetes than to type 2 diabetes (Fig. 1); however, one patient with type 2 diabetes (T2DM-10) clustered with the type 1 diabetes group. No particular clinical feature exhibited by this patient distinguished him from the type 2 diabetes group, except that patient was usually compensated in terms of glucose (65 mg/dL) and HbA1c (6.5 %) levels.
Dendrogram showing the clustering of samples according to the gene expression profile encompassing 3,747 differentially and significantly expressed genes in patients with type 1 (T1DM), type 2 (T2DM) and gestational diabetes mellitus (GDM). The hierarchical clustering discriminated each type of diabetes and clustered gestational diabetes closer to type 1 diabetes than to type 2 diabetes
The meta-analysis encompassing type 1, type 2 and gestational diabetes revealed 3,747 differentially and significantly expressed genes, i.e., these genes exhibited fold-change ≥2.0 in at least one comparison between the diabetes groups. Among these genes, 805 were up-regulated and 570 were down-regulated. Overall, up-regulated genes were clustered into five major biological functions: (i) multicellular organism development (20.3 %), (ii) signal transduction (17.9 %), (iii) response to stress (12.2 %), (iv) cell differentiation (10.7 %), and (v) immune system processes (6.8 %). The down-regulated genes were primarily clustered into three processes: (i) metabolism regulation (30 %), (ii) biosynthetic pathways (26.9 %), and (iii) transcription machinery (22 %).
The multiple comparisons between the three types of diabetes revealed that: (i) 1,171 genes were differentially expressed between type 1 and gestational diabetes, (ii) 2,405 genes were differentially expressed between type 2 and gestational diabetes, and (iii) 1,509 genes were differentially expressed between type 1 and type 2 diabetes, of which, 486 genes were characteristic of gestational diabetes, 202 genes were specific for type 1, and 651 genes were typical of type 2 diabetes. Twenty-two transcripts were shared by type 1, type 2 and gestational diabetes, of which 19 have been defined by public gene banks. These data are shown in Fig. 2.
Sets of comparisons between type 1 (T1DM), type 2 (T2DM) and gestational diabetes mellitus (GDM) patients, showing private and shared genes in each type of diabetes. Twenty-two transcripts were shared and up-regulated in the three types of diabetes, of which 19 have been described in public databanks presenting known molecular and biological functions. The gene name, gene symbol and gene cytoband are also shown
A more restrictive analysis of modulated genes exhibiting fold-change ≥2.0 in all comparisons of the three diabetes groups yielded seven genes, that were up-regulated in all comparisons between groups (GDM vs T1DM, GDM vs T2DM, and T1DM vs T2DM) (Table 2).
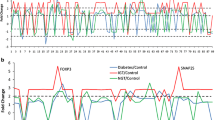
To circumvent the possible influence of gender on transcriptome profile, we performed a meta-analysis excluding men, and the expression profiles were maintained (Fig. 3). Considering that the median age of type 2 diabetes patients was higher than that of patients with other types, we reanalyzed data according to median age stratification of each group (GDM = 24 years; T1D = 33 years and T2D = 50 years), yielding four subgroups: (i) patients aged <24 years, (ii) patients aged between 24 and 33 years, (iii) patients aged between 33 and 50 years, and (iv) patients aged more than 50 years. Hierarchical clustering was not influenced by age, as shown in Fig. 4.
The clustering of samples according to the gene expression profile (3,966 differentially and significantly expressed genes), considering only female patients with type 1 (T1DM), type 2 (T2DM) and gestational diabetes mellitus (GDM), exhibited a similar profile as that observed encompassing both genders
Discussion
In this study, we assessed the hypothesis that each type of diabetes mellitus may display a specific expression profile signatures, and also may share sets of genes with similar expression profiles. To achieve this goal we performed a meta-analysis of the transcription profiles exhibited by each patient group, confirming that the overall gene expression profile is characteristic for each group of diabetic patients, and was not influenced by patient gender or age. Although these variables did not influence gene profiles, other variables including body mass index, disease duration, glucose and glycated hemoglobin levels, subset of peripheral lymphomononuclear cells, type of hypoglycemic agent, compensate or uncompensated disease, and others, may also be confounder factors that need to be evaluated, and will be a matter of our further and larger studies. Despite these possible confounding factors, we unveiled shared genes in each set of comparison between the three types of diabetes.
Several lines of clinical evidence emphasize more similarities between gestational diabetes and type 2 diabetes, rather than between gestational and type 1 diabetes [5]; however, the present study showed that the overall gestational diabetes transcriptional profile was closer to type 1 than to type 2 diabetes. Considering the whole group of gestational diabetes, these patients exhibited 5 % of their modulated genes in susceptibility regions previously described in association with type 1 diabetes [insulin-dependent diabetes mellitus regions (IDDM-1, 2, 3, 4, 6, 7, 8, 10, 11, 12, 13, 15, 17, 18, X) and PTPN22], and gestational diabetes exhibited only 0.5 % of differentially expressed genes that coincided with or were close to previously described type 2 diabetes susceptibility genes/regions. In addition, in the meta-analysis of the transcription profiles obtained for the three types of diabetes we observed that 50 (6.8 %) of the up-regulated genes were related to the immune response, including chemokines and chemokine receptors, interleukins, complement receptors, lymphocyte receptors among others. These findings corroborate the data of a recent study indicating that immune pathogenic mechanisms might be involved in gestational diabetes [7].
Considering the seven genes that were highly up-regulated in all patient comparisons, four of them (EGF, FAM46C, HBEGF, and ID1) have been previously described in association with at least one type of diabetes, but they have not been studied in all types of diabetes yet. Compared to healthy individuals, the expression of the EGF gene has been reported to be decreased after the onset of type 2 diabetes [10]. On the other hand, compared to non-diabetic pregnant women, it has been reported that gestational diabetes patients and their macrosomic children exhibited increased serum levels of EGF, and increased expression of the EGF receptor in placenta [11]. Taken together, the differential relative expression of EGF may be associated with an impairment of pancreas endocrine function and diabetes complications in gestational diabetes.
FAM46C encodes a type 1 interferon-stimulated protein that mediates the defense against invading viral pathogens and appears to contribute to the development of autoimmune diseases, including lupus, rheumatoid arthritis, multiple sclerosis, Sjögren’s syndrome and type 1 diabetes [12, 13]. Since the expression of this gene was up-regulated in gestational diabetes, and since it has been associated with autoimmune diseases, FAM46C gene may be of interest regarding the follow-up of gestational diabetes patients who develop post-pregnancy diabetes.
The HBEGF gene encodes an adipocytokine that contributes to the development of vascular diseases, and plasma HBEGF levels increase with the extent of obesity and of visceral adiposity [14]. The differential expression of this gene in three types of diabetes may be used as a tool to correlate body mass index and disease complications. The ID1 gene encodes a transcription factor that plays an important role during development and differentiation of many tissues and cells, and is essential for lymphocyte function and development. ID1 gene has been reported to be up-regulated in patients with rheumatoid arthritis [15] and in type 1 diabetes [16]. Therefore, the differential modulation of this gene in gestational and type 1 diabetes in relation to type 2 diabetes (Table 1) further supports the role of immune system genes on the pathogenesis of gestational diabetes.
The other three up-regulated genes (SH3BGRL2, VEPH1, and TMEM158) have not been previously studied in diabetes, deserving further studies. The SH3BGRL2 gene participates in mature red cell function and is important to protect erythrocytes against injurious oxygen effects [17]. The VEPH1 gene encodes a protein that is expressed during the development of the central nervous system [18], and the TMEM158 gene, which encodes a transmembrane protein, is up-regulated in response to the activation of the RAS pathway [19].
This is the first transcriptome study evaluating the three major types of diabetes using the same microarray platform. The meta-analysis of transcriptome profiles displayed by the three types of diabetes discriminated hybridization signatures, which were distinctive of each type of the disease, and showed that gestational diabetes hybridization signature is closer to type 1 than to type 2 diabetes. Besides, irrespective of the pathogenetic mechanisms involved in each type of diabetes, common sets of genes are similarly modulated.
References
Mehers KL, Gillespie KM (2008) The genetic basis for type 1 diabetes. Br Med Bull 88:115–129
Pugliese A, Miceli D (2002) The insulin gene in diabetes. Diabetes Metab Res Rev 18:13–25
Kahn CR (1994) Banting Lecture. Insulin action, diabetogenes, and the cause of type II diabetes. Diabetes 43:1066–1084
Prokopenko I, McCarthy MI, Lindgren CM (2008) Type 2 diabetes: new genes, new understanding. Trends Genet 24:613–621
Petry CJ (2010) Gestational diabetes: risk factors and recent advances in its genetics and treatment. Br J Nutr 104:775–787
Cho YM, Kim TH, Lim S, Choi SH, Shin HD, Lee HK, Park KS, Jang HC (2009) Type 2 diabetes-associated genetic variants discovered in the recent genome-wide association studies are related to gestational diabetes mellitus in the Korean population. Diabetologia 52:253–261
Lapolla A, Dalfra MG, Fedele D (2009) Diabetes related autoimmunity in gestational diabetes mellitus: is it important? Nutr Metab Cardiovasc Dis 19:674–682
Planas R, Pujol-Borrell R, Vives-Pi M (2010) Global gene expression changes in type 1 diabetes: insights into autoimmune response in the target organ and in the periphery. Immunol Lett 133:55–61
Kaizer EC, Glaser CL, Chaussabel D, Banchereau J, Pascual V, White PC (2007) Gene expression in peripheral blood mononuclear cells from children with diabetes. J Clin Endocrinol Metab 92:3705–3711
Al-Salam S, Hameed R, Parvez H, Adeghate E (2009) Pattern of distribution of IGF-1 and EGF in pancreatic islets of type 2 diabetic patients. Islets 1:102–105
Grissa O, Yessoufou A, Mrisak I, Hichami A, Amoussou-Guenou D, Grissa A, Djrolo F, Moutairou K, Miled A, Khairi H, Zaouali M, Bougmiza I, Zbidi A, Tabka Z, Khan NA (2010) Growth factor concentrations and their placental mRNA expression are modulated in gestational diabetes mellitus: possible interactions with macrosomia. BMC Pregnancy Childbirth 10:1–10
Crow MK (2010) Type I interferon in organ-targeted autoimmune and inflammatory diseases. Arthritis Res Ther 12(Supp l):S5
Silva GL, Junta CM, Sakamoto-Hojo ET, Donadi EA, Louzada-Junior P, Passos GA (2009) Genetic susceptibility loci in rheumatoid arthritis are differentially expressed and their mRNAs establish regulatory networks with other gene transcripts. Ann N Y Acad Sci 1173:521–537
Matsuzawa Y (2005) White adipose tissue and cardiovascular disease. Best Pract Res Clin Endocrinol Metab 19:637–647
Sakurai D, Yamaguchi A, Tsuchiya N, Yamamoto K, Tokunaga K (2001) Expression of ID family genes in the synovia from patients with rheumatoid arthritis. Biochem Biophys Res Commun 284:436–442
van Oostrom O, de Kleijn DP, Fledderus JO, Pescatori M, Stubbs A, Tuinenburg A, Lim SK, Verhaar MC (2009) Folic acid supplementation normalizes the endothelial progenitor cell transcriptome of patients with type 1 diabetes: a case–control pilot study. Cardiovasc Diabetol 8:1–11
De Andrade T, Moreira L, Duarte A, Lanaro C, De Albuquerque D, Saad S, Costa F (2010) Expression of new red cell-related genes in erythroid differentiation. Biochem Genet 48:164–171
Muto E, Tabata Y, Taneda T, Aoki Y, Muto A, Arai K, Watanabe S (2004) Identification and characterization of Veph, a novel gene encoding a PH domain-containing protein expressed in the developing central nervous system of vertebrates. Biochimie 86:523–531
Silva J, Silva JM, Barradas M, García JM, Domínguez G, García V, Peña C, Gallego I, Espinosa R, Serrano M, Bonilla F (2006) Analysis of the candidate tumor suppressor Ris-1 in primary human breast carcinomas. Mutat Res 594:78–85
Acknowledgments
This work was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP #2008/56594-8, FAPESP #2010/05622-1, FAPESP #210/00932-2, FAPESP #2010/12069-7).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Collares, C.V.A., Evangelista, A.F., Xavier, D.J. et al. Transcriptome meta-analysis of peripheral lymphomononuclear cells indicates that gestational diabetes is closer to type 1 diabetes than to type 2 diabetes mellitus. Mol Biol Rep 40, 5351–5358 (2013). https://doi.org/10.1007/s11033-013-2635-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-013-2635-y