Abstract
Mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes (MELAS) is a disease that should be considered as a differential diagnosis to acute ischemic stroke taking into account its onset pattern and neurological symptoms, which are similar to those of an ischemic stroke. Technological advancements in neuroimaging modalities have greatly facilitated differential diagnosis between stroke and MELAS on diagnostic imaging. Stroke-like episodes in MELAS have the following features: (1) symptoms are neurolocalized according to lesion site; (2) epileptic seizures are often present; (3) lesion distribution is inconsistent with vascular territory; (4) lesions are common in the posterior brain regions; (5) lesions continuously develop in adjacent sites over several weeks or months; (6) neurological symptoms and stroke-like lesions tend to be reversible, as presented on magnetic resonance imaging; (7) the rate of recurrence is high; and; (8) brain dysfunction and atrophy are slowly progressive. The m.3243ANG mutation in the MT-TL1 gene encoding the mitochondrial tRNALeu(UUR) is most commonly associated with MELAS. Although the precise pathophysiology is still unclear, one possible hypothesis for these episodes is a neuronal hyperexcitability theory, including neuron–astrocyte uncoupling. Supplementation, such as with L-arginine or taurine, has been proposed as preventive treatments for stroke-like episodes. As this disease is still untreatable and devastating, numerous drugs are being tested, and new gene therapies hold great promise for the future. This article contributes to the understanding of MELAS and its implications for clinical practice, by deepening their insight into the latest pathophysiological hypotheses and therapeutic developments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebrovascular diseases (e.g., cerebral infarction, cerebral hemorrhage, and subarachnoid hemorrhage) are commonly referred to as strokes, which generally develop suddenly and often present with an acute onset of neurological symptoms. The diagnosis in the clinical setting begins by asking patients and those around them the details about the condition at the time of onset. However, non-stroke diseases may also present with similar onset patterns and clinical symptoms. These diseases may be contraindicated for the same treatment as that for stroke; thus, care must be taken to distinguish between them.
One study has reported that 25% of 354 patients consecutively admitted to a stroke care unit had diseases other than stroke, as diagnosed by a non-specialist. Thus, when diagnosing stroke, clinicians must also keep these other diseases in mind (Rønning and Thommessen 2005). Generally, the frequency of stroke-mimicking diseases is about 15%–25%, and their diagnosis can greatly vary depending on the evaluator and timing of the evaluation (Gargalas et al. 2017; McClelland et al. 2019). The accuracy of stroke diagnosis is about 50%–60% in the emergency services department and improves to about 75%–85% in the initial treatment department and specialized stroke department. By adding image inspection, the frequency of diagnosing a stroke-mimicking disease as a stroke is greatly reduced; the frequency after brain computed tomography (CT) is 4%–5%, and after brain magnetic resonance imaging (MRI), it is 1%–2% (Davis et al. 2006; Vilela 2017).
However, in the case of mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes (MELAS), it is often difficult to distinguish this disease from acute ischemic stroke despite the close examination of its onset and diagnosis. In this article, we review the body of research on MELAS.
Features of MELAS
MELAS is a typical mitochondrial disease in that it is caused by abnormal metabolism in the mitochondria. Other mitochondrial diseases include myoclonus epilepsy associated with ragged-red fibers, Kearns–Sayre syndrome, and Leber’s hereditary optic neuropathy (LHON), which is the first disease associated with a mitochondrial DNA (mtDNA) point mutation. MELAS is characterized by hyperlactic acidosis, headache with nausea and vomiting similar to migraine, epilepsy, and stroke-like episodes, and in 1984, Pavlakis et al. (1984) proposed the concept of this disease.
Biochemically, in MELAS, the activity of Complex I nicotinamide adenine dinucleotide–coenzyme Q reductase and Complex IV cytochrome c oxidase, which are involved in the electron transport chain of mitochondria, is decreased. Such a decrease impairs the production of adenosine triphosphate (ATP), which is the energy required for cell activity. Symptoms are more likely to appear in the skeletal muscle and central nervous system, which are highly dependent on ATP produced by mitochondria. Table 1 presents the frequency of the clinical symptoms and complications of MELAS based on previous research and analyses, and the clinical findings can vary from case to case, and patients with the m.3243A > G mutation in MELAS are at increased risk for hypertension, with a reported rate of about 50% (Hirano and Pavlakis 1994; Yatsuga et al. 2012; El-Hattab et al. 2015; Pauls et al. 2020).
Numerous cases of MELAS develop by the time patients reach adulthood, with frequent epileptic seizures and stroke-like neurological symptoms. Biochemical tests can show elevated levels of lactate and pyruvate in the blood and cerebrospinal fluid. At the time of a stroke-like attack, brain neuroimaging findings suggest ischemia or edema showing a low absorption area on CT and a high signal area on MRI, including fluid-attenuated inversion recovery (FLAIR) and diffusion-weighted image (DWI), which are similar to a lesion found in cerebral infarction.
In 1990, Goto et al. identified the adenine-to-guanine transition at position 3243 of mtDNA (m.3243ANG) in the MT-TL1 gene encoding transfer RNA (tRNA)Leu(UUR) as the causative gene of MELAS (Goto et al. 1990). About 80% of patients with MELAS have this point mutation, but many other gene mutations have also been reported. Although mtDNA is maternally inherited, the mothers of patients with MELAS are often asymptomatic or have mild symptoms even with mutant mtDNA. This is because mtDNA is in a heteroplasmy state, in which mutant and wild types are mixed, and the proportion of mutant types is low in mothers. Moreover, the differences in the proportion of mutants due to heteroplasmy are observed not only within individuals but also within organs, tissues, and cells, indicating that cell function is impaired when the proportion of mutants exceeds a certain threshold. The clinical picture is also diversified by this heteroplasmy. Despite the existence of full-blown MELAS clinical presentation, which consists of mitochondrial encephalomyopathies, lactate acidosis, and stroke-like episodes (Yatsuga et al. 2012), the majority of m.3243A > G patients have a blinder phenotype, which implies that many carriers are clinically asymptomatic or have only mild disease not recognized as mitochondrial (Pickett et al. 2018). Although the gene mutations in MELAS have been elucidated, the pathological mechanism from mutation to stroke-like episodes is often unclear.
Recent studies have demonstrated that mitochondrial disease is one of the most prevalent groups of hereditary neurological diseases. The minimum prevalence rate for mtDNA mutations is 1 in 5,000, and the nuclear mutations for mitochondrial disease clinically affect 2.9–9.2 per 100,000 adults (Schaefer et al. 2008; Gorman et al. 2015). One study has found that 16.5 in 100,000 unaffected children and adults younger than the retirement age have a risk for developing mitochondrial disease (Schaefer et al. 2008). The m.3243A > G mutation responsible for MELAS is the most common pathogenic mtDNA point mutation, with a minimum prevalence of 3.5 of 100,000 people (Gorman et al. 2015).
Responsibility lesion and symptoms of stroke-like episodes
Researchers are still developing the pathophysiology for the stroke-like episodes of MELAS. However, clinically, MELAS has the following characteristics:
-
It presents with neurolocalization symptoms according to lesion site.
-
It is often accompanied by epileptic seizures.
-
The distribution of stroke-like lesions is inconsistent with a vascular territory.
-
The lesions are common in the posterior brain regions (i.e., the temporoparietal junction and the parietal and occipital lobes).
-
The cerebral cortex is preferentially involved, with bright thickened cortical bands showing on FLAIR images.
-
The lesions continuously develop to adjacent sites over several weeks or months.
-
Patients with MELAS tend to present spontaneous reversibility in both neurological symptoms and stroke-like lesions.
-
Both neurological symptoms and stroke-like lesions are highly recurrent.
-
Brain dysfunction and atrophy slowly progress.
Contrarily, in ischemic stroke, the lesions consistent with the cerebrovascular control area are observed on neuroimaging, and once captured on the image, the lesions do not disappear. Hemiplegia and dysarthria, which are typical stroke symptoms, are not common in MELAS. Even if those are observed, they are often caused by the effects of transient Todd’s paralysis, which is a complication following seizures or cerebral edema (Demarest et al. 2014).
As mentioned above, the lesion sites of MELAS are mostly in the posterior brain regions, but clinical symptoms can also reflect disorders in these brain regions. Cortical blindness, Anton syndrome, prosopagnosia, and regional geographic disorientation have been reported as visual symptoms of the occipital lobe (Kolb et al. 2003; Alemdar et al. 2007). Cases of sensory aphasia and auditory agnosia as symptoms of temporal lobe lesions have been reported, as have cases with constitutional disorders, left–right agnosia, and dysgraphia as symptoms of parietal lobe and related brain area lesions (Almasi et al. 2017; Tetsuka et al. 2017).
Figures 1 and 3 present the images of our MELAS cases (Tetsuka et al. 2017). A 68-year-old female patient developed convulsive seizures and was admitted to our hospital for epilepsy. Although she was an older adult, we suspected MELAS and detected elevated levels of pyruvic and lactic acids. A genetic test revealed a point mutation in the mtDNA (m.3243A > G) that led to a definitive diagnosis. However, the patient had been hospitalized twice in the previous year for suspected acute ischemic stroke and seizures.
(A, B and C): MRI examinations from May 2014 showing the MELAS migratory lesions. Cortical FLAIR (A) and DWI (B and C) sequences revealed hyperintensity in the left temporal lobe. (D, E and F): MRI examinations from October 2014 showing the MELAS migratory lesions. Cortical FLAIR (D) and DWI (E and F) sequences revealed hyperintensity in the right temporal lobe. Previous MRI findings of lesions on the right posterior temporal lobe had disappeared until the second admission after 5 months
At age 67 (in May 2014), the patient was admitted to another hospital for a suspected acute ischemic stroke, and a brain MRI there revealed hyperintensity in the left posterior temporal lobe (Fig. 1A, B, and C) (Tetsuka et al. 2017). No evident paralysis of the limbs was observed, but the patient exhibited a disturbance of consciousness and convulsive seizures. Five months after the previous admission (in October 2014), the patient was admitted to the same hospital for the same symptoms and received treatment for an acute ischemic stroke, for which a brain MRI revealed hyperintensity in the right posterior temporal lobe (Fig. 1D, E, and F) (Tetsuka et al. 2017). DWI and FLAIR of the brain MRI showed an acute ischemic stroke-like hyperintensity in the posterior part of the left temporal lobe, but previous MRI findings of the right posterior temporal lobe’s hyperintensity had disappeared. Similarities exist between the hyperintensity of DWI observed in the acute phase of seizure-induced lesions and that for an ischemic stroke. The abnormal signal of DWI in seizures is not caused by hypoxia/anoxia present during acute ischemic stroke but instead by a combination of impaired energy metabolism and hemodynamic changes. Therefore, DWI observed in seizures is often reversible (Shaw et al. 2012). MRI findings in the chronic phase are characterized by a variety of endpoints, including hypoperfusion, gadolinium enhancement, and regression of hyperintensities. Some stroke-like lesions tend to be spontaneously reversible, suggesting that neuronal and glial damage has not yet reached the point of irreversible damage (Finsterer and Aliyev 2020).
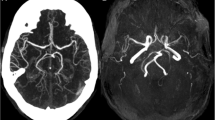
Figure 2 presents the single-photon emission CT (SPECT) and arterial spin labeling (ASL)-MRI at the time when an acute ischemic stroke-like lesion appeared with hyperintensity on the DWI and FLAIR sequence (Hongo et al. 2019). A significant increase in blood flow is observed at the lesion site in both SPECT and ASL-MRI (Fig. 2C and F), and this finding is clearly different from that for an acute ischemic stroke. In addition, normal and spontaneous brain activity in patients with MELAS was assessed using functional MRI in the recent study, and the reduction in brain activity was much more extensive than in stroke-like lesions (Wang et al. 2020).
Neuroimaging of adult-onset MELAS. Brain MRI (A, B) and 123I-IMP SPECT (C). DWI (A) and FLAIR (B) reveal slight hyperintensity in the left occipitotemporal cortex, and 123I-IMP SPECT marked hyperperfusion in the left occipitotemporal cortex (C). DWI (D) and FLAIR (E) demonstrate slight hyperintensity in the right medial frontal lobe and right occipital lobe, both of which are accompanied by focal hyperperfusion on the ASL-MRI (F). The figure was cited and reprinted by modifying from the reference (Hongo et al. 2019). Permission to reuse the figures has been granted by the publisher (Springer Nature)
A CT scan of the head revealed calcification around the basal ganglia (Fig. 3A and B) (Tetsuka et al. 2017). Mitochondrial disease is likely to be associated with abnormal calcium metabolism, and one study has reported that MELAS has been associated with calcification of the basal ganglia, occurring in up to 13% of cases (Majamaa et al. 1998). Although basal ganglia calcification is a common incidental finding in neuroimaging of older patients, this sign should enable clinicians to consider an underlying mitochondrial disease in the presence of other appropriate clinical features (Ciafaloni et al. 1992). As the disease state progresses, cerebral atrophy is a common feature of mitochondrial disease in childhood and adulthood (Fig. 3C) (Kim et al. 2009; Tetsuka et al. 2017). In a study of brain atrophy in MELAS patients using voxel-based morphometry, a significant decrease in gray matter volume was observed in the temporal subgyral regions (Tsujikawa et al. 2016). The cortical hyperintense signal during subacute or chronic stage compatible with cortical laminar necrosis pattern, this MRI finding is observed by a high incidence in patients with MELAS, suggesting a neuronal vulnerability (Fig. 3D) (Iizuka et al. 2002).
CT scan of the brain from April 2016 of a patient with MELAS. In retrospect, the additional clinical features and bilateral basal ganglia calcification (A and B) are suggestive of MELAS. MRI of the brain from April 2016 of a patient with MELAS. (C) Cortical atrophy was prominently recognized in the cerebellar cortex. FLAIR (D) sequences revealed white matter and cortical laminar necrosis-like findings and cortical atrophy in the left temporal lobe
As stroke-like lesions and brain atrophy as shown on the MRI spread slowly and progressively, Cognitive impairment develops in 40%–90% of patients with MELAS (Hirano and Pavlakis 1994; Yatsuga et al. 2012; El-Hattab et al. 2015). Damage to neurons throughout the brain due to mitochondrial dysfunction and cerebral cortex damage accumulated by stroke-like episodes can lead to cognitive impairment with impaired intelligence, language, perception, attention, and memory functions. On neuroimaging, despite the relatively mild frontal lobe abnormalities, executive dysfunction has been observed in patients with MELAS, suggesting a diffuse progressive neurodegeneration in addition to the damage caused by the stroke-like episodes (Sproule and Kaufmann 2008; El-Hattab et al. 2015). A recent study of cognitive impairment in MELAS patients with the m.3243A > G mutation showed a characteristic pattern of cognitive impairment: impaired attention, visual construction ability, and executive function and suggested that cognitive impairment in MELAS patients is caused in part by neurodegeneration and disturbances of brain metabolism (Kraya et al. 2019).
Seizure is another common neurological symptom that occurs in nearly 70%–90% of patients with MELAS (Hirano and Pavlakis 1994; Iizuka and Sakai 2010; Yatsuga et al. 2012; El-Hattab et al. 2015), which is a high frequency when compared with the incidence of early seizure accompanied by a stroke (8.9%) (Bladin 2000). In a study with 28 patients with MELAS, seizure or status epilepticus developed in 11 patients within 1 week after the onset of stroke-like episodes (Iizuka and Sakai 2010). However, some patients with MELAS can develop seizures without the finding of stroke-like lesions on the MRI (El-Hattab et al. 2015). Despite frequent, localized stroke-like episodes, both partial and generalized seizures can occur at about the same frequency (Iizuka and Sakai 2010). A high incidence of seizures during stroke-like episodes may suggest that the excitability of cortical neurons in the acute stroke-like lesions is higher in the active phase of these episodes compared with the interictal phase.
Pathogenesis of stroke-like episodes
Gene mutations such as the A3243G point mutation in mtDNA have been reported to cause MELAS; these mutations impair taurine modification at the first base of the anticodon of the tRNA against the wobble base pair (UUG). The mutant tRNA molecules are deficient in the uridine modification occurring in normal tRNALeu(UUR) at the first position of the anticodon wobble nucleotide. These modification defects can lead to the mistranslation of leucine into non-cognate phenylalanine codons by the mutant tRNALeu(UUR) (Yasukawa et al. 2000; Tsutomu et al. 2011). The pathogenic point mutation associated with MELAS is thought to prevent recognition by the tRNA-modifying enzymes. Taurine modification defects can lead to tRNA dysfunction, and human diseases caused by aberrant RNA modifications are now referred to as RNA modopathy, with MELAS being one of them (Torres et al. 2014; Asano et al. 2018). When translating a wobble base codon UUG, the codon can normally be recognized correctly by taurine modification of the first base of the corresponding tRNA, but research has demonstrated that the A3243G point mutation lacks taurine modification of tRNA during protein synthesis, resulting in unrecognized codon UUG and impaired protein synthesis (Fig. 4) (Yasukawa et al. 2001; Tsutomu et al. 2011; Kotrys and Szczesny 2019).
(A) Map of the human mitochondrial genome and the secondary structure of tRNALeu(UUR) associated with MELAS. (B and C) Distinct patterns of codon recognition identified in mutant tRNAs without wobble modification. (B) Normally, the taurine modification of uracil, the anticodon UAA of tRNALeu (UUR), can accurately recognize UUA as well as UUG and translate it into leucine. (C) Pathogenic point mutations (A3243G, G3244A, T3258C, T3271C, and T3291C) in mutant tRNALeu(UUR) of patients with MELAS causes a modification deficiency that results in a UUG codon-specific translational defect and induces impaired protein synthesis. The figure is cited by modifying from the references (Tsutomu et al. 2011; Kotrys and Szczesny 2019). Permission to reuse the figures has been granted by the publisher
However, the detailed pathological mechanism from impaired protein synthesis to stroke-like episodes has not been completely elucidated. Current theories explaining the mechanisms of stroke-like episodes include the mitochondrial angiopathy (vascular hypothesis) and mitochondrial cytopathy theories. The former is the theory of ischemic angiopathy caused by mitochondrial abnormalities inside the vascular smooth muscle cells and vascular endothelial cells on the cerebral surface arterioles and soft membrane arterioles. The latter is the theory of intracellular metabolic disorders caused by mitochondrial dysfunction (Iizuka and Sakai 2005). Regarding the vascular hypothesis, this theory assumes that when stroke-like episodes occur, a focal impairment of the cerebral arteries ensues. However, this has been inconsistent because magnetic resonance angiography (MRA) has usually been considered normal, with no arterial dilatation, significant stenosis, spasm, or dissection in any cerebral artery (Finsterer and Aliyev 2020). A recent systematic review has proposed the possibility of alterations in the caliber of major cerebral vessels on MRA during stroke-like episodes and the reversibility of vessel caliber alterations, which could play an important role in the pathophysiology of stroke-like lesions by altering intracranial hemodynamics (Gramegna et al. 2021). Mitochondrial metabolic dysfunction in the smooth muscle and endothelial cells of cerebral arteries may result in vessel caliber alterations, leading to mitochondrial angiopathy.
In addition, the excitability of neurons is enhanced because a stroke-like episode is likely to be accompanied by a convulsive attack. Therefore, neuronal hyperexcitability has been proposed as a pathological condition of a stroke-like episode (Iizuka and Sakai 2005). Furthermore, because acute ischemic stroke-like lesions expand to the surrounding cerebral cortex following a seizure, the epilepsy-like excitability of neurons is also considered to be involved in the expansion of lesion sites (Iizuka et al. 2003). The neuronal hyperexcitability theory predominantly assumes astrocyte dysfunction caused by ATP deficiency as the important mechanism. Astrocyte dysfunction causes poor uptake of glutamine via glutamate transporters and of Na+/K+ ATPase-mediated potassium into astrocytes. In addition, elevated glutamine and potassium levels in the synaptic cleft can induce not only vasodilation in cerebral small vessels but also neuronal cell death due to excitotoxicity (Fig. 5) (Haddy et al. 2006; Attwell et al. 2010; Iizuka and Sakai 2010; Chen et al. 2020). Given the spread of lesions with hyperperfusion beyond the arterial region (Fig. 2), stroke-like episodes are more likely to result from neuronal hyperexcitability than from mitochondrial angiopathy.
Neuronal hyperexcitability theory for MELAS predominantly assumes astrocyte dysfunction caused by ATP deficiency. Astrocyte dysfunction causes poor uptake of glutamine via glutamate transporters and of Na+/K+ ATPase-mediated potassium into astrocytes. Moreover, elevated glutamine and potassium levels in the synaptic cleft can induce not only vasodilation in cerebral small vessels but also neuronal cell death due to excitotoxicity. The oxygen metabolism of neurons and glucose metabolism of astrocytes are not coupled, resulting in a state of “neuron–astrocyte uncoupling,” and the prolongation of this condition is the pathological condition of the stroke-like episodes. Furthermore, astrocytes act on blood vessels to increase cerebral blood flow, but neurons cannot produce sufficient ATP, and the metabolism cannot keep up, resulting in an intracellular metabolic imbalance and damage to the cerebral cortex
Furthermore, the substances used by neurons as an energy source under normal conditions include both glucoses taken up from outside the cell and lactic acid supplied from astrocytes by the astrocyteneuron lactate shuttle (ANLS). Conversely, when the excitability of the neurons and the energy demand increase, the energy source becomes dependent on lactic acid derived from ANLS, which is used to produce ATP in the mitochondria (Pellerin et al. 2007). In addition, astrocytes activate themselves when they sense an increase in glutamate concentration in the synaptic cleft, that is, the activity of the neurons releases vasodilators and increases cerebral blood flow (Fig. 5). The action of these astrocytes synchronizes the increase and decrease of cerebral blood flow with brain activity and is referred to as neurovascular coupling (Iadecola 2017).
In MELAS, sufficient ATP cannot be produced to satisfy the energy demand, or the supplied lactic acid cannot be fully utilized due to the disorder of oxidative phosphorylation in the mitochondria. However, in the acute phase of stroke-like episodes, lactate supply from the astrocytes via ANLS increases. In other words, the oxygen metabolism of the neurons and the glucose metabolism of the astrocytes are not coupled, thus resulting in a state of “neuron–astrocyte uncoupling.” The prolongation of this condition may be the pathological condition of the stroke-like episodes. Moreover, astrocytes act on blood vessels to increase cerebral blood flow, but neurons cannot produce sufficient ATP, and the metabolism cannot keep up, resulting in an intracellular metabolic imbalance and damage to the cerebral cortex (Fig. 5) (Iizuka and Sakai 2005).
In MELAS, in addition to energy depletion, nitric oxide (NO) deficiency occurs, and research has demonstrated that this deficiency significantly influences the complication of the disease (El-Hattab et al. 2014). Nitric oxide synthase (NOS) is an enzyme that catalyzes the conversion of L-arginine to citrulline, and NO is also produced from L-arginine via NOS (Fig. 6). NOS mediates endothelium-dependent vascular relaxation. There are three known isoforms of NOS: two isoforms constitutively expressed (constitutive NOS), and inducible NOS, which becomes extremely abundant when stimulated by cytokines (Stuehr 1999). Citrulline is transformed into arginine by arginine succinate synthase and arginine succinate lyase. Therefore, both citrulline and arginine are required to produce NO. NO produced by vascular endothelial cells can relax vascular smooth muscle, which is necessary to maintain the patency of small vessels (Attwell et al. 2010). In MELAS, NO deficiency can result in impaired hemoperfusion in the microvasculature of various organs, thus affecting the etiology of some complications (El-Hattab et al. 2014). Decreased arginine and citrulline, which are NO precursors, can significantly affect impaired NO production. Decreased NO production can also result from the decreased activity of NOS caused by the overproduction of reactive oxygen species (ROS) due to the impaired electron transport chain (Desquiret-Dumas et al. 2012). Furthermore, oxidative stress caused by mitochondrial dysfunction can result in an increase in asymmetric dimethylarginine, an endogenous NOS inhibitor (El-Hattab et al. 2012). In the cerebrovascular endothelial smooth muscle cells, NO binds to guanylate cyclase and converts guanosine triphosphate to cyclic guanosine monophosphate (Fig. 6). This process leads to the relaxation of the smooth muscle cells and vasodilation of the blood vessels. NO has a strong affinity for cytochrome c in mitochondria, and the vascular endothelial cells and smooth muscle cells in patients with MELAS exhibit excessive activity of cytochrome c. As a result, NO binding is increased, and NO availability in the endothelial and smooth muscle cells is reduced (Fig. 6). Hemodynamic and metabolic stress further enhances NO mobilization and reduces circulating NO levels. NO deficiency causes episodes such as hypoxemia, seizure, and stroke in patients with MELAS (Vos et al. 2001). On the other hand, it has been reported that various cytokines in the cerebrospinal fluid are elevated in the acute phase of stroke-like attacks (Emsley and Tyrrell 2002). A recent study by utilizing induced pluripotent stem cells (iPSCs) derived from MELAS patient showed that the up-regulation of the expression levels of inflammatory genes such as intercellular adhesion molecule-1, vascular cell adhesion molecule-1, Interleukin-8 and Interleukin-6 in endothelial cells (MELAS iPSCs) (Pek et al. 2019). Considering these results, we can assume that because cytokines cause a NO-elevating effect, the resulting increased NO may cause vasodilatation in small vessels and hyperperfusion, leading to trigger a stroke-like episodes in MELAS.
Nitric oxide synthase (NOS) mediates endothelium-dependent vascular relaxation. NOS is an enzyme that catalyzes the conversion of L-arginine to citrulline. In the cerebrovascular endothelial smooth muscle cells, Nitric oxide (NO) binds to guanylate cyclase (GC) and converts guanosine triphosphate (GTP) to cyclic guanosine monophosphate (GMP). This process leads to the relaxation of the smooth muscle cells and vasodilation of the blood vessels. NO has a strong affinity for cytochrome c (Cyt c). In patients with MELAS, NO binding is increased, and NO availability is reduced
Management
Ubidecarenone, which is referred to as coenzyme Q, as an electron transport donor and Vitamins C and E as free radical scavengers may be administered to patients with MELAS, but currently, no radical treatment exists (Glover et al. 2010). Recently, L-arginine and taurine have been reported to be useful for suppressing stroke-like episodes, and future development is expected.
As mentioned above, NO exerts a vasodilatory effect, and L-arginine is a precursor of NO. Therefore, during a stroke-like attack, a decrease in L-arginine impairs arterial dilation, which might lead to cerebral ischemia. Furthermore, the administration of L-arginine to patients with MELAS results in vasodilation and might be effective in treating stroke-like episodes. In one clinical trial, L-arginine (0.5 g/kg) was administered intravenously during the acute phase of a total of 34 stroke-like episodes to 24 patients with MELAS. As a result, the scores of the subjective symptoms for headache, nausea, vomiting, visual field abnormalities, hemiplegia, and scintillating scotch improved in almost all cases within 30 min to 24 h after administration (Koga et al. 2005). Furthermore, 6 MELAS patients with frequent strokes were treated with oral L-arginine (0.15–0.3 g/kg/day) for 18 months as a preventive treatment for these strokes. As a result, the frequency of attacks per month was significantly reduced after administration (0.09 ± 0.09 times) than before administration (0.78 ± 0.42 times) (Koga et al. 2005).
In addition, in a 2-year clinical trial and a 7-year follow-up study, the systematic administration of oral and intravenous L-arginine to 15 and 10 patients with MELAS, respectively, was conducted prospectively (Koga et al. 2018). Oral L-arginine therapy prolonged the interictal phase (p = 0.0625) and reduced the incidence and severity of ictuses, and intravenous L-arginine therapy decreased the incidence of four major symptoms, namely, headache, nausea/vomiting, impaired consciousness, and visual disturbance. Furthermore, the systematic administration of L-arginine to patients with MELAS significantly improved their survival rate and maintaining the plasma arginine concentration of at least 168 mmol/l can prevent the ictuses (Koga et al. 2018). Although large-scale randomized controlled trials are required to better evaluate the efficacy of using L-arginine treatment for stroke-like episodes, these results can bring hopeful expectations to patients with MELAS (Ng et al. 2019).
As mentioned above, the MELAS mutation causes a disorder of taurine modification of the mitochondrial tRNALeu (UUR) in the MT-TL1 gene, and MELAS and taurine deficiency have been reported to be similar. The symptoms of MELAS, such as myocardial damage, diabetes, failure to thrive, hearing loss, muscle weakness, motor intolerance, and retinopathy, commonly appear in taurine deficiency in humans and various animals. Moreover, MELAS and taurine deficiency may have a common pathological mechanism (Schaffer et al. 2013). Rikimaru et al. conducted basic experiments and clinical studies on patients with MELAS to determine if high doses of taurine could improve neurological function and symptoms (Rikimaru et al. 2012). First, when taurine was added to cybrid cells into which mtDNA derived from MELAS patients was introduced, an increase in oxygen consumption, recovery of the decreased membrane potential, and reduction of oxidative stress were observed. In addition, when taurine (0.25 g/kg/day) was administered to two MELAS patients who had repeated seizures and stroke-like episodes, no recurrence of the seizures or episodes was observed thereafter. Serum lactic acid and pyruvate levels also decreased, and no new cerebral infarction-like lesions appeared on the MRI (Rikimaru et al. 2012).
Furthermore, a Phase III clinical trial of high-dose taurine supplementation has evaluated its efficacy for the prevention of the stroke-like episodes of MELAS (Ohsawa et al. 2019). In the trial, 10 patients with MELAS received oral high-dose taurine (9 or 12 g per day) for 52 weeks. As a result, six patients demonstrated complete elimination of their stroke-like episodes, and taurine reduced the annual relapse rate of these episodes from 2.22 to 0.72 (p = 0.001). A significant increase in the taurine modification of mitochondrial tRNALeu (UUR) was observed in the peripheral blood leukocytes of five patients, suggesting that high-dose taurine supplementation modified the mitochondrial tRNALeu (UUR) taurine deficiency and suppressed the recurrence of the stroke-like episodes (Ohsawa et al. 2019). On the basis of these results, additional insurance coverage has been approved for this treatment in Japan. However, a limitation of this study is the small number of patients satisfying the inclusion criteria. This means that a double-blind, placebo-controlled group could not be used in the previous clinical trials. On the other hand, a more recent study using iPSCs from a patient with MELAS has reported that MELAS iPSCs were affected by oxidative stress, and the deficits were rescued by taurine administration (Homma et al. 2021).
Many potential treatments for MELAS have been proposed and are currently in different stages of development. The mechanisms of action for these drugs are different and include decreasing ROS production, increasing NO production, enhancing mitochondrial biogenesis (nicotinamide riboside), and stabilizing the oxidized nicotinamide adenine dinucleotide modulator (Rahman and Rahman 2018). In addition, gene therapy using viral vectors to restore mitochondrial function has exhibited great potential in studies with animal models. The ultimate purpose of the gene therapy is the alternation of the heteroplasmy in the tRNA mutation model, sending the functional protein to the tissue with mutations of the respiratory chain subunit and correcting the mitochondrial defect through the use of viral vectors. A Phase III clinical trial of gene therapy is currently being conducted on patients with LHON, which is caused by mutations in the mitochondrially encoded MT-ND4 gene, and great expectations exist for the future, as these diseases are currently untreatable and devastating (Guy et al. 2017; Montano et al. 2021).
Conclusions
A quarter of a century has passed since the A3243G point mutation in the MT-TL1 gene, which is a typical causative gene for MELAS, was identified, and various pathological mechanisms are now being elucidated. Mitochondrial disease has a complicated pathological condition and is different from other hereditary diseases in numerous aspects, such as having the same gene mutation but different phenotypes. Several mechanisms can interact to result in stroke-like episodes in MELAS, including neuronal hyperexcitability, mitochondrial angiopathy, neuron–astrocyte uncoupling, and NO deficiency. However, in recent years, progress has been made toward the development of specific treatment methods. Because high-dose taurine supplementation modified the mitochondrial tRNALeu (UUR) taurine deficiency and suppressed the recurrence of stroke-like episodes in patients with MELAS, taurine administration has been a new practical and therapeutic approach for MELAS in the clinical setting. Due to the fact that this disease is this still untreatable and devastating, many drugs are currently being tested, and new gene therapies hold great promise for the future. It is hoped that the results of forthcoming research can lead to an improvement in the quality of life for patients with MELAS.
Data availability
The authors declare that data supporting the findings of this study are available within the article. The datasets are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- MELAS:
-
Mitochondrial encephalomyopathy with lactic acidosis and stroke-like episodes
- LHON:
-
Leber’s hereditary optic neuropathy
- mtDNA:
-
Mitochondrial DNA
- ATP:
-
Adenosine triphosphate
- FLAIR:
-
Fluid-attenuated inversion recovery
- DWI:
-
Diffusion-weighted image
- SPECT:
-
Single-photon emission CT
- ASL-MRI:
-
Arterial spin labeling MRI
- MRA:
-
Magnetic resonance angiography
- ANLS:
-
Astrocyteneuron lactate shuttle
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- ROS:
-
Reactive oxygen species
- iPSCs:
-
Induced pluripotent stem cells
- GC:
-
Guanylate cyclase
- GTP:
-
Converts guanosine triphosphate
- GMP:
-
Guanosine monophosphate
- Cyt c:
-
Cytochrome c
References
Alemdar M, Iseri P, Selekler M et al (2007) MELAS presented with status epilepticus and anton-babinski syndrome; value of adc mapping in MELAS. J Neuropsychiatr 19:482–483. https://doi.org/10.1176/appi.neuropsych.19.4.482
Almasi M, Motamed MR, Mehrpour M et al (2017) A mitochondrial disorder in a middle age iranian patient: report of a rare case. Basic Clin Neurosci 8:337–343. https://doi.org/10.18869/nirp.bcn.8.4.337
Asano K, Suzuki T, Saito A et al (2018) Metabolic and chemical regulation of tRNA modification associated with taurine deficiency and human disease. Nucleic Acids Res 46:1565–1583. https://doi.org/10.1093/nar/gky068
Attwell D, Buchan AM, Charpak S et al (2010) Glial and neuronal control of brain blood flow. Nature 468:232–243. https://doi.org/10.1038/nature09613
Bladin CF (2000) Seizures after stroke. Arch Neurol 57:1617. https://doi.org/10.1001/archneur.57.11.1617
Chen J, Zhang S, Wu J et al (2020) Essential role of nonessential amino acid glutamine in atherosclerotic cardiovascular disease. DNA Cell Biol 39:8–15. https://doi.org/10.1089/dna.2019.5034
Ciafaloni E, Ricci E, Shanske S et al (1992) MELAS: Clinical features, biochemistry, and molecular genetics. Ann Neurol 31:391–398. https://doi.org/10.1002/ana.410310408
Davis DP, Robertson T, Imbesi SG (2006) Diffusion-weighted magnetic resonance imaging versus computed tomography in the diagnosis of acute ischemic stroke. J Emerg Med 31:269–277. https://doi.org/10.1016/j.jemermed.2005.10.003
Demarest ST, Whitehead MT, Turnacioglu S et al (2014) Phenotypic analysis of epilepsy in the mitochondrial encephalomyopathy, lactic acidosis, and strokelike episodes-associated mitochondrial DNA A3243G mutation. J Child Neurol 29:1249–1256. https://doi.org/10.1177/0883073814538511
Desquiret-Dumas V, Gueguen N, Barth M et al (2012) Metabolically induced heteroplasmy shifting and l-arginine treatment reduce the energetic defect in a neuronal-like model of MELAS. Biochim Biophys Acta - Mol Basis Dis 1822:1019–1029. https://doi.org/10.1016/j.bbadis.2012.01.010
El-Hattab AW, Hsu JW, Emrick LT et al (2012) Restoration of impaired nitric oxide production in MELAS syndrome with citrulline and arginine supplementation. Mol Genet Metab 105:607–614. https://doi.org/10.1016/j.ymgme.2012.01.016
El-Hattab AW, Emrick LT, Chanprasert S et al (2014) Mitochondria: Role of citrulline and arginine supplementation in MELAS syndrome. Int J Biochem Cell Biol 48:85–91. https://doi.org/10.1016/j.biocel.2013.12.009
El-Hattab AW, Adesina AM, Jones J, Scaglia F (2015) MELAS syndrome: Clinical manifestations, pathogenesis, and treatment options. Mol Genet Metab 116:4–12. https://doi.org/10.1016/j.ymgme.2015.06.004
Emsley HCA, Tyrrell PJ (2002) Inflammation and infection in clinical stroke. J Cereb Blood Flow Metab 22:1399–1419. https://doi.org/10.1097/01.WCB.0000037880.62590.28
Finsterer J, Aliyev R (2020) Metabolic stroke or stroke-like lesion: Peculiarities of a phenomenon. J Neurol Sci 412:116726. https://doi.org/10.1016/j.jns.2020.116726
Gargalas S, Weeks R, Khan-Bourne N et al (2017) Incidence and outcome of functional stroke mimics admitted to a hyperacute stroke unit. J Neurol Neurosurg Psychiatry 88:2–6. https://doi.org/10.1136/jnnp-2015-311114
Glover EI, Martin J, Maher A et al (2010) A randomized trial of coenzyme Q10 in mitochondrial disorders. Muscle Nerve 42:739–748. https://doi.org/10.1002/mus.21758
Gorman GS, Schaefer AM, Ng Y et al (2015) Prevalence of nuclear and mitochondrial DNA mutations related to adult mitochondrial disease. Ann Neurol 77:753–759. https://doi.org/10.1002/ana.24362
Goto YI, Nonaka I, Horai S (1990) A mutation in the tRNALeu(UUR) gene associated with the MELAS subgroup of mitochondrial encephalomyopathies. Nature 348:651–653
Gramegna LL, Cortesi I, Mitolo M, et al (2021) Major cerebral vessels involvement in patients with MELAS syndrome: Worth a scan? A systematic review. J Neuroradiol = J Neuroradiol. https://doi.org/10.1016/j.neurad.2021.02.002
Guy J, Feuer WJ, Davis JL et al (2017) Gene therapy for leber hereditary optic neuropathy: low- and medium-dose visual results. Ophthalmology 124:1621–1634. https://doi.org/10.1016/j.ophtha.2017.05.016
Haddy FJ, Vanhoutte PM, Feletou M (2006) Role of potassium in regulating blood flow and blood pressure. Am J Physiol - Regul Integr Comp Physiol 290:546–552. https://doi.org/10.1152/ajpregu.00491.2005
Hirano M, Pavlakis SG (1994) Mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes (MELAS): Current concepts. J Child Neurol 9:4–13. https://doi.org/10.1177/088307389400900102
Homma K, Toda E, Osada H et al (2021) Taurine rescues mitochondria-related metabolic impairments in the patient-derived induced pluripotent stem cells and epithelial-mesenchymal transition in the retinal pigment epithelium. Redox Biol 41:101921. https://doi.org/10.1016/j.redox.2021.101921
Hongo Y, Kaneko J, Suga H et al (2019) A cluster of disseminated small cortical lesions in MELAS: its distinctive clinical and neuroimaging features. J Neurol 266:1459–1472. https://doi.org/10.1007/s00415-019-09283-3
Iadecola C (2017) The neurovascular unit coming of age: a journey through neurovascular coupling in health and disease. Neuron 96:17–42. https://doi.org/10.1016/j.neuron.2017.07.030
Iizuka T, Sakai F (2005) Pathogenesis of stroke-like episodes in melas: Analysis of neurovascular cellular mechanisms. Curr Neurovasc Res 2:29–45. https://doi.org/10.2174/1567202052773544
Iizuka T, Sakai F (2010) Pathophysiology of stroke-like episodes in MELAS: Neuron-astrocyte uncoupling in neuronal hyperexcitability. Future Neurol 5:61–83. https://doi.org/10.2217/fnl.09.71
Iizuka T, Sakai F, Suzuki N et al (2002) Neuronal hyperexcitability in stroke-like episodes of MELAS syndrome. Neurology 59:816–824. https://doi.org/10.1212/WNL.59.6.816
Iizuka T, Sakai F, Kan S, Suzuki N (2003) Slowly progressive spread of the stroke-like lesions in MELAS. Neurology 61:1238–1244. https://doi.org/10.1212/01.WNL.0000091888.26232.FE
Kim JT, Lee YJ, Lee YM et al (2009) Clinical characteristics of patients with non-specific and non-categorized mitochondrial diseases. Acta Paediatr Int J Paediatr 98:1825–1829. https://doi.org/10.1111/j.1651-2227.2009.01428.x
Koga Y, Akita Y, Nishioka J et al (2005) L-Arginine improves the symptoms of strokelike episodes in MELAS. Neurology 64:710–712. https://doi.org/10.1212/01.WNL.0000151976.60624.01
Koga Y, Povalko N, Inoue E et al (2018) Therapeutic regimen of l-arginine for MELAS: 9-year, prospective, multicenter, clinical research. J Neurol 265:2861–2874. https://doi.org/10.1007/s00415-018-9057-7
Kolb SJ, Costello F, Lee AG et al (2003) Distinguishing ischemic stroke from the stroke-like lesions of MELAS using apparent diffusion coefficient mapping. J Neurol Sci 216:11–15. https://doi.org/10.1016/S0022-510X(03)00218-1
Kotrys AV, Szczesny RJ (2019) Mitochondrial gene expression and beyond-novel aspects of cellular physiology. Cells 9. https://doi.org/10.3390/cells9010017
Kraya T, Neumann L, Paelecke-Habermann Y et al (2019) Cognitive impairment, clinical severity and MRI changes in MELAS syndrome. Mitochondrion 44:53–57. https://doi.org/10.1016/j.mito.2017.12.012
Majamaa K, Moilanen JS, Uimonen S et al (1998) Epidemiology of A3243G, the mutation for mitochondrial encephalomyopathy, lactic acidosis, and strokelike episodes: Prevalence of the mutation in an adult population. Am J Hum Genet 63:447–454. https://doi.org/10.1086/301959
McClelland G, Rodgers H, Flynn D, Price CI (2019) The frequency, characteristics and aetiology of stroke mimic presentations: A narrative review. Eur J Emerg Med 26:2–8. https://doi.org/10.1097/MEJ.0000000000000550
Montano V, Gruosso F, Simoncini C et al (2021) Clinical features of mtDNA-related syndromes in adulthood. Arch Biochem Biophys 697:108689. https://doi.org/10.1016/j.abb.2020.108689
Ng YS, Bindoff LA, Gorman GS et al (2019) Consensus-based statements for the management of mitochondrial stroke-like episodes. Wellcome Open Res 4:1–13. https://doi.org/10.12688/wellcomeopenres.15599.1
Ohsawa Y, Hagiwara H, Nishimatsu SI et al (2019) Taurine supplementation for prevention of stroke-like episodes in MELAS: A multicentre, open-label, 52-week phase III trial. J Neurol Neurosurg Psychiatry 90:529–536. https://doi.org/10.1136/jnnp-2018-317964
Pauls AD, Sandhu V, Young D et al (2020) High rate of hypertension in patients with m.3243A>G MELAS mutations and POLG variants. Mitochondrion 53:194–202. https://doi.org/10.1016/j.mito.2020.05.011
Pavlakis SG, Phillips PC, DiMauro S et al (1984) Mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes: A distinctive clinical syndrome. Ann Neurol 16:481–488. https://doi.org/10.1002/ana.410160409
Pek NMQ, Phua QH, Ho BX et al (2019) Mitochondrial 3243A > G mutation confers pro-atherogenic and pro-inflammatory properties in MELAS iPS derived endothelial cells. Cell Death Dis 10. https://doi.org/10.1038/s41419-019-2036-9
Pellerin L, Bouzier-Sore A-K, Aubert A et al (2007) Activity-dependent regulation of energy metabolism by astrocytes: An update. Glia 55:1251–1262. https://doi.org/10.1002/glia.20528
Pickett SJ, Grady JP, Ng YS et al (2018) Phenotypic heterogeneity in m.3243A>G mitochondrial disease: The role of nuclear factors. Ann Clin Transl Neurol 5:333–345. https://doi.org/10.1002/acn3.532
Rahman J, Rahman S (2018) Mitochondrial medicine in the omics era. Lancet 391:2560–2574. https://doi.org/10.1016/S0140-6736(18)30727-X
Rikimaru M, Ohsawa Y, Wolf AM et al (2012) Taurine Ameliorates Impaired the Mitochondrial Function and Prevents Stroke-like Episodes in Patients with MELAS. Intern Med 51:3351–3357. https://doi.org/10.2169/internalmedicine.51.7529
Rønning OM, Thommessen B (2005) [Stroke: when the diagnosis is wrong]. Tidsskr den Nor Laegeforening 125:1655–1657. https://tidsskriftet.no/2005/06/aktuelt/nar-hjerneslagdiagnosen-er-feil. Accessed 22 Apr 2021
Schaefer AM, McFarland R, Blakely EL et al (2008) Prevalence of mitochondrial DNA disease in adults. Ann Neurol 63:35–39. https://doi.org/10.1002/ana.21217
Schaffer SW, Jong CJ, Warner D et al (2013) Taurine deficiency and MELAS are closely related syndromes. Adv Exp Med Biol 776:153–165. https://doi.org/10.1007/978-1-4614-6093-0_16
Shaw S, Kim P, Millett D (2012) Status epilepticus amauroticus revisited: Ictal and peri-ictal homonymous hemianopsia. Arch Neurol 69:1504–1507. https://doi.org/10.1001/archneurol.2012.317
Sproule DM, Kaufmann P (2008) Mitochondrial encephalopathy, lactic acidosis, and strokelike episodes: Basic concepts, clinical phenotype, and therapeutic management of MELAS syndrome. Ann N Y Acad Sci 1142:133–158. https://doi.org/10.1196/annals.1444.011
Stuehr DJ (1999) Mammalian nitric oxide synthases. Biochim Biophys Acta - Bioenerg 1411:217–230. https://doi.org/10.1016/S0005-2728(99)00016-X
Tetsuka S, Tagawa A, Ogawa T et al (2017) Importance of distinguishing between mitochondrial encephalomyopathy with elderly onset of stroke-like episodes and cerebral infarction. J Clin Med Res 9:812–819. https://doi.org/10.14740/jocmr3122w
Torres AG, Batlle E, Ribas de Pouplana L (2014) Role of tRNA modifications in human diseases. Trends Mol Med 20:306–314. https://doi.org/10.1016/j.molmed.2014.01.008
Tsujikawa K, Senda J, Yasui K et al (2016) Distinctive distribution of brain volume reductions in MELAS and mitochondrial DNA A3243G mutation carriers: A voxel-based morphometric study. Mitochondrion 30:229–235. https://doi.org/10.1016/j.mito.2016.08.011
Tsutomu S, Asuteka N, Takeo S (2011) Human mitochondrial diseases caused by lack of taurine modification in mitochondrial tRNAs. Wiley Interdiscip Rev RNA 2:376–386. https://doi.org/10.1002/wrna.65
Vilela P (2017) Acute stroke differential diagnosis: Stroke mimics. Eur J Radiol 96:133–144. https://doi.org/10.1016/j.ejrad.2017.05.008
Vos MH, Lipowski G, Lambry JC et al (2001) Dynamics of nitric oxide in the active site of reduced cytochrome c oxidase aa3. Biochemistry 40:7806–7811. https://doi.org/10.1021/bi010060x
Wang R, Li Y, Lin J et al (2020) Altered spontaneous brain activity at attack and remission stages in patients with mitochondrial encephalomyopathy, lactic acidosis and stroke-like episodes (MELAS): Beyond stroke-like lesions. Mitochondrion 54:49–56. https://doi.org/10.1016/j.mito.2020.07.002
Yasukawa T, Suzuki T, Suzuki T et al (2000) Modification defect at anticodon wobble nucleotide of mitochondrial tRNAs(Leu)(UUR) with pathogenic mutations of mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes. J Biol Chem 275:4251–4257. https://doi.org/10.1074/jbc.275.6.4251
Yasukawa T, Suzuki T, Ishii N et al (2001) Wobble modification defect in tRNA disturbs codon-anticodon interaction in a mitochondrial disease. EMBO J 20:4794–4802. https://doi.org/10.1093/emboj/20.17.4794
Yatsuga S, Povalko N, Nishioka J et al (2012) MELAS: A nationwide prospective cohort study of 96 patients in Japan. Biochim Biophys Acta - Gen Subj 1820:619–624. https://doi.org/10.1016/j.bbagen.2011.03.015
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Contributions
The concept and idea of the study was designed by ST. The manuscript was written by ST and TO. ST, RH and HK revised the manuscript and edited English. RH and HK critically revised the important content of the revision. RH and HK contributed immensely to the amendments. All authors have approved final article version.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Informed consent to participate
A written parental consent was obtained for publication of the MRI and CT material that is inserted in Figs. 1 and 3.
Consent for publication
All authors have read the manuscript and given their consent for publication.
Conflict of interest
Authors declare no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Lesion distribution is inconsistent with vascular territory.
• MELAS tends to present spontaneous reversibility of both neurological symptoms and stroke-like lesions, but both of those are prone to relapse later.
• The m.3243ANG mutation in the MT-TL1 gene encoding the mitochondrial tRNALeu(UUR) is commonly associated with MELAS.
• The mutation affects the taurine modification of tRNA and impairs protein synthesis.
• Neuronal hyperexcitability is a hypothesized cause of these episodes.
• Taurine administration is a new, practical, and therapeutic approach for MELAS.
• New gene therapies hold great promise for the future.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tetsuka, S., Ogawa, T., Hashimoto, R. et al. Clinical features, pathogenesis, and management of stroke-like episodes due to MELAS. Metab Brain Dis 36, 2181–2193 (2021). https://doi.org/10.1007/s11011-021-00772-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-021-00772-x