Abstract
Maple syrup urine disease (MSUD) is characterized by a deficiency in the mitochondrial branched-chain α-keto acid dehydrogenase complex activity and, consequently, accumulation of the branched-chain amino acids and their respective branched-chain α-keto acids in fluids and the tissue. MSUD clinical symptoms include neurological alterations. KIC is considered one of the significant neurotoxic metabolites since its increased plasma concentrations are associated with neurological symptoms. We evaluated the effect of KIC intracerebroventricular (ICV) injection in hippocampal mitochondria function in rats. We also investigated the impact of KIC in cells’ metabolic activity (using MTT assay) and reactive species (RS) production in HT-22 cells. For this, thirty-day-old male rats were bilaterally ICV injected with KIC or aCSF. Thus, 1 hour after the administration, animals were euthanized, and the hippocampus was harvested for measured the activities of mitochondrial respiratory chain enzymes and RS production. Furthermore, HT-22 cells were incubated with KIC (1–10 mM) in 6, 12, and 24 h. Mitochondrial complexes activities were reduced, and the formation of RS was increased in the hippocampus of rats after KIC administration. Moreover, KIC reduced the cells’ metabolic ability to reduce MTT and increased RS production in hippocampal neurons. Impairment in hippocampal mitochondrial function seems to be involved in the neurotoxicity induced by KIC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maple syrup urine disease (MSUD) is an inborn error generated by the deficiency in the activity of the branched-chain α-keto acid dehydrogenase complex (BCKAD). This impairment in the complex enzymatic activity leads to an accumulation of the branched-chain amino acids (BCAAs) and their respective branched-chain α-keto acids (BCKA), α-ketoisocaproic acid (KIC), α-keto-β-methylvaleric acid (KMV) and α-ketoisovaleric acid (KIV), in tissue and biological fluids (Chuang and Shih 2001; Strauss and Morton 2003). MSUD has a worldwide incidence of 1: 185,000 live births (Chuang and Shih 2001).
The clinical symptoms frequently presented by MSUD patients are convulsions, ketoacidosis, apnea, ataxia, psychomotor delay, mental retardation, coma, and hypomyelination/demyelination (Chuang and Shih 2001). Moreover, BCAA metabolism disorders can cause abnormalities in glutamate synthesis, leading to various neurological problems in affected patients (Scaini et al. 2017).
Although numerous mechanisms have been proposed, the exact pathophysiology of MSUD has not yet been described. It is worth mentioning that KIC and Leucine are considered the primary neurotoxic metabolites. In fact, increased plasma concentrations of these metabolites are associated with the appearance of neurological symptoms (Snyderman et al. 1964; Chuang and Shih 2001). Moreover, it has been described that metabolites accumulation in MSUD causes inhibition in the brain energy metabolism (i.e., mitochondrial dysfunction) (Sgaravatti et al. 2003; Ribeiro et al. 2008), reduced antioxidant defenses (Bridi et al. 2005; Taschetto et al. 2017), oxidative stress (Bridi et al. 2005; Mescka et al. 2011; Sitta et al. 2014; Funchal et al. 2006), and decreased brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF) levels in the brain structures (Wisniewski et al. 2016).
A model used to mimic the damage caused by KIC is through the intracerebroventricular (ICV) administration of the KIC, which was first performed by De Castro Vasques and collaborators (De Castro Vasques2004) and adapted by Wisniewski and collaborators (Wisniewski et al. 2016). These studies demonstrated that KIC in the brain triggered learning deficits and behavioral changes in rats (De Castro Vasques et al. 2004; Taschetto et al. 2017), as well as led to decreased brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF) levels and oxidative stress in the cerebral regions, such as the hippocampus (Wisniewski et al. 2016; Taschetto et al. 2017). Some in vitro studies also reported decreased cerebral energy metabolism caused by KIC exposure, characterized by the inhibited activity of α-ketoglutarate dehydrogenase, reduced oxygen consumption in state 3 respiration, impaired ΔΨm mitochondrial (Amaral et al. 2010), reduced oxygen uptake by brain slices (Howell and Lee 1963), inhibition of CO2 formation, and increased lactate release (Sgaravatti et al. 2003). In this regard, this study’s purpose was to demonstrate the effects of KIC on mitochondrial function and formation of reactive species (RS) in the hippocampus in vivo and in vitro. Importantly, the hippocampus is the brain area more associated with behavior (Izquierdo and Medina 1997) and memory formation (Voss et al. 2017), which were affected by KIC in experimental models and MSUD patients.
Materials and methods
In vivo Study
Animals
In this study were used 25 young male Wistar rats (30-day-old) obtained from the Central Animal House of the Universidade do Extremo Sul Catarinense (UNESC) (weighing 60–80 g). Rats were caged in groups of five with free access to water and food and maintained on a 12-h light/dark cycle at the constant temperature of 23 ºC. All experimental procedures were approved by the ethics committee of the UNESC (protocol number 050/2018-1), following the Brazilian regimentation for the care and use of animals for scientific and didactic purposes.
KIC intracerebroventricular administration
Thirty-day-old male Wistar rats were anesthetized with ketamine (80 mg/kg) and xylazine (10 mg/kg), i.p. Next, animals were placed on a stereotaxic apparatus, and two small holes (bilateral) were drilled in the skull for the injection of 2 µL KIC or aCSF (control). The solutions were slowly injected over 4 min into the lateral ventricle. The needle was left in the place for another 1 min before being softly removed. The coordinates for injections were as follows: 0.6 mm posterior to bregma, 1.0 mm lateral to the midline, and 3.2 mm ventral from the dura mater (Paxinos and Watson 2007). The KIC solution (4 µmol, pH 7.4) was dissolved in freshly prepared artificial CSF (aCSF) (147 mM NaCl; 2.9 mM KCl; 1.6 mM MgCl2; 1.7 mM CaCl2 and 2.2 mM dextrose) (De Castro Vasques et al. 2004). One hour after the administration, the animals were killed by decapitation, and the hippocampus was dissected (Fig. 1a).
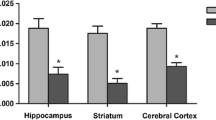
Acute effect of intracerebroventricular administration of α-ketoisocaproic acid (KIC) on complex I (b), complex II (c), complex II-III (d), complex IV (e) activities of mitochondrial respiratory chain and DCF levels (f) in the hippocampus of young rats (n = 6 animals per group). The values are representative of mean + SEM. *p < 0.05 compared with the control group. ***p < 0.001 compared with the control group). (Student’s t test)
In vitro study
Cell culture
The HT-22 cells (mouse hippocampal cells) were maintained in Dulbecco’s modified Eagle’s medium (DMEM) with 10% fetal bovine serum (FBS) and antibiotics (100 IU/ml penicillin and 100 µg/ml streptomycin) at 37 °C, with 5% CO2, under standard conditions. The HT-22 cells were gently donated by Professor Marcelo Farina (Universidade Federal de Santa Catarina, Departamento de Bioquímica, SC, Brazil).
Biochemical analysis
Activities of mitochondrial respiratory chain enzymes
The hippocampus was weighed and then homogenized in SETH buffer (1:10, w/v) (250 mM sucrose, 2 mM EDTA, 10 mM Trizma base, 50 IU/ml heparin), pH 7.4. The homogenates were centrifuged at 3,000 RPM for 10 min, at 4 ºC, and the supernatants kept at -70 °C until being used the determination of respiratory chain enzyme activities.
NADH dehydrogenase (complex I) activity was evaluated according to Cassini and Radi (1996). The activity of complex II (succinate-2,6-dichloroindophenol -oxidoreductase) and the activity of succinate: cytochrome c oxidoreductase (complex III) were evaluated, according to the method of Fischer et al. (1985). Finally, the activity of cytochrome c oxidase (complex IV) was measured, according to Rustin et al. (1994) method. All the results were expressed as nmol.min-1.mg protein-1.
MTT assay
Cells’ metabolic activity was evaluated by MTT assay. HT-22 cells were seeded into 96-well plates in DMEM with 10% FBS (1 × 104 cells/well). After 24 h of incubation, the cells were treated with different concentrations of KIC (1, 2, 5, and 10 mM dissolved in aCSF) or aCSF in DMEM with 1% FBS. The incubation times were 6, 12, and 24 h. Next, the cells were incubated with MTT solution (5 mg/mL) for three h at 37ºC. Then, the cells’ metabolic activity was measured by the reduction of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), which assesses the activity of labile mitochondrial dehydrogenases. The formazan formed was dissolved in 300 µL of dimethyl sulfoxide (DMSO). The formazan formed was dissolved in 300 µL of dimethyl sulfoxide (DMSO). Results of MTT tests were expressed as the percentage of cells incubated with aCSF. All experiments were performed in technical triplicate (Fig. 2a).
KIC reduced cells’ metabolic activity and induced intracellular RS formation in HT-22 cells. HT-22 cells were exposed to different KIC concentrations (1, 2, 5, 10 mM) for 6, 12 and 24 h. Cell viability was evaluated by the reduction of MTT (b). RS production in mouse hippocampal neuronal cells (c and d). HT-22 cells were exposed to KIC (1, 2, 5 and 10 mM) for 6, 12 and 24 hours (c) or 1 h (d). Results of the MTT test are expressed as the percentage of MTT reduction with respect to control values. (n = 6 animals per group). The values are representative of mean + SEM *p < 0.05 compared with your respective control. **p < 0.01 compared with your respective control, ****p < 0.0001 compared with your respective control, #p < 0.05compared with respective concentration in 6 hour, ###p < 0.001 compared with respective concentration in 6 hour, &p < 0.05 compared with respective concentration in 12 hour, $$p < 0.005 compared with 1 mM in respective time, $$$p < 0.001 compared with 1 mM in respective time, $$p < 0.0001 compared with 1 mM in respective time, ++++<0.0001 compared with 5 mM in respective time. (One-way and two-way ANOVA). RFU = Relative Fluorescence Units
Measurement of reactive species (RS) production
For the in vivo studies, the tissue was homogenized in a 50 mM phosphate buffer with 20 mM KCl. The resulting suspension was centrifuged at 3,000 × g for 10 min in the sequence, and the supernatant was used for the tests. The oxidation intracellular 2′,7′-dichlorofluorescein (DCF) were monitored in samples incubated with 2′,7′- dichlorodihydrofluorescein diacetate (DCFH-DA). The oxidized fluorescent derivate formation was monitored at excitation and emission wavelengths of 488 and 525 nm, respectively, using a fluorescence spectrophotometer (Lebel et al. 1990), and results were expressed as U fluorescence/mg protein.
For the in vitro study, the level of intracellular RS was detected using 2′7′-dichlorofluorescein diacetate DCFH-DA. HT-22 cells were seeded into 96-well plates at a density of 1 × 104 cells/well. After 24 h of incubation, cells were treated with DCFH-DA (10 µM) 30 minutes before (for the kinetic protocol) or after (in the 6, 12, and 24 h assay) the KIC exposure (1, 2, 5, and 10 mM dissolved in aCSF). The fluorescence intensity was measured using a spectrofluorometer (488 nm excitation and 520 nm emission), and results were expressed as Relative Fluorescence Units (RFU).
Protein Determination
Protein content was determined by the method described by Lowry and collaborators (Lowry et al. 1951), using bovine serum albumin as standard.
Statistical analyses
Data are displayed as means + SEM. Data were carried out using Student’s t-test (in vivo studies) one-way (Measurement of RS production in 1 hour) and two-way analysis of variance (ANOVA) (MTT assay and measurement of RS production). Differences between the groups were considered to be significant at p < 0.05. All analyses were carried using the STATISTICA8® software package (StatSoft Inc, Tulsa, OK, USA).
Results
KIC reduced mitochondrial complexes activity in the hippocampus of rats
The respiratory chain consists of four complexes. The mitochondrial complexes produce most of the ATP needed by the aerobic cells. Dysfunction of mitochondrial energy metabolism leads to reduced ATP production and increased generation of RS (Halliwell 2001). Herein we evaluated the effects of KIC exposure on respiratory complexes activities in the hippocampus of infant rats. The protocol of administration used for mimic the damage of KIC in the brain reduced the complex I (t (10) = 3.005, p = 0.0132) (Fig. 1b), complex II – III (t (10) = 5.533, p = 0.0003) activities (Fig. 1d) in the hippocampus of infant rats, in comparison with control rats. In contrast, KIC exposure did not alter the complex II (t (12) = 0.4983, p = 0.6273) (Fig. 1c) and complex IV (t (8) = 1.293, p = 0.2322) (Fig. 1e) activities.
KIC exposure induced elevated RS production in the hippocampus of rats
Intracellular production of RS occurs mainly in mitochondria, mainly in Complex I (Zorov et al. 2014). Thereby, mitochondrial respiratory chain complexes dysfunction could lead to an elevated RS formation. Our results showed that the ICV administration of KIC caused a significant increase in oxidation of DCFH in the hippocampus (t = 2.792, p = 0.0190) compared with the control group (Fig. 1f).
KIC reduced metabolic activity and increased intracellular RS production in HT-22 cells
In sequence, KIC at concentrations of 1, 2, 5 and 10 mM were tested on HT-22 cells for 6, 12 and 24 h (Fig. 2a). Figure 2b shows that the cells’ metabolic ability to reduce MTT decreased after exposure to 10 mM KIC for 6 h (p = < 0,0001), 12 h (p = 0,0004) and 24 h (p = 0,0430). Significant difference also was observed between concentration of 1 (p = 0,0026) and 2 mM (p = 0,0049) KIC in 12 h and 1 mM (p = 0,0078), 2 mM(p = 0,0421), 5 mM (p = 0,0191) and 10 mM (p = 0,0430) KIC for 24 h compared with control groups. Moreover, when compared the same concentration in different hours, is possible to observe that cell ability to reduce MTT was reduced in cells treated with 2 mM KIC for 12 hours compared with 6 hours (p = 0,0469).
To investigate whether KIC-induced reduction in the cells’ metabolic activity was associated with the RS production, we assessed RS production in the HT-22 cells exposed to KIC (1,2,5 and 10 mM) for 6, 12, and 24 h (Fig. 2c) or 1 h (Fig. 2d). The results indicated a significant effect for KIC treatment on RS after 1 h in 10 mM (p = 0.0165) (Fig. 2d) compared with control. Moreover, our results demonstrated that KIC increased the RS formation in cells incubated for 12 hours with 2 mM (p = < 0.0001), as well as in cells incubated 24 hours with KIC 2 mM (p = 0.0164) and 10 mM (p = 0.0064) compared with control.
Interestingly, we observed that in 6 hours, 5 mM (p = 0.0010) of KIC caused increased RS production in cells compared with 1 mM. In 12 hours, the cells exposed to the concentrations of 2 mM (p < 0.0001), 5 mM (p = 0.0433) presented increased RS formation compared with those treated with KIC 1 mM. Also, cells incubated with 2 mM for 12 hours exhibited a higher RS content than the same concentration in 6 hours (p = 0.0002).
Regarding 24 hours of exposure, 1 mM of KIC increased the RS production compared with the same concentration in 12 hours (p = 0.0214), and 6 hours (p = 0.0003). Finally, KIC 10 mM for 24 hours increased RS formation compared with 5 mM (p = 0.0017) at the same time, as well as was higher than the same concentration for 12 hours (p = 0.0290) and 6 hours (p = 0.0003) (Fig. 2c).
Discussion
MSUD is a disease of autosomal recessive inheritance. The MSUD is characterized by a metabolism disorder due to deficiency in the BCKAD complex activity (Chuang and Shih 2001). BCKAD complex initiates oxidative decarboxylation of α-ketoacids. Thus, this deficiency leads to accumulation in BCAA and its α-ketoacids in the blood and tissues. Moreover, MSUD patients present severe neurological damage, which may appear in the first week of life. However, the mechanisms that BCAA and its α-ketoacids lead to neuronal damage are still unclear. Importantly, neuronal dysfunction in this neurometabolic disorder has been connected to impairments in mitochondrial metabolism and coexistent oxidative stress, as well as with learning and memory deficits (De Castro Vasques et al. 2004; Taschetto et al. 2017). Additionally, it has been demonstrated that KIC and Leucine are the major toxic metabolites associated with MSUD (Snyderman et al. 1964; Chuang and Shih 2001). In this regard, herein, we investigated the impact of KIC in the mitochondrial function, using in vivo and in vitro experimental models. Moreover, we chose to study the hippocampus, once this cerebral area is more associated with behavior (Izquierdo and Medina 1997) as well as memory formation (Voss et al. 2017).
De Castro Vasques and colleagues (2004) were the first to study brain KIC administration’s effect on rats. These authors demonstrated that intrahippocampal administration of KIC resulted in learning deficits 24 hours after administration (i.e., an acute effect) (De Castro Vasques et al. 2004). Also, ICV administration of KIC induced impaired habituation memory and long-term memory impairment decline, 15 days after administration (long-term effect) (Taschetto et al. 2017). Together, these findings demonstrate that KIC toxicity is associated with behavioral changes and impaired memory.
Thus, more research is needed to point out the underlying mechanisms responsible for the neurological disorders induced by KIC. One crucial question is which mechanisms are involved in the behavioral alterations induced by KIC. In this regard, dysregulation of the neurotrophin levels leads to behavioral changes once are critical molecules related to learning and memory formation (Miranda et al. 2019). In this regard, acute ICV administration of KIC caused a decrease in the BDNF levels in the hippocampus, striatum, and cerebral cortex and a reduction in the NGF levels in the hippocampus of rats (Wisniewski et al. 2016).
Additionally, previous experimental studies have shown that BCKA, especially KIC, caused mitochondrial dysfunction (Howell and Lee 1963; Halestrap et al. 1974; Ribeiro et al. 2008; Amaral et al. 2010). KIC caused mitochondrial bioenergetic dysfunction (Amaral et al. 2010), impairment of energy production (Howell and Lee 1963), inhibition of mitochondrial pyruvate transports (Halestrap et al. 1974), and ultimately, oxidative stress (Funchal et al. 2006; Taschetto et al. 2017) in the brains of rats. In fact, neurons strongly depend on mitochondrial function for normal functionality (Kann and Kovács 2007). Herein, we observed a decrease in complex I activity in the hippocampus of young rats. In line with this, Sgaravatti and collaborators (Sgaravatti et al. 2003), demonstrated in vitro in the cerebral cortex homogenates treated with 1 mM KIC, reduction in complex I activity. Another important point is that Sgaravatti and collaborators (Sgaravatti et al. 2003) did not observe alterations in the other respiratory complexes activities in the brain homogenates exposed to KIC. By contrast, our results showed an impact of KIC exposure also in the complex II-III activities in rat’s hippocampus. Some active mechanisms in vivo can explain this phenomenon. Moreover, we are the first do demonstrate the effect of KIC on mitochondrial activity in vivo in the hippocampus.
The mitochondria are essential for the energetic stability of some cells. Moreover, mitochondria are the largest RS generators, mainly complex I (Zorov et al. 2014). Actually, mitochondrial complexes have many redox centers that allow the leakage of electrons for the oxygen. This electrons leak leads to RS’s formation in most tissues, including the brain (Halliwell 2001; Turrens 2003; Stefanatos and Sanz 2018). Therefore, mitochondrial dysfunction, particularly impairment in the mitochondrial complexes’ capacity, is related to energy defects and oxidative stress. In this study, we demonstrated that the ICV administration of KIC caused increased production of RS in the hippocampus. In this sense, previous studies demonstrated that the accumulation of KIC is associated with lipid peroxidation in the hippocampus, striatum, and cerebral cortex (Bridi et al. 2005; Taschetto et al. 2017), as well as protein carbonylation and DNA damage in the hippocampus (Taschetto et al. 2017). It is well known that RS triggers damage to macromolecules, such as membrane lipids, proteins, and DNA, and consequently, loss of cell function and death (Halliwell 2001).
Next, in order to evaluate the direct impact of KIC exposure in the hippocampal cells, we treated HT-22 cell (i.e., mouse hippocampal neuronal cells) with different concentrations of KIC (1, 2, 5, and 10 mM) in different times (6, 12 and 24 hours) and we performed MTT assay and intracellular RS formation measured. The MTT assay demonstrates the mitochondrial metabolic rate by the capacity of mitochondrial dehydrogenases, primarily succinate dehydrogenase that to reduce the MTT to formazan, which indirectly displays cell viability (Rai et al. 2018).
Our results showed that the cells treated with KIC exhibited a decrease in the ability to reduce MTT. This find demonstrates that mitochondrial metabolic activity is impaired. Interestingly, KIC caused a maximum effect in MTT reduction by about 20 to 25% in most concentrations in 12 and 24 hours of incubation. In this regard, corroborating our results, a previous study has shown that KIC led to a decrease in MTT reduction by about 23–26% with 10 mM in C6 cells (rat glioma), N1E-115 cells (mouse neuroblastoma/rat glioma hybrid), and B104 cells (rat neuroblastoma) for 20 hours (Jouvet et al. 2000).
After, we evaluated whether the decrease in mitochondrial metabolic activity was associated with an increase in RS production. Our results demonstrated that KIC induced an increase in RS generation in the hippocampal neurons.
Previously experimental studies have also shown that KIC incubation reduced α-ketoglutarate dehydrogenase (αKGDH) activity in brain mitochondrial preparations of young rats (Amaral et al. 2010) and pyruvate dehydrogenase (PDH) activity in the cerebral cortex homogenates (Ribeiro et al. 2008). Additionally, studies reported a reduction in the ADP/O ratio (Amaral et al. 2010), decreased CO2 production, and increased glucose uptake (Ribeiro et al. 2008), demonstrating inhibition of the Krebs cycle or the mitochondrial respiratory chain as well as increase of anaerobic metabolism. Moreover, another critical point is that KIC stimulated the lactate release in cerebral cortex homogenates (Sgaravatti et al. 2008), which also is found in proton spectroscopy in patients during metabolic crises (Jan et al. 2003). Together these studies corroborate with our finds either in vivo and in vitro, pointing that mitochondrial dysfunction could be associated with KIC toxicity and, consequently, the behavioral changes in rats that received ICV administration of KIC (Taschetto et al. 2017).
In conclusion, our results demonstrated, for the first time, the in vivo impact of KIC in the mitochondrial complexes activity in the hippocampus of young rats. The impaired mitochondrial complexes caused an elevation in intracellular RS formation. The in vitro studies’ findings reinforced the neuronal mitochondrial dysfunction in the hippocampus and increased RS production induced by KIC.
References
Amaral AU, Leipnitz G, Fernandes CG, Seminotti B, Schuck PF, Wajner M (2010) Alpha-ketoisocaproic acid and leucine provoke mitochondrial bioenergetic dysfunction in rat brain. Brain Res 1324:75–84
Bridi R, Braun CA, Zorzi GK, Wannmacher CM, Wajner M, Lissi EG, Dutra-Filho CS (2005) Alpha-keto acids accumulating in maple syrup urine disease stimulate lipid peroxidation and reduce antioxidant defences in cerebral cortex from young rats. Metab Brain Dis 20:155–167
Cassina A, Radi R (1996) Differential inhibitory action of nitric oxide and peroxynitrite on mitochondrial electron transport. Arch Biochem Biophys 328:309–316
Chuang DT, Shih VE (2001) Maple syrup urine disease (branched-chain ketoaciduria). In: Scriver CR, Beaudet AL, Sly WL, Valle D (eds) The metabolic and molecular bases of inherited disease, 8th edn. McGraw-Hill, New York, pp 1971–2005
de Castro Vasques V, de Boer MA, Diligenti F, Brinco F, Mallmann F, Mello CF, Wajner M (2004) Intrahippocampal administration of the alpha-keto acids accumulating in maple syrup urine disease provokes learning deficits in rats. Pharmacol Biochem Behav 77:183–190
Fischer JC, Ruitenbeek W, Berden JA, Trijbels JM, Veerkamp JH, Stadhouders AM, Sengers RC, Janssen AJ (1985) Differential investigation of the capacity of succinate oxidation in human skeletal muscle. Clin Chim Acta 153:23–36
Funchal C, Latini A, Jacques-Silva MC, Dos Santos AQ, Buzin L, Gottfried C, Wajner M, Pessoa-Pureur R (2006) Morphological alterations and induction of oxidative stress in glial cells caused by the branched-chain alpha-keto acids accumulating in maple syrup urine disease. Neurochem Int 49:640–650
Halestrap AP, Brand MD, Denton RM (1974) Inhibition of mitochondrial pyruvate transport by phenylpyruvate and alpha-ketoisocaproate. Biochim Biophys Acta 367:102–108
Halliwell B (2001) Role of free radicals in the neurodegenerative diseases: therapeutic implications for antioxidant treatment. Drugs Aging 18:685–716
Howell RK, Lee M (1963) Influence of alpha-ketoacids on the respiration of brain in vitro. Proc Soc Exp Biol Med 113:660–663
Izquierdo I, Medina JH (1997) Memory formation: the sequence of biochemical events in the hippocampus and its connection to activity in other brain structures. Neurobiol Learn Mem 68:285–316
Jan W, Zimmerman RA, Wang ZJ, Berry GT, Kaplan PB, Kaye EM (2003) MR diffusion imaging and MR spectroscopy of maple syrup urine disease during acute metabolic decompensation. Neuroradiology 45:393–399
Jouvet P, Kozma M, Mehmet H. (2000). Primary human fibroblasts from a maple syrup urine disease patient undergo apoptosis following exposure to physiological concentrations of branched chain amino acids. Ann N Y Acad Sci. 926:116–21
Kann O, Kovács R (2007) Mitochondria and Neuronal Activity. Am J Physiol Cell Physiol 292:C641–C657
Lebel CP, Ali SF, McKee M, Bondy SC (1990) Organometal-induced increases in oxygen reactive species: The potential of 2’,7’- dichlorofluorescin diacetate as an index of neurotoxic damage. Toxicol Appl Pharmacol 104:17–24
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Mescka C, Moraes T, Rosa A, Mazzola P, Piccoli B, Jacques C, Dalazen G, Coelho J, Cortes M, Terra M, Regla Vargas C, Dutra-Filho CS (2011) In vivo neuroprotective effect of L-carnitine against oxidative stress in maple syrup urine disease. Metab Brain Dis 26:21–28
Miranda M, Morici JF, Zanoni MB, Bekinschtein P (2019) Brain-Derived Neurotrophic Factor: A Key Molecule for Memory in the Healthy and the Pathological Brain. Front Cell Neurosci 13:363
Paxinos G, Watson C (2007) The Rat Brain in Stereotaxic Coordinates. Academic Press, Cambridge
Rai Y, Pathak R, Kumari N, Sah DK, Pandey S, Kalra N, Soni R, Dwarakanath BS, Bhatt AN (2018) Mitochondrial biogenesis and metabolic hyperactivation limits the application of MTT assay in the estimation of radiation induced growth inhibition. Sci Rep 8:1531
Ribeiro CA, Sgaravatti AM, Rosa RB, Schuck PF, Grando V, Schmidt AL, Ferreira GC, Perry ML, Dutra-Filho CS, Wajner M (2008) Inhibition of brain energy metabolism by the branched-chain amino acids accumulating in maple syrup urine disease. Neurochem Res 33:114–124
Rustin P, Chretien D, Bourgeron T, Gérard B, Rötig A, Saudubray JM, Munnich A (1994) Biochemical and molecular investigations in respiratory chain deficiencies. Clin Chim Acta 228:35–51
Scaini G, Tonon T, de Souza C, Schuk PF, Ferreira GC, Neto JS, Amorin T, Schwartz I, Streck EL (2017) Serum Markers of Neurodegeneration in Maple Syrup Urine Disease. Mol Neurobiol 54:5709–5719
Sgaravatti AM, Rosa RB, Schuck PF, Ribeiro CA, Wannmacher CM, Wyse AT, Dutra-Filho CS, Wajner M (2003) Inhibition of brain energy metabolism by the alpha-keto acids accumulating in maple syrup urine disease. Biochim Biophys Acta 1639:232–238
Sitta A, Ribas GS, Mescka CP, Barschak AG, Wajner M, Vargas CR (2014) Neurological damage in MSUD: the role of oxidative stress. Cell Mol Neurobiol 34:157–165
Snyderman SE, Norton PM, Roitman E, Holt LE (1964) Maple syrup urine disease with particular reference to diet therapy. Pediatrics 34:454–472
Stefanatos R, Sanz A (2018) The role of mitochondrial ROS in the aging brain. FEBS Lett 592:743–758
Strauss KA, Morton DH (2003) Branched-chain ketoacyl dehydrogenase deficiency: maple syrup urine disease. Curr Treat Options Neurol 5:329–341
Taschetto L, Scaini G, Zapelini HG, Ramos ÂC, Strapazzon G, Andrade VM, Réus GZ, Michels M, Dal-Pizzol F, Quevedo J, Schuck PF, Ferreira GC, Streck EL (2017) Acute and long-term effects of intracerebroventricular administration of α-ketoisocaproic acid on oxidative stress parameters and cognitive and noncognitive behaviors. Metab Brain Dis 32:1507–1518
Turrens JF (2003) Mitochondrial formation of reactive oxygen species. J Physiol 552:335–344
Voss JL, Bridge DJ, Cohen NJ, Walker JA (2017) A Closer Look at the Hippocampus and Memory. Trends Cogn Sci 21:577–588
Wisniewski MS, Carvalho-Silva M, Gomes LM, Zapelini HG, Schuck PF, Ferreira GC, Scaini G, Streck EL (2016) Intracerebroventricular administration of α-ketoisocaproic acid decreases brain-derived neurotrophic factor and nerve growth factor levels in brain of young rats. Metab Brain Dis 31:377–383
Zorov DB, Juhaszova M, Sollott SJ (2014) Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiological reviews 94:909–950
Acknowledgements
The authors would like to thank Prof. Marcelo Farina for donate HT-22 cells. This research was supported by grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação De Aperfeiçoamento De Pessoal De Nível Superior (CAPES), Universidade do Extremo Sul Catarinense (UNESC), and Fundação de Amparo à Pesquisa e Inovação do Estado de Santa Catarina (FAPESC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have reviewed the contents of the manuscript, have a approved of its contents and validated the accuracy of the data and they have no financial or personal conflicts of interest related to this work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Farias, H.R., Gabriel, J.R., Cecconi, M.L. et al. The metabolic effect of α-ketoisocaproic acid: in vivo and in vitro studies. Metab Brain Dis 36, 185–192 (2021). https://doi.org/10.1007/s11011-020-00626-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-020-00626-y