Abstract
Glutamine synthetase (GS) is highly active in astrocytes, and these cells are physiologically and morphologically compromised by hyperammonemia. Hyperammonemia in end-stage acute liver failure (ALF) is often associated with cerebral edema and astrocyte pathology/swelling. Many studies of animal models of hyperammonemia, and, more recently, nuclear magnetic resonance studies of liver disease patients, have shown that cerebral glutamine is elevated in hyperammonemia, contributing to the edema and encephalopathy. The GS inhibitor L-methionine-S,R-sulfoximine (MSO) is protective in animal models against acute ammonia intoxication. MSO is also an inhibitor of glutamate cysteine ligase, is converted to metabolic products, and causes convulsions at high doses. However, the susceptibility to MSO-induced convulsions is species dependent, with primates being relatively resistant. Moreover, it is possible to chronically maintain cerebral GS activity in mice at low levels by MSO treatment without any obvious untoward effects. Furthermore, MSO is protective in a mouse model of ALF. Extreme caution would be needed in administering MSO to patients. Nevertheless, inhibition of brain GS by MSO (or other GS inhibitors) may have therapeutic benefit in ALF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperammonemia is a major contributor to the neuropathology associated with both chronic and acute liver failure (ALF). The glutamine synthetase (GS) reaction (Eq. 1) is the major route for removing cerebral ammonia.Footnote 1 Although the exact mechanism is debated there is considerable evidence obtained from experimental animal models of ALF that excess ammonia leads to increased cerebral glutamine, which is a major factor contributing to excess water content and increased intracranial pressure (e.g. Desjardins et al. 2012). Therefore, we have suggested that a selective inhibitor of GS, such as L-methionine-S,R-sulfoximine (MSO),Footnote 2 may have beneficial effects in ALF by lowering brain glutamine and correcting water balance (Brusilow et al. 2010).
The GS-catalyzed reaction proceeds through a tetrahedral phosphate intermediate (Fig. 1a). MSO binds in the active site as a glutamine mimic and is phosphorylated on the imine N. The phosphorylated compound acts as a stable tight binding intermediate (Fig. 1b) (Meister 1980).
The glutamine synthetase reaction (GS) and its inhibition by the L,S-isomer of MSO. a Reaction mechanism. Phosphorylation of the γ-carboxyl group results in the formation of a γ-glutamyl phosphate intermediate, presumably via a transition state intermediate with tetrahedral geometry at the γ carbon [RC(OH)2PO 2-3 ]. b Interaction of MSO at the active site. Phosphorylation of the imine nitrogen results in a phosphorylated intermediate (MSO phosphate) with tetrahedral geometry at the sulfur [RS(O)(CH3) = NPO 2-3 ] that mimics the natural substrate tetrahedral intermediate. MSO phosphate is stable and binds tightly at the active site (Meister 1980)
Importance of the liver for ammonia homeostasis
Ammonia is generated throughout the body, including the brain, via many reactions (Cooper and Plum 1987). In the liver, ammonia is incorporated into urea and excreted. However, extrahepatic tissues do not contain a complete urea cycle and largely rely on GS to remove ammonia (e.g. Chatauret et al. 2006). Glutamine released from extrahepatic tissues, including the brain, is taken up by the periportal cells of the liver where it is hydrolyzed to glutamate and ammonia. This ammonia serves as a precursor of urea. Perivenous cells are highly enriched in GS. Effectively, the periportal cells remove glutamine and perivenous cells release glutamine. The liver thus acts as a rheostat for homeostatic control of circulating glutamine and ammonia (Brosnan and Brosnan 2009).
Disruption of ammonia homeostasis in liver disease
Damage to the liver compromises the glutamine rheostat. As a result, blood ammonia and glutamine levels rise substantially. Normal ammonia concentrations in human plasma/blood are <40 μM (slightly higher in rodents). However, during hyperammonemia as a result of liver disease, defects of the urea cycle or some other inborn errors of metabolism, blood ammonia levels may rise substantially. Although blood ammonia levels may fluctuate widely, the degree of hepatic encephalopathy (HE) in liver disease patients correlates approximately with blood ammonia, averaging about 200 μM in patients with grade 4 HE (Ong et al. 2003). But how does blood ammonia correlate with brain ammonia? This is an important question because many investigators subject brain slices or neural cells in culture to 5 mM ammonium to simulate hyperammonemic brain.
In order to obtain reliable estimates of the concentrations of ammonia and other rapidly turning over cerebral metabolites, quenching of metabolic processes must be extremely rapid. Decapitating a mouse and allowing the severed head to fall into liquid nitrogen or even immersing the whole mouse in liquid nitrogen will not freeze the brain rapidly enough to prevent ischemia/hypoxia-induced changes of compounds that are metabolically labile (Pontén et al. 1973). To overcome this problem Pontén et al. (1973 and references cited therein) introduced a method in which the cortex of an anesthetized, paralyzed and ventilated rat is frozen in situ. A second technique to rapidly arrest cerebral metabolism is “freeze blowing” in which the forebrain of an immobilized rat is rapidly extruded through a hollow needle and frozen against a block of aluminum precooled to the temperature of liquid nitrogen (Veech et al. 1973). A third technique is focused microwave irradiation.
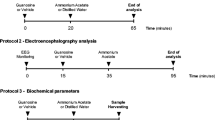
It is not possible to obtain human post mortem brain tissue rapidly enough to prevent perturbed ammonia metabolism. Therefore, we have relied on ammonia measurements in rapidly frozen rat brain as a surrogate for human brain ammonia (Table 1). In our hands, the normal concentration of rat brain ammonia is ~0.18 mM, rising to ~0.27 mM in portacaval shunted (PCS) rats (a model of chronic liver disease) and ~0.42 mM in urease-treated rats (a model of acute hyperammonemia). When rats were pretreated with MSO brain ammonia levels increased to ~0.82 mM. Ammonium acetate infusion resulted in brain ammonia close to 1 mM. Brain ammonia exceeded 1 mM only when MSO-treated rats were infused with ammonium acetate.
Our data for cerebral concentrations of ammonia in normal and hyperammonemic rat brain agree well with data obtained with microwaved rodent brain (Hawkins et al. 1993; Mans et al. 1994). In an earlier paper, Mans et al. (1979) used the brain blowing technique to measure brain ammonia in normal rats, PCS rats, and rats subjected to PCS plus hepatic artery ligation. The reported values were 0.36 ± 0.04, 0.52 ± 0.04 and 3.90 ± 0.44 μmol/g wet weight. However, the normal brain ammonia concentration reported in this study is higher than that reported later using the microwave focusing technique of 0.166 ± 0.006 (Hawkins et al. 1993) and 0.222 ± 0.048 μmol/g wet weight (Mans et al. 1994). In summary, normal values of rat brain ammonia are ~0.18 mM (corrected for 80 % water content). Values over 2 mM, often used in in vitro experiments, may therefore be supra physiological.
Importance of GS in the cerebral metabolism of ammonia in normal and hyperammonemic brain
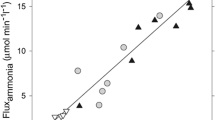
Work from our laboratory using 13N (positron-emitter; t1/2 9.96 min) as a tracer has shown for rat brain: 1) ammonia metabolism is very rapid (seconds); 2) the overwhelming route (~95 %) for the metabolism of blood-derived and cerebrospinal fluid (CSF)-derived ammonia under normal conditions is GS-catalyzed incorporation into the amide group of glutamine; 3) the GS reaction is also the major route for removal of ammonia in PCS rats and urease-treated rats; 4) in MSO-treated rats, in which the brain GS reaction is inhibited by ~85 %, the incorporation of blood-derived [13N]ammonia into glutamine is greatly curtailed; and 5) in MSO-treated rats there is no additional mechanism to effectively remove ammonia, and brain ammonia rises and glutamine falls (Cooper et al. 1979, 1983, 1985) (Fig. 2).
Compartmentation of ammonia metabolism in the rat brain. Ammonia entering the brain by diffusion from either the blood or CSF is rapidly metabolized in astrocytes predominately to glutamine. Ammonia generated endogenously in both the neuronal and astrocytic compartments is also rapidly incorporated into glutamine in astrocytes. For convenience the protonated form of ammonia (ammonium, NH +4 ) is not shown in the brain compartments. The thickness of the arrows indicates the relative contribution of the GS reaction [NH3→glutamine Gln)] and glutamate dehydrogenase (GDH) reaction [NH3→glutamate (Glu)] to the metabolism of endogenously produced ammonia and blood/CSF-derived ammonia. a Compartmentation under normal conditions. The GDH reaction plays a minor role in metabolizing brain ammonia. In the neurons the GDH reaction is a mechanism for net oxidative deamination of glutamate and is therefore not shown as a source for removing ammonia. b Loss of compartmentation in MSO-treated rats. When the rats are pretreated with MSO such that brain GS is inhibited by ~85 % conversion of ammonia to glutamine continues at a diminished rate. As a result, brain ammonia levels increase and glutamine levels decrease. Ammonia can now equilibrate among the different compartments and some ammonia can be incorporated into glutamate in the neuronal compartment. However, the GDH reaction cannot quantitatively replace the GS reaction and there is little net change in brain glutamate. CSF cerebrospinal fluid; BBB blood-brain barrier
In the brain, GS is located primarily in astrocytes (Norenberg and Martinez-Hernandez 1979) – an important feature of the cerebral glutamine cycle. In this cycle, glutamate released during neurotransmission is taken up largely by astrocytes and converted therein to glutamine. In turn, glutamine is released to the extracellular space to be taken up by neurons. In the neurons, glutaminase converts glutamine to glutamate and ammonia, thereby completing the cycle. Flux through the glutamine cycle appears to be about 25 % that of the TCA cycle in normal rat brain (Sibson et al. 2001). Nuclear magnetic resonance spectroscopy studies indicate that the GS rate in normoammonemic rat brain is ~0.18 – 0.2 μmol/min/g rising to ~0.3 – 0.4 μmol/min/g in hyperammonemia (Sibson et al. 2001; Duarte et al. 2011; reviewed by Cooper 2012). These results show that the rat brain has the capacity to increase flux into glutamine during hyperammonemia despite the fact that the level of brain GS may be decreased slightly as a result of hyperammonemia (Cooper et al. 1985; Desjardins et al. 2012). This finding is consistent with the K m reported by Pamiljans et al. (1962) of 0.18 mM for ovine brain GS and a likely concentration of ammonia in astrocytes of <0.18 mM. Moreover, using positron emission tomography and [13N]ammonia, Keiding et al. (2006) reported net metabolic fluxes of ammonia from blood to brain (and presumably trapping of most of the label as intracellular glutamine) in the cerebral cortex of healthy controls, patients with liver cirrhosis without HE, and liver cirrhosis patients with HE of 2.6, 7.4 and 13.4 μmol/min/L tissue, respectively. This finding is additional evidence that brain GS is not normally saturated with ammonia.
MSO is beneficial in animal models of hyperammonemia
Warren and Schenker (1964) showed that prior administration of MSO protected mice against a lethal dose of ammonia. This finding has been confirmed in many subsequent animal studies (reviewed in Brusilow et al. 2010). Table 2 lists several protective effects afforded by MSO against neuropathological changes in acutely hyperammonemic rats. Because astrocytic GS is not normally saturated with ammonia, hyperammonemia results in increased glutamine synthesis. Eventually, this increased synthesis (perhaps together with an ammonia-induced decrease in glutamine transport (Desjardins et al. 2012)) results in pathological accumulation of glutamine in astrocytes (Brusilow et al. 2010). As noted in the introduction, this increased glutamine is often associated with increased water content in the brains of experimental hyperammonemic animals with ALF, a finding that has been confirmed in patients with ALF by nuclear magnetic resonance techniques (Chavarria et al. 2011). Thus, a GS inhibitor, such as MSO, may be neuroprotective against hyperammonemia in human ALF.
Prior exposure of human subjects to MSO
Early last century it was noted that many hunting dogs in the southern US and in the UK were prone to running fits. Eventually it was realized that the fits were due to ingestion of biscuits made with agenized flour (i.e. flour bleached with NCl3) (Mellanby 1946). The toxic principal was later identified as MSO resulting from the modification of methionine protein residues in the agenized flour. MSO is released to the circulation following proteolytic digestion of the agenized flour (Bentley et al. 1951). Shortly thereafter it was recognized that MSO is a potent in vitro and in vivo inhibitor of GS (Pace and McDermott 1952; Sellinger and Weliler 1963 and references cited therein).
Because flour used for human consumption had been bleached with NCl3 for many years a sizable population of the human population in the US and UK had unwittingly been exposed to chronically low levels of MSO for decades as a result of ingestion of agenized flour. Bleaching of flour by NCl3 was banned in the US and UK by late 1948, but there was considerable concern at the time that neurological damage may have occurred in a considerable portion of the US and UK populations as a result of long-term ingestion of agenized flour. Fortunately, this appears not to have been the case, and it is probable that MSO is much less toxic to primates, including humans, than to dogs. Thus, no untoward effects were noted in adult humans and children given food containing agenized flour (Pollock 1949; Newell et al. 1949). In the study of Pollack (1949) one adult female and two adult male epileptic volunteers were fed half their body weight in agenized flour baked into bread and cookies, fortified with minerals and vitamins for a period of 2 to 3 months. No seizure activity was noted. On the other hand, dogs fed a similar diet showed severe signs of neurotoxicity within 18 hours. In this same study, cats and monkeys were much more resistant than dogs to the toxic effects of agenized flour. Gershoff and Elvehjem (1951) investigated the toxicity of MSO (D,L-methionine-S,R-sulfoximine mixture) to various mammalian species. These authors reported that 3 of 4 puppies given this mixture of MSO isomers (3 mg/kg) exhibited convulsions and three died. On the other hand, there was no observable effect on monkeys treated intraperitoneally with MSO (100 mg/kg).
A study has been published in which MSO (D,L-methionine-S,R-sulfoximine mixture) was administered orally to seven terminally ill cancer patients as a possible anti-cancer agent. [In this study there is no mention of its purity or from where the MSO was obtained.] Disappointingly, there was no evidence of tumor regression in any of the patients. However, there were no changes in hepatic or renal function, or in hematological status. Krakoff (1961) noted that a dose of 200 – 400 mg daily produced toxic psychoses in 3–5 days in four patients, but smaller doses could be administered for much longer periods without evidence of neurotoxic effects.
Conclusion – MSO treatment in ALF patients?
Based on the above discussion, one possible GS inhibitor for treatment of ALF patients is MSO. However, certain possible problems concerning use of MSO in patients must be considered. MSO is a substrate of at least three enzymes. For example, MSO is a substrate of glutamine transaminases, cystathionine γ-lyase, and L-amino acid oxidase, yielding a) the corresponding α-keto acid, b) α-ketobutyrate and methane sulfinamide, and c) vinylglyxoylate and methane sulfinamide, respectively (Cooper et al. 1976). Some of these metabolites may be toxic. Moreover, in addition to GS, MSO is an inhibitor of glutamate cysteine ligase (important in glutathione synthesis) (Griffith and Meister 1978,1979). Finally, as noted above, MSO is a convulsant in experimental animals.
The mechanism by which MSO acts as a convulsant has been the subject of lively debate. Convulsive doses of MSO have been shown to increase brain glycogen and possibly interfere with cerebral metabolism (Folbergrová et al. 1969). Sellinger and colleagues have suggested that due to the similarity of MSO to methionine, MSO acts as a convulsant by interfering with the normal functions of methionine in the brain, most notably as a source of methyl groups and as a building block in protein synthesis (Sellinger et al. 1986 and references cited therein). On the other hand, Meister and colleagues have strongly argued that the convulsant activity of MSO is mainly due to its inhibition of GS. α-Ethyl MSO was shown to be a strong inhibitor of GS but not of glutamate cysteine ligase (Griffith and Meister, 1978), whereas buthionine sulfoximine (BSO, an MSO analogue in which the terminal methyl group is replaced with a butyl group) was shown to be a strong inhibitor of glutamate cysteine ligase, but not of GS (Griffith and Meister 1979). Interestingly, α-ethyl MSO, but not BSO, was shown to produce convulsions in rats. Moreover, unlike MSO, α-ethyl MSO cannot be a substrate of transaminases, cystathionine γ-lyase or L-amino acid oxidase (all require an intact α C-H bond). The data of Griffith and Meister (1978,1979) are fully consistent with the hypothesis that the convulsant activity of MSO is associated with its ability to inhibit GS. However, based on the findings of Blin et al. (2002), discussed in the next paragraph, convulsions will occur after administration of MSO only when the brain GS activity is decreased beyond a threshold value, most likely by >85 %.
As noted above, the susceptibility to MSO-induced convulsions is species dependent. Dogs are especially sensitive whereas primates are relatively resistant (Brusilow et al. 2010 and references cited therein). Moreover, 4-week old mice treated with a sub-convulsive dose of MSO thrice weekly for ten weeks (Blin et al. 2002) and monkeys acutely treated with a sub-convulsive dose of MSO (Brusilow et al. 2010) exhibited no obvious untoward effects. In the study of Blin et al. (2002) the brain GS activity was decreased by about 85 % after the chronic MSO treatment. These authors stated “Thus, our data suggest that long-term administration of non-convulsive and non-glycogenic doses of MSO do not alter the spatial memory of mice. Our results do not support the hypothesis that chronic treatment with MSO influences hippocampus-dependent learning abilities in mice.” Most importantly, a recent study has shown that MSO treatment increases survival and decreases cytokine response in a mouse model of ALF (Jambekar et al. 2011).
In conclusion, it is strongly suggested that MSO (or other GS inhibitors) be considered for the treatment of ALF patients provided stringent safety concerns can be met. It is also suggested that α-ethyl MSO may be a promising alternative candidate.
Notes
Ammonia free base (NH3) has a pK a of ~9.2. Thus, under normal intracellular physiological conditions (pH 7.2 – 7.4) ammonia exists predominantly (~99 %) as the conjugate acid, ammonium (NH +4 ). For convenience, ammonia is used throughout the text to indicate the sum of NH3 plus NH +4 .
Commercially available MSO exists as a pair of diastereoisomers (L,S and L,R). The L,S diastereoisomer is a potent GS inhibitor, whereas the L,R diastereoisomer is not (Rowe and Meister 1970). In some studies, as noted in the text, a mixture of D,L-methionine-S,R-sulfoximine isomers was used.
References
Bentley HR, McDermott EE, Whitehead JK (1951) Action of nitrogen trichloride on certain proteins. II. Synthesis of methionine sulphoximine and other sulphoximines. Proc R Soc Lond B Biol Sci 138(891):265–272
Blin M, Crusio WE, Hévor T, Cloix J-F (2002) Chronic inhibition of glutamine synthetase is not associated with impairment of learning and memory in mice. Brain Res Bull 57:11–15
Brosnan ME, Brosnan JT (2009) Hepatic glutamate metabolism: a tale of 2 hepatocytes. Am J Clin Nutr 90:857S–861S
Brusilow SW, Koehler RC, Traystman RJ, Cooper AJL (2010) Astrocyte glutamine synthetase: importance in hyperammonemic syndromes and potential target for therapy. Neurotherapeutics 7:452–470
Chatauret N, Desjardins P, Zwingmann C, Rose C, Rao KV, Butterworth RF (2006) Direct molecular and spectroscopic evidence for increased ammonia removal capacity of skeletal muscle in acute liver failure. J Hepatol 44:1083–1088
Chavarria L, Alonso J, Rovira A, Córdoba J (2011) Neuroimaging in acute liver failure. Neurochem Int 59:1175–1180
Cooper AJL (2012) The role of glutamine synthetase and glutamate dehydrogenase in cerebral ammonia homeostasis. Neurochem Res. [Epub ahead of print]
Cooper AJL, Plum F (1987) Biochemistry and physiology of brain ammonia. Physiol Rev 67:440–519
Cooper AJL, Stephani RA, Meister A (1976) Enzymatic reactions of methionine sulfoximine. Conversion to the corresponding α-imino and α-keto acids and to α-ketobutyrate and methane sulfinimide. J Biol Chem 251:6674–6682
Cooper AJL, McDonald JM, Gelbard AS, Gledhill RF, Duffy TE (1979) The metabolic fate of 13N-labeled ammonia in rat brain. J Biol Chem 254:4982–4992
Cooper AJL, Vergara F, Duffy TE (1983) Cerebral glutamine metabolism. In: Hertz L, Kvamme E, McGeer EG, Schousboe A (eds) Glutamine, glutamate and GABA in the central nervous system. Alan R Liss, Inc, New York, pp 77–93
Cooper AJL, Mora SN, Cruz NF, Gelbard AS (1985) Cerebral ammonia metabolism in hyperammonemic rats. J Neurochem 44:1716–1723
Desjardins P, Du T, Jiang W, Peng L, Butterworth RF (2012) Pathogenesis of hepatic encephalopathy and brain edema in acute liver failure: Role of glutamine redefined. Neurochem Int 60:690–696
Duarte JMN, Lanz B, Gruetter R (2011) Compartmentalised cerebral metabolism of [1,6-13C]glucose determined by in vivo 13C NMR spectroscopy at 14.1T. Front Neuroenergetics 3:3
Folbergrová J, Passonneau JV, Lowry OH, Schulz DW (1969) Glycogen, ammonia and related metabolities in the brain during seizures evoked by methionine sulphoximine. J Neurochem 16:191–203
Gershoff SN, Elvehjem CA (1951) The relative effect of methionine sulfoximine on different animal species. J Nutr 45:451–458
Griffith OW, Meister A (1978) Differential inhibition of glutamine and γ-glutamylcysteine synthetases by α-alkyl analogs of methionine sulfoximine that induce convulsions. J Biol Chem 253:2333–2338
Griffith OW, Meister A (1979) Potent and specific inhibition of glutathione synthesis by buthionine sulfoximine (S-n-butyl homocysteine sulfoximine). J Biol Chem 254:7558–7560
Hawkins RA, Jessy J, Mans AM, De Joseph MR (1993) Effect of reducing brain glutamine synthesis on metabolic symptoms of hepatic encephalopathy. J Neurochem 60:1000–1006
Jambekar AA, Palma E, Nicolosi L, Rasola A, Petronilli V, Chiara F, Bernardi P, Needleman R, Brusilow WS (2011) A glutamine synthetase inhibitor increases survival and decreases cytokine response in a mouse model of acute liver failure. Liver Int 31:1209–1221
Keiding S, Sørensen M, Bender D, Munk OL, Ott P, Vilstrup H (2006) Brain metabolism of 13N-ammonia during acute hepatic encephalopathy in cirrhosis measured by positron emission tomography. Hepatology 43:42–50
Krakoff IH (1961) Effect of methionine sulfoximine in man. Clin Pharmacol Ther 2:599–604
Mans AM, Saunders SJ, Kirsch RE, Biebuyck JF (1979) Correlation of plasma and brain amino acid and putative neurotransmitter alterations during acute hepatic coma in the rat. J Neurochem 32:285–292
Mans AM, DeJoseph MR, Hawkins RA (1994) Metabolic abnormalities and grade of encephalopathy in acute hepatic failure. J Neurochem 63:1829–1838
Meister A (1980) Catalytic mechanism of glutamine synthetase; overview of glutamine metabolism. In: Mora J, Palacios R (eds) Glutamine metabolism, enzymology, and regulation. Academic Press, New York, pp 1–40
Mellanby E (1946) Diet and canine hysteria; experimental production by treated flour. Br Med J 2(4484):885–887
Newell GW, Erickson TC, Gilson WE, Gershoff SN, Elvehjem CA (1949) Studies on human subjects receiving highly agenized food materials. J Lab Clin Med 34:239–245
Norenberg MD, Martinez-Hernandez A (1979) Fine structural localization of glutamine synthetase in astrocytes of rat brain. Brain Res 161:303–310
Ong JP, Aggarwal A, Krieger D, Easley KA, Karafa MT, Van Lente F, Arroliga AC, Mullen KD (2003) Correlation between ammonia levels and the severity of hepatic encephalopathy. Am J Med 114:188–193
Pace J, McDermott E (1952) Methionine sulphoximine and some enzyme systems involving glutamine. Nature 169:415–416
Pamiljans V, Krishnaswamy PR, Dumville G, Meister A (1962) Studies on the mechanism of glutamine synthesis; Isolation and properties of the enzyme from sheep brain. Biochemistry 1:153–158
Pollock GH (1949) Species specificity of agene toxicity. J Appl Physiol 1:802–806
Pontén U, Ratcheson RA, Salford LG, Siesjö BK (1973) Optimal freezing conditions for cerebral metabolites in rats. J Neurochem 21:1127–1138
Rowe WB, Meister A (1970) Identification of L-methionine-S-sulfoximine as the convulsant isomer of methionine sulfoximine. Proc Natl Acad Sci U S A 66:500–506
Sellinger OZ, Weliler P Jr (1963) the nature of the inhibition in vitro of cerebral glutamine synthetase by the convulsant, methionine sulfoximine. Biochem Pharmacol 12:989–1000
Sellinger OZ, Schatz RA, Gregor P (1986) Cerebral methylations in epileptogenesis. Adv Neurol 44:465–473
Sibson NR, Mason GF, Shen J, Cline GW, Herskovits AZ, Wall JE, Behar KL, Rothman DL, Shulman RG (2001) In vivo 13C NMR measurement of neurotransmitter glutamate cycling, anaplerosis and TCA cycle flux in rat brain during [2-13C]glucose infusion. J Neurochem 76:975–989
Veech RL, Harris RL, Veloso D, Veech EH (1973) Freeze-blowing: a new technique for the study of brain in vivo. J Neurochem 20:183–188
Warren KS, Schenker S (1964) Effect of an inhibitor of glutamine synthesis (methionine sulfoximine) on ammonia toxicity and metabolism. J Lab Clin Med 64:442–449
Acknowledgments
I thank Dr. Saul Brusilow for his help and encouragement and for providing me with some pertinent references regarding the history of MSO. Dr. Brusilow has been a major proponent for the possible use of a GS inhibitor in the treatment of ALF. I also thank Dr. Boris F. Krasnikov for help in construction of the figures. Some of the author’s work mentioned in this review was supported by NIH grant DK 16739.
Conflict of interest
No potential conflict of interest relevant to this article is reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cooper, A.J.L. Possible treatment of end-stage hyperammonemic encephalopathy by inhibition of glutamine synthetase. Metab Brain Dis 28, 119–125 (2013). https://doi.org/10.1007/s11011-012-9338-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-012-9338-2