Abstract
Minimal hepatic encephalopathy (MHE) is intermittently present in up to 2/3 of patients with chronic liver disease. It impairs their daily living and can be treated. However, there is no consensus on diagnostic criteria except that psychometric methods are required. We compared two easy-to-perform reproducible bedside methods: the critical flicker frequency (CFF) and continuous reaction times (CRT) tests. A CFF <39 Hz and CRT-index <1.9 (index: the ratio 50/(90 minus 10) percentiles of reaction times) indicates cerebral dysfunction. 154 patients with acute or chronic liver disease with out overt hepatic encephalopathy (HE) underwent both tests at the same occasion. Both tests were abnormal in 20% of the patients and both tests were normal in 40% of the patients. In more than 1/3 the two tests were not in agreement as CFF classified 32% and CRT-index classified 48% of the patients as having MHE (p < 0.005). The two tests were weakly linearly correlated (r2 = 0.14, p < 0.001) and neither test correlated with the metabolic liver function measured by the Galactose Elimination Capacity (GEC), nor with the blood ammonia concentration. Both tests identified a large fraction of the patients as having MHE and cleared only 40%. The two tests did not show concordant results, likely because they describe different aspects of MHE: the CFF gives a measure of astrocytic metabolic state and hence pathogenic aspects of MHE, whereas the CRT measures a composite key performance, viz. the ability of reacting appropriately to a sensory stimulus. The choice of test depends on the information needed in the clinical and scientific care and study of the patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Minimal hepatic encephalopathy (MHE) is the designation for the cerebral dysfunction occurring in patients with liver disease without overt encephalopathy and where other causes of encephalopathy are excluded.
Up to two thirds of patients with cirrhosis may intermittingly suffer from MHE (Prasad et al. 2007). MHE profoundly disturbs the patients’ quality of life by compromising cognitive functions, social interactions, emotional behaviour, mobility and sleep (Groeneweg et al. 1998). Discrete deficits in attention, vigilance and orientation are often present along with slowing of psychomotor speed (Amodio et al. 2004; Bajaj 2008). MHE can render keeping meaningful family relations, a normal job or driving a car impossible (Ortiz et al. 2005; Schomerus and Hamster 2001). In most cases, it is possible to treat or improve the condition by means of nutrition therapy supplemented with lactulose or other pre- and probiotics or antibiotics (Prasad et al. 2007; Romero-Gomez 2010; Shukla et al. 2011)
Because MHE is frequent, debilitating and treatable, it is important to be able to diagnose it and to follow-up on treatment effects. Yet, there is no golden standard and no professional consensus on how this is done (Dhiman et al. 2010; Ferenci et al. 2002; Randolph et al. 2009). The clinical criteria are based on presence of relevant liver disease, usually cirrhosis and/or porto-systemic shunts, and absence of overt hepatic encephalopathy (HE), e.g. slow-cerebration, confusion or stupor. The positive diagnosis of MHE requires an abnormal neuro-psychological test—and several such tests have been developed (Ortiz et al. 2005). For routine use, such tests have to be easily performed by clinical staff. In our department we have used the Continuous Reaction Times (CRT) test for many years. Other institutions prefer the Critical Flicker Frequency (CFF) test.
This study describes the single-center parallel clinical use of these two conceptually different computerized tests. We expected both tests to diagnose a considerable fraction of the patients as having MHE and we also expected both tests to identify the same patients as having MHE. The aim was to perform both tests on the same occasion in an unselected group of liver patients without overt HE. The test results were related to the patients’ metabolic liver function and to their blood ammonia concentration.
Patients and methods
Patients
The study population comprised 154 patients with liver disease who underwent a CFF and CRT test on the same occasion between September 2007 and November 2010. On the same day the metabolic liver function was assessed by the galactose elimination capacity test (GEC) in 98 patients and the serum ammonia concentration measured in 36. The patients were referred to the tests by the clinical hepatologists with the purpose of identifying MHE and decide on treatment. Most patients suffered from alcoholic liver disease (Table 1). The average patient age was 55 years (range 19–87, SD 11), and 36 of them were females and 118 males. Patients with signs of overt hepatic encephalopathy were not referred. Likewise, patients with other possible causes for cerebral involvement than the liver disease, eg. severe electrolyte disturbances, use of psychoactive drugs and alcohol withdrawal, were not referred. All the tests were conducted within the department by one of two laboratory technicians between 9:00 and 14:00 in an undisturbed location.
Critical flicker frequency
In a pair of spectacles shielding against outside light the person watches a red diode light that pulses at a 1:1 ratio at a frequency of 60 Hz. At this high frequency the red light is perceived as fused. The light pulse frequency is then gradually decreased until the light is perceived as flickering or pulsating. The patient is instructed to press a handgrip button when this happens. Nine measurements are conducted and the patient’s critical flicker frequency (CFF) is the average of the measurements. Each test, including patient instruction and data collection, takes 15 to 20 min. Based on a large normal and patient material, a CFF lower than 39 Hz is taken to indicate cerebral dysfunction(Kircheis et al. 2002). CFF was measured using a HEPAtonorm analyzer (Accelab GmbH, D-72127 Kusterdingen, Germany). Nineteen patients were unable to complete the measurements due to problems focusing on the light diode or fogging of the glasses. These patients were not included in the study population.
Continuous reaction time
With the dominant hand the person holds a grip with a trigger button on top, connected via the signal generator to a laptop PC. The generator delivers 100 auditory signals at 500 Hz and 90 dB at random intervals of 2 to 6 s via a set of calibrated sound isolated headphones. The person is instructed to press the button with his thumb as soon as the signal is heard and the reaction time is registered. Reaction times above 2 s or no reaction before the next signal are registered as “no-response”. The reaction times‘ 10th, 50th and 90th percentiles and their variation, the ‘index’ are calculated (index: the ratio 50/(90 minus 10) percentiles of reaction times). Based on a large normal and patient material the index results in the best discrimination between patients with hepatic encephalopathy and other test populations, and a CRT-index <1.9 is abnormal (Elsass et al. 1981). Each test, including patient instruction and data collection takes 10 to 15 min. No patient was unable to complete the test. The equipment was an EKHO system (Bitmatic, Aarhus, Denmark) coupled to an ordinary laptop PC.
The galactose elimination capacity
Following intravenous injection of galactose, repeated arterialized capillary blood samples were secured for 1 h and urine was collected quantitatively. Samples were analyzed for galactose concentration. The galactose elimination capacity (GEC) was calculated from the slope of the linear blood galactose concentration over time decay curve, corrected for urinary loss (Tygstrup 1964).
Blood tests
Venous blood was secured in cooled, gas tight syringes for dry film enzymatic measurement of ammonia concentration. These analyses were preformed according to standard certified clinical chemistry laboratory methods.
Statistical analysis
Histograms showed that the results of the CFF, CRT, GEC and ammonia measurements could be described by the normal distribution. Correlations between test results were calculated using the Person r2. McNemar’s test was used to evaluate the level of concordance between the CFF and CRT test results. p values below 0.05 were considered statistically significant.
Results
Table 2 shows the distribution of 154 patients who underwent both tests. Both test results were abnormal in 20% (31) of the patients and both tests were normal in 40% (61). Only 62% of the patients with an abnormal CFF had an abnormal CRT, and only 42% of the patients with an abnormal CRT had an abnormal CFF.
32% (50 patients) had a CFF-mean <39 Hz, indicating MHE and 48% (74 patients) had a CRT-index <1.9, indicating MHE (Table 2). Hence, the two tests disagreed on the diagnosis in 40% of cases (p < 0.005) (Table 2).
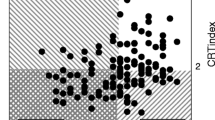
The two tests were weakly but significantly correlated (Fig. 1, r 2 = 0.14, p < 0.001). The same was the case with the subgroup of patients with verified cirrhosis (r 2 = 0.12, p = 0.001).
Relation between the Continuous Reaction Time index (CRT-index) and the Critical Flicker Frequency mean (CFF-mean) measured in 154 clinically non-encephalopathic patients with liver disease. The dotted lines indicate cut-off values (CRT-index <1.9 and CFF-mean <39 Hz). The black dots represent patients with cirrhosis of the liver (n = 85). The figure shows a weak but statically significant positive correlation between the two measures (r 2 = 0.12, p = 0.001)
There was no correlation between the galactose elimination capacity and either psychometric test (Fig. 2). This was also the case in patients with cirrhosis.
There was no correlation between the patients’ serum ammonia concentration and their CFF-mean or CRT-index.
Discussion
In accordance with our a priori expectations, both tests indicated MHE in one third to one half of the patients. However, the results of the tests were unexpectedly dissimilar. In almost half of the patients the two tests were discordant and categorized the patients differently.
Both tests were performed by skilled staff and according to the test guidelines. Our every-day use of the tests during the study confirmed that they were both easy to apply and acceptable to the patients although the CFF test resulted in more than 10% dropouts from the study. The test equipments were of the newest generation to enter clinical use. Published independent patient populations defined the cut-off values. The patients were referred to the tests by physicians well trained in recognizing overt encephalopathy and no such patient was referred.
It may seem surprising that such a high fraction of liver patients without overt HE did in fact have signs of MHE. Still, this finding is in accordance with several previous reports (Dhiman et al. 2010; Ferenci et al. 2002; Li et al. 2004; Prasad et al. 2007; Sharma and Sharma 2010). It emphasizes the need for routine psychometric screening of all liver patients. The clinical benefit of doing so is very large because MHE ruins the quality of the patients’ life (Amodio et al. 2004; Bajaj 2008; Bao et al. 2007; Groeneweg et al. 1998; Kircheis et al. 2009a, b; Schomerus and Hamster 2001) and because the problem in the large majority of cases is treatable.
It would be highly desirable to reach a consensus and a standard for how to perform such screening. This would render uniform recommendations possible and secure treatment of most patients. Furthermore, it would be possible to conduct multi-centre trials and improve the treatment of MHE on the evidence-based level. A considerable number of complex or simple methods have been suggested and presented in selected patient populations (Amodio et al. 1996; Bajaj 2008; Groeneweg et al. 2000; Kircheis et al. 2009a, b; Montagnese et al. 2004). Unfortunately, however, it has not been possible to establish a standard. This study, which compares the performances of two of the simplest machine-based tests, illustrates the difficulties.
The lack of agreement between the tests was probably not due to characteristics of the study population. Restricting the study to patients with diagnosed cirrhosis or with alcoholic vs. non-alcoholic aetiology did not improve the agreement (Fig. 1). Use of opioids and tranquilizers might disturb the CRT more than the CFF—but patients on such medication were not included(Roback et al. 1952; Sjogren et al. 2000a, b; Sjogren 2000a, b; Smith and Misiak 1976). Selection bias, i.e. due to referral pattern, should not disturb the lack of agreement between the tests. Finally, we did not identify cut-off values that improved the agreement over that obtained by the use of the original cut-offs. Likewise, replacing the CRT-index with either the patients’ slowest reaction times (the 90th percentile) or the fastest reaction times (the 10th percentile) did not improve the concordance with the CFF test results. The lack of concordance, therefore, should be ascribed to characteristics of the condition MHE, and to physiological characteristics of the tests.
MHE is a complex global neuropsychiatric brain function disturbance. There is no single manifestation that consistently pervades the clinical picture. One test therefore, cannot encompass the spectrum of deficits of the condition and hence cannot approve or dismiss all cases. Because there is no diagnostic gold standard for MHE a ‘true’ specificity and sensitivity of a test (or a battery) cannot be calculated. The diagnostic possibility is comparisons of tests, as in this study, and for interventional studies to choose those tests that measure the defined qualities of MHE that are under study.
The two tests we used here measure biologically and conceptually different aspects of MHE: the CFF test reflects biological activity in retinal cells, whereas the CRT test measures a personal performance. The CFF gives a measure of mitochondrial energy restoration capacity in the light sensitive retinal cells that are anatomically specialized astrocytes. The test, therefore, is taken to reflect astrocytic metabolic functional state (Haussinger et al. 2002) which plays a central role in prevailing hypotheses on the patho-aetiology of HE. The test gives information on visual processing, but also cognitive functions such as arousal and attention. In contrast, the CRT is a global senso-cognitive-motoric function measure of patient’s ability to deliver a motor reaction adequately and repeatedly (Jakobsen et al. 2010). The test evaluates sustained attention, cerebral processing time, including reaction time and response inhibition, and nerve conduction speed. These differences are likely responsible for the disagreement between the tests.
There was no relationship between the residual metabolic liver function as measured by the GEC and either psychometric test. This was also unexpected because the GEC predicts the emergence of overt hepatic encephalopathy and the prognosis of cirrhosis patients (Jepsen et al. 2010). This may indicate that subclinical compromised brain function and decreased liver function are dissociated manifestations of liver disease, and MHE and overt HE are differently related to the metabolic capacity of the sick liver.
In conclusion, the CFF- and the CRT- test both identified a large fraction of clinically non-encephalopatic liver patients as having MHE. The tests, however, did not show concordant results, likely because they describe different aspects of MHE. The choice of the CFF or the CRT test depends on the information needed in different settings of care and study of the patients.
References
Amodio P, Quero JC, Del Piccolo F, Gatta A, Schalm SW (1996) Diagnostic tools for the detection of subclinical hepatic encephalopathy: comparison of standard and computerized psychometric tests with spectral-eeg. Metab Brain Dis 11:315–327
Amodio P, Montagnese S, Gatta A, Morgan MY (2004) Characteristics of minimal hepatic encephalopathy. Metab Brain Dis 19:253–267
Bajaj JS (2008) Minimal hepatic encephalopathy matters in daily life. World J Gastroenterol 14:3609–3615
Bao ZJ, Qiu DK, Ma X et al (2007) Assessment of health-related quality of life in chinese patients with minimal hepatic encephalopathy. World J Gastroenterol 13:3003–3008
Dhiman RK, Saraswat VA, Sharma BK et al (2010) Minimal hepatic encephalopathy: consensus statement of a working party of the indian national association for study of the liver. J Gastroenterol Hepatol 25:1029–1041. doi:10.1111/j.1440-1746.2010.06318.x
Elsass P, Christensen SE, Ranek L, Theilgaard A, Tygstrup N (1981) Continuous reaction time in patients with hepatic encephalopathy. A quantitative measure of changes in consciousness. Scand J Gastroenterol 16:441–447
Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT (2002) Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th world congresses of gastroenterology, vienna, 1998. Hepatology 35:716–721. doi:10.1053/jhep.2002.31250
Groeneweg M, Quero JC, De Bruijn I et al (1998) Subclinical hepatic encephalopathy impairs daily functioning. Hepatology 28:45–49. doi:10.1002/hep.510280108
Groeneweg M, Moerland W, Quero JC, Hop WC, Krabbe PF, Schalm SW (2000) Screening of subclinical hepatic encephalopathy. J Hepatol 32:748–753
Haussinger D, Schliess F, Kircheis G (2002) Pathogenesis of hepatic encephalopathy. J Gastroenterol Hepatol 17(Suppl 3):S256–S259
Jakobsen LH, Sorensen JM, Rask IK, Jensen BS, Kondrup J (2010) Validation of reaction time as a measure of cognitive function and quality of life in healthy subjects and patients. Nutrition.doi:10.1016/j.nut.2010.08.003
Jepsen POP, Andersen PK, Sørensen HT, Vilstrup H (2010) The clinical course of alcoholic cirrhosis with ascites: effects of liver and kidney function, hyponatremia, and alcohol. Hepatology 52:896A
Kircheis G, Wettstein M, Timmermann L, Schnitzler A, Haussinger D (2002) Critical flicker frequency for quantification of low-grade hepatic encephalopathy. Hepatology 35:357–366. doi:10.1053/jhep.2002.30957
Kircheis G, Bode JG, Hilger N, Kramer T, Schnitzler A, Haussinger D (2009a) Diagnostic and prognostic values of critical flicker frequency determination as new diagnostic tool for objective he evaluation in patients undergoing tips implantation. Eur J Gastroenterol Hepatol 21:1383–1394. doi:10.1097/MEG.0b013e328310e0c3
Kircheis G, Knoche A, Hilger N et al (2009b) Hepatic encephalopathy and fitness to drive. Gastroenterology 137:1706–1715. doi:10.1053/j.gastro.2009.08.003
Li YY, Nie YQ, Sha WH et al (2004) Prevalence of subclinical hepatic encephalopathy in cirrhotic patients in China. World J Gastroenterol 10:2397–2401
Montagnese S, Amodio P, Morgan MY (2004) Methods for diagnosing hepatic encephalopathy in patients with cirrhosis: a multidimensional approach. Metab Brain Dis 19:281–312
Ortiz M, Jacas C, Cordoba J (2005) Minimal hepatic encephalopathy: diagnosis, clinical significance and recommendations. J Hepatol 42(Suppl):S45–S53. doi:10.1016/j.jhep.2004.11.028
Prasad S, Dhiman RK, Duseja A, Chawla YK, Sharma A, Agarwal R (2007) Lactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology 45:549–559. doi:10.1002/hep.21533
Randolph C, Hilsabeck R, Kato A et al (2009) Neuropsychological assessment of hepatic encephalopathy: ishen practice guidelines. Liver Int 29:629–635. doi:10.1111/j.1478-3231.2009.02009.x
Roback GS, Krasno LR, Ivy AC (1952) Effect of analeptic drugs on the somnifacient effect of seconal and antihistaminics as measured by the flicker fusion threshold. J Appl Physiol 4:566–574
Romero-Gomez M (2010) Pharmacotherapy of hepatic encephalopathy in cirrhosis. Expert Opin Pharmacother 11:1317–1327. doi:10.1517/14656561003724721
Schomerus H, Hamster W (2001) Quality of life in cirrhotics with minimal hepatic encephalopathy. Metab Brain Dis 16:37–41
Sharma P, Sharma BC (2010) Predictors of minimal hepatic encephalopathy in patients with cirrhosis. Saudi J Gastroenterol 16:181–187. doi:10.4103/1319-3767.65189
Shukla S, Shukla A, Mehboob S, Guha S (2011) Meta-analysis: the effects of gut flora modulation using prebiotics, probiotics and synbiotics on minimal hepatic encephalopathy. Aliment Pharmacol Ther. doi:10.1111/j.1365-2036.2010.04574.x
Sjogren P, Olsen AK, Thomsen AB, Dalberg J (2000a) Neuropsychological performance in cancer patients: the role of oral opioids, pain and performance status. Pain 86:237–245
Sjogren P, Thomsen AB, Olsen AK (2000b) Impaired neuropsychological performance in chronic nonmalignant pain patients receiving long-term oral opioid therapy. J Pain Symptom Manage 19:100–108
Smith JM, Misiak H (1976) Critical flicker frequency (cff) and psychotropic drugs in normal human subjects-a review. Psychopharmacologia 47:175–182
Tygstrup N (1964) The galactose elimination capacity in control subjects and in patients with cirrhosis of the liver. Acta Med Scand 175:281–289
Acknowledgements
The authors wish to thank laboratory technicians I. Schjødt and B. Nielsen of the Department of Medicine V Clinical and Research Laboratory and Professor Michael Vaeth of the Institute of Biostatistics, Aarhus University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lauridsen, M.M., Jepsen, P. & Vilstrup, H. Critical flicker frequency and continuous reaction times for the diagnosis of minimal hepatic encephalopathy. A comparative study of 154 patients with liver disease. Metab Brain Dis 26, 135–139 (2011). https://doi.org/10.1007/s11011-011-9242-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-011-9242-1