Abstract
Many chronic medical conditions are accompanied by cognitive disturbances but these have only to a very limited extent been psychometrically quantified. An exception is liver cirrhosis where hepatic encephalopathy is an inherent risk and mild forms are diagnosed by psychometric tests. The preferred diagnostic test battery in cirrhosis is often the Continuous Reaction Time (CRT) and the Portosystemic Encephalopathy (PSE) tests but the effect on these of other medical conditions is not known. We aimed to examine the effects of common chronic (non-cirrhosis) medical conditions on the CRT and PSE tests. We studied 15 patients with heart failure (HF), 15 with end stage renal failure (ESRF), 15 with dysregulated type II diabetes (DMII), 15 with chronic obstructive pulmonary disease (COPD), and 15 healthy persons. We applied the CRT test, which is a 10-min computerized test measuring sustained attention and reaction time stability and the PSE test, which is a paper-pencil test battery consisting of 5 subtests. We found that a high fraction of the patients with HF (8/15, 0.002) or COPD (7/15, p = 0.006) had pathological CRT test results; and COPD patients also frequently had an abnormal PSE test result (6/15, p < 0.0001). Both tests were unaffected by ESRF and DMII. Half of the patients with HF or COPD had psychometrically measurable cognitive deficits, whereas those with ESRF or DMII had not. This adds to the understanding of the clinical consequences of chronic heart- and lung disease, and implies that the psychometric tests should be interpreted with great caution in cirrhosis patients with heart- or lung comorbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many common chronic medical conditions are accompanied by cognitive disturbances but these have only to a very limited extent been quantified by means of psychometric tests. An exception is liver cirrhosis where hepatic encephalopathy (HE) is an inherent risk and mild forms are diagnosed using psychometric tests. Heart failure (HF), end stage renal failure (ESRF), type II diabetes (DMII) and chronic obstructive pulmonary disease (COPD) can all cause brain disturbances (Athilingam et al. 2013; Bugnicourt et al. 2013; Cannon et al. 2015; Geijselaers et al. 2015; Kurella Tamura et al. 2010; Leto and Feola 2014; Ravona-Springer et al. 2014; Yaffe et al. 2010) and the cognitive impairment found in these chronic medical conditions have many features similar to HE: impairment is known to vary with age and disease severity; causes are multi factorial and to a high degree unclear; inflammation and oxidative stress are central in the pathogenesis. Further, as seen in HE, a broad spectrum of nonspecific cognitive domains is often affected.
The preferred diagnostic test battery used to diagnose and quantify HE is often the Continuous Reaction Time test (CRT) and the Portosystemic Encephalopathy test (PSE). The CRT test is used routinely in Scandinavia as a screening tool for minimal hepatic encephalopathy (MHE) and the PSE is having more widespread use and often serves as an inter-study comparator (Goldbecker et al. 2013; Lauridsen et al. 2012). It has been shown that the reaction time stability measured by the CRT test is severely affected in metabolic but not organic brain disturbance and the reaction time stability is unaffected by gender, age and intelligence level (Elsass et al. 1985; Lauridsen et al. 2013). Likewise, the age corrected PSE test results are not affected by gender and education (Schomerus and Hamster 1998). Still, the effect on these tests of non-cirrhosis medical conditions is not known. This issue is important to our understanding of the cognitive consequences of chronic organ failure and because comorbid medical conditions are present in 40 % of cirrhosis patients and, via their cognitive effects, may confound the diagnosis of HE (Jepsen 2014; Jepsen et al. 2008). Apart from being able to cause brain disturbances the medical conditions we have chosen to focus on often co-exist with cirrhosis and impact mortality (Jepsen 2014; Jepsen et al. 2008). DMII is the most frequently occurring chronic medical comorbidity present in 10 % of cirrhosis patients; HF or COPD is present in approximately 5 % and have a marked additive effect on mortality rates; and severe renal disease is present in 1 % and had an even more profound impact on mortality (Jepsen 2014; Jepsen et al. 2008). Other conditions i.e., psychiatric disorders, organic brain disease, alcoholism and ulcers are also common in cirrhosis, but for the purpose of this study they are not relevant because they have an obvious effect on brain functioning or are unlikely to cause brain involvement. The aim of this study was therefore to test the effects of HF, ESRF, DMII and COPD on the two established and validated psychometric tests used in diagnosing MHE: The continuous reaction time (CRT) and the Portosystemic Encephalopathy (PSE) tests.
Patients and methods
Patients were recruited form Hospital of Southwest Jutland’s medical out patient clinics from April 2013 to March 2015. All were aged > 18 years, had no liver disease or known cerebral impairment, none used psychoactive medications on the test day; all had a stable chronic medical condition and no other significant competing comorbid diseases. Patients were ineligible if creatinine was > 150 mg/dL except in the case of ESRF. We included 4 patients groups: 15 patients with HF New York Heart Association Class (NYHA) IIA–IIIA all of whom received standard medical treatment including angiotensin converting enzyme antagonists (9/15), diuretics (9/15) and beta blockers (14/15); 15 ESRF patients immediately prior to haemodialysis with mean creatinine 819.3 mg/dL (SD 220.1, 95 % CI 697.4–941.2); 15 patients with DMII and a BMI of 34 (SD 7.1, 95 % CI 30.1–37.9), mean hemoglobin A1c 62.9 (SD 18.8, 95 % CI 52.5–73.2) of whom 4 had one or more diabetic complications, 3 were insulin treated and the rest received oral anti diabetics. Lastly, 15 patients with moderate to severe COPD with mean forced expiratory volume/ forced vital capacity (FEV1/FVC) of 41.2 (SD 12.5, 96 % CI 34.5–48.9). Three received home oxygen therapy and all were treated with standard inhalation in various combinations.
Fifteen age matched healthy persons with no chronic medical conditions or known brain impairment served as a reference group.
The cognitive functions of all patients and controls were evaluated between 9 am and 5 pm using two psychometric tests at the same occasion. Test staff was thoroughly trained prior to patient inclusion.
The continuous reaction time test (CRT)
A simple and fast, computerized test of 10 min duration which measures and combines motor reaction speed, sustained attention, and inhibitory control – all key functions of daily life (Lauridsen et al. 2013). The test is run from a normal lab top computer using dedicated software, headphones, and a handheld trigger button (EKHO, www.Bitmatic.com, Aarhus, Denmark). The patient is left alone to complete the test after a 2–min instruction. During the test the patient is presented with 150 randomly occurring, sound stimuli (beeps at 500 Hz and 90 dB at 2–6 s intervals). The patient must press the button as fast as possible in response to each beep. During the test the programme registers response times and calculates the 10, 50 and 90 percentiles and a CRTindex (the ratio: 50 percentile/ (90 minus 10 percentile)), which is a measure of intra personal reaction time stability. A CRTindex value below 1.9 is abnormal and indicates MHE.
The portosystemic encephalopathy test (PSE)
Measures attention, working speed and -accuracy, visual orientation, and visuo-spatial construction and has been shown to predict overt HE and death (Kato et al. 2004; Montagnese et al. 2011). PSE is a 15-min paper-pencil test battery comprised of 5 sub-tests: Digit Symbol test (DST), Number Connection Test A (NCT-A), Number Connection Test B (NCT-B), Serial Dotting Test (SDOT), and Line Tracing Test (LTT, time and errors). Four versions of the test battery are available to prevent learning effect at repeated testing. Staff must be present for guidance and timing during the entire test session and post-test manual calculation of the final test result – the portosystemic hepatic encephalopathy score (PHES) that is calculated within very few minutes using age-adjusted norms. The PHES is a composite score calculated from the time (seconds) spent on each sub-test converted into a score that ranges between -3 and 1. The LTT is converted into 2 scores – a time score and an error score. A score of 0 is given for a performance within +/- 1 SD. The PHES is the sum of the scores and ranges from −18 to 6. A result below -4 is abnormal and may indicate MHE. We evaluated the test using the age adjusted norm data provided in the German test manual.
Study approval
The Danish National Committee on Health Research Ethics approved the study (approval code S-20120196) and all participants gave their written informed consent.
Statistical analysis
Statistical analysis and graphing was performed using GraphPad Prism 6.0 for Mac. CRTindex is a continuous numeric outcome variable whereas the PSE test result (portosystemic hepatic encephalopathy score, PHES) is a discrete numeric variable. CRTindex and PHES did not show Gaussian distribution therefore test results between disease groups were compared using Kruskal–Wallis test with multiple comparisons and ANOVA. We used Pearson r to describe correlation between variables. Results were considered statistical significant at p ≤ 0.05. In contingency analysis Chi-square test or Fisher’s exact test was used.
Results
HF negatively affects the CRT test
The patients with HF had unstable reaction times and therefore an abnormal CRT result (CRTindex < 1.9) in 8/15 cases (p = 0.002). Mean CRTindex was 1.5 ± 0.22 vs. 2.3 ± 0.08 in the control group (p = 0.002). The PSE test was unaffected in HF patients as 14/15 achieved a normal result (p = 0.30) although mean PHES was slightly worse (−0.77 ± 0.82 vs. 1.7 ± 0.49, p = 0.01). NYHA class was not correlated to CRTindex and PHES (r = 0.05, p = 0.88 and 0.19, p = 0.57).
ESRF and DMII do not affect the CRT and PSE tests
Of the ESRF patients 12/15 had a normal CRTindex (p = 0.2). The mean CRTindex was not different from that of healthy persons (2.2 ± 0.12 vs. 2.3 ± 0.08, p = 0.65). In the PSE test 2/15 had an abnormal result (p = 0.5) but the mean PSE result was lower (1.7 ± 0.49 vs. −0.3 ± 0.76, p = 0.03). Of the DMII patients 4/10 had an abnormal CRTindex (p = 0.09) but their mean CRTindex did not differ from the control group (2.2 ± 0.21 vs. 2.3 ± 0.08, p = 0.8). PHES was also not significantly affected by diabetes as 2/15 had abnormal PHES (p = 0.5) but again mean PHES was lower (1.7 ± 0.49 vs. −0.6 ± 0.82, p = 0.02).
COPD negatively affects both the CRT and PSE tests
Among the COPD patients 7/15 and 6/15 had an abnormal CRT and PSE test, respectively (p = 0.006 and p = 0.01). Further, the mean CRTindex and PSE result was lower than in the control group: mean CRTindex 1.7 ± 0.15 vs. 2.3 ± 0.08 (p = 0.004) and mean PHES −4.6 ± 1.3 vs. 1.7 ± 0.49 (p = 0.0002). FEV1/FVC was not correlated to CRTindex or PHES (r = −0.18, p = 0.53 and r = −0.1, p = 0.71).
Discussion
Our results show that chronic medical conditions do have adverse cognitive consequences as measured psychometrically by the CRT and PSE tests. The effects were most marked for heart and lung failure and were most widespread for the CRT test. This has not previously been systematically and quantitatively examined except for in chronic liver disease. Demographics do not explain the differences between the groups as the groups we studied were comparable regarding age, gender and educational level and anyway neither age nor gender affects the outcome of either test. Hence, the cognitive defects are likely to be a consequence of the medical conditions we studied and this has implications when using the CRT and PSE test for diagnosing MHE in liver cirrhosis patients.
The diagnosis of MHE is important to establish because MHE negatively impacts quality of life, the risk of encephalopathy related hospital admission and is treatable by simple means (Groeneweg et al. 1998; Luo et al. 2011; Patidar et al. 2014). However, the MHE diagnosis can only be assigned to patients with known liver disease and no other cause for cerebral impairment (Vilstrup et al. 2014). We knew beforehand that HF and COPD could cause cognitive impairment and we have now established that this is in fact detected by two of the tests most commonly used to find MHE. Consequently, MHE cannot casually be diagnosed using the CRT and PSE test in cirrhosis patients with concomitant HF and/or COPD. This finding is both pathophysiologically plausible and in accordance with other studies.
In HF, cognitive decline is reported to occur in 30–80 %; and both organic (occult embolic infarction) and metabolic (chronic hypo-perfusion, sustained low-grade systemic inflammation) mechanisms play a role (Athilingam et al. 2013; Cannon et al. 2015). It has previously been shown that organic encephalopathy does not compromise the CRT test i.e. the reaction time stability (Elsass et al. 1985). Hence, our results point towards the metabolic component as being the cause for an abnormal CRT test in HF patients. In previous psychometric studies HF has been found to compromise primarily psychomotor speed, attention, learning memory and executive function (Leto and Feola 2014; Nordlund et al. 2015). These mental qualities are largely the qualities measured by the CRT test so our quantitative findings are well in line with the general understanding. Some of the affected domains may improve after medical treatment and examining HF patients before and after treatment onset would have been interesting (Leto and Feola 2014). An association between ejection fraction and cognitive function remains to be established and in our small study group we also did not find such an association (Huijts et al. 2013).
The cognitive impairment in COPD seems also to be of mixed organic and metabolic origin: inflammation and oxidative stress caused by hypoxia and hypercapnia and vascular insults related to smoking seem to play a role (Dal Negro et al. 2014). A correlation to the degree of hypoxemia and forced expiratory volume has also been reported although we were not able to confirm this in our data (Cleutjens et al. 2014; Dodd et al. 2010). The COPD related cognition defects manifests in a variety of ways but attention deficits are prominent and in accordance with the abnormal CRT test results we observed. COPD patients have previously been shown to have poor results in NCT-A and B tests (subtests of PSE test battery) indicative of low psychomotor speed and poor cognitive flexibility and shifting capacity (Dal Negro et al. 2014, 2015). We also found problems in relation to motor speed and accuracy in the PSE test and the most striking observation was that only two patients performed within +/−1 SD in the line tracing (time) and only one in the serial dotting tests. COPD inhalation treatments do not seem to improve cognition noteworthy but home oxygen treatment has been shown to improve NCT-A and B results (Dal Negro et al. 2015; Dodd et al. 2010). Interestingly, all 3 patients in our small study achieved normal scores in the PSE test, which includes the NCT-A and B and this could be an effect of oxygen treatment.
DMII did not significantly impact the tests we used but DMII is often associated with mild cognitive impairment especially in case of long-term poor glycemic control and the same is the case for ESRF where cognition worsens with declining eGFR (Davey et al. 2013; Ravona-Springer et al. 2014; Silverwood et al. 2014; West et al. 2014; Zammit et al. 2015). However, such defects as clinically described were not documented by our psychometric tests. A recent study examined the effect of diabetes and nephropathy on the PSE and 3 other tests for MHE and in accordance with our findings, it was concluded that the PSE test was not influenced by diabetes and low estimated glomerular filtration rate (eGFR) (Goldbecker et al. 2013). The effect of COPD or HF was not evaluated in that particular study.
In conclusion, our study provides new and useful knowledge on the clinical consequences of heart- and lung failure, and implies that psychometric tests should be interpreted with great caution in cirrhosis patients with heart- or lung comorbidity (Table 1 and Fig. 1).
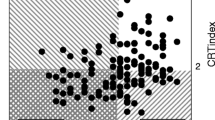
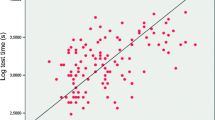
PHES and CRTindex in healthy persons and patients with common medical conditions. Patients with heart failure and COPD often have lower mean reaction time stability when compared to healthy persons; and COPD patients also a lower mean PHES. Abbreviations HF Heart failure, ESRF End stage renal failure, DM II Type II diabetes, COPD Chronic obstructive pulmonary disease, CRT Continous reaction time test (abnormal if below 1.9), PHES Portosystemic hepatic encephalopathy score (abnormal if below -4)
References
Athilingam P, Moynihan J, Chen L, D’Aoust R, Groer M, Kip K (2013) Elevated levels of interleukin 6 and C-reactive protein associated with cognitive impairment in heart failure. Congestive Heart Fail 19:92–98. doi:10.1111/chf.12007
Bugnicourt JM, Godefroy O, Chillon JM, Choukroun G, Massy ZA (2013) Cognitive disorders and dementia in CKD: the neglected kidney-brain axis. J Am Soc Nephrol : JASN 24:353–363. doi:10.1681/ASN.2012050536
Cannon JA, McMurray JJ, Quinn TJ (2015) ‘Hearts and minds’: association, causation and implication of cognitive impairment in heart failure. Alzheimers Res Ther 7:22. doi:10.1186/s13195-015-0106-5
Cleutjens FA, Janssen DJ, Ponds RW, Dijkstra JB, Wouters EF (2014) COgnitive-pulmonary disease BioMed Res Int 2014:697825 doi:10.1155/2014/697825
Dal Negro RW, Bonadiman L, Tognella S, Bricolo FP, Turco P (2014) Extent and prevalence of cognitive dysfunction in chronic obstructive pulmonary disease, chronic non-obstructive bronchitis, and in asymptomatic smokers, compared to normal reference values. Int J Chron Obstructive Pulm Dis 9:675–683. doi:10.2147/COPD.S63485
Dal Negro RW, Bonadiman L, Bricolo FP, Tognella S, Turco P (2015) Cognitive dysfunction in severe chronic obstructive pulmonary disease (COPD) with or without Long-Term Oxygen Therapy (LTOT) Multidiscip. Respir Med 10:17. doi:10.1186/s40248-015-0013-4
Davey A, Elias MF, Robbins MA, Seliger SL, Dore GA (2013) Decline in renal functioning is associated with longitudinal decline in global cognitive functioning, abstract reasoning and verbal memory. Nephrol Dial Transplant : Off Publ Eur Dialysis Transplant Assoc - Eur Renal Assoc 28:1810–1819. doi:10.1093/ndt/gfs470
Dodd JW, Getov SV, Jones PW (2010) Cognitive function in COPD. Eur Respir J 35:913–922. doi:10.1183/09031936.00125109
Elsass P, Christensen SE, Mortensen EL, Vilstrup H (1985) Discrimination between organic and hepatic encephalopathy by means of continuous reaction times. Liver 5:29–34
Geijselaers SL, Sep SJ, Stehouwer CD, Biessels GJ (2015) Glucose regulation, cognition, and brain MRI in type 2 diabetes: a systematic review. Lancet Diabetes Endocrinol 3:75–89. doi:10.1016/S2213-8587(14)70148-2
Goldbecker A et al (2013) Comparison of the most favoured methods for the diagnosis of hepatic encephalopathy in liver transplantation candidates. Gut 62:1497–1504. doi:10.1136/gutjnl-2012-303262
Groeneweg M, Quero JC, De Bruijn I, Hartmann IJ, Essink-bot ML, Hop WC, Schalm SW (1998) Subclinical hepatic encephalopathy impairs daily functioning. Hepatology 28:45–49. doi:10.1002/hep.510280108
Huijts M et al (2013) Cognitive impairment in heart failure: results from the Trial of Intensified versus standard Medical therapy in Elderly patients with Congestive Heart Failure (TIME-CHF) randomized trial. Eur J Heart Fail 15:699–707. doi:10.1093/eurjhf/hft020
Jepsen P (2014) Comorbidity in cirrhosis. World J Gastroenterol 20:7223–7230. doi:10.3748/wjg.v20.i23.7223
Jepsen P, Vilstrup H, Andersen PK, Lash TL, Sorensen HT (2008) Comorbidity and survival of Danish cirrhosis patients: a nationwide population-based cohort study. Hepatology 48:214–220. doi:10.1002/hep.22341
Kato A et al (2004) Development of quantitative neuropsychological tests for diagnosis of subclinical hepatic encephalopathy in liver cirrhosis patients and establishment of diagnostic criteria-multicenter collaborative study in Japanese. Hepatol Res : Off J Japan Soc Hepatol 30:71–78. doi:10.1016/j.hepres.2004.07.001
Kurella Tamura M et al (2010) Prevalence and correlates of cognitive impairment in hemodialysis patients: the Frequent Hemodialysis Network trials. Clin J Am Soc Nephrol : CJASN 5:1429–1438. doi:10.2215/CJN.01090210
Lauridsen MM, Gronbaek H, Naeser EB, Leth ST, Vilstrup H (2012) Gender and age effects on the continuous reaction times method in volunteers and patients with cirrhosis. Metab Brain Dis. doi:10.1007/s11011-012-9318-6
Lauridsen MM, Thiele M, Kimer N, Vilstrup H (2013) The continuous reaction times method for diagnosing, grading, and monitoring minimal/covert hepatic encephalopathy. Metab Brain Dis. doi:10.1007/s11011-012-9373-z
Leto L, Feola M (2014) Cognitive impairment in heart failure patients. J Geriatr Cardiol : JGC 11:316–328. doi:10.11909/j.issn.1671-5411.2014.04.007
Luo M, Li L, Lu CZ, Cao WK (2011) Clinical efficacy and safety of lactulose for minimal hepatic encephalopathy: a meta-analysis. Eur J Gastroenterol Hepatol 23:1250–1257. doi:10.1097/MEG.0b013e32834d1938
Montagnese S et al (2011) Different biochemical correlates for different neuropsychiatric abnormalities in patients with cirrhosis. Hepatology 53:558–566. doi:10.1002/hep.24043
Nordlund A, Berggren J, Holmstrom A, Fu M, Wallin A (2015) Frequent mild cognitive deficits in several functional domains in elderly patients with heart failure without known cognitive disorders. J Card Fail. doi:10.1016/j.cardfail.2015.04.006
Patidar KR et al (2014) Covert hepatic encephalopathy is independently associated with poor survival and increased risk of hospitalization. Am J Gastroenterol. doi:10.1038/ajg.2014.264
Ravona-Springer R et al (2014) Trajectories in glycemic control over time are associated with cognitive performance in elderly subjects with type 2 diabetes. PLoS One 9, e97384. doi:10.1371/journal.pone.0097384
Schomerus H, Hamster W (1998) Neuropsychological aspects of portal-systemic encephalopathy. Metab Brain Dis 13:361–377
Silverwood RJ et al (2014) Cognitive and kidney function: results from a British birth cohort reaching retirement age. PLoS One 9, e86743. doi:10.1371/journal.pone.0086743
Vilstrup H et al (2014) Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study Of Liver Diseases and the European Association for the Study of the Liver. Hepatology 60:715–735. doi:10.1002/hep.27210
West RK et al (2014) The association of duration of type 2 diabetes with cognitive performance is modulated by long-term glycemic control. Am J Geriatr Psychiatr : Off J Am Assoc Geriatr Psychiatr 22:1055–1059. doi:10.1016/j.jagp.2014.01.010
Yaffe K et al (2010) Chronic kidney disease and cognitive function in older adults: findings from the chronic renal insufficiency cohort cognitive study. J Am Geriatr Soc 58:338–345. doi:10.1111/j.1532-5415.2009.02670.x
Zammit AR, Katz MJ, Lai JY, Zimmerman ME, Bitzer M, Lipton RB (2015) Association between renal function and cognitive ability domains in the einstein aging study: a cross-sectional analysis. J Gerontol Ser A Biol Sci Med Sci 70:764–770. doi:10.1093/gerona/glu185
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lauridsen, M.M., Poulsen, L., Rasmussen, C.K. et al. Effects of common chronic medical conditions on psychometric tests used to diagnose minimal hepatic encephalopathy. Metab Brain Dis 31, 267–272 (2016). https://doi.org/10.1007/s11011-015-9741-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-015-9741-6