Abstract
Although cognitive dysfunction manifested by severe memory and attention deficits has been reported in up to 70% of cancer patients undergoing chemotherapy, the mechanisms of this serious side effect have not been defined. In particular, it has not been decisively resolved whether the dysfunction is attributable to the chemotherapy or to the malignancy itself. In the present study we tested whether cognitive dysfunction can be induced in an experimental setting by the administration of commonly used chemotherapeutics to rats. Female 10 month old Sprague–Dawley rats were injected intraperitoneally with a combination of 2.5 mg/kg of adriamycin (ADR) and 25 mg/kg of cytoxan (CTX). A total of four doses were given at weekly intervals. The control group was treated with saline only. No mortality and no apparent morbidity were observed in either group. However, the chemotherapeutic treatment severely impaired memory function of rats as measured by a passive avoidance test. This memory deficiency was fully prevented by the administration of an antioxidant, N-acetyl cysteine (NAC) injected subcutaneously three times a week at 200 mg/kg in the course of chemotherapeutic treatment. These results indicate that chemotherapeutic agents alone, i.e., in the absence of malignancy, damage the brain resulting in memory dysfunction. Moreover, the results strongly indicate that the damaging effect is mediated by oxidative stress, as memory dysfunction is preventable by the co-administration of NAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy with the combination of ADR (or doxorubicin) and CTX (or cyclophosphamide) is widely used as an adjuvant treatment in cancer patients (Goldhirsch et al. 2003). Unfortunately, cognitive dysfunction manifested by severe memory and attention deficits in up to 70% of patients is a serious side effect of chemotherapy (Ahles et al. 2002; Brezden et al. 2000; Schagen et al. 1999; van Dam et al. 1998; Wefel et al. 2004b). Moreover, only about half of affected patients show long-term improvement (Wefel et al. 2004b). However, the mediators of cognitive dysfunction have not been defined. In addition, it has not been decisively resolved whether the dysfunction is a bona fide effect of chemotherapy or is instigated, at least partially, by the malignancy itself (Meyers et al. 2005; Wefel et al. 2004a).
Oxidative stress is the chief candidate among several possible mechanisms for chemotherapy-related cognitive dysfunction (for review see Ahles and Saykin 2007). Different reports have shown decreases in antioxidant levels in patients after chemotherapy treatment (Durken et al. 1995; Durken et al. 2000; Erhola et al. 1996), as well as beneficial association between the plasma concentration of antioxidants and response to chemotherapy (Kennedy et al. 2005). It has also been shown that antioxidant supplementation can reduce chemotherapy related toxicities (Hu et al. 1997; Kennedy et al. 2004), lower recurrence rates (Lamm et al. 1994), and prolong survival time (Jaakkola et al. 1992; Lockwood et al. 1994). Importantly, the efficacy of chemotherapy appears not to be compromised by antioxidant supplementation (Block et al. 2007; Simone et al. 2007a; Simone et al. 2007b).
The present study was undertaken to determine whether the cognitive dysfunction observed in patients undergoing chemotherapy can be replicated in an experimental setting by chronic administration of chemotherapeutics to rats. Furthermore, we wanted to test whether such chemotherapy-induced cognitive dysfunction can be prevented by antioxidant supplementation.
Materials and methods
Materials
ADR was from Bedford Laboratories (Bedford, OH) and CTX was from Bristol-Myers Squibb Co. (Princeton, NJ). N-acetyl cysteine (NAC) and all other chemicals were of the highest obtainable purity from Sigma Chemical Co. (St. Louis, MO).
Chemotherapy treatment
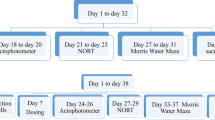
Because breast cancer patients undergoing chemotherapy are typically peri- and postmenopausal women, we used retired breeder rats. Ten-month-old female Sprague–Dawley rats were obtained from Hilltop Lab Animals Inc. (Scottdale, PA), and were housed in the animal quarters under 12 h light/dark conditions with free access to normal rat chow and water. After one week acclimatization animals with no apparent pathologies were selected for the study. All procedures were approved by the West Virginia University Animal Care and Use Committee, and conducted in compliance with the guidelines published in the NIH Guide for the Care and Use of Laboratory Animals. The chemotherapy regimen consisted of intraperitoneal injections of 2.5 mg/kg of ADR and 25 mg/kg of CTX (AC group). A total of four doses were given at weekly intervals. In parallel, a group of rats was injected three times per week for 4 weeks with 200 mg/kg of NAC (an antioxidant) during the course of the chemotherapeutics treatment (AC+N group). The control group (SAL) was treated with saline only.
Open field test
Locomotor activity of the rats was tested 4 days before and 7 days after the chemotherapeutic treatment. The testing was performed in a designated room under standard illumination. Individual rats were placed in an 80 × 80 × 40 cm black wooden box. The floor of this box was divided into nine equal squares by white lines. The number of line crossings and rears was recorded for 30 min by an unbiased observer.
Passive avoidance test
Cognitive function of the animals was examined by the step-through passive avoidance test essentially as described by Zhang et al. (2004). The test was performed using a Shuttle box ENV-010 from Med Associates Inc. (St. Albans, VT) that consisted of an illuminated and a darkened compartment connected by a guillotine door. The floor of the darkened compartment consisted of stainless steel rods through which electric shock could be delivered to the feet. Briefly, 2 days after treatment cessation, rats were habituated to the apparatus by allowing free exploration of both compartments for 5 min. The next day (the training day) a rat was placed in the illuminated compartment facing away from the closed guillotine door for 1 min. Then, the door was raised and the latency of entering into the darkened compartment was recorded by an unbiased observer. As soon as the rat entered the darkened compartment the door was closed and an electric shock of 0.5 mA was administered for 3 s. Twenty four hours later (the testing day), the rat was again placed in the illuminated compartment with the door opened, and the latency of entering into the darkened compartment was recorded for up to 180 s.
Statistical analysis
Results are presented as mean values ± SDs and analyzed by t-test with p < 0.05 considered to be statistically significant.
Results
We used a schedule consisting of four weekly injections with the combination of ADR and CTX at a 1:10 ratio to simulate clinical regimen for patients undergoing breast cancer chemotherapy. In the initial experiments we tested a spectrum of dosages of the chemotherapeutics, and found that dosages as high as 2.5 mg/kg of ADR and 25 mg/kg of CTX produced no apparent morbidity and/or mortality in rats during the four week-treatment. Also, no adverse effects were seen in the rats within a few weeks after the cessation of the treatment. For example, as seen from Fig. 1 (vide infra) the treatment did not affect locomotor activity of the animals. A decreased locomotor activity is an index of the sickness behavior. However, doubling this dosage led to overt pathology and death during and soon after the treatment. Consequently, in the present study we used the schedule of four weekly injections of 2.5 mg/kg of ADR and 25 mg/kg of CTX to assess the effect of chronic administration of these chemotherapeutics on cognitive function.
Locomotor activity. Rats were subjected to the open field test before and after the 4-week treatment with the combination of ADR and CTX (AC), with the chemotherapeutics and NAC (AC+N) or with saline only (SAL) as described in “Materials and methods.” The locomotor activity was assessed by the open field test before and after the treatment. The results show the total number of line crossings (upper panel) and rears (lower panel) during 30 min of testing. Bars represent averages ± SDs. The numbers of animals in each group were 7, 4 and 8 for AC, AC+N and SAL, respectively
The step-through passive avoidance test was deemed to be well suited to assess short-term memory of rats as it is a well-established, non-invasive, relatively simple and highly reproducible procedure. However, one has to be cognizant of the fact that locomotor activity of the animals, which represents an entirely different behavioral entity, may significantly skew the latency measured in the passive avoidance test. Therefore, we tested the animals by the open field test to measure their locomotor activity. This observational, non-invasive test was performed before the chemotherapeutic treatment to assure that there was no significant variability in the locomotor activity among groups. We also performed this evaluation at the end of the experiment to exclude the possibility that changes in the latency of entering the dark compartment during the passive avoidance test resulted from altered locomotor activity caused by the treatment. Figure 1 shows that there was no significant difference among the three groups before the treatment as seen from either the number of line crossings or the number of rears. Neither the 4-week treatment with the chemotherapeutic drugs (AC) nor the treatment with the chemotherapeutic drugs plus NAC altered locomotor activity as compared to the control group that was injected with saline only (SAL). However, there was an overall 60% reduction in the locomotor activity of all animal groups after the treatment as compared to animals before the treatment. This significant decrease likely reflects behavioral differences in the novel (before the treatment) vs. the familiar (after the treatment) environment of the testing box. The recognition of familiar environment after 5 weeks represents a type of long-term memory. Consequently, the open field test also revealed that long-term memory was not significantly affected by the AC-treatment.
As seen from Fig. 2 the passive avoidance test revealed a profound dysfunction of short-term memory induced by the chemotherapeutic treatment. Thus, on the training day rats in all groups rapidly (the average latency of 10 s) hid in the darkened compartment of the apparatus. Once in the darkened compartment the animals experienced an electric shock. On the testing day the control rats (SAL) remembered the electric shock, and consequently, either avoided the darkened compartment or entered it with a long delay. On the average the latency time was 136 s. On the other hand, the memory of the electric shock in the rats subjected to chemotherapeutic treatment (AC) was impaired, and the animals entered the darkened compartment with the average latency of 16 s. Supplementation of chemotherapeutic-treated rats with NAC (AC+N) prevented the drug-induced memory impairment. Thus, the average latency for this group was 110 s, which is significantly longer than the latency for the AC group and comparable to the latency for the SAL animals.
Cognitive function. Rats were treated with the combination of ADR and CTX (AC), with the chemotherapeutics and NAC (AC+N) or with saline only (SAL) as described in Materials and Methods. Subsequently, their memory function was evaluated by the passive avoidance test. The latency of entering the dark compartment was recorded on the training day and on the testing day (24 h later). Bars represent averages ± SDs. The numbers of animals in each group were 7, 4 and 8 for AC, AC+N and SAL, respectively. Asterisk denotes significant differences within each group between the latency on the training and testing day; pound sign denotes significant differences in latency from SAL group on the testing day
Discussion
Clinical studies showed that up to 33% of breast cancer patients exhibited cognitive dysfunction before the commencement of chemotherapy (Wefel et al. 2004a). After chemotherapy treatment 61% of the same cohort exhibited a decline relative to baseline. These results clearly indicate that although the carcinoma by itself may cause brain dysfunction, the chemotherapeutics also have a negative effect on the integrity of higher-order brain function. Other studies have also reported chemotherapy-related cognitive dysfunction with frequencies ranging from 17–70% (Ahles et al. 2002; Brezden et al. 2000; Schagen et al. 1999; van Dam et al. 1998; Wefel et al. 2004b). Moreover, this chemotherapy-induced effect seems not to be related to the neoplasia (Ahles et al. 2002). Our present studies in rats demonstrate that chronic administration of commonly used chemotherapeutics, i.e., the combination of ADR and CTX, impairs short-term (24 h) memory function (Fig. 2). This is an important finding because it proves that chemotherapeutic agents alone, i.e., in the absence of malignancy, can instigate higher-order brain dysfunction, and thus, supports clinical observations. Interestingly, the chemotherapeutics do not seem to affect long-term (five weeks) memory as seen from the recognition of the box environment in the open field test (Fig. 1).
The mechanisms of chemotherapeutic action of ADR and CTX are complex as these drugs affect a multitude of cellular processes. For example, ADR disturbs chromosomal replication by inhibiting DNA synthesis (Cummings et al. 1991; Gewirtz 1999; Tanaka and Yoshida 1980) and topoisomerase II (Chuang and Chuang 1979; Tewey et al. 1984), and thus, targets malignant cells. However, ADR can also generate free radicals, such as the superoxide radical and lipid peroxides (De Beer et al. 2001; Goodman and Hochstein 1977; Olson and Mushlin 1990; Singal et al. 2000), which are responsible for the non-targeted cytotoxicity of ADR. CTX requires metabolic activation by the cytochrome P450 mixed function oxidase system to form phosphoramide mustard (Sladek 1971; Sladek 1972a; Sladek 1972b), the principal alkylating anti-neoplastic metabolite (Friedman et al. 1976). However, this oxidative conversion also generates free radicals (Bhattacharya et al. 2003; Stankiewicz et al. 2002). In addition, another CTX metabolite, acrolein, is a very reactive compound that binds to and depletes intracellular GSH (Kehrer and Biswal 2000). Consequently, antioxidants have been used during chemotherapy treatments to offset the non-targeted effects of these drugs. Nevertheless, it has been cautioned that the oxidative stress may also contribute to the eradication of neoplastic cells and that antioxidants may diminish the effectiveness of the chemotherapeutics. However, recent comprehensive clinical reviews demonstrate no alterations in the effectiveness of chemotherapeutic treatment when antioxidants are co-administered (Block et al. 2007; Simone et al. 2007a; Simone et al. 2007b).
Although the exact mechanisms by which ADR and CTX mediate cognitive dysfunction have not been defined, oxidative stress seems to play a causative role. Thus, systemic administration of either chemotherapeutic agent has been shown to augment the level of oxidative stress indicators in the brain, and this effect can be mitigated by antioxidants (Bhatia et al. 2006; Joshi et al. 2005; Joshi et al. 2007). Glutathione (GSH) is of a particular interest as it is a major component of the antioxidant armamentarium of cells. Decreased levels of GSH have been reported in brains of animals treated with ADR (Joshi et al. 2007; Julka et al. 1993) and CTX (Bhatia et al. 2006). Joshi et al. (2007) also found that the administration of γ-glutamyl cystein ethyl ester, which elevates intracellular GSH concentration, ameliorated brain oxidative stress induced by acute ADR toxicity in mice. In the present study we used NAC that also replenishes intracellular GSH and showed that this antioxidant prevented memory dysfunction induced by chronic administration of the combination of ADR and CTX in rats. This protective effect of NAC buttresses the notion that oxidative stress mediates the cognitive dysfunction caused by these chemotherapeutics. Taken together, the aforementioned studies indicate clinical potential of GSH boosters to ameliorate chemotherapy-related brain dysfunction.
In conclusion, our experimental paradigm provides a convenient model system to study the mechanisms of brain dysfunction elicited by chemotherapy and for testing the potency of putative preventive agents. The well tolerated antioxidant, such as NAC and/or other GSH boosters may provide efficient ways to combat the cognitive dysfunction associated with ADR/CTX chemotherapy observed in clinical settings.
References
Ahles TA, Saykin AJ (2007) Candidate mechanisms for chemotherapy-induced cognitive changes. Nat Rev Cancer 7:192–201
Ahles TA, Saykin AJ, Furstenberg CT, Cole B, Mott LA, Skalla K, Whedon MB, Bivens S, Mitchell T, Greenberg ER, Silberfarb PM (2002) Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol 20:485–493
Bhatia AL, Manda K, Patni S, Sharma AL (2006) Prophylactic action of linseed (Linum usitatissimum) oil against cyclophosphamide-induced oxidative stress in mouse brain. J Med Food 9:261–264
Bhattacharya A, Lawrence RA, Krishnan A, Zaman K, Sun D, Fernandes G (2003) Effect of dietary n-3 and n-6 oils with and without food restriction on activity of antioxidant enzymes and lipid peroxidation in livers of cyclophosphamide treated autoimmune-prone NZB/W female mice. J Am Coll Nutr 22:388–399
Block KI, Koch AC, Mead MN, Tothy PK, Newman RA, Gyllenhaal C (2007) Impact of antioxidant supplementation on chemotherapeutic efficacy: a systematic review of the evidence from randomized controlled trials. Cancer Treat Rev 33(5):407–18
Brezden CB, Phillips KA, Abdolell M, Bunston T, Tannock IF (2000) Cognitive function in breast cancer patients receiving adjuvant chemotherapy. J Clin Oncol 18:2695–2701
Chuang RY, Chuang LF (1979) Inhibition of chicken myeloblastosis RNA polymerase II activity by adriamycin. Biochemistry 18:2069–2073
Cummings J, Anderson L, Willmott N, Smyth JF (1991) The molecular pharmacology of doxorubicin in vivo. Eur J Cancer 27:532–535
De Beer EL, Bottone AE, Voest EE (2001) Doxorubicin and mechanical performance of cardiac trabeculae after acute and chronic treatment: a review. Eur J Pharmacol 415:1–11
Durken M, Agbenu J, Finckh B, Hubner C, Pichlmeier U, Zeller W, Winkler K, Zander A, Kohlschutter A (1995) Deteriorating free radical-trapping capacity and antioxidant status in plasma during bone marrow transplantation. Bone Marrow Transplant 15:757–762
Durken M, Herrnring C, Finckh B, Nagel S, Nielsen P, Fischer R, Berger HM, Moison RM, Pichlmeier U, Kohlschutter B, Zander AR, Kohlschutter A (2000) Impaired plasma antioxidative defense and increased nontransferrin-bound iron during high-dose chemotherapy and radiochemotherapy preceding bone marrow transplantation. Free Radic Biol Med 28:887–894
Erhola M, Kellokumpu-Lehtinen P, Metsa-Ketela T, Alanko K, Nieminen MM (1996) Effects of anthracyclin-based chemotherapy on total plasma antioxidant capacity in small cell lung cancer patients. Free Radic Biol Med 21:383–390
Friedman OM, Wodinsky I, Myles A (1976) Cyclophosphamide (NSC-26271)-related phosphoramide mustards—recent advances and historical perspective. Cancer Treat Rep 60:337–346
Gewirtz DA (1999) A critical evaluation of the mechanisms of action proposed for the antitumor effects of the anthracycline antibiotics adriamycin and daunorubicin. Biochem Pharmacol 57:727–741
Goldhirsch A, Wood WC, Gelber RD, Coates AS, Thurlimann B, Senn HJ (2003) Meeting highlights: updated international expert consensus on the primary therapy of early breast cancer. J Clin Oncol 21:3357–3365
Goodman J, Hochstein P (1977) Generation of free radicals and lipid peroxidation by redox cycling of adriamycin and daunomycin. Biochem Biophys Res Commun 77:797–803
Hu YJ, Chen Y, Zhang YQ, Zhou MZ, Song XM, Zhang BZ, Luo L, Xu PM, Zhao YN, Zhao YB, Cheng G (1997) The protective role of selenium on the toxicity of cisplatin-contained chemotherapy regimen in cancer patients. Biol Trace Elem Res 56:331–341
Jaakkola K, Lahteenmaki P, Laakso J, Harju E, Tykka H, Mahlberg K (1992) Treatment with antioxidant and other nutrients in combination with chemotherapy and irradiation in patients with small-cell lung cancer. Anticancer Res 12:599–606
Joshi G, Sultana R, Tangpong J, Cole MP, St Clair DK, Vore M, Estus S, Butterfield DA (2005) Free radical mediated oxidative stress and toxic side effects in brain induced by the anti cancer drug adriamycin: insight into chemobrain. Free Radic Res 39:1147–1154
Joshi G, Hardas S, Sultana R, St Clair DK, Vore M, Butterfield DA (2007) Glutathione elevation by gamma-glutamyl cysteine ethyl ester as a potential therapeutic strategy for preventing oxidative stress in brain mediated by in vivo administration of adriamycin: Implication for chemobrain. J Neurosci Res 85:497–503
Julka D, Sandhir R, Gill KD (1993) Adriamycin-induced oxidative stress in rat central nervous system. Biochem Mol Biol Int 29:807–820
Kehrer JP, Biswal SS (2000) The molecular effects of acrolein. Toxicol Sci 57:6–15
Kennedy DD, Tucker KL, Ladas ED, Rheingold SR, Blumberg J, Kelly KM (2004) Low antioxidant vitamin intakes are associated with increases in adverse effects of chemotherapy in children with acute lymphoblastic leukemia. Am J Clin Nutr 79:1029–1036
Kennedy DD, Ladas EJ, Rheingold SR, Blumberg J, Kelly KM (2005) Antioxidant status decreases in children with acute lymphoblastic leukemia during the first six months of chemotherapy treatment. Pediatr. Blood Cancer 44:378–385
Lamm DL, Riggs DR, Shriver JS, vanGilder PF, Rach JF, DeHaven JI (1994) Megadose vitamins in bladder cancer: a double-blind clinical trial. J Urol 151:21–26
Lockwood K, Moesgaard S, Hanioka T, Folkers K (1994) Apparent partial remission of breast cancer in ‘high risk’ patients supplemented with nutritional antioxidants, essential fatty acids and coenzyme Q10. Mol Aspects Med 15(Suppl):s231–s240
Meyers CA, Albitar M, Estey E (2005) Cognitive impairment, fatigue, and cytokine levels in patients with acute myelogenous leukemia or myelodysplastic syndrome. Cancer 104:788–793
Olson RD, Mushlin PS (1990) Doxorubicin cardiotoxicity: analysis of prevailing hypotheses. FASEB J 4:3076–3086
Schagen SB, van Dam FS, Muller MJ, Boogerd W, Lindeboom J, Bruning PF (1999) Cognitive deficits after postoperative adjuvant chemotherapy for breast carcinoma. Cancer 85:640–650
Simone CB, Simone NL, Simone V, Simone CB (2007a) Antioxidants and other nutrients do not interfere with chemotherapy or radiation therapy and can increase kill and increase survival, part 1. Altern Ther Health Med 13:22–28
Simone CB, Simone NL, Simone V, Simone CB (2007b) Antioxidants and other nutrients do not interfere with chemotherapy or radiation therapy and can increase kill and increase survival, Part 2. Altern Ther Health Med 13:40–47
Singal PK, Li T, Kumar D, Danelisen I, Iliskovic N (2000) Adriamycin-induced heart failure: mechanism and modulation. Mol Cell Biochem 207:77–86
Sladek NE (1971) Metabolism of cyclophosphamide by rat hepatic microsomes. Cancer Res 31:901–908
Sladek NE (1972a) Therapeutic efficacy of cyclophosphamide as a function of inhibition of its metabolism. Cancer Res 32:1848–1854
Sladek NE (1972b) Therapeutic efficacy of cyclophosphamide as a function of its metabolism. Cancer Res 32:535–542
Stankiewicz A, Skrzydlewska E, Makiela M (2002) Effects of amifostine on liver oxidative stress caused by cyclophosphamide administration to rats. Drug Metabol Drug Interact 19:67–82
Tanaka M, Yoshida S (1980) Mechanism of the inhibition of calf thymus DNA polymerases alpha and beta by daunomycin and adriamycin. J Biochem (Tokyo) 87:911–918
Tewey KM, Rowe TC, Yang L, Halligan BD, Liu LF (1984) Adriamycin-induced DNA damage mediated by mammalian DNA topoisomerase II. Science 226:466–468
van Dam FS, Schagen SB, Muller MJ, Boogerd W, vd Wall E, Droogleever Fortuyn ME, Rodenhuis S (1998) Impairment of cognitive function in women receiving adjuvant treatment for high-risk breast cancer: high-dose versus standard-dose chemotherapy. J Natl Cancer Inst 90:210–218
Wefel JS, Lenzi R, Theriault R, Buzdar AU, Cruickshank S, Meyers CA (2004a) ‘Chemobrain’ in breast carcinoma?: a prologue. Cancer 101:466–475
Wefel JS, Lenzi R, Theriault RL, Davis RN, Meyers CA (2004b) The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer 100:2292–2299
Zhang HT, Zhao Y, Huang Y, Dorairaj NR, Chandler LJ, O’Donnell JM (2004) Inhibition of the phosphodiesterase 4 (PDE4) enzyme reverses memory deficits produced by infusion of the MEK inhibitor U0126 into the CA1 subregion of the rat hippocampus. Neuropsychopharmacology 29:1432–1439
Acknowledgements
This study was supported by DOD research grant DAMD17-02-1-0621.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Konat, G.W., Kraszpulski, M., James, I. et al. Cognitive dysfunction induced by chronic administration of common cancer chemotherapeutics in rats. Metab Brain Dis 23, 325–333 (2008). https://doi.org/10.1007/s11011-008-9100-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-008-9100-y