Abstract
Maple Syrup Urine Disease (MSUD) is an autossomal recessive metabolic disorder caused by a deficiency of branched-chain α-keto acid dehydrogenase complex activity leading to accumulation of the branched-chain amino acids leucine, isoleucine and valine and their corresponding branched-chain α-keto acids. Affected patients usually present hypoglycemia, ketoacidosis, convulsions, poor feeding, coma, psychomotor delay and mental retardation. Considering that the pathophysiology of MSUD is still poorly understood, in this study we evaluated some parameters of oxidative stress, namely thiobarbituric acid-reactive substances (TBARS), total antioxidant reactivity (TAR) and total antioxidant status (TAS) in plasma from treated MSUD patients presenting high and low plasma leucine levels. We verified a significant increase of TBARS (lipid peroxidation) and a decrease of TAR (capacity to rapidly react with free radicals) in plasma from treated MSUD patients with low and with high plasma levels of leucine compared to the control group. It was also verified that TAS (quantity of tissue antioxidants) was not altered in plasma from treated MSUD patients with low and high blood leucine levels. Finally, we found no correlation between leucine, valine and isoleucine levels with the various parameters of oxidative stress. These results are indicative that increased lipid oxidative damage and decreased antioxidant defenses occur in plasma of MSUD patients and that the accumulating branched-chain amino acids are probably not directly associated to oxidative stress in this disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maple Syrup Urine Disease (MSUD) is an inherited disorder affecting the metabolism of branched-chain amino acids (BCAA) leucine (Leu), isoleucine (Ile) and valine (Val). The activity of the branched-chain α-keto acid dehydrogenase complex (BCKAD) is deficient in MSUD leading to tissue accumulation of BCAA (Leu, Ile e Val), as well as their corresponding transaminated branched-chain α-keto acids (BCKA) α-ketoisocaproate, α-keto-β-methylvalerate and α-ketoisovalerate (Chuang and Shih 2001; Treacy et al. 1992).
The clinical and biochemical phenotypes of MSUD patients are heterogeneous. Patients can be divided into five phenotypes ranging from the classical form with a neonatal onset to milder variants with later onset (Chuang and Shih 2001; Schadewaldt and Wendel 1997). Individuals with MSUD usually present poor feeding, convulsions, ketoacidosis, apnea, hypoglycemia, coma, ataxia, psychomotor delay and mental retardation, as well as generalized edema and hypomyelination/demyelination on magnetic resonance imaging studies of the central nervous system (CNS) (Chuang and Shih 2001; Schönberger et al. 2004). Therapy for this disease is based on a natural protein restricted diet with low BCAA supplemented with a semi-synthetic formula of essential amino acids, vitamins and minerals. This treatment minimizes the accumulation of the toxic metabolites and contributes to the survival of the affected individuals, but do not prevent a variable degree of neurological dysfunction evidenced by developmental delay and mental retardation whose pathogenesis is poorly known (Chuang and Shih 2001). Leucine and/or α-ketoisocaproate are thought to be the main neurotoxic metabolites in this disorder once their increased concentrations have been associated to the appearance of neurological symptoms (Chuang and Shih 2001; Snyderman et al. 1964).
Free radicals and oxidative stress have been associated with a large number of diseases including various neurodegenerative disorders, epileptic seizures, demyelination and dementia (Halliwell 1994; Reznick and Packer 1993; Przedborski et al. 1996; Ben-Menachem et al. 2000). This may occur because the CNS is highly susceptible to oxidative damage due to the relatively low activity of antioxidant defenses, high iron content, high lipid content, specially unsaturated fatty acids, and high oxygen consumption (Halliwell and Gutteridge 2001). Oxidative stress has been also observed in some inborn errors of intermediary metabolism, and this has been attributed to the accumulation of toxic metabolites which are able to induce excessive free radical generation (Colome et al. 2000; Wajner et al. 2004). We cannot also exclude the possibility that the restricted diets used to treat patients with metabolic disorders may decrease the tissue antioxidant defenses since they potentially deplete essential nutrients involved in the antioxidant defenses (Halliwell and Gutteridge 2001).
With regards to MSUD, experimental animal studies have demonstrated that lipid peroxidation is stimulated in vitro by the BCAA and their respective BCKA in brain homogenates of rats (Fontella et al. 2002). It was also verified that these metabolites reduce in vitro the cerebral capacity to modulate the damage associated to increased free radical production (Bridi et al. 2003; Bridi et al. 2005a) and that the increased lipid peroxidation induced in vitro in cerebral cortex of rats by leucine is attenuated by the free radicals scavengers ascorbic acid, α-tocopherol, gluthatione and superoxide dismutase (Bridi et al. 2005b).
On the other hand, we recently verified that the antioxidant status and lipid peroxidation were significantly altered in plasma of MSUD patients at diagnosis, suggesting the involvement of oxidative stress in the pathogenesis of this disease (Barschak et al. 2006). In the present study, we evaluated various parameters of oxidative stress in blood from treated MSUD patients showing high and low blood leucine levels, in order to test whether this amino acid could be involved in the oxidative stress. The parameters analyzed were thiobarbituric acid-reactive substances (TBARS), total antioxidant reactivity (TAR) and total antioxidant status (TAS).
Materials and methods
Reagents
All chemicals were of PA purity and were purchased from Sigma (St. Louis, MO, USA) except thiobarbituric acid that was purchased from Merck (Darmstadt, Germany) and a kit for TAS measurement that was purchased from Randox Laboratories (Antrim, United Kingdom). TAR was assayed using a beta liquid scintillation spectrometer (Wallac model 1409), TBARS was measured in a spectrofluorimeter (Hitachi F2000) and TAS in a double-bean spectrophotometer with temperature control (Hitachi U-2001).
Subjects
Plasma specimens from ten treated MSUD patients with the classic form and five age matched controls were used to evaluate the parameters of oxidative stress. The patients were aged between 15 days and 4 months at diagnosis and followed a treatment that consisted of a natural protein restricted diet with low BCAA and supplemented with a semi-synthetic formula of essential amino acids, vitamins and minerals. The patients ingested the following amounts of Leu (before 12 months of age: 40–80 mg kg−1 day−1; after 1 year of age: 275–535 mg/day), Ile (before 12 months of age: 20–50 mg kg−1 day−1; after 1 year of age: 165–325 mg/day) and Val (before 12 months of age: 20–60 mg kg−1 day−1; after 1 year of age: 190–375 mg/day). Plasma samples obtained from MSUD patients under treatment were divided into two groups depending on blood Leu levels. In group I plasma Leu levels were lower than 100 μmol/l (36.3 ± 17.1 μmol/l, treatment duration was 18.6 ± 12.9 months), whereas in group II plasma Leu levels were higher than 600 μmol/l (1,314 ± 914 μmol/l, treatment duration was 17.2 ± 20.1 months). The control group corresponded to healthy age matched individuals (leucine 158 ± 37.6 μmol/l; isoleucine 76.5 ± 18.0 μmol/l; valine 260 ± 39.8 μmol/l) (Table 1).
The present study was approved by the Ethical Committee of Hospital de Clínicas de Porto Alegre, RS, Brazil (protocol number 04-256). The parents of the patients included in the present study gave informed consent.
Plasma preparation and amino acids determination
Plasma was prepared from whole blood samples obtained from fasting individuals (controls and MSUD patients) by venous puncture with heparinized vials. Whole blood was centrifuged at 1,000×g and plasma was removed by aspiration and frozen at −80°C until analysis. Blood amino acids levels were measured by HPLC (Joseph and Marsden 1986), with slight modifications (Wajner et al. 2000).
Thiobarbituric acid-reactive substances (TBARS)
Thiobarbituric acid-reactive substances (TBARS) were determined according to the method described by Buege and Aust 1978. Briefly, 250 μl of 10% trichloroacetic acid were added to 125 μl of plasma. Then 375 μl 0.67% thiobarbituric acid (in 7.1% sodium sulphate) were added and incubated at 100°C for 30 min. After the incubation, the mixture was extracted with 750 μl butanol. The resulting pink stained TBARS were determined in a spectrofluorimeter at 515 nm. Calibration curve was performed using 1,1,3,3-tetramethoxypropane subjected to the same treatment as that of the samples. TBARS were calculated as nmol TBARS/mg protein.
Total antioxidant reactivity (TAR)
TAR, which represents the quality of the tissue antioxidants, was determined by measuring the luminol chemiluminescence intensity induced by 2,2′-azo-bis-(2-amidinopropane) (ABAP) according to the method of Lissi et al. (1992). The background chemiluminescence was measured by adding 4 ml of 2 mM ABAP (in 0.1 M glycine buffer, pH 8.6) into a glass scintillation vial. Ten microliters of luminol (4 mM) were added to each vial and the chemiluminescence was measured. This was considered to be the basal value. Ten microliters of 25–200 μM Trolox (curve calibration) or plasma was then added and the chemiluminescence was measured during 60 s. The Trolox and plasma addition reduce the chemiluminescence. The rapid reduction in luminol intensity is considered as a measure of the TAR capacity. TAR measurement was calculated as nmol Trolox/mg protein.
Total antioxidant status (TAS)
TAS, which represents the quantity of the tissue antioxidants, was determined by using a kit from RANDOX Laboratories. The plasma sample was incubated with ABTS (2,2′-azino-di-[3-ethylbenzthiazoline sulphonate]) plus a peroxidase (metmyoglobin) and H2O2 to produce the cation ABTS+. A relatively stable blue–green color occurred and was measured at 37°C at 600 nm. Antioxidants in the added sample cause suppression of this color production to a degree which is proportional to their concentration (Miller et al. 1993; Yu and Ong 1999). The results were expressed in millimole per liter.
Protein determination
Protein concentrations were determined by the Biuret method from Labtest® (Gornall et al. 1949), using bovine serum albumin as standard.
Statistical analysis
Results were analyzed by one-way ANOVA, followed by the Duncan multiple range test when appropriated (Altman 1991). Only significant F values are shown in the text. Correlations of plasma Leu, Val and Ile levels with TBARS, TAR or TAS were carried out using the Pearson correlation coefficient. A p value less than 0.05 was considered significant. All analyses were performed using the Statistical Package for the Social Sciences (SPSS) software in a PC-compatible computer.
Results
Figure 1 shows that TBARS measurement was significantly increased in plasma from MSUD patients both with low (group I) and high (group II) Leu levels, as compared to the control group [F(2,12) = 4.289, p < 0.05]. These data indicate that lipid peroxidation is stimulated in plasma from MSUD patients.
Comparison between thiobarbituric acid reactive substances (TBARS) in plasma from MSUD patients during treatment and controls. Data represent the mean ± SE (n = 5). Single asterisk p < 0.05, compared to controls (ANOVA, followed by the Duncan multiple range test). Group I: low plasma leucine levels; group II: high plasma leucine levels
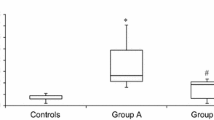
Furthermore, TAR measurement was significantly reduced in plasma of MSUD patients independently of the concentration of Leu (high and low Leu levels), as compared to the control group [F(2,12) = 30.196, p < 0.001] (Fig. 2). It can be also observed in the figure that group I is different from group II. Considering that TAR measurement reflects the tissue capacity to react with free radicals, these results suggest a deficient capacity of plasma from treated MSUD patients to modulate the damage associated with the enhanced production of reactive species.
Comparison between total antioxidant reactivity (TAR) in plasma from MSUD patients during treatment and controls. Data represent the mean ± SE (n = 5). Single asterisk p < 0.001, compared to controls (ANOVA, followed by the Duncan multiple range test). Pound sign p < 0.001, compared to group II (ANOVA, followed by the Duncan multiple range test). Group I: low plasma leucine levels; group II: high plasma leucine levels
We also observed that TAS measurement, which represents the quantity of tissue antioxidants, was not altered in plasma from treated MSUD patients (group I and group II), as compared to the control group [F(2,12) = 3.352, p > 0.05] (Fig. 3).
Finally we found no correlation between Leu, Ile and Val blood levels and TBARS, TAR and TAS measurements (results not shown).
Discussion
MSUD treatment is directed to minimize the accumulation of the toxic metabolites BCAA and BCKA and decisively contributes to the survival of affected individuals. However, some patients present a variable degree of developmental delay and mental retardation that are attributed to a poor adherence to the restricted diet (Chuang and Shih 2001).
Although the mechanisms underlying the pathophysiology of the brain damage in MSUD are still poorly understood, high plasma levels of Leu and its ketoacid derivative α-ketoisocaproate have been correlated with the appearance of neurological symptoms (Chuang and Shih 2001). Furthermore, it has been demonstrated that the metabolites accumulating in MSUD cause impairment of energy metabolism by inhibiting the electron transport chain (Sgaravatti et al. 2003) and creatine kinase activity (Pilla et al. 2003), induce neuronal apoptosis (Jouvet et al. 2000), convulsions (Coitinho et al. 2001), impairment of neurotransmitter synthesis and function (Zielke et al. 1996; Tavares et al. 2000), induce alterations of myelin synthesis or degradation (Treacy et al. 1992; Tribble and Shapira 1983; Taketomi et al. 1983) and also reduce the uptake of essential amino acids by the brain (Araújo et al. 2001).
Human and animal studies have indicated that metabolites accumulating in various inborn errors of metabolism induce excessive free radical production and reduce the tissue antioxidant defenses (Colome et al. 2000; Wajner et al. 2004). In this context, oxidative stress has been demonstrated in patients with phenylketonuria (Sirtori et al. 2005) and adrenoleukodystrophy (Vargas et al. 2004) and leucine and α-ketoisocaproate were shown to stimulate in vitro lipid peroxidation and reduce the cerebral antioxidant reactivity in cerebral homogenates from young rats (Fontella et al. 2002; Bridi et al. 2003; Bridi et al. 2005a).
We have recently verified that plasma from MSUD patients at diagnosis present increased lipid peroxidation and decreased antioxidant reactivity, indicating the involvement of oxidative stress in the pathogenesis of this disease (Barschak et al. 2006). In order to extend this investigation and better understand the involvement of oxidative stress in the pathophysiology of MSUD, in the present study we measured TBARS, TAR and TAS in plasma from MSUD patients with high and low levels of leucine and compared to plasma from normal age matched individuals. We also investigated whether alterations of those parameters were correlated with plasma leucine concentrations, as well as, isoleucine and valine.
We demonstrated that TBARS measurement was significantly increased in plasma from treated MSUD patients with both high and low leucine levels. Since TBARS reflects the formation of malondialdehyde, an end product of membrane fatty acid peroxidation (Halliwell and Gutteridge 2001; Esterbauer and Cheeseman 1990), these data suggest that patients under treatment present increased lipid oxidative damage (lipid peroxidation) independently of plasma Leu levels. Furthermore, we did not find a correlation between plasma concentrations of leucine, valine and isoleucine with the lipid peroxidation parameter TBARS. Taken together these observations, it may be presumed that leucine and the other BCAA are not directly associated to free radical production in MSUD.
We also observed that TAR measurement, which represents the capacity of a tissue to modulate the damage associated with an increased production of free radicals, reflecting the quality of non enzymatic antioxidants (Lissi et al. 1995), was significantly decreased in plasma from treated MSUD patients and that this decrease was not dependent on the plasma concentrations of leucine. In addition, TAS (total antioxidant status) measurement, which corresponds to the total quantity of tissue non enzymatic antioxidants, was not altered plasma of MSUD patients presenting low and high leucine levels. It may be therefore presumed that the dietetic treatment (low protein diet) contributed to reduce the tissue antioxidants in these patients since strict protein ingest may secondarily deplete essential substances involved in the antioxidant system, like minerals, vitamins and selenium. We believe that lack of nutrients may be involved in the reduction of antioxidant defenses observed in our present study since patients with low blood leucine levels (more adherent to treatment) would theoretically have greater nutrient deficiency than those with high plasma leucine concentrations and consequently much lower TAR, what was observed in ours patients. These observations, allied to the fact that no correlation was found between leucine, valine and isoleucine with TBARS, TAR and TAS values, indicate that other factors than the BCAA should be investigated to explain our present results.
In summary, taken together the present and previous findings (Barschak et al. 2006), it can be concluded that MSUD patients present increased lipid peroxidation and decreased antioxidant defenses at diagnosis and after treatment, which is strongly indicative that oxidative stress may be an underlying mechanism of tissue damage in this disorder. We also observed that the alterations observed were not associated to the plasma levels of leucine, suggesting that other factors, including the BCKA, which are primarily accumulated in these patients, are potentially responsible for the oxidative damage in this disorder. It could be therefore presumed that oxidative stress may contribute at least in part to the chronic progressive neurological damage observed in MSUD patients. Thus, it is desirable that more studies involving other oxidative stress parameters and a larger number of treated patients are carried out in order to better understand the contribution of oxidative stress in MSUD pathophysiology.
References
Altman DG (1991) Practical statistics for medical research. Chapman & Hall, London
Araújo PR, Wassermann GF, Tallini K, Furlanetto V, Vargas CR, Wannmacher CMD, Dutra-Filho CS, Wyse ATS, Wajner M (2001) Reduction of large neutral amino acid level in plasma and brain of hyperleucinemic rats. Neurochem Int 38:529–537
Barschak AG, Sitta A, Deon M, Oliveira MH, Haeser A, Dutra-Filho CS, Wajner M, Vargas CR (2006) Evidence that oxidative stress is increased in plasma from patients with Maple Syrup Urine Disease. Metab Brain Dis 21:279–286
Ben–Menachem E, Kyllerman R, Markleind S (2000) Superoxide dismutase and glutathione peroxidase function in progressive myoclonus epilepsies. Epilepsy Res 40:33–39
Bridi R, Araldi J, Sgarbi MB, Testa CG, Durigon K, Wajner M, Dutra-Filho CS (2003) Induction of oxidative stress in rat brain by the metabolites accumulating in maple syrup urine disease. Int J Dev Neurosci 21:327–332
Bridi R, Braun CA, Zorzi GK, Wannmacher CMD, Wajner M, Lissi EG, Dutra-Filho CS (2005a) Alpha-keto acids accumulating in maple syrup urine disease stimulate lipid peroxidation and reduce antioxidant defences in cerebral cortex from young rats. Metab Brain Dis 20:155–167
Bridi R, Latini A, Braum CA, Zorzi GK, Wajner M, Lissi E, Dutra-Filho CS (2005b) Evaluation of the mechanism involved in leucine-induced oxidative damage in cerebral córtex of young rats. Free Radic Res 39:71–79
Buege JA, Aust SD (1978) Microssomal lipid peroxidation. Methods Enzymol 52:302–309
Chuang DT, Shih VE (2001) Maple syrup urine disease (branched-chain ketoaciduria). In: Scriver CR, Beaudt AL, Sly WL, Valle D (eds) The metabolic and molecular bases of inherited disease. McGraw-Hill, New York, pp 1971–2005
Coitinho AS, de Mello CF, Lima TT, de Bastiani J, Fighera MR, Wajner M (2001) Pharmacological evidence that alpha-keto isovaleric acid induces convulsions through GABAergic and glutamatergic mechanisms in rats. Brain Res 894:68–73
Colome C, Sierra C, Vilaseca MA (2000) Congenital errors of metabolism: cause of oxidative stress? Med Clin 115:111–117
Esterbauer H, Cheeseman KH (1990) Determination of aldehydic lipid peroxidation products: malonaldehyde and 4-hydroxynonenal. Methods Enzymol 186:407–421
Fontella FU, Gassen E, Pulrolnik V, Wannmacher CMD, Klein AB, Wajner M, Dutra CS (2002) Stimulation of lipid peroxidation in vitro in rat brain by metabolites accumulating in maple syrup urine disease. Metab Brain Dis 17:47–54
Gornall AG, Bardawill CJ, David MM (1949) Determination of serum proteins by means of the biuret reaction. J Biol Chem 177:751–766
Halliwell B (1994) Free radicals, antioxidants and human disease: curiosity, cause or consequence? Lancet 344:721–724
Halliwell B, Gutteridge JMC (eds) (2001) Free radicals in biology and medicine. Oxford University Press, Oxford
Joseph MH, Marsden CA (1986) Amino acids and small peptides. In: Lim CF (ed) HPLC of small peptides. IRL Press, Oxford, pp 13–27
Jouvet P, Rustin P, Taylor DL, Pocock JM, Felderhoff-Mueser U, Mazarakis ND, Sarraf C, Joashi U, Koszma M, Greewood K, Edwards AD, Mehmet H (2000) Branched chain amino acids induce apoptosis in neural cells without mitochondrial membrane despolarization or cytochrome c release: implications for neurological impairment associated with maple syrup urine disease. Mol Biol Cell 11:1919–1932
Lissi E, Pascual C, Del Castillo MD (1992) Luminol luminescence induced by 2,2′-azo-bis-(2-amidinopropane) thermolysis. Free Radic Res Commun 17:299–311
Lissi E, Salim-Hanna M, Pascual C, Del Castillo MD (1995) Evaluation of total antioxidant potential (TRAP) and total antioxidant reactivity from luminol-enhanced chemiluminescence measurements. Free Radic Biol Med 18:153–158
Miller NJ, Rice-Evans C, Davies MJ, Gopinathan V, Milner A (1993) A novel method for measuring antioxidant capacity and its application to monitoring the antioxidant status in premature neonates. Clin Sci 84:407–412
Pilla C, de Oliveira Cardozo RF, Dutra-Filho CS, Wyze ATS, Wajner M, Wannmacher CMD (2003) Effect of leucine administration on creatine kinase activity in rat brain. Metab Brain Dis 18:17–25
Przedborski S, Donaldson DBS, Jakowec M, Kish JS, Guttman M, Rosoklija G, Hays AP (1996) Brain superoxide dismutase, catalase and glutathione peroxidase activities in amyotrophic lateral sclerosis. Ann Neurol 39:158–165
Reznick AZ, Packer L (1993) Free radicals and antioxidants in muscular neurological diseases and disorders. In: Poli G, Albano E, Dianzani MU (eds) Free radicals: from basic science to medicine. Birkhäuser Verlag, Basel, pp 425–437
Schadewaldt P, Wendel U (1997) Metabolism of branched-chain amino acids in maple syrup urine disease. Eur J Pediatr 156(suppl. 1):S62–S66
Schönberger S, Schweiger B, Schwahn B, Schwarz M, Wendel U (2004) Dysmyelination in the brain of adolescents and young adults with maple syrup urine disease. Mol Genet Metab 82:69–75
Sgaravatti AM, Rosa RB, Schuck PF, Ribeiro CAJ, Wannmacher CMD, Wyse ATS, Dutra-Filho CS, Wajner M (2003) Inhibition of brain energy metabolism by the α-keto acids accumulating in maple syrup urine disease. Biochim Biophys Acta 1639:232–238
Sirtori LR, Dutra-Filho CS, Fitarelli D, Sitta A, Haeser A, Barschak AG, Wajner M, Coelho DM, Llesuy S, Belló-Klein A, Giugliani R, Deon M, Vargas CR (2005) Oxidative stress in patient with phenylketonuria. Biochim Biophys Acta 1740:68–73
Snyderman SE, Norton PM, Roitman E, Holt LE Jr (1964) Maple syrup urine disease with particular reference to dietotherapy. Pediatrics 34:454–472
Taketomi T, Kunishita T, Hara A, Mizushima S (1983) Abnormal protein and lipid compositions of the cerebral myelin in patient with maple syrup urine disease. Jpn J Exp Med 53:109–116
Tavares RG, Santos CE, Tasca CI, Wajner M, Souza DO, Dutra-Filho CS (2000) Inhibition of glutamate uptake into synaptic vesicles of rat brain by the metabolites accumulating in maple syrup urine disease. J Neurol Sci 181:44–49
Treacy E, Clow CL, Reade TR, Chitayat D, Mamer OA, Scriver CR (1992) Maple syrup urine disease: interrelationship between branched-chain amino-, oxo- and hydroxyacids; implications for treatment; associations with CNS dysmyelination. J Inherit Metab Dis 15:121–135
Tribble D, Shapira R (1983) Myelin proteins: degradation in rat brain initiated by metabolites causative of maple syrup urine disease. Biochem Biophys Res Commun 114:440–446
Vargas CR, Wajner M, Sirtori LR, Goulart L, Chiochetta M, Coelho D, Latini A, Llesuy S, Belló-Klein A, Giugliani R, Deon M, Mello CF (2004) Evidence that oxidative stress is increased in patients with X-linked adrenoleukodystrophy. Biochim Biophys Acta 1688:26–32
Wajner M, Coelho DM, Barschak AG, Araujo PR, Pires RF, Lulhier FL, Vargas CR (2000) Reduction of large neutral amino acid concentrations in plasma and CSF of patients with maple syrup urine disease during crises. J Inherit Metab Dis 23:505–512
Wajner M, Latini A, Wyse ATS, Dutra-Filho CS (2004) The role of oxidative damage in the neuropathology of organic acidurias: insights from animal studies. J Inherit Metab Dis 27:427–448
Yu TW, Ong CN (1999) Lag-time measurement of antioxidant capacity using myoglobin and 2,29-azino-bis(3-ethyl-benzthiazoline-6-sulfonic acid): rationale, application and limitation. Anal Biochem 275:217–223
Zielke HR, Huang Y, Tildon JT, Zielke CL, Baab PJ (1996) Elevation of amino acids in the interstitial space of the rat brain following infusion of large neutral amino and keto acids by microdialysis: leucine infusion. Dev Neurosci 18:420–425
Acknowledgements
This work was supported by grants from Brazilian National Research Council (CNPq), CAPES, FAPERGS, and FIPE/HCPA—Brazil.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barschak, A.G., Sitta, A., Deon, M. et al. Oxidative stress in plasma from maple syrup urine disease patients during treatment. Metab Brain Dis 23, 71–80 (2008). https://doi.org/10.1007/s11011-007-9077-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-007-9077-y