Abstract
Maple Syrup Urine Disease (MSUD) is a metabolic disorder caused by a severe deficiency of the branched-chain α-keto acid dehydrogenase complex activity which leads to the accumulation of branched-chain amino acids (BCAA) leucine (Leu), isoleucine and valine and their respective α-keto-acids in body fluids. The main symptomatology presented by MSUD patients includes ketoacidosis, failure to thrive, poor feeding, apnea, ataxia, seizures, coma, psychomotor delay and mental retardation, but, the neurological pathophysiologic mechanisms are poorly understood. The treatment consists of a low protein diet and a semi-synthetic formula restricted in BCAA and supplemented with essential amino acids. It was verified that MSUD patients present L-carnitine (L-car) deficiency and this compound has demonstrated an antioxidant and anti-inflammatory role in metabolic diseases. Since there are no studies in the literature reporting the inflammatory profile of MSUD patients and the L-car role on the inflammatory response in this disorder, the present study evaluates the effect of L-car supplementation on plasma inflammatory cytokines interleukin-1β (IL-1β), interleukin-6 (IL-6), interferon-gamma (INF-ɣ), and a correlation with malondialdehyde (MDA), as a marker of oxidative damage, and with free L-car plasma levels in treated MSUD patients. Significant increases of IL-1β, IL-6, and INF-ɣ were observed before the treatment with L-car. Moreover, there is a negative correlation between all cytokines tested and L-car concentrations and a positive correlation among the MDA content and IL-1β and IL-6 values. Our data show that L-car supplementation can improve cellular defense against inflammation and oxidative stress in MSUD patients and may represent an additional therapeutic approach to the patients affected by this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maple syrup urine disease (MSUD) is an inherited disorder caused by mutation in any of the 4 subunits (E1α, E1β, E2, E3) of the branched chain α-keto acid dehydrogenase (BCKAD) enzyme complex. Due to BCKAD deficiency high concentrations of the branched-chain amino acids (BCAA) leucine (Leu), valine and isoleucine as well as the respective branched chain α-keto acids (BCKA) α-ketoisocaproic (KIC), α-keto-β-methylvaleric and α-keto acids α-ketoisovaleric acids accumulate in patients on an unrestricted diet and during episodes of metabolic decompensation crisis (Chuang and Shih 2001; Chuang 1998). The worldwide frequency is approximately 1 in 180,000 newborns and patients can be divided into five phenotypes ranging from the classical form with a neonatal onset to milder variants with later onset (Chuang and Shih 2001).
The clinical features of classic MSUD include poor feeding, convulsions, failure to thrive, ketoacidosis, apnea, hypoglycemia, coma, ataxia, seizures, psychomotor delay and mental retardation. In addition, severe generalized brain edema, cerebral atrophy and hypomyelination are usually seen in MSUD patients, the mechanisms underlying brain damage is poorly known and needs to be exploited further explored (Chuang and Shih 2001; Schönberger et al. 2004). Literature has shown that Leu and its transamination product (KIC) are considered the main toxic metabolites to the central nervous system once their increased concentrations have been associated to the appearance of neurological symptoms (Chuang and Shih 2001; Hoffmann et al. 2006). Also, it has been demonstrated that the metabolites accumulated in MSUD can decrease neurotransmitter metabolism (Zielke et al. 1997; Tavares et al. 2000), leads to neuronal apoptosis (Jouvet et al. 2000), alter energy metabolism in rat brain (Sgaravatti et al. 2003; Ribeiro et al. 2008; Amaral et al. 2010), reduce the uptake of essential amino acids by brain tissue (Araújo et al. 2001) and can reduce the ability to also modulate the damage associated to increased free radical production (Bridi et al. 2003, 2005a; b; Fontella et al. 2002).
Therapy for MSUD comprises a lifelong strict and carefully adjusted semi-synthetic diet with widely restricted amounts of protein, with low BCAA supplemented with a formula of essential amino acids, vitamins and minerals (Frazier et al. 2014). The goal of treatment is to protect the brain from functional disturbances and structural damage by keeping the plasma branched-chain metabolites continually close to normal range (Strauss et al. 2010). However, it has been already verified that MSUD patients under treatment present a marked deficiency in antioxidants compounds and this may possibly be secondary to the protein restricted diet that implies in smaller amounts of these micronutrients (Barschak et al. 2007; Sitta et al. 2014). In this context, recently it was demonstrated that treated MSUD patients have L-carnitine deficiency, which can be obtained mainly from dietary protein supply (Mescka et al. 2013).
L-carnitine (L-car) or 3-hydroxy-4-methylammoniobutanoate regulates the flux substrate and energy balance across cell membranes by modulating both the transport of long-chain fatty acids into mitochondria and the subsequent β-oxidation. Foods of animal origin contain substantial amounts of L-car, but this compound is produced endogenously also in lesser amount using the amino acids lysine and methionine (Foster 2004). It has been demonstrated that L-car shows antioxidant capacity by reducing lipid peroxidation with a degree comparable to that observed with α-tocopherol and also an antioxidant protective role by scavenging reactive oxygen species as superoxide anion, hydrogen peroxide and by inhibiting hydroxyl radical formation in the Fenton reaction system (Gulcin 2006; Reznick et al. 1992). There has been an increased number of studies reporting interesting effects of L-car on cells of the immune system (Izgüt-Uysal et al. 2003; Pertosa et al. 2005; Szefel et al. 2012) and there are no data in the literature reporting the inflammatory profile of MSUD patients, much less the L-car role on the inflammatory response in this disorder. Hence, the present study was designed to investigate the effects of L-car supplementation on plasma inflammatory cytokines interleukin-1β (IL-1β), interleukin-6 (IL-6), interferon-gamma (IFN -ɣ), and malondialdehyde (MDA), as a marker of oxidative stress, in treated MSUD patients, as well as to establish a possible relation between this parameters.
Materials and methods
Patients and controls
The study was approved by the Ethics Committee of Hospital de Clínicas de Porto Alegre, RS, Brazil (project n° 140191). Informed consent was obtained according to the guidelines of our committee. Classical MSUD patients were recruited from the Medical Genetic Service of Hospital de Clínicas de Porto Alegre, Brazil. Plasma samples were obtained from seven MSUD patients under protein restricted diet protocol (mean age 8.28 ± 2.87 years) and six healthy individuals (control group) with comparable age and sex (mean age 6.0 ± 3.12 years). The main features of patients with MSUD at diagnosis were convulsions, ketoacidosis, poor feeding, hypoglycemia and psychomotor delay. Dietary treatment (median 0,95 year – range 15 days to 9,83 years) consisted of a protein-restricted diet supplemented with a semi-synthetic formula of essential amino acids, vitamins and minerals and not containing L-car (MSUD 1 or MSUD 2 Milupa1). Furthermore, for this study, MSUD patients were supplemented with L-car capsules, at a dose of 50 mg/kg/day, not exceeding 1.5 g/day for 2 months. Inflammatory cytokines, MDA and free L-car levels were analyzed in blood of MSUD patients before (No L-car) and after one (L-car 1) and 2 months (L-car 2) of L-car supplementation.
Biological sample collection and preparation
Blood samples from patients and controls were processed and stored by the same procedure. Blood samples from six age- and gender-matched controls (mean age 6.0 ± 3.12 years) were recruited anonymously from the laboratory of Faculdade de Farmácia da UFRGS, RS, Brazil. After venous puncture and collection in heparinized vials, plasma and cells were separated by centrifugation at 3,000 g for 10 min at 4 °C. Plasma was removed by aspiration and stored at −80 °C until further analysis.
Inflammatory cytokines measurement: IL-1β, IL-6, IFN -ɣ
Plasma IL-1β, IL-6 and IFN-ɣ were measured by enzyme-linked immunosorbent assay (ELISA) kits (Mabtech AB, Sweden). The assay utilizes ELISA strip plates pre-coated with a capture monoclonal antibody (mAb), to which samples are added. Captured cytokine is detected by adding a biotinylated mAb followed by streptavidin-horseradish peroxidase. Addition of the enzyme substrate TMB results in a colored substrate product. Intensity of the color is directly proportional to the concentration of cytokine in the sample, which is determined by comparison with a serial dilution of recombinant cytokine standard analyzed in parallel. The results were expressed as pg/mL.
MDA content
MDA was measured by following method described by Karatepe (2004). Briefly, 100 μL of plasma was mixed with 100 μL of 0.1 M perchloric acid and 1 mL of distilled water. The samples then were centrifugated at 1,500 g for 5 min and used for HPLC analysis. The column used was Supelcosil C18 (5 μm) 15 cm × 4.6 mm, the mobile phase was 82.5:17.5 (v/v) 30 mM monobasic potassium phosphate (pH 3.6)-methanol and the flow rate was 1.2 mL/min. The detection was monitored at 250 nm. The system was calibrated with a standard solution of MDA, which was used for quantification. Results were expressed in μmol/L of MDA.
Free L-car determination
Free L-car levels were determined in blood spots by liquid chromatography electrospray tandem mass spectrometry (LC/MS/MS), using the multiple reaction monitoring (MRM) mode (Chace et al. 1997). Results were reported in μmol/L.
Statistical analysis
Data were expressed as mean ± standard deviation. Comparison between means was analyzed for repeated measures of ANOVA followed by the Tukey multiple range test when the F value was significant. Correlations were carried out using the Pearson correlation coefficient. A p value lower than 0.05 was considered significant.
Results
In this study we evaluated the L-car supplementation effect on the inflammatory response in plasma from MSUD patients treated with a protein-restricted diet. The MSUD patients were divided into three groups: before supplementation with L-car (Group No L-car), after 1 month of L-car supplementation (L-car 1) and after 2 months of treatment with this compound (L-car 2). The MSUD patients under treatment (Group No L-car) have L-car deficiency compared to control group. After 1 month of L-car supplementation (L-car 1), the concentrations of this micronutrient have reached levels comparable to the control group (Control Group: 43.85 ± 8.89 μmol/L; Group No L-car: 24.28 ± 10.83 μmol/L; Group L-car 1: 49.01 ± 8.60 μmol/L; L-car 2: 53.18 ± 10.79 μmol/L) [F (3,22) = 6.253, p < 0.05]. The lipid peroxidation levels (measured as plasma malondialdehyde) were significantly elevated compared to controls and a reversal of lipid peroxidation to control levels occurred in 2 months of L-car therapy (Group L-car 2) (Control Group: 0.027 ± 0.003 μmol/L; Group No L-car: 0.087 ± 0.006 μmol/L; Group L-car 1: 0.038 ± 0.003 μmol/L; L-car 2: 0.035 ± 0.003 μmol/L) [F (3.29) = 19.541, p < 0.05] (Mescka et al. 2013).
Thereafter, we examined the L-car supplementation influence on the inflammatory profile in MSUD patients. It was found that MSUD patients (Group No L-car) have significantly increased pro-inflammatory cytokines levels compared to the control group. L-car supplementation (Group L-car 1 and Group L-car 2) induced a reversion of IL-1β [F (3,22) = 6.032, p < 0.05] and IFN-ɣ [F (3,24) = 10.84, p < 0.05] concentrations to control levels (Fig. 1a and b, respectively) and a reduction of IL-6 close to control levels [F (3,24) = 37.69, p < 0.05] (Fig. 1c).
a interleukin-1β (IL-1β), b interleukin-6 (IL-6), c interferon-gamma (IFN-ɣ) measurements in plasma of MSUD patients and controls. Group No L-car: patients before supplementation with L-car. Group L-car 1: patients after 1 month of L-car supplementation. Group L-car 2: patients after 2 months of L-car supplementation. Data represent the mean ± SD. Number of MSUD patients = 5–7. Number of controls = 6. * p < 0.05 compared to controls, # p < 0.05 compared to Group No L-car, # P < 0.05 compared to Group L-car 1 (Tukey multiple range test)
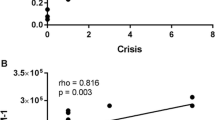
As it can be seen in Fig. 2, strongly significant inverse correlations between free L-car levels and IL-1β (r = −0.7505; p < 0.05, Fig. 2a), IL-6 (r = −0.8235; p < 0.05, Fig. 2b), and IFN-ɣ (r = −0.6279; p < 0.05, Fig. 2c) concentrations were observed, indicating a possible L-car anti-inflammatory role in the plasma of patients MSUD.
Lastly, we found significant positive correlations between MDA values and IL-1β (r = 0.6645; p < 0.05, Fig. 3a), IL-6 (r = 0.5197; p < 0.05, Fig. 3b) and IFN-ɣ did not show significant correlation with MDA concentrations (r = 0.1616; p > 0.05, Fig. 3c).
Discussion
Inflammation occurs in response to any alteration of tissue integrity, in order to restore tissue homeostasis through the induction of various repair mechanisms (Muriach et al. 2014). During this dysregulation of physiological functions, occurs a local and finally a systemic inflammation that is characterized by production of high levels of reactive oxygen species (ROS) and can leads to oxidative stress and damage of biomolecules, such as proteins, lipids and DNA (Brüne et al. 2013).
There are few studies that correlate inflammatory processes with MSUD. It has been shown that BCAAs are able to influence the immunological properties of microglia cell culture by changing the responsiveness to pro-inflammatory signals (De Simone et al. 2013). Furthermore, Scaini et al. (2014) suggest that this inflammatory process associated with high levels of BCAA may contribute to a blood brain barrier breakdown in patients MSUD and its can be related to the neurological dysfunction observed in this disorder. Clinically is well described that inflammatory process, such as infection, may often precipitate acute metabolic decompensation with complications in MSUD patients (Chuang and Shih 2001), but in the best of our knowledge there are no studies in the literature reporting the inflammatory profile of MSUD patients, much less the possible L-car role on the inflammatory response in this disorder.
Therefore, in our study, it was observed that MSUD patients in treatment with restricted protein diet and without L-car supplementation have high levels of pro-inflammatory cytokines IL-1β, IL-6 and IFN-ɣ in relation to the control group. After the beginning of L-car treatment, there was a significant decrease in the levels of these cytokines to concentrations similar to the control group, demonstrating that L-car was able to reverse the inflammatory process modulated by these cytokines. These pro-inflammatory cytokines are increased during immune activation and inflammation and can induce the production of oxidants, prostaglandins, and mitochondrial ROS by macrophages, thus contributing to inflammatory responses (Muralidharan and Mandrekar 2013). Macrophages and monocytes are the major source of IL-1β, molecule able to induce inflammatory and proapoptotic responses mediated by factors such as prostaglandins, ROS, inducible NO synthase, and NO. IL-6 is a pleiotropic cytokine that affects immune responses and antigen-specific inflammatory reactions being a major mediator of the acute phase inflammation and can be produced by several cell types, including T and B cells, monocytes, macrophages, fibroblasts and endothelial cells. The cytokine IFN-ɣ is mainly produced by T helper cell type 1 (Th1) lymphocytes, natural killer (NK) cells, B cells and NKT cells. During Th1-type response, IFN-ɣ is probably the most important trigger for high ROS production in macrophages by phagocytic NADPH oxidase (NOX).
There was also an inverse significant correlation between the inflammatory markers analyzed and the L-car concentrations, showing a possible anti-inflammatory effect of this compound, since L-car supplementation significantly decreased the inflammatory markers tested. Moreover, there was a positive significant correlation in plasma of MSUD patients between pro-inflammatory cytokines IL-1β and IL-6 and MDA values, the main marker of lipid peroxidation. These results evidence a possible direct relationship between inflammation and increased oxidative stress in MSUD patients.
Patients with inflammatory diseases usually exhibit antioxidants reduced levels, which might be due to insufficient nutritional intake or caused by an to increased antioxidant demand for oxidation due to continuous high levels ROS production by the activation of immune competent cells (Muñoz and Costa 2013; Mangge et al. 2014). Thus, the finding of an inverse correlation between L-car concentrations and inflammatory cytokines could be related to an insufficient dietetic supply of this compound and an increased requirement for antioxidant molecules during inflammatory episodes and this may contribute to decompensation metabolic crisis in MSUD patients.
L-car is considered nowadays one of the nutraceuticals that has pleiotropic crucial biologic effects. L-car deficiency may cause damage to cellular metabolism, which can be primary, as a result of defects in the specific transport of L-car into the cells, or secondary, as reported in some inborn errors of metabolism and acquired medical conditions such as organic aciduria, mitochondrial respiratory chain defects and methylenetetrahydrofolate reductase deficiency (Famularo and De Simone 1995; Shakeri et al. 2010; Ribas et al. 2014). Various pathological disorders including epilepsy, cirrhosis, malabsorption have been also associated with secondary L-car deficiency and oral dosage forms are nowadays approved by the US Food and Drug Administration for primary and secondary systemic L-car deficiency. Some unlabeled uses of this compound are for the treatment or prophylaxis of valproate toxicity, Alzheimer’s disease, muscle disorders, cardiovascular diseases, HIV infection, and male infertility (Hatamkhani et al. 2013).
The most important recognized functions of the L-car are transport of long-chain fatty acid across the inner mitochondrial membrane, where β-oxidation occurs, and the removal from the mitochondria of potentially toxic end-products of fatty acid metabolism. However, a series of studies have been performed to determine L-car effect on cells of the immune system. Several data indicate that L-car deficiency is a contributing factor to the progression of infection in patients with human immunodeficiency virus, and that L-car therapy in those patients could counteract the unregulated process of lymphocyte apoptosis and improve CD4 counts (Famularo et al. 2004). Izgüt-Uysal and colleagues (2003) demonstrate that L-car is capable to restore the age-related changes in the inflammatory cells functions and play a protective role in the tissue destruction in inflammation by decreasing the superoxide anion production. Other studies have shown that L-car has a therapeutic effect on morbidity and lipid metabolism in cachexia and septic shock rat models, and that these effects could be the result of down-regulation of cytokine production and/or increased clearance of cytokines (Winter et al. 1995). Regular L-car supplementation in hemodialysis patients demonstrated to increase cellular defense against chronic inflammation and oxidative stress, most likely by modulating the specific signal transduction cascade activated by an overproduction of pro-inflammatory cytokines and free radicals action (Pertosa et al. 2005).
Although the L-car actions in the brain are not yet fully established, in the last years studies in animals and cells have demonstrated numerous neuroprotective, neuromodulatory and neurotrophic properties of this compound (Ribas et al. 2014). However, there are no data in the literature showing an improvement in the clinical condition of MSUD patients supplemented with L-car, but there are few and recent reports of clinical improvement in other disorders. For instance, Cuturic et al. (2013) observed in Huntington’s disease, that the patients with low serum L-car levels who received low-dose of levocarnitine supplementation, during a mean period of 7.3 months, showed improvement in motor, cognitive and behavioral measures. They speculated that the observed clinical improvement is related with the resolution of reversible metabolic encephalopathy and myopathy associated with secondary carnitine deficiency. In a randomized, double-blind, placebo-controlled study, it was verified an improvement of cognitive deficits, the reduction of ammonia, and the modification of electroencephalogram analysis in treated L-car patients with severe hepatic encephalopathy (Malaguarnera et al. 2011a). The same research group also showed that acetyl-l-carnitine reduces depression and improves life quality in patients with minimal hepatic encephalopathy (Malaguarnera et al. 2011b).
L-car supplementation has been usually considered safe and with low risk of adverse effects, which makes it a promising candidate for the prevention and treatment of oxidative alterations in many diseases. Is important to emphasize that supplementation with L-car in MSUD patients of our study, who were deficient in L-car, was held for a period of 2 months, and perhaps the clinical improvement effects of the administration would be better evaluated in a long-term treatment. Moreover, it was verified a higher excretion of KIC, the major neurotoxic acid accumulated in this disorder, in the urine of MSUD patients treated with L-car, what reinforces the importance of this compound in the elimination of the toxic metabolites in these patients (Guerreiro et al. 2015). These findings may represent a new perspective for the use of L-car as a possible antioxidant adjunct treatment. For this purpose, we intended to do in a future a translational and clinical study to fully explore this potential.
Evidence accumulated over the past decades has pointed to significant connections between inflammation and oxidative stress, both processes contributing to fuel the other one, thereby establishing a vicious cycle able to perpetuate and propagate the inflammatory response (Lugrin et al. 2014). Taken together, these data highlight that the maintenance of normal L-car concentrations in MSUD patients could have an important role in inflammatory process. The L-car system seems to be a relevant endogenous physiologic mediator to protect against damage during the inflammatory response and the unregulated production of ROS can act as a major factor in triggering cell injury. This study showed a possible beneficial influence of L-car supplementation on immune system functions in MSUD patients. Furthermore, we suggest that L-car could be useful in MSUD therapy representing a new approach to the current treatment, which consists of protein restrict diet. Future studies will examine the mechanism of the reduction of cytokine levels by L-car determining whether L-car lowers its levels by increasing clearance, or by reducing production of cytokines in MSUD.
Abbreviations
- MSUD:
-
Maple syrup urine disease
- BCKAD:
-
Branched chain α-keto acid dehydrogenase
- BCAA:
-
Branched-chain amino acid
- Leu:
-
Leucine
- BCKA:
-
Branched chain α-keto acids
- KIC:
-
α-ketoisocaproic acid
- L-car:
-
L-carnitine
- IL-1β:
-
Interleukin-1β
- IL-6:
-
Interleukin-6
- IFN -ɣ:
-
Interferon-gamma
- MDA:
-
Malondialdehyde
- ROS:
-
Reactive oxygen species
References
Amaral AU, Leipnitz G, Fernandes CG et al (2010) Alpha-ketoisocaproic acid and leucine provokemitochondrial bioenergetic dysfunction in rat brain. Brain Res 1324:75–84
Araújo P, Wassermann GF, Tallini K et al (2001) Reduction of large neutral amino acid levels in plasma and brain of hyperleucinemic rats. Neurochem Int 38:529–537
Barschak AG, Sitta A, Deon M et al (2007) Erythrocyte glutathione peroxidase activity and plasma selenium concentration are reduced in maple syrup urine disease patients during treatment. Int J Dev Neurosci 25:335–338
Bridi R, Araldi J, Sgarbi M et al (2003) Induction of oxidative stress in rat brain by the metabolites accumulating in maple syrup urine disease. Int J Dev Neurosci 21:327–332
Bridi R, Latini A, Braum CA et al (2005a) Evaluation of the mechanisms involved in leucine-induced oxidative damage in cerebral cortex of young rats. Free Radic Res 39:71–79
Bridi R, Braun CA, Zorzi GK et al (2005b) a-Keto acids accumulating in maple syrup urine disease stimulate lipid peroxidation and reduce antioxidant defenses in cerebral cortex from young rats. Metab Brain Dis 20:155–167
Brüne B, Dehne N, Grossmann N et al (2013) Redox control of inflammation in macrophages. Antioxid Redox Signal 19:595–637
Chace DH, Hillman SL, Van Hove JL, Naylor EW (1997) Rapid diagnosis of MCAD deficiency: quantitative analysis of octanoylcarnitine and other acylcarnitines in newborn blood spots by tandem mass spectrometry. Clin Chem 43:2106–2113
Chuang DT (1998) Maple syrup urine disease: it has come a long way. J Pediatr 132:17–23
Chuang DT, Shih VE (2001) Maple syrup urine disease (branched- chain ketoaciduria). In: Scriver CR, Beaudt AL, Sly WL, Valle D (eds) The metabolic and molecular bases of inherited disease. McGraw-Hill, New York, pp 1971–2005
Cuturic M, Abramson RK, Moran RR et al (2013) Serum carnitine levels and levocarnitine supplementation in institutionalized Huntington’s disease patients. Neurol Sci 34:93–98
De Simone R, Vissicchio F, Mingarelli C et al (2013) Branched-chain amino acids influence the immune properties of microglial cells and their responsiveness to pro-inflammatory signals. Biochim Biophys Acta 1832:650–659
Famularo G, De Simone C (1995) A new era for carnitine? Immunol Today 16:211–213
Famularo G, De Simone C, Trinchieri V, Mosca L (2004) Carnitines and its congeners: a metabolic pathway to the regulation of immune response and inflammation. Ann N Y Acad Sci 1033:132–138
Fontella FU, Gassen E, Pulronik V et al (2002) Stimulation of lipid peroxidation in vitro in rat brain by the metabolites accumulating in maple syrup urine disease. Metab Brain Dis 17:47–54
Foster DW (2004) The role of the carnitine system in human metabolism. Ann NY Acad Sci 1033:1–16
Frazier DM, Allgeier C, Homer C et al (2014) Nutrition management guideline for maple syrup urine disease: an evidence- and consensus-based approach. Mol Genet Metab 112:210–217
Guerreiro G, Mescka CP, Sitta A et al (2015) Urinary biomarkers of oxidative damage in maple syrup urine disease: the l-carnitine role. Int J Dev Neurosci 42:10–14
Gulcin I (2006) Antioxidant and antiradical activities of L-carnitine. Life Sci 78:803–811
Hatamkhani S, Karimzadeh I, Elyasi S et al (2013) Carnitine and sepsis: a review of an old clinical dilemma. J Pharm Pharm Sci 16:414–423
Hoffmann B, Helbling C, Schadewaldt P, Wendel U (2006) Impact of longitudinal plasma leucine levels on the intellectual outcome in patients with classic MSUD. Pediatr Res 59:17–20
Izgüt-Uysal VN, Ağaç A, Derin N (2003) Effect of L-carnitine on carrageenan-induced inflammation in aged rats. Gerontology 49:287–292
Jouvet P, Rustin P, Taylor DL et al (2000) Branched chain amino acids induce apoptosis in neural cells without mitochondrial membrane depolarization or cytochrome c release: implications for neurological impairment associated with maple syrup urine disease. Mol Biol Cell 11:1919–1932
Karatepe M (2004) Simultaneous determination of ascorbic acid and free malondialdehyde in human serum by HPLC–UV. LCGC N Am 22:362–365
Lugrin J, Rosenblatt-Velin N, Parapanov R, Liaudet L (2014) The role of oxidative stress during inflammatory process. Biol Chem 395:203–230
Malaguarnera M, Vacante M, Motta M et al (2011a) Acetyl-L-carnitine improves cognitive functions in severe hepatic encephalopathy: a randomized and controlled clinical trial. Metab Brain Dis 26:281–289
Malaguarnera M, Bella R, Vacante M et al (2011b) Acetyl-L-carnitine reduces depression and improves quality of life in patients with minimal hepatic encephalopathy. Scand J Gastroenterol 46:750–759
Mangge H, Becker K, Fuchs D, Gostner JM (2014) Antioxidants: inflammation and cardiovascular disease. World J Cardiol 6:462–477
Mescka CP, Wayhs CA, Vanzin CS (2013) Protein and lipid damage in maple syrup urine disease patients: l-carnitine effect. Int J Dev Neurosci 31:21–24
Muñoz A, Costa M (2013) Nutritionally mediated oxidative stress and inflammation. Oxidative Med Cell Longev 2013:610950
Muralidharan S, Mandrekar P (2013) Cellular stress response and innate immune signaling: integrating pathways in host defense and inflammation. J Leukoc Biol 94:1167–1184
Muriach M, Flores-Bellver M, Romero FJ, Barcia JM (2014) Diabetes and the brain: oxidative stress, inflammation, and authophagy. Oxidative Med Cell Longev 2014:102158
Pertosa G, Grandaliano G, Simone S et al (2005) Inflammation and carnitine in hemodialysis patients. J Ren Nutr 15:8–12
Reznick AZ, Kagan VE, Ramsey R et al (1992) Antiradical effects in L-propionyl carnitine protection of the heart against ischemia-reperfusiom injury: the possible role of iron chelation. Arch Biochem Biophys 296:394–401
Ribas GS, Vargas CR, Wajner M (2014) L-carnitine supplementation as a potencial antioxidant therapy for inherited neurometabolic disorders. Gene 533:469–476
Ribeiro CA, Sgaravatti AM, Rosa RB et al (2008) Inhibition of brain energy metabolism by the branched-chain amino acids accumu- lating in maple syrup urine disease. Neurochem Res 33:114–124
Scaini G, Morais MO, Galant LS et al (2014) Coadministration of branched-chain amino acids and lipopolysaccharide causes matrix metalloproteinase activation and blood–brain barrier breakdown. Mol Neurobiol 50:358–367
Schönberger S, Schweiger B, Schwahn B et al (2004) Dysmyelination in the brain of adolescents and young adults with maple syrup urine disease. Mol Genet Metab 82:69–75
Sgaravatti AM, Rosa RB, Schuck PF et al (2003) Inhibition of brain energy metabolism by the α-keto acids accumulating in maple syrup urine disease. Biochim Biophys Acta 1639:232–238
Shakeri A, Tabibi H, Hedayati M (2010) Effects of L-carnitine supplement on serum inflammatory cytokines, C-reactive protein, lipoprotein (a), and oxidative stress in hemodialysis patients with Lp (a) hyperlipoproteinemia. Hemodial Int 14:498–504
Sitta A, Ribas GS, Mescka CP et al (2014) Neurological damage in MSUD: the role of oxidative stress. Cell Mol Neurobiol 34:157–165
Strauss KA, Wardley B, Robinson D et al (2010) Classical maple syrup urine disease and brain development: principles of management and formula design. Mol Genet Metab 99:333–345
Szefel J, Kruszzewski WJ, Ciesielski M et al (2012) L-carnitine and cancer cachexia. II. Effects of lipid emulsion used in total parenteral nutrition on parameters of hemostasis and inflammatory state in L-carnitine deficiency in myocytes. Oncol Rep 28:324–329
Tavares RG, Santos CE, Tasca CI et al (2000) Inhibition of glutamate uptake into synaptic vesicles of rat brain by the metabolites accumulating in maple syrup urine disease. J Neurol Sci 181:44–49
Winter BK, Fiskum G, Gallo LL (1995) Effects of L-carnitine on serum triglyceride and cytokine levels in rat models of cachexia and septic shock. Br J Cancer 72:1173–1179
Zielke HR, Huang Y, Baab PJ et al (1997) Effect of alpha-ketoisocaproate and leucine on the in vivo oxidation of glutamate and glutamine in the rat brain. Neurochem Res 22:1159–1164
Acknowledgments
Very special thanks are dedicated to the physicians at the Medical Genetic Service of Hospital de Clinicas de Porto Alegre, families and patients who participated in this study. This work was supported in part by grants from FAPERGS, CNPq and FIPE/HCPA-Brazil.
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mescka, C.P., Guerreiro, G., Donida, B. et al. Investigation of inflammatory profile in MSUD patients: benefit of L-carnitine supplementation. Metab Brain Dis 30, 1167–1174 (2015). https://doi.org/10.1007/s11011-015-9686-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-015-9686-9