Abstract
Vascular endothelial cell growth factor-C (VEGF-C) is a member of the VEGF family and plays a role in various biological activities. VEGF-C enhances proliferation and migration of lymphatic endothelial cells and vascular endothelial cells through VEGF receptor 2 (VEGFR2) and/or receptor 3 (VEGFR3), and thereby induces lymphangiogenesis or angiogenesis. However, it remains unclear whether VEGF-C promotes the migration of mesenchymal stem cells (MSCs). Here, we investigated the effects of VEGF-C on the migration of MSCs and evaluated the underlying molecular mechanisms. VEGF-C treatment significantly induced the migration of MSCs, which is accompanied by the promotion of actin cytoskeletal reorganization and focal adhesion assembly. VEGF-C treatment enhanced the phosphorylation of VEGFR2 and VEGFR3 proteins in MSCs, and pretreatment with VEGFR2 and VEGFR3 kinase inhibitors effectively suppressed the VEGF-C-induced MSC migration. In addition, VEGF-C treatment promoted phosphorylation of ERK and FAK proteins in MSCs, and inhibition of VEGFR2 and VEGFR3 signaling pathways abolished the VEGF-C-induced activation of ERK and FAK proteins. Furthermore, treatment with ERK and FAK inhibitors suppressed VEGF-C-induced actin cytoskeletal reorganization and focal adhesion assembly, and then significantly inhibited MSCs migration. These results suggest that VEGF-C-induced MSC migration is mediated via VEGFR2 and VEGFR3, and follows the activation of the ERK and FAK signaling pathway. Thus, VEGF-C may be valuable in tissue regeneration and repair in MSC-based therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, stem cell therapy has been anticipated as a new strategy for regenerative medicine. Bone marrow-derived mesenchymal stem cells (MSCs) are multipotent cells that can differentiate into osteoblasts, chondrocytes, adipocytes, and smooth muscle cells [1]; therefore, MSCs are a promising cell source for regeneration and repair of damaged tissues. MSCs are known to migrate to injury sites after transplantation, and they differentiate into various cell types in the local environments [2]. However, previous studies reported that large proportions of transplanted MSCs were unable to reach the injury site [3, 4], or some of the transplanted MSCs dislodged from the transplanted site [5], and these problems may lead to limited therapeutic effect. Therefore, enhancing the migration capacity of MSCs will promote regeneration and repair of damaged tissues.
Previous studies have demonstrated that various cytokines such as stromal cell derived factor-1 (SDF-1), basic fibroblast growth factor (bFGF), and platelet-derived growth factor BB (PDGF-BB) enhance the migration of MSCs [6, 7]. Vascular endothelial growth factor (VEGF) is a key regulator of angiogenesis through proliferation and migration of vascular endothelial cells [8]. The VEGF family consists of seven members: VEGF-A, VEGF-B, VEGF-C, VEGF-D, VEGF-E, VEGF-F, and the placental growth factor (PlGF). These VEGF ligands bind with specific tyrosine kinase receptors (VEGFR1, VEGFR2, and VEGFR3). While several studies have demonstrated that VEGF-A promotes MSC migration [9], the effect of other VEGF members has not been fully elucidated.
VEGF-C is well known to promote proliferation and migration of lymphatic endothelial cells, and is a key regulator for lymphangiogenesis [10]. Previous studies have demonstrated that VEGF-C signaling participates in various biological processes besides lymphangiogenesis, such as neural stem cell activation, and promotion of osteoclastic bone resorption [11, 12]. Recently, we also reported that VEGF-C promotes osteogenic differentiation of MSCs [13].
Cell migration is a complex and multi-step process that requires the ordered changes in the cytoskeleton and turnover of focal adhesions [14]. It has been reported that several intracellular signaling pathways participate in the cell migration process [15,16,17]. Focal adhesion kinase (FAK) is a nonreceptor cytoplasmic tyrosine kinase that plays an important role in the regulation of cell migration [18]. FAK is a primary signaling mediator of dynamic changes in actin cytoskeletal reorganization, and FAK activation is necessary for focal adhesion turnover [19,20,21]. Mitogen-activated protein kinase (MAPK) signaling also plays an important role in various cell migration [17]. Extracellular signal-regulated kinase (ERK1/2), c-Jun N-terminus kinase (JNK), and stress activated protein-kinase 2 (p38) are the members of the classical MAP kinase cascade [22]. In MSCs, ERK signaling is involved in MSCs migration [23]. In our previous study, we had demonstrated that VEGF-C induces the phosphorylation of ERK protein in MSCs [13]. Previously, some studies reported that VEGF-C promoted the migration of human and murine MSC lines [24, 25]. However, the mechanisms of VEGF-C-induced MSCs migration are not fully understood. In this study, we examined the effects of VEGF-C on migration of MSCs and evaluated the underlying molecular mechanisms.
Materials and methods
Materials
Recombinant human VEGF-C protein was obtained from Wako (Osaka, Japan). VEGF receptor 2 kinase inhibitor (Ki8751), VEGF receptor 3 kinase inhibitor (MAZ51), and MAP kinase inhibitor (U0126) were purchased from Calbiochem/Merck Millipore (San Diego, CA, USA). FAK inhibitor (PF-573228) was obtained from Sigma (St Louis, MO, USA).
Cell culture
Human MSCs were purchased from Lonza (Walkersville, MD, USA). MSCs were cultured in α-minimal essential medium (MEM) supplemented with 10% fetal bovine serum (FBS), and 1% antibiotics (Life Technologies, Waltham, MA, USA) at 37 °C, 5% CO2. Cells between passage 3 and 5 were used for the experiments.
Migration assay
Migration assay was performed with transwell 24-well tissue culture plates composed of a polycarbonate membrane with 8 µm pores (Corning, NY, USA). MSCs were seeded on the inner chamber of the transwell plate at a concentration of 1 × 105 cells/100 µL. In some experiments, MSCs were pretreated with Ki8751 (10 nM), MAZ51 (5 µM), U0126 (10 µM), or PF-573228 (10 µM) for 1 h. The inner chamber was placed into the outer chamber filled with 600 µL serum-free α-MEM that contained VEGF-C (1–50 ng/mL) or saline and incubated for 6 h at 37 °C. Cells that migrated onto the outer surface of the membrane were fixed with 4% paraformaldehyde and cold methanol, and then stained by the May-Giemsa method. The number of migrated cells was counted in five randomly chosen fields of the triplicated chambers at a magnification of × 10 for each sample.
Immunoblotting analysis
MSCs were treated with VEGF-C (10 ng/mL) or saline for indicated times and were lysed in RIPA lysis buffer (ThermoFisher Scientific, Rockford, IL, USA). Cell lysates were subjected to immunoblotting. In some experiments, MSCs were pretreated with Ki8751 (10 nM), MAZ51 (5 µM), U0126 (10 µM), or PF-573228 (10 µM) at 37 °C for 1 h. The following antibodies were used: anti-VEGF receptor 2, anti-phospho-VEGF receptor 2 (Tyr1175), anti-phospho-ERK (Thr202/Tyr204), anti-ERK, anti-phospho-JNK (Thr183/Tyr185), anti-JNK, anti-phospho-p38 (Thr180/Tyr182), anti-p38, anti-phospho-FAK (Tyr397), anti-FAK, and anti-β-actin (Cell Signaling Technology, Danvers, MA, USA); anti-VEGF receptor 3 (Abcam, Cambridge, UK); anti-phospho-VEGF receptor 3 (Tyr1230/1231) antibody (Cell applications, San Diego, CA, USA). Horseradish peroxidase (HRP)-conjugated anti-rabbit IgG and enhanced chemiluminescence (ECL) system were obtained from GE Healthcare (Buckinghamshire, UK).
Immunofluorescent staining
Before the experiment, MSCs were placed in serum-free α-MEM for 15 h for serum starvation and then the cells were treated with VEGF-C (10 ng/mL) or saline for 2 h. In some experiments, MSCs were pretreated with U0126 (10 µM) or PF-573228 (10 µM) at 37 °C for 1 h. After that, cells were washed with PBS and fixed with 4% paraformaldehyde for 15 min and permeabilized with cold methanol at -20 °C for 15 min. After washing with PBS, cells were incubated with 0.1% Triton X-100 and 1% BSA in PBS for 1 h. Afterwards, the cells were stained with Alexa Fluor 488 phalloidin (Molecular Probes, Eugene, OR) and anti-paxillin antibody (BD Biosciences, Franklin Lakes, NJ, USA), and nuclei were stained with the DNA binding dye 4, 6-diamino-2-phenylindole (DAPI) (Dojindo, Kumamoto, Japan) for 10 min.
Statistical analysis
The data are presented as mean ± SD values. Statistical analysis for multiple comparisons among the groups was performed using one-way ANOVA. p < 0.05 was considered to indicate a statistically significant difference.
Results
VEGF-C promotes MSC migration, and regulates actin cytoskeletal reorganization and focal adhesion assembly
To evaluate whether VEGF-C induces MSC migration, MSCs were treated with VEGF-C (1–50 ng/mL) or saline for control. Treatment with VEGF-C promoted MSCs migration (Fig. 1a). Quantitative analysis demonstrated that VEGF-C significantly induced MSC migration in a dose-dependent manner. We used 10 ng/mL VEGF-C in subsequent experiments.
VEGF-C promotes MSCs migration, and regulates actin cytoskeletal reorganization and focal adhesion assembly. a Representative photomicrographs of migrating MSCs treated with VEGF-C (1–50 ng/mL) or saline for 6 h. Migrating cells were counted in five fields randomly chosen from the triplicated chambers. Results are presented as mean ± S.D.; *p < 0.05 versus 0 ng/mL; scale bar 20 µm. b Immunofluorescent microscopic analysis for F-actin filament formation and paxillin accumulation in MSCs treated with or without VEGF-C (10 ng/mL) for 2 h. Staining with phalloidin (green), anti-paxillin antibody (red), and DAPI (blue); scale bar 20 µm. (Color figure online)
Cell migration is a complex process that requires cytoskeletal dynamics and reorganization, and turnover of focal adhesions [14]. We evaluated whether VEGF-C treatment regulates actin cytoskeletal organization and assembly of focal adhesions in MSCs. Phalloidin staining revealed that treatment with 10 ng/mL VEGF-C promotes F-actin filament formation in MSCs (Fig. 1b). Staining with antibody against paxillin, a focal adhesion-associated protein, showed that VEGF-C treatment promoted paxillin accumulation in MSCs (Fig. 1b).
VEGF-C induces MSC migration in a VEGFR2 and VEGFR3-dependent manner
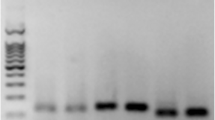
VEGF-C signaling is mediated through activation of specific transmembrane tyrosine kinase receptors VEGFR2 and VEGFR3 [10]. We, therefore, assessed the participation of VEGFR2 and/or VEGFR3 signaling in the observed VEGF-C-induced migration of MSCs. Treatment with 10 ng/mL VEGF-C stimulated the phosphorylation of both VEGFR2 and VEGFR3 proteins in MSCs, while there was no effect on total VEGFR2 and VEGFR3 protein levels (Fig. 2a). We next investigated whether VEGFR2 and VEGFR3 signaling pathway is involved in VEGF-C-induced migration of MSCs. MSCs were treated with VEGFR2 kinase inhibitor (Ki8751) or VEGFR3 kinase inhibitor (MAZ51), and then MSC migration was measured. Treatment with Ki8751 and MAZ51 significantly inhibited VEGF-C-induced MSC migration (Fig. 2b).
Involvement of VEGFR2 and VEGFR3 signaling in the VEGF-C-induced MSC migration. a Immunoblotting with the indicated antibodies was performed on MSCs treated with VEGF-C (10 ng/mL) for the indicated times. Representative blots are shown. b Effects of VEGFR2 and VEGFR3 kinase inhibitors on VEGF-C-induced MSCs migration. MSCs were pretreated with Ki8751 (10 nM) or MAZ51 (5 µM) for 1 h, and then treated with VEGF-C (10 ng/mL) for 6 h (n = 3). The migration assay was performed. Representative photomicrographs are shown. Migrating cells were counted in five fields randomly chosen from the triplicated chambers. Results are presented as mean ± SD; *p < 0.05 versus VEGF-C(−)/Ki8751(−)/MAZ51(−), #p < 0.05 versus VEGF-C(+)/Ki8751(−)/MAZ51(−); scale bar 20 µm
VEGF-C activates ERK and FAK signaling in MSCs
Previous studies have shown that VEGF-C binds to VEGFR2 and VEGFR3, which is induced following autophosphorylation of VEGFR2 and VEGFR3, and then activates various downstream signaling pathways such as phosphatidylinositol 3-kinase (PI3K)/Akt, mitogen activated protein kinase (MAPK), and focal adhesion kinase (FAK), which are involved in the regulation of lymphatic endothelial cells proliferation and migration [10, 26, 27]. We, therefore, examined the signaling pathways that are involved in the VEGF-C-induced MSC migration. Treatment with VEGF-C increased phosphorylation of ERK and FAK proteins in MSCs (Fig. 3a), while there was no effect on activation of JNK and p38 proteins. Treatment with VEGF-C had no effect on total ERK, FAK, JNK, and p38 protein levels.
VEGF-C activates ERK and FAK signaling in a VEGFR2 and VEGFR3 dependent manner. a Immunoblotting with indicated antibodies was performed on MSCs treated with VEGF-C (10 ng/mL) for the indicated times. Representative blots are shown. b Effects of VEGFR2 and VEGFR3 kinase inhibitors on VEGF-C-induced phosphorylation of ERK and FAK. MSCs were pretreated with Ki8751 (10 nM) or MAZ51 (5 µM) for 1 h, and then treated with VEGF-C (10 ng/mL) or saline for 10 min. Relative phosphorylation levels were normalized to the total protein signal. Results are presented as mean ± SD. (n = 3); *p < 0.05 versus VEGF-C(−)/Ki8751(−)/MAZ51(−), #p < 0.05 versus VEGF-C(+)/Ki8751(−)/MAZ51(−)
To further investigate the involvement of VEGFR2 and VEGFR3 signaling in the VEGF-C-induced activation of ERK and FAK proteins, MSCs were treated with Ki8751 and MAZ51, and then the phosphorylation of ERK and FAK was assessed. Treatment with both Ki8751 and MAZ51 effectively suppressed the phosphorylation of ERK and FAK proteins (Fig. 3b).
Involvement of ERK and FAK signaling in VEGF-C mediated MSCs migration
It is well known that ERK and FAK signaling pathway plays a critical role in regulating various cell migration [17, 19,20,21]. To further investigate whether ERK and FAK signaling pathway participates in VEGF-C-induced MSC migration, MSCs were treated with ERK inhibitor (U0126) and FAK inhibitor (PF573228). Treatment with U0126 and PF573228 significantly suppressed VEGF-C-induced phosphorylation of ERK and FAK proteins (Fig. 4a). Interestingly, treatment with PF573228 inhibited phosphorylation of ERK protein, whereas, U0126 did not affect the phosphorylation level of FAK protein. We next examined the effect of ERK and FAK signaling inhibition on the VEGF-C-induced MSCs migration. Treatment with U0126 and PF573228 suppressed VEGF-C-induced actin cytoskeletal reorganization and paxillin accumulation in MSCs (Fig. 4b). In addition, pretreatment with U0126 and PF573228 significantly attenuated VEGF-C-induced MSC migration (Fig. 4c).
Involvement of ERK and FAK signaling in VEGF-C-induced MSCs migration. a Effects of ERK and FAK inhibitors on VEGF-C-induced phosphorylation of ERK and FAK. MSCs were pretreated with U0126 (10 µM) or PF-573228 (10 µM) for 1 h, and treated with VEGF-C (10 ng/mL) or saline for 10 min. Relative phosphorylation levels were normalized to the total protein signal. Results are presented as mean ± SD. (n = 3); *p < 0.05 versus VEGF-C(−)/U0126(−)/PF-573228(−), #p < 0.05 versus VEGF-C(+)/U0126(−)/PF-573228(−). b Effects of ERK and FAK inhibitors on VEGF-C-induced actin cytoskeletal reorganization and paxillin accumulation. MSCs were pretreated with U0126 (10 µM) or PF-573228 (10 µM) for 1 h, and then treated with VEGF-C (10 ng/mL) or saline for 2 h. Immunofluorescent microscopic analysis for F-actin filament formation and paxillin accumulation. Staining with phalloidin (green), anti-paxillin antibody (red), and DAPI (blue); scale bar 20 µm. c Effects of ERK and FAK inhibitors on VEGF-C-induced MSCs migration. MSCs were pretreated with U0126 (10 µM) or PF-573228 (10 µM) for 1 h, and then treated with VEGF-C (10 ng/mL) or saline for 6 h. Representative photomicrographs are shown. Migrating cells were counted in five fields randomly chosen from the triplicated chambers. Results are presented as mean ± SD.; *p < 0.05 versus VEGF-C(−)/U0126(−)/PF-573228(−), #p < 0.05 versus VEGF-C(+)/U0126(−)/PF-573228(−). scale bar 20 µm. (Color figure online)
Discussion
In the present study, we have demonstrated that VEGF-C induces actin cytoskeletal reorganization and focal adhesion assembly, leading to the promotion of MSCs migration.
It is well known that MSCs secrete a variety of cytokines and growth factors that show therapeutic effect for various damaged tissues [28, 29]. Accumulating evidence suggests that MSCs mediate their therapeutic effects primarily through a paracrine mechanism [30, 31]. Therefore, the appropriate homing of MSCs to the injured area is an essential step to enhance the therapeutic effects. A better understanding of the molecular mechanisms that regulate the MSCs migration, will play an important role for the improvement of therapeutic benefit.
Recently, we had reported that MSCs secrete VEGF-A, but not VEGF-C in normal culture conditions [13]. Previous report showed that MSCs did not secrete VEGF-C in normoxic culture conditions, but VEGF-C secretion was induced by near anoxia (0.1% O2) conditions [32]. Furthermore, another report indicated that VEGF-C expression was slightly increased at later stages of osteogenic differentiation in preosteoblast-like cells [33]. In the present study, we performed all experiments using undifferentiated MSCs at normoxic and normal culture conditions. Therefore, the observed VEGF-C-induced MSC migration was possibly promoted by exogenously added VEGF-C. However, in the present study, we did not investigate whether VEGF-C treatment promotes autocrine secretion of VEGF-C in MSCs, and thus further studies may be needed to elucidate this issue.
It is well established that VEGF-C promotes proliferation and migration of lymphatic endothelial cells, and thereby induces lymphangiogenesis [10]. In lymphatic endothelial cells, VEGF-C binds and activates two related receptor tyrosine kinases, VEGFR2 and VEGFR3, which are induced during several signal transduction pathways such as ERK, p38, Akt, and FAK [10, 34]. Previous studies have reported that VEGFR2 and VEGFR3 are expressed in human and murine MSCs [13, 25, 35]. Consistent with these observations, VEGFR2 and VEGFR3 expression were confirmed in the MSCs used in this study, and treatment with VEGF-C induced phosphorylation of VEGFR2 and VEGFR3. Furthermore, inhibition of VEGFR2 and VEGFR3 signaling by Ki8751 and MAZ51 significantly suppressed VEGF-C-induced MSC migration, indicating that VEGF-C-induced MSC migration is dependent on both VEGFR2 and VEGFR3 signaling pathway.
Previous studies had reported that VEGF-C promoted migration of human and murine MSC lines [24, 25], but the underlying molecular mechanisms were not fully identified. It has been reported that the coordination of actin cytoskeletal changes and focal adhesion turnover is essential for various cell migration [14]. In our study, treatment with VEGF-C promoted F-actin filament formation and paxillin accumulation in MSCs. These findings indicate that VEGF-C-induced MSC migration is regulated by cytoskeletal rearrangement and focal adhesion formation.
We have shown that the treatment with VEGF-C activates ERK and FAK signaling in MSCs; however, there was no effect on activation of JNK and p38. It is well established that ERK and FAK signaling is involved in MSC migration process [23]. Treatment with Ki8751 and MAZ51 effectively abrogated VEGF-C-induced phosphorylation of ERK and FAK. These results indicate that VEGF-C-induced phosphorylation of ERK and FAK is mediated via both VEGFR2 and VEGFR3-dependent signaling. Furthermore, treatment with U0126 and PF573228 suppressed VEGF-C-induced actin cytoskeletal reorganization and paxillin accumulation, and thereby suppressed MSC migration. These results demonstrate that VEGF-C-induced MSC migration is mediated by the activation of ERK and FAK dependent signaling pathway.
Activation of FAK stimulates several signal transduction pathways such as Ras/MEK/ERK and PI3K/Akt pathways [36]. In the present study, we found that the treatment with PF573228 inhibited not only VEGF-C-induced phosphorylation of FAK but also phosphorylation of ERK. These results indicated that FAK may be an upstream effector to ERK signaling in VEGF-C-induced MSC migration. Consistent with our data, previous studies also have shown that PF573228 treatment suppressed phosphorylation of ERK protein in various cells [37,38,39]. Furthermore, it has been reported that transfection with shRNA targeting FAK decreased phosphorylation of ERK protein in the distracted callus [40]. Src tyrosine kinase is known to play critical roles in cell migration. A previous study indicated that Src-induced the phosphorylation of FAK, and subsequently activated downstream ERK signaling, and thereby promoted cell migration [41]. Recently, it has been reported that VEGF-C promotes macrophage migration via Src signaling activation [42]. These results indicate that Src signaling may be involved in the VEGF-C-induced MSC migration. Further studies may be needed to elucidate this issue. To understand precise mechanisms of VEGF-C-induced MSC migration, these possibilities need to be investigated in the future.
In conclusion, our data demonstrate that VEGF-C-induced MSC migration is mediated through ERK and FAK signaling dependent mechanism. These findings suggest that VEGF-C might be employed in regenerative therapeutic strategies to enhance various tissue repair.
References
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284(5411):143–147
Barry FP, Murphy JM (2004) Mesenchymal stem cells: clinical applications and biological characterization. Int J Biochem Cell Biol 36(4):568–584. https://doi.org/10.1016/j.biocel.2003.11.001
Pittenger MF, Martin BJ (2004) Mesenchymal stem cells and their potential as cardiac therapeutics. Circ Res 95(1):9–20. https://doi.org/10.1161/01.RES.0000135902.99383.6f95/1/9
Zhang M, Methot D, Poppa V, Fujio Y, Walsh K, Murry CE (2001) Cardiomyocyte grafting for cardiac repair: graft cell death and anti-death strategies. J Mol Cell Cardiol 33(5):907–921. https://doi.org/10.1006/jmcc.2001.1367S0022-2828(01)91367-7
Quintavalla J, Uziel-Fusi S, Yin J, Boehnlein E, Pastor G, Blancuzzi V, Singh HN, Kraus KH, O’Byrne E, Pellas TC (2002) Fluorescently labeled mesenchymal stem cells (MSCs) maintain multilineage potential and can be detected following implantation into articular cartilage defects. Biomaterials 23(1):109–119
Liu X, Duan B, Cheng Z, Jia X, Mao L, Fu H, Che Y, Ou L, Liu L, Kong D (2011) SDF-1/CXCR4 axis modulates bone marrow mesenchymal stem cell apoptosis, migration and cytokine secretion. Protein Cell 2(10):845–854. https://doi.org/10.1007/s13238-011-1097-z
Ozaki Y, Nishimura M, Sekiya K, Suehiro F, Kanawa M, Nikawa H, Hamada T, Kato Y (2007) Comprehensive analysis of chemotactic factors for bone marrow mesenchymal stem cells. Stem Cells Dev 16(1):119–129. https://doi.org/10.1089/scd.2006.0032
Herbert SP, Stainier DY (2011) Molecular control of endothelial cell behaviour during blood vessel morphogenesis. Nat Rev Mol Cell Biol 12(9):551–564. https://doi.org/10.1038/nrm3176
Wang H, Wang X, Qu J, Yue Q, Hu Y, Zhang H (2015) VEGF enhances the migration of MSCs in neural differentiation by regulating focal adhesion turnover. J Cell Physiol 230(11):2728–2742. https://doi.org/10.1002/jcp.24997
Deng Y, Zhang X, Simons M (2015) Molecular controls of lymphatic VEGFR3 signaling. Arterioscler Thromb Vasc Biol 35(2):421–429. https://doi.org/10.1161/ATVBAHA.114.304881
Han J, Calvo CF, Kang TH, Baker KL, Park JH, Parras C, Levittas M, Birba U, Pibouin-Fragner L, Fragner P, Bilguvar K, Duman RS, Nurmi H, Alitalo K, Eichmann AC, Thomas JL (2015) Vascular endothelial growth factor receptor 3 controls neural stem cell activation in mice and humans. Cell Rep 10(7):1158–1172. https://doi.org/10.1016/j.celrep.2015.01.049
Zhang Q, Guo R, Lu Y, Zhao L, Zhou Q, Schwarz EM, Huang J, Chen D, Jin ZG, Boyce BF, Xing L (2008) VEGF-C, a lymphatic growth factor, is a RANKL target gene in osteoclasts that enhances osteoclastic bone resorption through an autocrine mechanism. J Biol Chem 283(19):13491–13499. https://doi.org/10.1074/jbc.M708055200
Murakami J, Ishii M, Suehiro F, Ishihata K, Nakamura N, Nishimura M (2017) Vascular endothelial growth factor-C induces osteogenic differentiation of human mesenchymal stem cells through the ERK and RUNX2 pathway. Biochem Biophys Res Commun 484(3):710–718. https://doi.org/10.1016/j.bbrc.2017.02.001
Friedl P, Wolf K (2009) Proteolytic interstitial cell migration: a five-step process. Cancer Metastasis Rev 28(1–2):129–135. https://doi.org/10.1007/s10555-008-9174-3
Chen BH, Tzen JT, Bresnick AR, Chen HC (2002) Roles of Rho-associated kinase and myosin light chain kinase in morphological and migratory defects of focal adhesion kinase-null cells. J Biol Chem 277(37):33857–33863. https://doi.org/10.1074/jbc.M204429200
Jimenez C, Portela RA, Mellado M, Rodriguez-Frade JM, Collard J, Serrano A, Martinez AC, Avila J, Carrera AC (2000) Role of the PI3K regulatory subunit in the control of actin organization and cell migration. J Cell Biol 151(2):249–262
Huang C, Jacobson K, Schaller MD (2004) MAP kinases and cell migration. J Cell Sci 117(Pt 20):4619–4628. https://doi.org/10.1242/jcs.01481
Zhao X, Guan JL (2011) Focal adhesion kinase and its signaling pathways in cell migration and angiogenesis. Adv Drug Deliv Rev 63(8):610–615. https://doi.org/10.1016/j.addr.2010.11.001
Abedi H, Zachary I (1997) Vascular endothelial growth factor stimulates tyrosine phosphorylation and recruitment to new focal adhesions of focal adhesion kinase and paxillin in endothelial cells. J Biol Chem 272(24):15442–15451
Hu Y, Lu J, Xu X, Lyu J, Zhang H (2017) Regulation of focal adhesion turnover in SDF-1alpha-stimulated migration of mesenchymal stem cells in neural differentiation. Sci Rep 7(1):10013. https://doi.org/10.1038/s41598-017-09736-7
Hu YL, Lu S, Szeto KW, Sun J, Wang Y, Lasheras JC, Chien S (2014) FAK and paxillin dynamics at focal adhesions in the protrusions of migrating cells. Sci Rep 4:6024. https://doi.org/10.1038/srep06024
Zhang W, Liu HT (2002) MAPK signal pathways in the regulation of cell proliferation in mammalian cells. Cell Res 12(1):9–18. https://doi.org/10.1038/sj.cr.7290105
Gao H, Priebe W, Glod J, Banerjee D (2009) Activation of signal transducers and activators of transcription 3 and focal adhesion kinase by stromal cell-derived factor 1 is required for migration of human mesenchymal stem cells in response to tumor cell-conditioned medium. Stem Cells 27(4):857–865. https://doi.org/10.1002/stem.23
Conrad C, Niess H, Huss R, Huber S, von Luettichau I, Nelson PJ, Ott HC, Jauch KW, Bruns CJ (2009) Multipotent mesenchymal stem cells acquire a lymphendothelial phenotype and enhance lymphatic regeneration in vivo. Circulation 119(2):281–289. https://doi.org/10.1161/CIRCULATIONAHA.108.793208
Igarashi Y, Chosa N, Sawada S, Kondo H, Yaegashi T, Ishisaki A (2016) VEGF-C and TGF-beta reciprocally regulate mesenchymal stem cell commitment to differentiation into lymphatic endothelial or osteoblastic phenotypes. Int J Mol Med 37(4):1005–1013. https://doi.org/10.3892/ijmm.2016.2502
Coso S, Zeng Y, Opeskin K, Williams ED (2012) Vascular endothelial growth factor receptor-3 directly interacts with phosphatidylinositol 3-kinase to regulate lymphangiogenesis. PLoS ONE 7(6):e39558. https://doi.org/10.1371/journal.pone.0039558
Yang WH, Chang AC, Wang SW, Wang SJ, Chang YS, Chang TM, Hsu SK, Fong YC, Tang CH (2016) Leptin promotes VEGF-C production and induces lymphangiogenesis by suppressing miR-27b in human chondrosarcoma cells. Sci Rep 6:28647. https://doi.org/10.1038/srep28647
Kuo TK, Hung SP, Chuang CH, Chen CT, Shih YR, Fang SC, Yang VW, Lee OK (2008) Stem cell therapy for liver disease: parameters governing the success of using bone marrow mesenchymal stem cells. Gastroenterology 134(7):2111–2121. https://doi.org/10.1053/j.gastro.2008.03.015
Cai M, Shen R, Song L, Lu M, Wang J, Zhao S, Tang Y, Meng X, Li Z, He ZX (2016) Bone marrow mesenchymal stem cells (BM-MSCs) improve heart function in swine myocardial infarction model through paracrine effects. Sci Rep 6:28250. https://doi.org/10.1038/srep28250
Yao Y, Huang J, Geng Y, Qian H, Wang F, Liu X, Shang M, Nie S, Liu N, Du X, Dong J, Ma C (2015) Paracrine action of mesenchymal stem cells revealed by single cell gene profiling in infarcted murine hearts. PLoS ONE 10(6):e0129164. https://doi.org/10.1371/journal.pone.0129164
Gnecchi M, He H, Melo LG, Noiseaux N, Morello F, de Boer RA, Zhang L, Pratt RE, Dzau VJ, Ingwall JS (2009) Early beneficial effects of bone marrow-derived mesenchymal stem cells overexpressing Akt on cardiac metabolism after myocardial infarction. Stem Cells 27(4):971–979. https://doi.org/10.1002/stem.12
Paquet J, Deschepper M, Moya A, Logeart-Avramoglou D, Boisson-Vidal C, Petite H (2015) Oxygen tension regulates human mesenchymal stem cell paracrine functions. Stem Cells Transl Med 4(7):809–821. https://doi.org/10.5966/sctm.2014-0180
Deckers MM, Karperien M, van der Bent C, Yamashita T, Papapoulos SE, Lowik CW (2000) Expression of vascular endothelial growth factors and their receptors during osteoblast differentiation. Endocrinology 141(5):1667–1674. https://doi.org/10.1210/endo.141.5.7458
Iwasaki T, Takeda Y, Maruyama K, Yokosaki Y, Tsujino K, Tetsumoto S, Kuhara H, Nakanishi K, Otani Y, Jin Y, Kohmo S, Hirata H, Takahashi R, Suzuki M, Inoue K, Nagatomo I, Goya S, Kijima T, Kumagai T, Tachibana I, Kawase I, Kumanogoh A (2013) Deletion of tetraspanin CD9 diminishes lymphangiogenesis in vivo and in vitro. J Biol Chem 288(4):2118–2131. https://doi.org/10.1074/jbc.M112.424291
Sorrentino A, Ferracin M, Castelli G, Biffoni M, Tomaselli G, Baiocchi M, Fatica A, Negrini M, Peschle C, Valtieri M (2008) Isolation and characterization of CD146 + multipotent mesenchymal stromal cells. Exp Hematol 36(8):1035–1046. https://doi.org/10.1016/j.exphem.2008.03.004
Cao W, Zheng W, Chen T (2015) Ruthenium polypyridyl complex inhibits growth and metastasis of breast cancer cells by suppressing FAK signaling with enhancement of TRAIL-induced apoptosis. Sci Rep 5:9157. https://doi.org/10.1038/srep09157
Aksamitiene E, Achanta S, Kolch W, Kholodenko BN, Hoek JB, Kiyatkin A (2011) Prolactin-stimulated activation of ERK1/2 mitogen-activated protein kinases is controlled by PI3-kinase/Rac/PAK signaling pathway in breast cancer cells. Cell Signal 23(11):1794–1805. https://doi.org/10.1016/j.cellsig.2011.06.014
Sun J, Luo Q, Liu L, Song G (2018) Low-level shear stress promotes migration of liver cancer stem cells via the FAK-ERK1/2 signalling pathway. Cancer Lett 427:1–8. https://doi.org/10.1016/j.canlet.2018.04.015
Yanoshita M, Hirose N, Okamoto Y, Sumi C, Takano M, Nishiyama S, Asakawa-Tanne Y, Horie K, Onishi A, Yamauchi Y, Mitsuyoshi T, Kunimatsu R, Tanimoto K (2018) Cyclic tensile strain upregulates pro-inflammatory cytokine expression via FAK-MAPK signaling in chondrocytes. Inflammation 41(5):1621–1630. https://doi.org/10.1007/s10753-018-0805-8
Song J, Ye B, Liu H, Bi R, Zhang N, Hu J, Luo E (2018) Fak-Mapk, Hippo and Wnt signalling pathway expression and regulation in distraction osteogenesis. Cell Prolif 51(4):e12453. https://doi.org/10.1111/cpr.12453
Westhoff MA, Serrels B, Fincham VJ, Frame MC, Carragher NO (2004) SRC-mediated phosphorylation of focal adhesion kinase couples actin and adhesion dynamics to survival signaling. Mol Cell Biol 24(18):8113–8133. https://doi.org/10.1128/MCB.24.18.8113-8133.2004
Deng Y, Yang Y, Yao B, Ma L, Wu Q, Yang Z, Zhang L, Liu B (2018) Paracrine signaling by VEGF-C promotes non-small cell lung cancer cell metastasis via recruitment of tumor-associated macrophages. Exp Cell Res 364(2):208–216. https://doi.org/10.1016/j.yexcr.2018.02.005
Acknowledgements
This work was in part supported by Grant-in Aid for Scientific Research B (Grant No. 17H04394), and Grant-in Aid for Scientific Research C (Grant No. 15K11169).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Ishii, M., Takahashi, M., Murakami, J. et al. Vascular endothelial growth factor-C promotes human mesenchymal stem cell migration via an ERK-and FAK-dependent mechanism. Mol Cell Biochem 455, 185–193 (2019). https://doi.org/10.1007/s11010-018-3481-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-018-3481-y