Abstract
Chlamydia trachomatis, the most common human pathogen that causes trachoma and sexually transmitted disease, has developed various strategies for inhibiting host cell apoptosis. Activation of the PI3K (phosphoinositide 3-kinase)/AKT-mediated MDM2 (murine double minute 2)-p53 pathway plays a prominent role in the apoptosis resistance arising from C. trachomatis infection. However, the precise upstream mechanisms by which C. trachomatis activates this pathway have not been adequately investigated. Here, we reveal that the secreted C. trachomatis plasmid-encoded protein Pgp3 inhibits apoptosis in HeLa cells. This process requires the activation of the PI3K/AKT signaling pathway, thereby leading to phosphorylation and nuclear entry of MDM2, and p53 degradation. PI3 K inhibitor LY294002 and MDM2 inhibitor Nutlin-3a block Pgp3-induced inhibition of HeLa cell apoptosis, suggesting a critical role for the PI3K/AKT pathway and its effect on the MDM2-p53 axis in Pgp3 anti-apoptotic activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chlamydia trachomatis is a common, obligate intracellular, gram-negative bacterial pathogen that causes various widespread diseases threatening human health [1]. It is the predominant sexually transmitted bacterial pathogen and is also the causative agent of trachoma, which can lead to blindness [2]. Most C. trachomatis infection is asymptomatic and can therefore easily lead to chronic, persistent sequelae, including pelvic inflammatory disease, infertility and ectopic pregnancy [3]. Moreover, there is a correlation between C. trachomatis and human papillomavirus infection and coinfection with both pathogens increasing the risk of cervical cancer [4].
Chlamydia trachomatis has a unique life cycle that begins with the invasion of host cells by infectious elementary bodies (EBs). These EBs are engulfed in a membrane-bound vacuole and differentiate into non-infectious and propagative reticulate bodies (RBs), which then re-differentiate into EBs and initiate a new cycle following host cell lysis or exocytosis [1]. To successfully replicate in this way, and to develop a persistent infection in the host, chlamydia must modulate cell apoptosis to escape host immune clearance. Chlamydia has developed various strategies to inhibit both the intrinsic and extrinsic pathways of host cell apoptosis [5]. The intrinsic apoptosis pathway is governed by the Bcl-2 (B cell lymphoma 2) protein family, which consists of three subfamilies that differ in function and their complement of protein homology domains: the pro-survival proteins, which include Bcl-2, Mcl-1, A1, and Bcl-xL, have three to four BH (Bcl-2 homology) domains; the pro-apoptosis Bax family, which includes Bax and Bak, have three BH domains; and the BH3-only proteins, which include Bid, Bik, and Puma, possess a single BH domain, as their name suggests [6]. Among these proteins, Bax and Bak have a decisive effect on mitochondrial outer membrane permeability, resulting in the release of cytochrome c. which then forms a complex with apoptotic protease-activating factor (Apaf-1), leading to the formation of caspase 9-associated apoptosome, followed by activation of the downstream effector caspase 3, which is responsible for cleavage of intracellular proteins that eventually lead to apoptosis. The anti-apoptotic Bcl-2 proteins can antagonize Bax/Bak activation and thereby inhibit apoptosis [7, 8]. Chlamydia promotes inhibition of pro-apoptotic proteins Bax and Bak and activation of anti-apoptotic Bcl-2, resulting in the blockage of mitochondrial cytochrome c release and inhibition of caspase activation, which ultimately lead to inhibition of apoptosis [5, 9].
The tumor suppressor protein p53 is involved in the determination of cell cycle arrest and cell death, as well as the response to cellular stressors such as DNA damage. In its role as a transcription factor, p53 controls the expression of several apoptosis genes, including Bax, Puma, Apaf-1, and Bcl-2 [10]. A recent study found that infection with various chlamydia species activates the MDM2-p53 axis, leading to p53 degradation. Inhibition of this pathway impairs both the development of chlamydia and its anti-apoptotic effect [11]. Siegl et al. [12] emphasized that p53 represses glucose-6-phosphate dehydrogenase, a key enzyme of the pentose phosphate pathway, which is necessary for chlamydial growth. They also found that the PI3K/AKT pathway plays a crucial role in activating the MDM2-p53 axis, but precisely how C. trachomatis regulates the PI3K/AKT pathway remains unclear.
Many C. trachomatis strains share a 7.5-kb cryptic plasmid that encodes eight open reading frames (ORFs), designated pORF1 to 8, and that significantly promotes chlamydial infection and pathogenicity [13]. Among these pORFs, pORF5, which is also known as Pgp3, is the only plasmid-encoded protein to be secreted from the bacterium and is therefore mainly distributed in the cytosol of chlamydia-infected cells [14]. More importantly, it has been demonstrated that Pgp3 is a major virulence factor and promotes chlamydial ascension and tubal inflammation [15]. Recently, our research group found that Pgp3 can induce production of pro-inflammatory cytokines via the TLR2 (Toll-like receptor 2) signaling pathway and by NALP3 inflammasome activation, suggesting that Pgp3 can manipulate host signaling pathways [16, 17].
Here, we investigated the role of Pgp3 in the regulation of apoptosis in host cells and found that it can block the intrinsic pathway. This is mediated by the activation of the PI3K/AKT signaling pathway, which is necessary for phosphorylation and nuclear entry of MDM2, and subsequent degradation of p53.
Methods and materials
Cell culture and stimulation
HeLa 229 cells (ATCC) were maintained in DMEM medium (HyClone) containing 10% fetal bovine serum (Gibco) in an incubator at 37 °C, 5% CO2. Expression and purification of Pgp3 protein were performed as previously described [16]. For the stimulation experiments, HeLa cells were grown in 6-well plates (Corning) at a density of 1–5 × 106/well or in 24-well plates (Corning) at a density of 1–5 × 105/well. The medium was then replaced by serum-free medium, followed by addition of Pgp3 at different concentrations for various time periods. For certain inhibitor incubation experiments, HeLa cells were pre-treated with a specific inhibitor or DMSO as control for 1 h before Pgp3 stimulation. The inhibitors used were LY294002 (#9901, Cell Signaling) and Nutlin-3a (N6287, Sigma).
Western blotting
HeLa cells were grown in 6-well plates at a density of 1–5 × 106/well. Each cell sample was washed three times in cold PBS. Proteins were extracted using RIPA lysis buffer (50 mM Tris pH 7.4, 150 mM NaCl, 1% sodium deoxycholate, 1% Triton X-1000, 1% SDS) supplemented with 1 mM protease inhibitor (phenylmethanesulfonyl fluoride; Beyotime) for 30 min on ice and protein concentration was measured by BCA protein assay (Beyotime). Protein samples were transferred onto PVDF membranes (Millipore) after separation by 12% SDS-PAGE gel electrophoresis and blocked in 5% non-fat milk diluted in TBS containing 0.1% Tween-20 for 2 h at room temperature. Membranes were incubated with diluted antibodies at 4 °C overnight. The following monoclonal antibodies were used: anti-Bax (#5023, Cell signaling), anti-Bcl-2 (#2870, Cell signaling), anti-p53 (#2527, Cell signaling), anti-Caspase 3(#9662, Cell signaling), anti-p-AKT (#4060, Cell signaling), anti-AKT (#4691, Cell signaling), anti-p-MDM2 (ab170880, Abcam), anti-MDM2 (ab178938, Abcam), and anti-GAPDH (Proteintech). Bound antibodies were revealed with HRP anti-rabbit secondary antibody and an ECL detection kit (Thermo).
Hoechst staining
HeLa cells were seeded in 24-well plates at 80% confluence prior to stimulation with Pgp3 or treatment with TNF-α (Sigma). Each group was washed three times in cold PBS and fixed with 4% paraformaldehyde (Beyotime) for 30 min at 4 °C. After permeabilization with 0.1 Triton X-100 for 5 min, cells were stained with 10 μM nucleic acid dye Hoechst 33342 at 37 °C for 20 min and washed three times in PBS. Nuclear morphology was viewed under a fluorescence microscope (×200). Five fields were randomly selected, and total cell nuclei and apoptosis-positive cells were counted.
Indirect immunofluorescence
Cells were grown on glass coverslips in 24-well plates at a density of 2–5 × 105/well. After experimental treatment, cells were washed three times with PBS and fixed with 4% paraformaldehyde for 30 min at 4 °C, permeabilized with 0.1 Triton X-100 for 5 min, then incubated with 2.5% BSA in PBS at 37 °C for 2 h. Cells were sequentially probed with diluted primary antibodies at 4 °C overnight, washed three times, and incubated with Cy-3 secondary antibody (Proteintech) and diluted nucleic acid dye DAPI (Sigma) mixture for 1 h at 37 °C. The cells were examined by fluorescence microscopy (200×).
Flow cytometry
Cell death was measured by flow cytometry using an annexin V-APC/7-AAD apoptosis kit (Multi Sciences). HeLa cells were grown according to manufacturer guidelines in 6-well plates at a density of 1–3 × 106/well. After experimental treatment, cell samples were washed twice with cold PBS and resuspended in 1× Binding Buffer, followed by incubation with annexin V-APC and 7-AAD, while controls were incubated only with annexin V-APC or 7-AAD. After 15 min in the dark at room temperature, 380 μl 1× Binding Buffer was added to each group and cells were analyzed by flow cytometry (BD FACSCalibur).
Statistical analysis
Data are shown as the mean ± standard deviation (SD) of three independent experiments. Statistically significant differences were assessed using the χ2 test of the SPSS-13.0 software package. p < 0.05 was considered statistically significant.
Results
Pgp3 inhibits host cell apoptosis
Chlamydia trachomatis has evolved many strategies to inhibit host cell apoptosis, including the inhibition of pro-apoptotic protein Bax and activation of anti-apoptotic protein Bcl-2, which results in cytochrome c release from the mitochondria and consequent activation of caspases [18]. To ask whether chlamydial secretion protein Pgp3 interrupts host cell apoptosis, we evaluated the expression of Bax and Bcl-2 after stimulation of HeLa cells with Pgp3 at different concentrations and for various time periods. As shown in Fig. 1a, Pgp3 began to inhibit HeLa cell apoptosis at a concentration of 10 μg/ml, with the effect becoming very clear at 15 μg/ml. Therefore, a concentration of 15 μg/ml was used to stimulate HeLa cells for various time periods, and showed that Pgp3 conferred resistance to apoptosis from 8 h, with the greatest effect at 24 h. Caspase 3 is thought to be an essential effector of cell death, and its activation is inhibited by chlamydial intracellular infection [9]. We further evaluated the caspase 3 enzymatic activity by measuring the level of Cleaved Caspase-3, after stimulation of HeLa cells with Pgp3 at 15 μg/ml and for 24 h, the expression of Cleaved Caspase-3 was down-regulated (Fig. 1b). We used a Hoechst stain to examine the nuclear morphology of HeLa cells after 24 h Pgp3 treatment, with positive cells showing a strong blue fluorescence; this revealed karyopyknosis and nuclear fragmentation, where present. In the TNF-α-treated positive control group, the apoptosis rate was 16.55%, while the rate was 10.53% in the PBS-treated control group. In contrast, the apoptosis rate in the Pgp3-treated group was much lower, at 4.4% (Fig. 1c). Consistent with the above results, flow cytometry suggested that Pgp3 treatment led to minimal cell death, the percentage of early- and late-stage apoptosis was 3.859%, while the apoptosis rate of the TNF-α-treated positive control group was 31.2%, and the apoptosis rate of the mock group was 12.336% (Fig. 1d). The above results suggest that Pgp3 inhibits apoptosis in HeLa cells in a dose- and time-dependent manner.
Pgp3 inhibits apoptosis in HeLa cells. a Serum-starved HeLa cells were stimulated with Pgp3 at different concentrations for 24 h or at 15 μg/ml for different time periods. Bax and Bcl-2 expression were determined by Western blotting. GAPDH served as loading control. b Serum-starved HeLa cells were stimulated with Pgp3 at 15 μg/ml for 24 h. Cleaved Caspase-3 and Caspase 3 were determined by Western blotting. GAPDH served as loading control. c Serum-starved HeLa cells were stimulated with Pgp3 at 15 μg/ml for 24 h. PBS was added to the control group, and positive controls were treated with 50 μM TNF-α for 4 h. Apoptotic cells, with apoptotic body formation or nuclear fragmentation, were measured by Hoechst staining under fluorescence microscopy (×200). Five different fields were counted randomly, with the bars representing the apoptosis rate (apoptotic cells/total cells) for each group. These data represent the results of three independent experiments. d Serum-starved HeLa cells were stimulated with Pgp3 at 15 μg/ml for 24 h. PBS was added to the control group, and positive controls were treated with 50 μM TNF-α for 4 h. Annexin 7AAD/V-APC was used with flow cytometry to assess the apoptosis status of the cell cultures. The upper- and lower-left quadrants represent dead and live cells, respectively, while the upper- and lower-right quadrants represent late- and early-stage apoptotic cells, respectively. These data represent three independent experiments
Pgp3-mediated anti-apoptosis depends on activation of the PI3K-AKT pathway
The PI3K/AKT pathway has a significant role in the resistance to apoptosis of host cells infected with C. trachomatis [14] and therefore we investigated whether Pgp3 activates this pathway. Significantly, Pgp3 increased the phosphorylation of AKT within 15–30 min post-stimulation, which then declined at 60 min, while the total AKT protein level was almost unchanged (Fig. 2a). To test whether AKT phosphorylation was PI3K-dependent, HeLa cells were pre-treated with selective PI3K inhibitor LY294002 (20 μM) to block PI3K kinase-dependent AKT phosphorylation. We found that phosphorylation of AKT was inhibited by this treatment (Fig. 2b), showing that Pgp3 does indeed activate the PI3K/AKT pathway. To further determine whether activation of the PI3K/AKT signaling pathway is involved in Pgp3-mediated resistance to apoptosis, the expression of Bax and Bcl-2 was tested after PI3K inhibition. Pre-treatment of HeLa cells with PI3K inhibitor LY294002 clearly led to an increase in Bax and a decrease in Bcl-2 levels (Fig. 2c). Flow cytometry revealed a significant increase in apoptotic cells in the LY294002 treatment group, in which the apoptosis rate was 11.59%, while that of the control group was 3.178% (Fig. 2d). Together, these results show that the PI3K/AKT pathway plays an important role in Pgp3-mediated anti-apoptosis in HeLa cells.
Activation of PI3K-AKT pathway in Pgp3-mediated anti-apoptosis in HeLa cells. a Serum-starved HeLa cells were stimulated with 15 μg/ml Pgp3 for different time periods. Western blotting shows the time course of phosphorylation of AKT, as well as total AKT and GAPDH in cells. b Serum-starved HeLa cells were pre-treated with 20 μM LY294002 or DMSO for 1 h, followed by incubation with 15 μg/ml Pgp3 for 30 min. Western blotting shows phosphorylated AKT, total AKT, and GAPDH. c Serum-starved HeLa cells were pre-treated with 20 μM LY294002 or DMSO for 1 h, followed by incubation with 15 μg/ml Pgp3 for 24 h. Western blotting shows the expression of Bax and Bcl-2. GAPDH served as loading control. d Serum-starved HeLa cells were pre-treated with 20 μM LY294002 or DMSO for 1 h and then stimulated with 15 μg/ml Pgp3 for 24 h. Annexin 7AAD/V-APC was used with flow cytometry to assess the apoptosis status of the cell cultures. The upper- and lower-left quadrants represent dead and live cells, respectively, while the upper- and lower-right quadrants represent late- and early-stage apoptotic cells, respectively. These data represent three independent experiments
Pgp3 induces phosphorylation and nuclear localization of MDM2 and decreases p53 expression
Activation of the PI3K/AKT pathway promotes the phosphorylation and nuclear entry of MDM2, and thus results in degradation of p53 [19]. To further determine the downstream effectors of the PI3K/AKT-dependent pathway that regulate Pgp3-mediated anti-apoptosis, we used Western blotting to monitor MDM2 phosphorylation at Ser166, which is necessary for its entry into the nucleus [19]. Following Pgp3 stimulation, phosphorylation of MDM2 increased from 15 to 30 min, and then decreased at 60 min (Fig. 3a). Indirect immunofluorescence was performed on serum-starved HeLa cells treated with Pgp3, in which DAPI was used to detect the cell nucleus, and the red fluorescent dye Cy3 was used to stain endogenous MDM2 (Fig. 3b). In contrast to the control group, MDM2 was located in the nucleus of HeLa cells in the presence of Pgp3, and this localization was blocked by LY294002. In the nucleus, MDM2 ubiquitinates and mediates nuclear export of p53, thus leading to its degradation [20]. We used immunoblotting to show that p53 levels decreased in a dose- and time-dependent manner upon Pgp3 stimulation (Fig. 3c). To further determine whether both p-MDM2 and p53 were regulated in a PI3K/AKT-dependent fashion, we showed that pre-treatment of HeLa cells with LY294002 increased p53 expression (Fig. 3d). These results demonstrate that Pgp3 activates the PI3K/AKT-mediated MDM2-p53 axis.
Pgp3 activates the MDM2-p53 axis. a Serum-starved HeLa cells were stimulated with 15 μg/ml Pgp3 for various times. Western blotting revealed phosphorylated and total MDM2, with GAPDH as loading control. b Serum-starved HeLa cells were pre-treated with 20 μM LY294002 or DMSO for 1 h and then stimulated with 15 μg/ml Pgp3 for 30 min. Fluorescence microscopy was used to determine the localization of MDM2. c Serum-starved HeLa cells were stimulated with Pgp3 at various concentrations for 24 h or at 15 μg/ml for various time periods. Western blotting revealed the expression of p53, with GAPDH serving as loading control. d Serum-starved HeLa cells were pre-treated with 20 μM LY294002 or DMSO for 1 h and then stimulated with 15 μg/ml Pgp3 for 24 h. Expression of p53 was determined by Western blotting, with GAPDH serving as loading control. These data represent the results of three independent experiments
Blocking the MDM2-p53 axis interrupts Pgp3-mediated apoptosis resistance
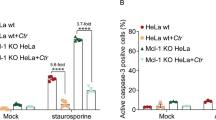
Nutlin-3a is a specific inhibitor which stabilizes p53 by disrupting MDM2-p53 interaction [21]. To examine the effects of MDM2-p53 axis on Pgp3-regulated p53 and apoptosis resistance, HeLa cells were pre-treated with 10 or 20 μM Nutlin-3a prior to stimulation with Pgp3. As shown in Fig. 4a, 20 μM Nutlin-3a was enough to reverse Pgp3-regulated p53. As expected, 20 μM Nutlin-3a was also sufficient to abolish Pgp3-mediated resistance to apoptosis in HeLa cells (Fig. 4b). Hoechst staining revealed a significant increase in apoptotic cells in the Nutlin-3a treatment group, in which the apoptosis rate was 12.77%, while that of the control group was 2.3% (Fig. 4c). Flow cytometry revealed a significant increase in apoptotic cells in the Nutlin-3a treatment group, in which the apoptosis rate was 12.05%, while that of the control group was 2.655% (Fig. 4d). In summary, these data suggest that the MDM2-p53 loop is involved in Pgp3-mediated anti-apoptotic activity.
Involvement of the MDM2-p53 pathway in Pgp3-mediated apoptosis resistance. a Serum-starved HeLa cells were pre-treated with 10 μM or 20 μM Nutlin-3a or DMSO for 1 h and then stimulated with 15 μg/ml Pgp3 for 24 h. The levels of p53 were determined by Western blotting, with GAPDH as loading control. b Serum-starved HeLa cells were pre-treated with 10 or 20 μM Nutlin-3a or DMSO for 1 h and then stimulated with 15 μg/ml Pgp3 for 24 h. Levels of Bax, Bcl-2, Cleaved Caspase-3, and Caspase 3 were determined by Western blotting, with GAPDH as loading control. c Serum-starved HeLa cells were pre-treated with 10 and 20 μM Nutlin-3a or DMSO for 1 h and then stimulated with 15 μg/ml Pgp3 for 24 h. Apoptotic cells, with apoptotic body formation or nuclear fragmentation, were counted by fluorescence microscopy (×200) after Hoechst staining. Five different fields were randomly counted, with the bars in the graph representing the apoptosis rate (apoptotic cells/total cells) of each group. d Serum-starved HeLa cells were pre-treated with 20 μM Nutlin-3a or DMSO for 1 h and then stimulated with 15 μg/ml Pgp3 for 24 h. Annexin 7AAD/V-APC was used with flow cytometry to assess the apoptosis status of the cell cultures. The upper- and lower-left quadrants represent dead and live cells, respectively, while the upper- and lower-right quadrants represent late- and early-stage apoptotic cells, respectively. These data represent three independent experiments
Discussion
Most C. trachomatis serovars carry a 7.5 kb cryptic plasmid, and plasmid-free variants have significantly attenuated pathogenicity in the mouse model, suggesting that this plasmid acts as a virulence factor [22]. The roles of plasmid-encoded pORFs in chlamydial infection have been extensively explored. Thus, pORF1 (Pgp7) and pORF2 (Pgp8) are involved in plasmid replication; pORF3 (Pgp1) and pORF4 (Pgp2) are essential for plasmid maintenance; pORF6 (Pgp4) is a master regulator of many chlamydial genes; while pORF7 (Pgp5) and pORF8 (Pgp6) participate in the regulation of partitioning and copy number [23, 24]. The protein featured in this work, pORF5, or Pgp3, is the only secreted plasmid-encoded protein and it is distributed throughout the cytosol of the infected host cell [14]. Pgp3 is a key virulence factor in C. muridarum (a model for studying C. trachomatis pathogenesis) and it promotes both chlamydial ascension and induction of tubal inflammation [25]. Pgp3 has also proved effective as a vaccine antigen in mice challenged with C. trachomatis [26]. Therefore, understanding the precise molecular pathogenic mechanisms of Pgp3 will lead to new possibilities for the prevention and treatment of C. trachomatis infection.
Apoptosis, a form of programmed cell death that is necessary for cellular homoeostasis, is also a means of removing microbial pathogens [27]. Apoptosis can be induced via three pathways: the extrinsic pathway (the death receptor pathway), the intrinsic pathway (the mitochondrial pathway), and the granzyme B/perforin pathway [28]. As an obligate intracellular human pathogen, chlamydia inhibits both the intrinsic and extrinsic apoptosis pathways, and thus promotes host cell survival and allows chronic infections to become established [5]. Mechanisms by which apoptosis can be inhibited include activation of the ERK mitogen-activated protein kinase [29], inhibition of mitochondrial cytochrome c release, and upregulation of IAPs (inhibitor of apoptosis proteins) [30]. However, how chlamydia manipulates host signaling pathways at the molecular level is only partially understood. Zhong [31] has reviewed the evidence showing that C. trachomatis can secrete effectors into infected cells to manipulate host signaling pathways. For example, a secreted serine protease, CPAF (chlamydia proteasome/protease-like activity factor), is distributed in the host cytosol [31] and can degrade pro-apoptotic BH3-only proteins to inhibit apoptosis [32]. As a protein that is secreted from the chlamydial cell into the host cytosol, the distribution of Pgp3 is similar to that of CPAF. Intriguingly, purified Pgp3 can induce the production of pro-inflammatory cytokines by manipulating the pattern recognition receptor TLR2 (Toll-like receptor 2) and the NALP3 (Natch domain, leucine-rich repeat, and PYD-containing protein 3) inflammasome in macrophages [16, 17]. Together, these studies indicate that Pgp3 can regulate host signaling pathways, but whether Pgp3 regulates apoptosis in this way was unclear prior to the current investigation. Here we showed that Pgp3 downregulates pro-apoptotic protein Bax and upregulates anti-apoptotic protein Bcl-2 and thereby inhibits host cell apoptosis in a dose- and time-dependent manner. Both proteins are involved in controlling the release of cytochrome c from mitochondria [33]. Moreover, we also showed that Pgp3 inhibits the effector caspase 3 activation, and therefore our data indicate that Pgp3 inhibits apoptosis via the intrinsic pathway in HeLa cells.
The PI3K/AKT pathway is involved in multiple cellular processes, including anti-apoptosis, cell survival, and differentiation and the pathway is inextricably linked with migration, adhesion, and angiogenesis of cancer cells [34]. Upon activation, PI3K produces phosphatidylinositol (3,4,5)-trisphosphate, which recruits AKT to the plasma membrane, where it is activated by phosphorylation at Ser473. AKT, also known as protein kinase B, has multiple downstream targets, resulting in phosphorylation of IKK kinase (a modulator of NF-κB) and mTOR (mammalian target of rapamycin), modulation of p21, p27, and MDM2 activity, suppression of Bad pro-apoptotic activity, and so on [35, 36]. Chlamydia infection results in persistent activation of the PI3K/AKT pathway, which in turn promotes chlamydial replication [37]. Targeted activation of the AKT pathway by C. trachomatis is an efficient strategy for stabilizing anti-apoptotic Mcl-1 and maintaining bad phosphorylation, thereby inhibiting host cell apoptosis [14]. Chlamydia induces AKT phosphorylation at Ser473, and activated p-AKT triggers MDM2 phosphorylation and nuclear entry, resulting in decreased levels of p53 [19]. In line with these results, we found that Pgp3 also induces phosphorylation and translocation of MDM2, which leads to degradation of p53 in a dose- and time-dependent manner. Treatment with specific PI3K inhibitor LY294002 leads to inhibition of the PI3K/AKT pathway and blockage of the downstream MDM2-p53 axis, ultimately reversing Pgp3-mediated resistance to apoptosis. Consistent with the above, the MDM2 inhibitor Nutlin-3a abrogated the effect of Pgp3 on p53 levels and restored apoptotic activity. These results show that the PI3K/AKT-mediated MDM2-p53 pathway plays a pivotal role in Pgp3-induced apoptosis resistance.
In conclusion, this study demonstrates that C. trachomatis plasmid-encoded virulence factor Pgp3 has an inhibitory effect on the intrinsic pathway of apoptosis in HeLa cells, which is mediated by activation of the classical MDM2-p53 axis and is dependent on the PI3K/AKT signaling pathway. Additional research into the molecular mechanisms of Pgp3 function may provide further important insights into chlamydial pathogenicity and improve the diagnosis, treatment, and prevention of C. trachomatis infection.
References
Bebear C, de Barbeyrac B (2009) Genital chlamydia trachomatis infections. Clin Microbiol Infect 15(1):4–10
Belland R, Ojcius DM, Byrne GI (2004) Chlamydia. Nat Rev Microbiol 2(7):530–531
Budrys NM, Gong S, Rodgers AK, Wang J, Louden C, Shain R, Schenken RS, Zhong G (2012) Chlamydia trachomatis antigens recognized in women with tubal factor infertility, normal fertility, and acute infection. Obstet Gynecol 119(5):1009–1016
Zhu H, Shen Z, Luo H, Zhang W, Zhu X (2016) Chlamydia Trachomatis infection-associated risk of cervical cancer: a meta-analysis. Medicine 95(13):e3077
Byrne GI, Ojcius DM (2004) Chlamydia and apoptosis: life and death decisions of an intracellular pathogen. Nat Rev Microbiol 2(10):802–808
Hardwick JM, Soane L (2013) Multiple functions of BCL-2 family proteins. Cold Spring Harb Perspect Biol 5(2):a008722
Czabotar PE, Lessene G, Strasser A, Adams JM (2014) Control of apoptosis by the BCL-2 protein family: implications for physiology and therapy. Nat Rev Mol Cell Bio 15(1):49–63
Adams JM (2003) Ways of dying: multiple pathways to apoptosis. Gene Dev 17(20):2481–2495
Fan T, Lu H, Hu H, Shi L, McClarty GA, Nance DM, Greenberg AH, Zhong G (1998) Inhibition of apoptosis in chlamydia-infected cells: blockade of mitochondrial cytochrome c release and caspase activation. J Exp Med 187(4):487–496
Bourdon JC, Laurenzi VD, Melino G, Lane D (2003) p53: 25 years of research and more questions to answer. Cell Death Differ 10(4):397–399
Gonzalez E, Rother M, Kerr MC, Al-Zeer MA, Abu-Lubad M, Kessler M, Brinkmann V, Loewer A, Meyer TF (2014) Chlamydia infection depends on a functional MDM2-p53 axis. Nat Commun 5:5201
Siegl C, Prusty BK, Karunakaran K, Wischhusen J, Rudel T (2014) Tumor suppressor p53 alters host cell metabolism to limit Chlamydia trachomatis infection. Cell Rep 9(3):918–929
Thomas NS, Lusher M, Storey CC, Clarke IN (1997) Plasmid diversity in Chlamydia. Microbiol 143(Pt 6):1847–1854
Rajalingam K, Sharma M, Lohmann C, Oswald M, Thieck O, Froelich CJ, Rudel T (2008) Mcl-1 is a key regulator of apoptosis resistance in Chlamydia trachomatis-infected cells. PLoS ONE 3(9):e3102
Zhong G (2016) Chlamydial plasmid-dependent pathogenicity. Trends Microbiol 25(2):141–152
Zhou H, Huang Q, Li Z, Wu Y, Xie X, Ma K, Cao W, Zhou Z, Lu C, Zhong G (2013) PORF5 plasmid protein of Chlamydia trachomatis induces MAPK-mediated pro-inflammatory cytokines via TLR2 activation in THP-1 cells. Sci China Life Sci 56(5):460–466
Cao W, Zou Y, Su S, He Z, Liu Y, Huang Q, Li Z (2015) Chlamydial plasmid-encoded protein pORF5 induces production of IL-1beta and IL-18 via NALP3 inflammasome activation and p38 MAPK pathway. Int J Clin Exp Med 8(11):20368–20379
Dong F, Pirbhai M, Xiao Y, Zhong Y, Wu Y, Zhong G (2005) Degradation of the proapoptotic proteins Bik, Puma, and Bim with Bcl-2 domain 3 homology in Chlamydia trachomatis-infected cells. Infect Immun 73(3):1861–1864
Mayo LD, Donner DB (2001) A phosphatidylinositol 3-kinase/Akt pathway promotes translocation of Mdm2 from the cytoplasm to the nucleus. Proc Natl Acad Sci USA 98(20):11598–11603
Chao CC (2015) Mechanisms of p53 degradation. Clin Chim Acta 438:139–147
Vassilev LT, Vu BT, Graves B, Carvajal D, Podlaski F, Filipovic Z, Kong N, Kammlott U, Lukacs C, Klein C, Fotouhi N, Liu EA (2004) In vivo activation of the p53 pathway by small-molecule antagonists of MDM2. Science 303(5659):844–848
Sigar IM, Schripsema JH, Wang Y, Clarke IN, Cutcliffe LT, Seth-Smith HM, Thomson NR, Bjartling C, Unemo M, Persson K, Ramsey KH (2014) Plasmid deficiency in urogenital isolates of Chlamydia trachomatis reduces infectivity and virulence in a mouse model. Pathog Dis 70(1):61–69
Gong S, Yang Z, Lei L, Shen L, Zhong G (2013) Characterization of Chlamydia trachomatis plasmid-encoded open reading frames. J Bacteriol 195(17):3819–3826
Song L, Carlson JH, Whitmire WM, Kari L, Virtaneva K, Sturdevant DE, Watkins H, Zhou B, Sturdevant GL, Porcella SF, McClarty G, Caldwell HD (2013) Chlamydia trachomatis plasmid-encoded Pgp4 is a transcriptional regulator of virulence-associated genes. Infect Immun 81(3):636–644
Liu Y, Huang Y, Yang Z, Sun Y, Gong S, Hou S, Chen C, Li Z, Liu Q, Wu Y, Baseman J, Zhong G (2014) Plasmid-encoded Pgp3 is a major virulence factor for Chlamydia muridarum to induce hydrosalpinx in mice. Infect Immun 82(12):5327–5335
Li Z, Wang S, Wu Y, Zhong G, Chen D (2008) Immunization with chlamydial plasmid protein pORF5 DNA vaccine induces protective immunity against genital chlamydial infection in mice. Sci China C Life Sci 11:973–980
Danial NN, Korsmeyer SJ (2004) Cell death: critical control points. Cell 116(2):205–219
Sharma M, Rudel T (2009) Apoptosis resistance in Chlamydia-infected cells: a fate worse than death? FEMS Immunol Med Microbiol 55(2):154–161
Kun D, Xiang-Lin C, Ming Z, Qi L (2013) Chlamydia inhibit host cell apoptosis by inducing Bag-1 via the MAPK/ERK survival pathway. Apoptosis 18(9):1083–1092
Ying S, Christian JG, Paschen SA, Häcker G (2008) Chlamydia trachomatis can protect host cells against apoptosis in the absence of cellular inhibitor of apoptosis proteins and Mcl-1. Microbes Infect 10(1):97–101
Zhong G (2011) Chlamydia trachomatis secretion of proteases for manipulating host signaling pathways. Front Microbiol 2:14
Pirbhai M, Dong F, Zhong Y, Pan KZ, Zhong G (2006) The secreted protease factor CPAF is responsible for degrading pro-apoptotic BH3-only proteins in Chlamydia trachomatis-infected cells. J Biol Chem 281(42):31495–31501
Ruiz-Vela A, Opferman JT, Cheng EH, Korsmeyer SJ (2005) Proapoptotic BAX and BAK control multiple initiator caspases. EMBO Rep 6(4):379–385
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Falasca M (2010) PI3K/Akt signalling pathway specific inhibitors: a novel strategy to sensitize cancer cells to anti-cancer drugs. Curr Pharm Design 16(12):1410–1416
Hennessy BT, Smith DL, Ram PT, Lu Y, Mills GB (2005) Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat Rev Drug Discov 4(12):988–1004
Subbarayal P, Karunakaran K, Winkler AC, Rother M, Gonzalez E, Meyer TF, Rudel T (2015) EphrinA2 receptor (EphA2) is an invasion and intracellular signaling receptor for Chlamydia trachomatis. PLoS Pathog 11(4):e1004846
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 31470277 and 81102230), Construct Program of the Key Discipline in Hunan Province (No. 2011-76), Hunan Provincial Key Laboratory for Special Pathogens Prevention and Control (No. 2014-5), and Hunan Province Cooperative innovation Center for Molecular Target New Drug Study (No. 2014-405).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Wenbo Lei contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zou, Y., Lei, W., Su, S. et al. Chlamydia trachomatis plasmid-encoded protein Pgp3 inhibits apoptosis via the PI3K-AKT-mediated MDM2-p53 axis. Mol Cell Biochem 452, 167–176 (2019). https://doi.org/10.1007/s11010-018-3422-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-018-3422-9