Abstract
Hyperhomocysteinemia is a risk factor for cardiovascular disease and the mechanism of homocysteine (HCY)-induced vascular endothelial cell injury has been intensively studied for many years. Recently, a large number of studies have shown inhibitory effects of genistein (GEN), a soy isoflavone, in the process of endothelial cell injury. In the present study, the protective effects of GEN in HCY-induced endothelial cell inflammatory injury were investigated. A model of HCY-induced endothelial cell (ECV-304) inflammatory injury was established in vitro, and the protective effect of GEN in this procession was explored. According to our results, GEN protected HCY-induced endothelial cell from viability decreases, meanwhile prevented the changes of cell morphology and the production of reactive oxygen species (ROS). The expression of NF-kB P-65, IL-6, and ICAM-1 was all down-regulated. During the HCY-induced endothelial cell injury, the endothelial cell apoptosis and proliferation disorder were alleviated. Therefore, we conclude that HCY-induced endothelial cell inflammatory injury could be blocked by GEN. The present findings suggest that GEN protects HCY-induced endothelial cell inflammatory injury may through reducing the release of ROS, inhibiting NF-kB activation, down-regulating the expression of cytokine IL-6 and adhesion molecules ICAM-1, avoiding inflammatory cells and platelet adhesion, accordingly, leading to a balance of endothelial cell proliferation and apoptosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arteriosclerosis (AS), a cardiovascular disease, is seriously dangerous to human health. Its occurrence and development rely on a variety of factors, such as elevated blood lipids, increased reactive oxygen species (ROS), the injury of endothelial cells, and activation of NF-kB signaling pathway [1–3]. Atherogenesis is a complex inflammatory process which initiates with endothelial dysfunction and leads to plaque formation mostly in the presence of excess cholesterol [4]. Although the pathogenesis of atherosclerotic vascular disease involves multifactorial processes, accumulating evidences demonstrated that inflammation and its subsequent endothelial dysfunction play a fundamental role in the initiation and progression of atherosclerosis [5]. The relationship between hyperhomocysteinemia and atherosclerosis was originally proposed more than 40 years ago by McCully [6]. Previous clinical and experimental studies have indicated that moderate increases in plasma HCY concentration are casual risk factors for vascular disease including atherosclerosis [7–10]. Previous studies have shown that HCY could induce the injury of vascular endothelial cell [11], but the mechanism remains controversial. Overproduction of ROS can damage vascular endothelial cells, numerous in vivo and in vitro studies have implicated that endothelial cell damage and death may play an important role in the development of atherogenesis [12]. Recent studies recognized that atherosclerosis is strongly modulated by proinflammatory mediators such as thrombin, tumor necrosis factor-alpha (TNF-α), and injured ECs-secreted cell adhesion molecules vascular cell adhesion molecule-1 (VCAM-1) and intracellular adhesion molecule-1 (ICAM-1) [13–15]. Further studies have indicated the elevated expression of proinflammatory chemokines such as IL-8 and adhesion molecules, including VCAM-1, ICAM-1, and endothelial-leukocyte adhesion molecule-1 [16–19]. These studies indicated that HCY influences endothelial cell injury, whereas the exact mechanism is still unclear.
GEN, the primary isoflavone found in soybeans, has been highlighted for its antioxidant effects and ability to activate the transcription of various genes. Due to its antioxidative properties, GEN effectively scavenges ROS and inhibits lipid peroxidation [20]. GEN has been shown to inhibit endothelial cell proliferation and angiogenesis in vitro and in vivo [21, 22]. Further research showed that GEN may be involved in the prevention of coronary heart disease by directly regulating human coronary artery endothelial cells (HCAEC) survival [23]. It also has been reported that GEN reduces hyperglycemia-induced vascular inflammation in ECs at physiological relevant concentrations [24]. However, the effects of GEN and the underlying mechanism about HCY-induced endothelial cell injury remain unclear. Here, we hypothesize that GEN alleviates HCY-induced vascular inflammation. In this study, we evaluate the effects of GEN in the prevention of HCY-induced endothelial inflammation in human umbilical vein ECs (HUVECs) at physiologically achievable concentration; we also analyzed various inflammatory components and examined the possible mechanisms involved in it.
Materials and methods
Materials
HCY(D090821), GEN(G0272), DCFH-DA(D6883), DMSO(D5879), and Hepes were purchased from Sigma-Aldrich (USA). Human umbilical vein endothelial cell (ECV-304) was purchased from Biological collection center, Wuhan University. Culture medium RPMI-1640 was purchased from GIBCO (USA). New calf serum was purchased from Sijiqing Company (Hangzhou). MTT(M8180) was purchased from Fluka (USA). IL-6(F20220) and ICAM-1(F20160) ELISA test kit were purchased from Shanghai west tang Biotechnology Company. Nucleo-capsid protein extraction kit (KGP1201) was purchased from Nanjing keygen engineering co., LTD. The primary antibodies of NF-κB p65 and β-actin were purchased from Santa Cruz (USA). Chemiluminescence enhance fluid was purchased from Pierce (USA).
Cell culture
All experimental operations were ethically approved and carried out by Zhengzhou traditional Chinese Medicine Hospital ethics committee. Human umbilical vein endothelial cell ECV-304 was cultured in RPMI 1640 medium containing 10 % new calf serum in 37 °C and 5 % CO2 incubator. All experimental manipulations are used logarithmic phase cells.
MTT assay
Cell viability was assessed by living cells mitochondrial succinate dehydrogenase can make the exogenous MTT [(3, 4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide] to formazan and deposition in the cell. Briefly, cell concentration was adjusted to 4 × 104/mL and seeded in 96-well plates, each well 100 μL then incubated for 24 h. When Adherent cell grown about 80 % of the plate, the original culture was abandoned, then we added different concentrations of GEN (0, 10, 50, 100 μM) and incubate for further 12 h. After that, we stimulated with 5.0 mM HCY in 100 μL RPMI 1640 for another 48 h. Subsequently, 20 μL MTT (5 mg/mL) was added into each sample and cells were incubated in the dark for 4 h, then 100 μL dissolved liquid (10 % SDS + 5 % isobutanol + 0.012 mol/l HCL)was added into each well until the formazan was dissolved. Cells viability was determined by measuring the absorbance at 570 nm using an ultraviolet spectrophotometer (BIO-RAD, USA). All cell survival assays were performed in quintuplicate and repeated in three independent experiments.
Cell morphology observation
Cells were seeded into 6-well plates in a concentration of 1 × 105/mL in cell culture medium. When the adherent cells were 80 % confluent, abandoned the original culture and treated the cells with different concentrations of GEN (0, 10, 50,100 μM) for 12 h. After that we incubated with 5.0 mM HCY for 48 h. Cell morphology was observed under an inverted microscope.
Detection of IL-6 and ICAM-1
The generation of IL-6 and ICAM-1 was detected by ELISA assay. When the adherent cells were about 80 % confluent, we abandon the original culture. Cells were treated with different concentrations (0, 10, 50,100 μM) of GEN for 12 h then added 5.0 mM HCY. The supernatant was collected at 0, 6, 12, 24 h and detected the expression levels of IL - 6 and ICAM - 1 in supernatant, respectively.
Flow cytometry assay
ECV-304 cells were seeded in 6-well plates in 2 mL RPMI 1640 complete culture medium at an equal density of 5 × 104/mL. When the adherent cells were about 80 % confluent, we abandon the original culture. Cells were treated with different concentrations (0, 10, 50, 100 μM) of GEN for 12 h then added 5.0 mM HCY for further 2 h. Subsequently, 10 μM DCFH-DA was added into each sample and cells were incubated at 37 °C for 20 min. After that, cells were digested by trypsin digestion and collected into a centrifuge tube 1,000 r/min for 5 min. Cells were washed twice and resuspended in 300 μL PBS and analyzed by FACS.
Western blotting analysis
Cells were resuspended in RIPA lysis buffer. Aliquots of cell extracts were resolved on a 10 % SDS-PAGE gel and then transferred onto a nitrocellulose membrane using a semi-dry transfer apparatus. The primary antibodies used were NF-kB p65 (1:200), β-actin (1:5,000). HRP-conjugated goat anti-mouse IgG was used as secondary antibodies. After washing with PBST, membranes were incubated with chemiluminescent substrate for 5 min. Protein bands were visualized by exposing the membranes to X-ray film.
Statistical analysis
The Data were presented as the mean ± SD. Results were analyzed by the one way ANOVA using SPSS 19.0 software. Experimental and control groups were compared using Dunnett-t test, P < 0.05 was considered different.
Results
GEN restores the ECV-304 cell damage induced by HCY
ECV-304 cells were pre-treated with different concentrations of GEN (0, 10, 50, 100 μM) for 12 h and then incubated with HCY (5.0 mM). Our results showed that after incubating with GEN, the cell activity of GEN group was significantly higher than HCY (5.0 mM) treatment group (Table 1, P < 0.01). Compared with the control group, HCY (5.0 mM)-treated group showed the lowest activity (P < 0.01). The cell activity was significantly increased along with the increase of GEN concentrations, but there is no significant difference when the concentration of GEN is 100 μM compare with control (P > 0.05). Therefore, HCY can really damage the endothelial cell and decreased cell activity, and different concentrations of GEN can suppress this injury and restore the endothelial cell damage (Table 1).
Compared with the control group,*P<0.05, **P<0.01; alone compared with 5.0 mM group, #P<0.01. A Normal control, B HCY 5.0 mM, C GEN 10 μM + HCY 5.0 mM, D GEN 50 μM + HCY 5.0 mM, E GEN 100 μM + HCY 5.0 mM.
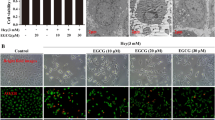
Cell morphology
Normal ECV-304 cells were smooth and plump, showing single cobblestone mosaic arrangement under an inverted microscope. After stimulate with 5.0 mM HCY, cell become shrink, round, connected to each other, and cell arrangement becomes cluttered and gathered into a group. These phenomena indicated that cell suffered from serious damage. Based on this, cells were pre-treated with different concentrations of GEN (0, 10, 50, 100 μM) for 12 h, and then incubated with 5.0 mM HCY for another 24 h, we found that cell morphology was gradually improved with the increase of GEN concentration.
We also found that the gap between cells was narrow; the connections between cells were more intend, and, cell boundary was more clearly, a few cells revert to short spindle when GEN at a low concentration was used. Cell morphology was significantly improved after stimulated with GEN in HCY 5.0 mM, most of cells showing short spindle, polygonal, or monolayer, some cells still express shedding phenomenon but has been greatly restored. In the high concentration of GEN group, cells plump, uniform size, and there are almost no visible shedding cells, morphology returned to normal, there is no significant difference when compared with the control (Fig. 1a).
a The changes in the morphology of ECV-304 cells induced by HCY and GEN. ECV-304 cells were pre-treated with various concentrations of GEN (0, 10, 50, and 100 μM) for 12 h and subsequently incubated with HCY (5.0 mM) for further 24 h; cell morphology was observed under the inverted microscope. A Normal control, B HCY 5.0 mM, C GEN 10 μM + HCY 5.0 mM, D GEN 50 μM + HCY 5.0 mM, E GEN 100 μM + HCY 5.0 mM. b The concentrations of IL-6, ICAM-1 treated by 5.0 mM HCY for different times. ECV-304 cells were treated with HCY (5.0 mM) for different times (0, 6, 12, and 24 h), the concentrations of IL-6 and ICAM-1 were measured with IL-6 and ICAM-1 ELISA test kit. c The inhibited effects of GEN on HCY-induced elevation of IL-6, ICAM-1. ECV-304 cells were pre-treated with different concentrations of GEN (0, 10, 50, and 100 μM) for 6 h, and then incubated with HCY (5.0 mM) for additional 12 h. The concentrations of IL-6 and ICAM-1 in the supernatant were measured with IL-6 and ICAM-1 ELISA test kit
HCY promotes the generation of IL-6 and ICAM-1
After incubating with 5.0 mM HCY for different times (6, 12, and 24 h), we found that the generation of IL-6 and ICAM-1 was significantly increased, and the peak appeared at about 12 h, followed by gradually decreasing. There has a significantly difference compared with 0 h (Fig. 1b, P < 0.01).
When we pre-treated the cells with GEN (0, 10, 50, 100 μM) for 6 h after incubating with 5.0 mM HCY, the generation of IL-6 and ICAM-1 was decreased. The IL-6 generation in the cells treated with GEN 100 μM plus HCY 5.0 mM decreased most acutely compared with that in the cells treated with HCY 5.0 mM alone and the difference was statistically significant (P < 0.05). There has no statistically significance of ICAM-1 generation between GEN 0 μM group and control group (Fig. 1c, P > 0.05).
GEN inhibits the generation of ROS induced by HCY
Our results showed that after treated with 5.0 mM HCY on ECV-304 cells for 2 h, the generation of ROS in cells was 170.12 ± 15.90, and the control group was 37.67 ± 5.61. The peak moved toward right and fluorescence changes more intensity. The differences between these two groups were statistically significant (P < 0.01). After pre-treating cells with different concentrations (0, 10, 50, 100 μM) of GEN for 12 h, then added 5.0 mM of HCY for further 2 h, the generation of ROS was 138.04 ± 16.02, 116.95 ± 14.09, 43.47 ± 9.86, respectively. The peak moved toward left along with the increase of GEN concentration. Therefore, GEN could inhibit the generation of ROS induced by HCY (Fig. 2).
The effects of HCY and its combination with GEN on ROS levels in ECV-304 cells. ECV-304 cells were pre-treated with different concentrations of GEN (0, 10, 50, and 100 μM) for 12 h, subsequently incubated with HCY (5.0 mM) for 2 h. ROS levels were measured with Flow cytometry (BECKMAN COULTER Gallios, USA). a Normal control, b HCY 5.0 mM, c GEN 10 μM + HCY 5.0 mM, d GEN 50 μM + HCY 5.0 mM, e GEN 100 μM + HCY 5.0 mM
GEN can block the expression of NF-kB p65 protein induced by HCY
After treating ECV-304 cells with 5.0 mM of HCY, the expression of nucleus NF-κB p65 protein showing a significant increase compared with the control, the difference was statistically significant (P < 0.05), indicated that HCY can promote nuclear translocation of NF-kB. When we added different concentrations (0, 10, 50, 100 μM) of GEN for 12 h, the expression of NF-κB p65 protein was gradually decreased along with the increase of GEN concentration (Fig. 3). Especially the group of 100 μM GEN had no significant difference in gray values when compared with the control group (P > 0.05), but had a significant difference when compared with the 5.0 mM HCY group (P < 0.01). Therefore, GEN showed an ability of blocking the expression of NF-kB p65 protein induced by HCY (Fig. 3).
The expressions of p65 protein in different groups of ECV-304 cells treated by Western blot (%). ECV-304 cells were seeded in 6-wells plates in a density of 5 × 105/mL, and exposed to GEN for various concentrations (0, 10, 50, 100 μM) after pre-treated with 5.0 mM of HCY. The expression of NF-kB p65 was determined by Western blot analysis. β-actin was used as an equal-loading control of samples
Discussion
Atherosclerosis results from injury to the vein endothelium caused by mechanical and environmental factors, resulting inflammatory response in the vessel wall [25]. Previous studies have shown that HCY-induced vascular endothelial cell injury is an independent risk factor for atherosclerosis [10, 11] and can result in large amounts of oxygen free radicals, reactive oxygen species, and so on. Overproduction of ROS can damage vascular endothelial cells, and numerous in vivo and in vitro studies have implicated that endothelial cell damage and death may play a role in the development of atherogenesis [12]. After endothelial cell injury, NF-kB is activated, allowing the increased expression of inflammatory cytokines IL-6 and adhesion molecules ICAM-1 promoting the formation of atherosclerotic plaques [17, 18, 26]. As it has been previously shown by Plazar and Jurdana, the normal and abnormal HCY levels are set by individual laboratories. However, the concentration of HCY is considered normal at levels <13 µM, levels between 13 and 60 µM are considered moderately elevated, and levels >60–100 µM are considered significantly elevated [27]. Elevated HCY levels are associated with increased formation of ROS, especially super oxide anion in vascular cells [28, 29] ,Therefore, our results suggest that high concentrations of HCY may diminish the synthesis of NO in endothelial cells, contributing to the development of atherothrombotic processes [30]. Endothelial apoptosis represents the critical event for the initiation of atherosclerosis [4]. Recently, the role of nitrative stress in HCY-induced endothelial dysfunction had drawn much attention. As we know, high levels of HCY may promote oxidative stress in endothelial cells as a result of production of reactive oxygen species [31].
Previous studies have shown that treatment with low (physiological) concentrations of the soya isoflavone GEN significantly protects vascular endothelial cells against oxidative stress-induced loss of cell viability and apoptosis [32]. In the present study, we used 5.0 mM of HCY-induced endothelial cell, and then adding different concentrations of GEN. In conclusion, GEN can protect against oxidative stress-induced endothelial cell injury by altering the expression of antioxidant genes and elevating antioxidant enzyme and GSH levels. The present results provide the basis for further evaluation of the effects of soya isoflavones with regard to their potential in the treatment of CVD. Moreover, the present findings suggest that the lower incidence of CVD in Asian populations compared with Western populations may be at least partially due to the higher plasma concentration of GEN in Asian individuals. It has been shown that GEN inhibits the activation of NF-kB and Akt signaling pathways [33, 34], both of which are known to maintain a homeostatic balance between cell survival and apoptosis. Moreover, GEN antagonizes estrogen- and androgen-mediated signaling pathways in the processes of carcinogenesis [35, 36]. Furthermore, GEN has been found to have antioxidant properties and has been shown to be a potent inhibitor of angiogenesis and metastasis [37, 38].The maximum attainable plasma concentration of GEN is approximately 1–4 IM for people taking a single soy meal [39]. Mounting evidence links the intake of isoflavones in soy rich foods to lower rates of prostate and breast cancers in Asian countries than in Western population [37]. GEN is the predominant isoflavone found in soybean-enriched foods. In addition to its anticancer properties, GEN has an excellent bioavailability via oral administration and safety use for clinical transition [40]. In line with this information, we started our work evaluating the anti-inflammatory activity of GEN in HCY-induced endothelial cell injury.
The vasculoprotective effects of GEN were also reported in previous studies, but the underlying mechanism remains elusive. The protective effect of GEN on vascular inflammation is independent of ERs or its potential antioxidant effect, but largely depends on a PKA-mediated mechanism. Other findings provide the evidences suggesting that GEN may be a novel agent to protect vasculature against TNF-α-caused inflammation and dysfunction [41]. The other study indicates that proteome analysis allows the rapid identification of cellular target proteins of GEN action in endothelial cells exposed to the endothelial stressor HCY, therefore enables the identification of molecular pathways of its antiatherosclerotic action [42]. In the present study, we found that GEN could down-regulate the expression of NF-kB p65, which associated with the proliferation and apoptosis of cells and the production of some cytokines. However, whether protection or activation of this pathway plays an essential role in mediating the anti-inflammatory effect of GEN in vivo needs further investigation.
The findings in the present study demonstrate that targeting NF-kB p65 or ROS, and inhibition of the expressions of cytokines IL-6 and adhesion molecules ICAM-1 by GEN may be an important mechanism for the suppression of anti-inflammatory activity (Fig. 4). This study provides a diagnose basis for the clinical therapy of cardiovascular disease using GEN.
References
Chen F, Castranova V, Li Z et al (2003) Inhibitor of nuclear factor kappaB kinase deficiency enhances oxidative stress and prolongs c-Jun NH2-terminal kinase activation induced by arsenic. Cancer Res 63:7689–7693
Yang G, Abate A, George AG et al (2004) Maturational differences in lung NF-κB activation and their role in tolerance to hyperoxia. Clin Invest 114:669–678
Lemarie A, Morzadec C, Delphine M et al (2006) Arsenic trioxide induces apoptosis of human monocytes during macrophagic differentiation through nuclear factor-kB related survival pathway down-regulation. J Pharmacol Exp Ther 316:304–314
Ross R (1999) Atherosclerosis-an inflammatory disease. N Engl J Med 340:115–126
Pearson TA, Mensah GA, Alexander RW et al (2003) Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107:499–511
McCully KS (1969) Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. Am J Pathol 56:111–128
Boushey CJ, Beresford SA, Omenn GS, Motulsky AG (1995) A quantitative assessment of plasma homocysteine as a risk factor for vascular disease. Probable benefts of increasing folic acid intakes. JAMA 274:1049–1057
Nygard O, Vollset SE, Refsum H et al (1995) Total plasma homocysteine and cardiovascular risk profile. The Hordaland HCY Study. JAMA 274:1526–1533
Ueland PM, Refsum H, Beresford SA, Vollset SE (2000) The controversy over homocysteine and cardiovascular risk. Am J Clin Nutr 72:324–332
Tehlivets O (2011) Homocysteine as a risk factor for atherosclerosis: is its conversion to s-adenosyl-L-homocysteine the key to deregulated lipid metabolism? J Lipids 2011:702853
Dong D, Wang B, Yin W et al (2013) Disturbance of copper homeostasis is a mechanism for homocysteine-induced vascular endothelial cell injury. PLoS One 8:e76209
Clarke M, Bennett M, Littlewood T (2007) Cell death in the cardiovascular system. Heart 93:659–664
Thompson SG, Kienast J, Pyke SD, Haverkate F, van de Loo JC (1995) Hemostatic factors and the risk of myocardial infarction or sudden death in patients with angina pectoris. European concerted action on thrombosis and disabilities angina pectoris study group. N Engl J Med 332:635–641
Danesh J, Wheeler JG, Hirschfield GM et al (2004) C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med 350:1387–1397
Ridker PM, Hennekens CH, Buring JE, Rifai N (2000) C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 342:836–843
Potenza MA, Gagliardi S, Nacci C, Carratu MR, Montagnani M (2009) Endothelial dysfunction in diabetes: from mechanisms to therapeutic targets. Curr Med Chem 16:94–112
Srinivasan S, Bolick DT, Hatley ME et al (2004) Glucose regulates interleukin- 8 production in aortic endothelial cells through activation of the p38 mitogen-activated protein kinase pathway in diabetes. J Biol Chem 279:31930–31936
Morigi M, Angioletti S, Imberti B et al (1998) Leukocyte-endothelial interaction is augmented by high glucose concentrations and hyperglycemia in a NF-kB-dependent fashion. J Clin Invest 101:1905–1915
Srinivasan S, Yeh M, Danziger EC et al (2003) Glucose regulates monocyte adhesion through endothelial production of interleukin-8. Circ Res 92:371–377
Exner M, Hermann M, Hofbauer R et al (2001) Genistein prevents the glucose autoxidation mediated atherogenic modification of low density lipoprotein. Free Radic Res 34:101–112
Fotsis T, Pepper M, Adlercreutz H et al (1993) Genistein, a dietary-derived inhibitor of in vitro angiogenesis. Proc Natl Acad Sci USA 90:2690–2694
Kiriakidis S, Högemeier O, Starcke S et al (2005) Novel tempeh (fermented soya bean) isoflavones inhibit in vivo angiogenesis in the chicken chorioallantoic membrane assay. Br J Nutr 93:317–323
Kayisli UA et al (2013) Genistein inhibits cell proliferation and stimulates apoptosis in human coronary artery endothelial cells. Gynecol Obstet Invest 75:235–242
Babu PV, Si H, Fu Z, Zhen W, Liu D (2012) Genistein prevents hyperglycemia-induced monocyte adhesion to human aortic endothelial cells through preservation of the cAMP signaling pathway and ameliorates vascular inflammation in obese diabetic mice. J Nutr 142:724–730
Homeister JW, Willis (2010) Atherosclerosis: pathogenesis, genetics and experimental models. Encyclopedia of life sciences. John Wiley, Sons Ltd, Chichester
Hofmann MA, Lalla E, Lu Y et al (2001) Hyperhomocysteinemia enhances vascular inflammation and accelerates atherosclerosis in a murine mode. Clin Invest 107:675–683
Plazar N, Jurdana M (2012) Hyperhomocysteinemia: relation to cardiovascular disease and venous thromboembolism. In: Abdelaal MA (ed) Pathophysiology and clinical aspects of venous thromboembolism in neonates, renal disease and cancer patients. InTech, Rijeka, pp 17–34
Edirimanne VE, Woo CW, Siow YL et al (2007) Homocysteine stimulates NADPH oxidase-mediated superoxide production leading to endothelial dysfunctionin rats. Can J Physiol Pharmacol 85:1236–1247
Weiss N (2005) Mechanisms of increased vascular oxidant stress in hyperhomocysteinemia and its impact on endothelial function. Curr Drug Metab 6:27–36
Cortes Magdalena P, Juan P (2013) Inhibition of ATP-induced calcium influx by homocysteine in human umbilical vein endothelial cells. Cell Biol Int 37:600–607
Tyagi N, Sedoris KC, Steed M et al (2005) Mechanisms of homocysteine-induced oxidative stress. Am J Physiol Heart Circ Physiol 289:H2649–H2656
Zhang T, Wang F, Xu HX et al (2012) Activation of nuclear factor erythroid 2-related factor 2 and PPARg plays a role in the genistein-mediated attenuation of oxidative stress-induced endothelial cell injury. Br J Nutr 2:1–13
El-Rayes BF, Ali S, Ali IF, Philip PA, Abbruzzese J, Sarkar FH (2006) Potentiation of the effect of erlotinib by genistein in pancreatic cancer: the role of Akt and nuclear factor-kappaB. Cancer Res 66:10553–10559
Li Y, Sarkar FH (2002) Inhibition of nuclear factor kappaB activation in PC3 cells by genistein is mediated via Akt signaling pathway. Clin Cancer Res 8:2369–2377
Manach C, Williamson G, Morand C, Scalbert A (2005) Re´me´sy C. Bioavailability and bioefficacy of polyphenols in humans. I. Review of 97 bioavailability studies. Am J Clin Nutr 81:230S–242S
Williamson G, Manach C (2005) Bioavailability and bioefficacy of polyphenols in humans. II. Review of 93 intervention studies. Am J Clin Nutr 81:243S–255S
Banerjee S, Li Y, Wang Z, Sarkar FH (2008) Multi-targeted therapy of cancer by genistein. Cancer Lett 269:226–242
Polkowski K, Mazurek AP (2000) Biological properties of genistein. A review of in vitro and in vivo data. Acta Pol Pharm 57:135–155
King RA, Bursill DB (1998) Plasma and urinary kinetics of the isoflavones daidzein and genistein after a single soy meal in humans. Am J Clin Nutr 67:867–872
Cassidy A, Faughnan M (2000) Phyto-oestrogens through the life cycle. Proc Nutr Soc 59:489–496
Jia Z, Babu PV, Si H et al (2013) Genistein inhibits TNF-α-induced endothelial inflammation through the protein kinase pathway A and improves vascular inflammation in C57BL/6 mice. Int J Cardiol 168:2637–2645
Fuchs D, Erhard P, Rimbach G et al (2005) Genistein blocks homocysteine-induced alterations in the proteome of human endothelial cells. Proteomics 5:2808–2818
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Han, S., Wu, H., Li, W. et al. Protective effects of genistein in homocysteine-induced endothelial cell inflammatory injury. Mol Cell Biochem 403, 43–49 (2015). https://doi.org/10.1007/s11010-015-2335-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-015-2335-0