Abstract
The aim of this study was to assess the oxidative stress status in rheumatoid arthritis (RA) by measuring markers of free radical production, systemic activity of disease, and levels of antioxidant. 52 RA patients and 30 healthy controls were included in the study, and clinical examination and investigations were performed and disease activity was assessed. Peripheral blood samples were used for all the assays. We assessed the markers of oxidative stress, including plasma levels of index of lipid peroxidation-thiobarbituric acid reactive substances (TBARS), hydrogen peroxide (H2O2), superoxide anion radical (O2 −), nitric oxide (NO), and superoxide dismutase activity (SOD), catalase activity (CAT) and glutathione levels in erythrocytes. In the RA group, levels of H2O2, O2 −, and TBARS were significantly higher than in controls (4.08 ± 0.31 vs. 2.39 ± 0.13 nmol/l, p < 0.01; 8.90 ± 1.28 vs. 3.04 ± 0.38 nmol/l, p < 0.01, 3.65 ± 0.55 vs. 1.06 ± 0.17 μmol/l, p < 0.01). RA patients had significantly increased SOD activity compared with healthy controls (2,918.24 ± 477.14 vs. 643.46 ± 200.63UgHbx103, p < 0.001). Patients had significantly higher levels of pro-oxidants (O2 −, H2O2, and TBARS) compared to controls, despite significantly higher levels of SOD. Significant differences were also observed in serum levels of NO in patients with high-diseases activity. Our findings support an association between oxidative/nitrosative stress and RA. Stronger response in samples with higher diseases activity suggests that oxidative/nitrosative stress markers may be useful in evaluating the progression of RA as well as in elucidating the mechanisms of disease pathogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease that affects ~1 % of the population. It is characterized by irreversible joint disorder accompanied by destruction of bone and cartilage [1]. Although the etiology is unknown, RA is certainly associated with autoimmune disorders, and its pathogenesis has been well investigated [2].
Apart from the present immunogenic targets, reactive oxygen species (ROS) are of considerable interest. ROS have also been considered as aggravating factors for autoimmune diseases [1], as there is a significant relation between the oxidative stress and such diseases [2]. ROS are spontaneously produced as by-product during electron transfer in oxidative phosphorylation [3]. ROS include superoxide, peroxide, hydroxyl radicals, and reactive nitrogen species (RNS). They oxidize various cellular and extracellular components, including nucleotides, DNA, proteins, polysaccharides, and lipids, by the unpaired free radicals.ROS could be produced as a result of inflammation which leads to the destruction of cartilage and bone, neutrophils degranulation, and release a variety of potentially harmful enzymes and peptides [4]. Furthermore, the numerous products that appear to be generated by ROS have been identified in clinical samples including peripheral blood and fluid from the joints in patients with RA [5–7]. Because of the highly reactive nature of ROS and RNS, it is difficult to directly demonstrate their presence in vivo. It is considerably more practical to measure the “footprints” of ROS and RNS, such as their effects on various lipids, proteins, and nucleic acids [8].
Direct evidence is also lacking about whether ROS prime the autoimmune response or reduce chronic inflammation in RA. NO has been shown to regulate T cell functions under physiological conditions, but overproduction of NO may contribute to T lymphocyte dysfunction [9]. Several investigators found correlations between serum nitrite concentration and RA disease activity or radiological progression while others did not find such correlations [10, 11].
Cells have different antioxidant systems to defend themselves against free radical attacks. Circulating human erythrocytes possess the ability to scavenge O2 − and H2O2 generated extracellularly by activated neutrophils, superoxide dismutase (SOD), catalase (CAT), and glutathione peroxidase (GSH-Px)-dependent mechanisms. The results about antioxidant state of patients with RA are inconsistent, since studies have reported both decreased and unaltered activity of antioxidant enzymes in serum and erythrocytes of RA patients [12–14].
The aim of this study was to assess the oxidative stress status in RA by measuring markers of free radical production and levels of antioxidant, as well as to analyze patients redox state considering the diseases activity and other clinical characteristics.
Patients and methods
Patients
Fifty-two patients with RA (mean age 52.46 years, SD ± 7.39, min 37–max 60 years) who fulfilled the 1987 [15] and 2010 [16] American College of Rheumatology criteria for RA were enrolled. Patients were recruited from the Outpatient unit of Rheumatology Department at the Clinical Center Kragujevac, Serbia, in 2011. The median duration of illness was 7 years (range 1–20 years). Erythrocyte sedimentation rate (ESR) was determined using the Westergren technique, and C reactive protein (CRP) was determined by nephelometry. Serum rheumatoid factor (RF) was measured by the latex agglutination technique. Patients were considered seropositive, if any determination during the study was positive. The presence of antibodies against cyclic citrullinated peptide (anti-CCP) in serum was detected using the Diastat kit (Axis-Shield Diagnostics, Dundee, UK) with a cut-off value of 5 U/mL. The disease activity of RA patients was calculated as diseases activity score 28 (DAS 28) according to the method of Prevoo et al. [17]. DAS 28 consisted number of 28 joint swelling and 28 joint tender, which included proximal interphalangeal joint, metacarpal phalangeal joint, wrist, elbow, shoulder, and knee (joints); together with erythrocyte sedimentation rate (ESR) and visual analog score (VAS). VAS was a scale that uses a horizontal 100-mm line, where patients would indicate degree of pain by placing a mark on a line between “no pain” (left end 0 mm) and “excruciating pain” (right end 100 mm). Values DAS 28 ≤ 3.2 mean low-diseases activity, and values DAS 28 > 3.2 mean moderate and high-diseases activity. At the time of the study, all patients were treated with one or two disease-modifying antirheumatic drugs (DMARD). The patients treated with high doses of steroids (>10 mg/day, including parenteral administration) and those treated with biologic therapy were excluded from the study in order to exclude possible role of systemic application of corticosteroids on endothelial (dys) function [18, 19]. COX-2 inhibitors and NSAIDs were applied only occasionally. All 30 controls–hospital personnel matched by age and sex (mean age 55.23 years ± SD 4.232, min. 43–max. 60 years) participated in the study. The following exclusion criteria were used for the both groups: smoking (past 5 years), alcohol intake (past 12 months), narcotic drugs (never), hypertension, diabetes mellitus, hypothyroidism, hyperthyroidism, and any other form of arthritis except RA. Patients on other lines of treatment such as ayurveda, homeopathy, and siddha were also excluded from this study. Informed consent was obtained from all subjects. The local institutional Ethical committee approved the study protocol.
Biochemical assays
Blood samples were taken from an antecubital vein into Vacutainer test tube containing sodium citrate anticoagulant. Blood samples were analyzed immediately. Blood was centrifuged to separate plasma and red blood cells (RBCs). Biochemical parameters were measured spectrophotometrically.
Superoxide anion radical determination
The level of superoxide anion radical (O2 −) was measured using nitro blue tetrazolium (NBT) reaction in TRIS-buffer combined with plasma samples and read at 530 nm [20].
Hydrogen peroxide determination
The protocol for measurement of hydrogen peroxide (H2O2) is based on oxidation of phenol red in the presence of horseradish peroxidase [21]. 200 μl sample with 800 μl PRS (phenol red solution) and 10 μl POD (Horseradish Peroxidase) were combined (1:20). The level of H2O2 was measured at 610 nm.
Nitric oxide determination
Nitric oxide (NO) decomposes rapidly to form stable metabolite nitrite/nitrate products. Nitrite (NO2 −) was determined as an index of nitric oxide production with Griess reagent [22]. 0.1 ml 3 N PCA (Perchloride acid), 0.4 ml 20 mM ethylenediaminetetraacetic acid (EDTA), and 0.2 ml plasma were put on ice for 15 min, then centrifuged 15 min at 6,000 rpm. After pouring off the supernatant, 220 μl K2CO3 was added. Nitrites were measured at 550 nm. Distilled water was used as a blank probe.
Index of lipid peroxidation (thiobarbituric acid reactive substances, TBARS)
The degree of lipid peroxidation in plasma was estimated by measuring of TBARS using 1 % TBA (thiobarbituric Acid) in 0.05 NaOH, incubated with plasma at 100 °C for 15 min and read at 530 nm. Distilled water was used as a blank probe. TBA extract was obtained by combining 0.8 ml plasma and 0.4 ml trichloro acetic acid (TCA), then samples were put on ice for 10 min, and centrifuged for 15 min at 6,000 rpm. This method was described previously [23].
Determination of antioxidant enzymes
Isolated RBCs were washed three times with three volumes of ice-cold 0.9 mmol/l NaCl, and hemolysates containing about 50 g Hb/l (prepared according to McCord and Fridovich [24]) were used for the determination of CAT activity. CAT activity was determined according to Beutler [25]. Then 50 μl CAT buffer, 100 μl sample, and 1 ml 10 mM H2O2 were added to the samples. Detection was performed at 360 nm. Distilled water was used as a blank probe. SOD activity was determined by the epinephrine method of Misra and Fridovich [26]. A hundred μl lysate and 1 ml carbonate buffer were mixed, and then 100 μl of epinephrine was added. Detection was performed at 470 nm.
Determination of glutathione
The level of reduced glutathione (GSH) was determined based on GSH oxidation with 5.5-dithio-bis-6.2-nitrobenzoic acid, using Beutler method [27]; the concentration is expressed as nanomoles per milliliter of RBCs.
Statistics
The statistical analysis was performed with SPSS 15.0 for Windows. Results are expressed as the mean ± standard error of the mean. Data distribution was checked with the Shapiro–Wilk test, and depending on its results, the appropriate parametric or nonparametric test was used. The differences between two groups were assessed using T test or Man-Whitney test, while the differences between the values of means from more than two groups were assessed by ANOVA or Kruskal–Wallis test. Correlation between various variables was found using Bivariate correlation, i.e., Spearman’s coefficient of correlation.
Results
The demographic and clinical characteristics of patients with RA and healthy controls are summarized in Table 1. Forty out of 52 (77 %) patients were RF seropositive and 47 of 52 (93 %) had anti-CCP antibodies. The DMARDS patients received were 26 methotrexate; 26 were receiving a combination of methotrexate and hydroxychloroquine phosphate. Additionally, 63 % patients received low doses corticosteroids for at least 1 year continuously (average dose 7.5 mg) (Table 1).
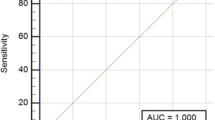
Parameters of oxidative stress are shown in Table 2. Regarding oxidative stress parameters, patients and controls differed in four out of seven investigated parameters: superoxide anion radical, hydrogen peroxide, index of lipid peroxidation, and activity of SOD- Figs. 1 and 2 (values are expressed as median and range). Besides increased activity of SOD in patients compared with controls (2,918.24 ± 477.14 U/g Hb ×103 compared to 643.46 ± 200.63, p < 0.01), the levels of O2 − in plasma of patients with RA were significantly increased compared to the control group (8.90 ± 1.28 compared to 3.04 ± 0.38 nmol/ml; p < 0.01), as well as H2O2 levels (4.08 ± 0.31 compared to 2.39 ± 0.13 nmol/ml; p < 0.01) and TBARS levels (3.65 ± 0.55 compared to 1.06 ± 0.17 μmol/ml; p < 0.01). There were no differences between RA cases and controls for levels of NO, CAT, and GSH. The increase in the levels of ESR and CRP in the patient group was found to be highly significant (p < 0.01) (Table 2). In RA patients we found negative correlation between NO2- and GSH and positive correlation between TBARS and GSH (Table 3). Other pro- and anti-oxidative parameters do not correlate significantly in RA patients (Table 3).
A statistically significant increase in the levels of total NO was also observed in the patients with moderate or higher diseases (DAS 28 > 3.2) when compared to the patients with low-diseases activity (DAS 28 ≤ 3.2) (p < 0.05) (Table 4). The serum oxidative stress markers (O2 −, H2O2, TBARS) and antioxidants (SOD, CAT, GSH) in RA patients were not associated with different DAS 28 activity scores.
There was no correlation between the measurements of the serum oxidative stress markers and antioxidant capacity and diseases duration, CRP, ESR, the presence of RF, anti-CCP antibodies, or the medications used in RA patients in the study (data not showed).
Discussion
Many studies have demonstrated a role of ROS in the pathogenesis of inflammatory chronic arthropathies, such as RA [5]. Therefore, an understanding of the complex interactions between these pathways might be useful for the development of novel therapeutic strategies for RA [5].
RA involves two basic recurring mechanisms of ROS production: via activated polymorphonuclear cells (PMNs) and ischemia–reperfusion in the inflamed joints [28]. These reactive species, if not scavenged, lead to lipid peroxidation. During lipid peroxidation, polyunsaturated fatty acids are oxidized to produce lipid peroxyl radicals that in turn lead to further oxidation of polyunsaturated fatty acid in a perpetuating chain reaction that can lead to cell membrane damage. RA patients in our study had significantly elevated levels of TBARS compared with healthy control subjects. This is in accordance with a number of previous studies [4, 28]. Studies with synovial fluids and tissues in RA have also demonstrated oxidative damage of lipoperoxidation products [29].
We observed significantly higher levels of superoxide anion radical and hydrogen peroxide in plasma of RA patients. Probably, superoxide anion radicals in plasma could be dismutated to produce hydrogen peroxide by increased SOD activity, but hydrogen peroxide was not detoxified by CAT or glutathione. Hydrogen peroxide possibly converted to hydroxyl radical by iron due to lower transferrin level might have led to increased serum lipid peroxidation in patients with RA [5]. Likewise, unchanged levels in CAT activity (Table 2) could be consequence of well known increase of H2S in RA patients [6].
Nitric oxide (NO) has been shown to regulate T cell functions under physiological conditions, but overproduction of NO may contribute to T lymphocyte dysfunction [10]. Ueki et al. [30] analyzed nitrite concentrations in serum and synovia of patients with RA and osteoarthritis OA. In our study, plasma NO level of RA patients was not significantly different from controls. Furthermore, according to our data presented in Table 3, NO2 − negatively correlates significantly only with GSH, what is possible consequence of compensatory effects of intracellular non-enzymatic antioxidative mechanisms to increased NO2 − production. So, patients suffering from RA slightly increased GSH compared to control, but in enough manner to start with adequate NO2 − scavenging.
Several studies in patients with RA have documented evidence for increased endogenous NO synthesis, suggesting that overproduction of NO may be important in the pathogenesis of RA. The inflamed joint in RA is the predominant source of NO [31]. Several investigators found correlations between serum nitrite concentration and RA disease activity or radiological progression while others did not find such correlations [10]. Jikimoto and other coauthors [32–34] reported a correlation between the disease activity and the presence of oxidative stress in patients with RA. Other authors have not found significant correlations between the disease activity and the presence of oxidative stress in patients with RA [35]. Our study also showed significant correlation between the moderate or higher disease activity and the presence of higher levels nitric oxide.
Several defence mechanisms have evolved to protect cellular systems from oxidative damage. The relationship between erythrocyte SOD and RA is not clear. In our study, patients had significantly increased SOD activity as compared to the controls. On the other hand, the level of SOD activity in RA patients was inconsistent in different studies where increased [36], decreased [37], or comparable level of SOD activity in RA patients to the healthy subjects were reported. On the other hand, only correlation what we found is positive correlation between TBARS and GSH, while other pro- and antioxidative parameters do not correlate significantly (Table 3). Possible explanation for that result is that in RA patients is increased second line of defence against oxidative stress, induced by oxidative modification of cell membranes, while first line, such SOD and CAT do not express any significant changes under the increased oxidative stress.
Unlike the increased SOD activity in our patients, CAT and GSH levels were comparable between patients and controls. In confirm with our finding, other studies reported a similar pattern of CAT level in RA patients [38]. On the other hand, a previous study found increased activity of CAT in RA patients [39]. Other studies also reported either unchanged [12] or elevated GSH levels and GSH-Px activity [40] levels in serum or erythrocytes of patients with RA.
One of the limitations of this study was that we did not measure ROS in neutrophils from peripheral blood or monocytes from both sources. That can be measured in some additional study, even we can not expect any significant changes, compared to red blood cells, because disease activity and white blood cells in RA do not fit, especially in our group, what is quite different compared to some other pathophysiological statements as chronic lymphocytic leukemia [41]. Moreover, during conduction of present study, our patients did not have active synovitis on the major joints, which have been recorded by clinical examination and ultrasound. Affected joints are not appropriate for function of synovial fluid.
Results of present study pointed out a significance of NO as a potential marker of disease activity. Furthermore, correction of oxidative stress in RA patients could be benefitial in reduction of inflammation. Also, additional investigations of the benefits of correction of oxidative stress levels for RA patients are needed, because this therapy has enormous potential, but is currently under-utilized and its benefits are not thoroughly explored.
References
Smith HS, Smith AR, Seidner P (2011) Painful rheumatoid arthritis. Pain Physician 14:E427–E458
McInnes IB, Schett G (2011) The pathogenesis of rheumatoid arthritis. N Engl J Med 365:2205–2219
Chinopoulos C, Adam-Vizi V (2006) Calcium, mitochondria and oxidative stress in neuronal pathology. Novel aspects of an enduring theme. FEBS J 273:433–450
Stamp LK, Khalilova I, Tarr JM, Senthilmohan R, Turner R, Haigh RC, Winyard PG, Kettle AJ (2012) Myeloperoxidase and oxidative stress in rheumatoid arthritis. Rheumatology (Oxford) 51:1796–1803
Filippin LI, Vercelino R, Marroni NP, Xavier RM (2008) Redox signalling and the inflammatory response in rheumatoid arthritis. Clin Exp Immunol 152:415–422
Winyard PG, Ryan B, Eggleton P, Nissim A, Taylor E, Lo Faro ML, Burkholz T, Szabó-Taylor KE, Fox B, Viner N, Haigh RC, Benjamin N, Jones AM, Whiteman M (2011) Measurement and meaning of markers of reactive species of oxygen, nitrogen and sulfur in healthy human subjects and patients with inflammatory joint disease. Biochem Soc Trans 39:1226–1232
Hadjigogos K (2003) The role of free radicals in the pathogenesis of rheumatoid arthritis. Panminerva Med 45:7–13
Vasanthi P, Nalini G, Rajasekhar G (2009) Status of oxidative stress in rheumatoid arthritis. Int J Rheum Dis 12(1):29–33
Nagy G, Koncz A, Telarico T, Fernandez D, Ersek B, Buzás E, Perl A (2010) Central role of nitric oxide in the pathogenesis of rheumatoid arthritis and systemic lupus erythematosus. Arthritis Res Ther 12(3):210
Universidade Federal do Rio Grande do Sul, Onur O, Akinci AS, Akbiyik F, Unsal I (2001) Elevated levels of nitrate in rheumatoid arthritis. Rheumatol Int 20:154–158
Choi JW (2003) Nitric oxide production is increased in patients with rheumatoid arthritis but does not correlate with laboratory parameters of disease activity. Clin Chim Acta 336:83–87
Cimen MY, Cimen OB, Kacmaz M, Ozturk HS, Yorgancioglu R, Durak I (2000) Oxidant/antioxidant status of the erythrocytes from patients with rheumatoid arthritis. Clin Rheumatol 19:275–277
Nivsarkar M (2000) Improvement in circulating superoxide dismutase levels: role of nonsteroidal anti-inflammatory drugs in rheumatoid arthritis. Biochem Biophys Res Commun 270:714–716
Afonso V, Champy R, Mitrovic D, Collin P, Lomri A (2007) Reactive oxygen species and superoxide dismutases: role in joint diseases. Joint Bone Spine 74:324–329
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Aletaha D, Neogi T, SIlman A, Funovits J, Felson DT et al (2010) 2010 rheumatoid arthritis classification criteria: an America college of rhuematology/European League against Rheumatism collaborative initiative. Ann Rheum Dis 69:1580–1588
Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48
Hirao M, Yamasaki N, Oze H, Ebina K, Nampei A, Kawato Y, Shi K, Yoshikawa H, Nishimoto N, Hashimoto J (2012) Serum level of oxidative stress marker is dramatically low in patients with rheumatoid arthritis treated with tocilizumab. Rheumatol Int 32(12):4041–4045
Hjeltnes G, Hollan I, Førre Ø, Wiik A, Lyberg T, Mikkelsen K, Agewall S (2012) Relations of serum COMP to cardiovascular risk factors and endothelial function in patients with rheumatoid arthritis treated with methotrexate and TNF-α inhibitors. J Rheumatol 39(7):1341–1347
Auclair C, Voisin E (1985) Nitroblue tetrazolium reduction. In: Greenvvald RA (ed) Handbook of methods for oxygen radical research. CRC Press, Boka Raton, pp 123–132
Pick E, Keisari Y (1980) A simple colorimetric method for the measurement of hydrogen peroxide produced by cells in culture. J Immunol Methods 38:161–170
Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR (1982) Analysis of nitrate, nitrite and [15N] nitrate in biological fluids. Anal Biochem 126:131–138
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
McCord JM, Fridovich I (1969) The utility of superoxide dismutase in studying free radical reactions. I. Radicals generated by the interaction of sulfite, dimethyl sulfoxide, and oxygen. J Biol Chem 244(22):6056–6063
Beutler E (1982) Catalase. In: Beutler E (ed) Red cell metabolism, a manual of biochemical methods. Grune and Stratton, New York, pp 105–106
Misra HP, Fridovich I (1972) The role of superoxide-anion in the autooxidation of epinephrine and a simple assay for superoxide dismutase. J Biol Chem 247:3170–3175
Beutler E (1975) Reduced glutathione—GSH. In: Beutler E (ed) Red cell metabolism: a manual of biochemical methods. Grane and Straton, New York, pp 112–114
Taysi S, Polat F, Gul M, Sari RA, Bakan E (2002) Lipid peroxidation, some extracellular anti-oxidants, and anti-oxidant enzymes in serum of patients with rheumatoid arthritis. Rheumatol Int 21:200–204
Baskol G, Demir H, Baskol M, Kilic E, Ates F, Karakukcu C, Ustdal M (2006) Investigation of protein oxidation and lipid peroxidation in patients with rheumatoid arthritis. Cell Biochem Funct 24(4):307–311
Ueki Y, Miyake S, Tominaga Y, Eguchi K (1996) Increased nitric oxide levels in patients with rheumatoid arthritis. J Rheumatol 23:230–236
Pham TN, Rahman P, Tobin YM, Khraishi MM, Hamilton SF, Alderdice C, Richardson VJ (2003) Elevated serum nitric oxide levels in patients with inflammatory arthritis associated with co-expression of inducible nitricoxide synthase and protein kinase C-eta in peripheral blood monocyte derived macrophages. J Rheumatol 30:2529–2534
Jikimoto T, Nishikubo Y, Koshiba M et al (2002) Thioredoxin as a biomarker for oxidative stress in patients with rheumatoid arthritis. Mol Immunol 38:765–772
Kundu S, Ghosh P, Datta S, Ghosh A, Chattopadhyay S, Chatterjee M (2012) Oxidative stress as a potential biomarker for determining disease activity in patients with rheumatoid arthritis. Free Radical Res 46(12):1482–1489
Hassan SZ, Gheita TA, Kenawy SA, Fahim AT, El-Sorougy IM, Abdou MS (2011) Oxidative stress in systemic lupus erythematosus and rheumatoid arthritis patients: relationship to disease manifestations and activity. Int J Rheum Dis 14(4):325–331
Altindag O, Karakoc M, Kocyigit A, Celik H, Soran N (2007) Increased DNA damage and oxidative stress in patients with rheumatoid arthritis. Clin Biochem 40:167–171
Karatas F, Ozates I, Canatan H, Halifeoglu I, Karatepe M, Colakt R (2003) Antioxidant status and lipid peroxidation in patients with rheumatoid arthritis. Indian J Med Res 118:178–181
Mazzetti I, Grigolo B, Borzì RM, Meliconi R, Facchini A (1996) Serum copper/zinc superoxide dismutase levels in patients with rheumatoid arthritis. Int J Clin Lab Res 26(4):245–249
Kalpakcioglu B, Senel K (2008) The interrelation of glutathione reductase, catalase, glutathione peroxidase, superoxide dismutase, and glucose-6-phosphate in the pathogenesis of rheumatoid arthritis. Clin Rheumatol 27(2):141–145
De Leo ME, Tranghese A, Passantino M, Mordente A, Lizzio MM, Galeotti T, Zoli A (2002) Manganese superoxide dismutase, glutathione peroxidase, and total radical trapping antioxidant capacity in active rheumatoid arthritis. J Rheumatol 29:2245–2246
Jacobson GA, Ives SJ, Narkowicz C, Jones G (2012) Plasma glutathione peroxidase (GSH-Px) concentration is elevated in rheumatoid arthritis: a case-control study. Clin Rheumatol 31(11):1543–1547
Zelen I, Djurdjevic P, Popovic S, Stojanovic M, Jakovljevic V, Radivojevic S, Baskic D, Arsenijevic N (2010) Antioxidant enzymes activities and plasma levels of oxidative stress markers in B-chronic lymphocytic leukemia patients. J BUON 15(2):330–336
Acknowledgments
This work is supported by Grant no. 175043 from the Ministry of Science and Technical Development of the Republic of Serbia.
Conflict of interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Veselinovic, M., Barudzic, N., Vuletic, M. et al. Oxidative stress in rheumatoid arthritis patients: relationship to diseases activity. Mol Cell Biochem 391, 225–232 (2014). https://doi.org/10.1007/s11010-014-2006-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-014-2006-6