Abstract
Plasma glutathione peroxidase (GSH-Px) by enzyme-linked immunosorbent assay (ELISA) offers a complimentary measurement approach to traditional GSH-Px activity methods. The aim was to investigate whether GSH-Px measured by ELISA in rheumatoid arthritis patients was elevated compared to controls. This was a case–control study with rheumatoid arthritis patients recruited from private practice and gender and age-matched controls randomly selected from the electoral role. GSH-Px concentration was measured by ELISA. Plasma malondialdehyde was used as a measure of oxidative stress, and antioxidant capacity was measured based on reduction of Cu++ to Cu+ by antioxidants in the sample. Disease severity was measured using the Health Assessment Questionnaire-Disability Index (HAQ-DI) and C-reactive protein was measured using an immunoturbidometric method. A total of 74 patients were recruited, consisting of 35 rheumatoid arthritis cases and 39 healthy controls. There were no differences between rheumatoid arthritis cases and controls for oxidative stress and antioxidant capacity; however, GSH-Px concentration was markedly elevated in the rheumatoid arthritis sufferers (85.9 ± 147.7 versus 17.3 ± 13.0 mg/L, respectively; mean ± SD; p < 0.01). GSH-Px levels were not associated with severity measured by the HAQ-DI or C-reactive protein. Patients with rheumatoid arthritis demonstrated increased GSH-Px consistent with an adaptive upregulation of GSH-Px to protect against oxidative stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Enzymatic antioxidants include superoxide dismutases, catalase and selenium-dependent glutathione peroxidase (GSH-Px) [1]. GSH-Px is the most abundant and appears to have a major role in reactive oxygen species (ROS) defences based on in vitro studies [2]. Plasma GSH-Px is made up of four subunits, each of 22 kDa precursors with the incorporated Se present as selenocysteine and a glycosylated N-terminal region [3, 4]. Plasma GSH-Px makes up around 20 % of total selenium based on high-performance liquid chromatography–inductively coupled plasma mass spectrometry and column chromatography methods [5, 6]. The importance of selenium and selenoproteins such as GSH-Px to human health has been well-documented [7].
There is good evidence that ROS play an important role as secondary messengers in inflammatory and immunological cellular response in rheumatoid arthritis and osteoarthritis as well as direct involvement in cartilage degradation [8]. Investigation of nitric oxide-induced cell death in chondrocytes and osteoarthritis synoviocytes is dependent on the presence of ROS which appears to be a major factor in both chondrocyte [9, 10] and synoviocyte cell death [11]. Chondrocyte lipid peroxidation and cartilage matrix protein (collagen) oxidation and degradation appear to be linked [12]. Data reported by Seutens et al. [13] support the hypothesis that Kashin–Beck disease, an endemic osteoarthropathy associated with low Se status, occurs as a consequence of oxidative damage to cartilage and bone cells when associated with decreased antioxidant defence. In support of this hypothesis, cartilage changes have been demonstrated with selenium deficiency in mice and rats [14, 15].
In rheumatoid arthritis, inflammation of the joint tissues is associated with the release of toxic substances in the synovium which leads to cartilage destruction [16]. Selenium and its role in rheumatoid arthritis are controversial as there have been few well-designed studies. It has been reported previously that selenium in plasma is lower in patients with rheumatoid arthritis [17], and a study in Finland with a cohort of 18,709 followed for 11–16 years examined the development of rheumatoid arthritis and found that low selenium status may be a risk factor for rheumatoid factor-negative rheumatoid arthritis [18]. Despite this, selenium supplementation has not been of benefit in a small and most likely underpowered trial in rheumatoid arthritis [19, 20], and the general consensus is that there is currently no convincing evidence that selenium supplementation is effective [21].
Previous work in our laboratory has focused on selenium status and the potential role of GSH-Px levels measured by enzyme-linked immunosorbent assay (ELISA) rather than GSH-Px activity as a measure of antioxidant pathogenesis. GSH-Px levels by ELISA have been found to be correlated with selenium status in healthy populations, but at levels above that expected, consistent with cross-reactivity of ELISA antibodies binding to a GSH-Px epitope preserved during various states of GSH-Px synthesis and degradation [22]. In patients with acute severe asthma with demonstrated increased oxidative stress, GSH-Px concentration measured by ELISA was elevated in severe asthma whereas GSH-Px activity was not [23]. These results were consistent with an adaptive upregulation and turnover of GSH-Px to protect against oxidative stress. Although several studies have investigated GSH-Px activity, plasma GSH-Px concentrations by ELISA have not previously been reported in rheumatoid arthritis, which may provide a better insight into the role of GSH-Px in rheumatoid arthritis. Given that GSH-Px concentrations measured by ELISA appear to offer some advantages over measurement of GSH-Px activity [22], the aim of this study was to investigate whether GSH-Px levels measured by ELISA in rheumatoid arthritis patients were elevated compared to healthy controls.
Patients and methods
Subject recruitment
Rheumatoid arthritis patients aged between 50 and 80 years were recruited consecutively from rheumatology private practices as part of normal clinical presentations. Eligibility was based on clinical assessment by a clinician (musculoskeletal specialist) with a diagnosis of rheumatoid arthritis, symptomatic for over 3 months. Controls, matched by gender and 5-year age bands, were selected from the Tasmanian Older Adult Cohort (TASOAC) study, an ongoing, prospective, population-based study in 1,100 subjects aged between 50 and 79 years randomly selected from the electoral role in Southern Tasmania (population 229,000). The aim of TASOAC was to identify the environmental, genetic and biochemical factors associated with the development and progression of osteoarthritis and osteoporosis (the overall response rate was 57 %). Institutionalised persons were excluded. Written informed consent was obtained. Age, gender and body mass index were recorded and blood samples were collected, and the plasma was harvested and frozen at −80 °C until analysis. The study was approved by the Human Research Ethics Committee (Tasmania) Network in accordance with the Helsinki Declaration.
Disability index
The Health Assessment Questionnaire-Disability Index (HAQ-DI) [24] was self-administered by rheumatoid arthritis patients at the time of recruitment. The HAQ-DI is a condition-specific measure of functional status (scale 0–3) consisting of 20 items across eight daily living activities, resulting in a score range of 0 (no disability) to 3 (severe disability) [25]. This tool was first reported in 1980, and since then, it has been well-validated in a number of studies of rheumatoid arthritis including observational studies and clinical trials [25].
C-reactive protein
C-reactive protein levels were measured in rheumatoid arthritis patients. C-reactive protein is released into the circulatory system in response to pro-inflammatory stimuli. C-reactive protein was measured in plasma using an immunoturbidometric method (ARCHITECT c Systems™; Abbott Diagnostics, Abbott Park, IL, USA) by Pathology Services at the Royal Hobart Hospital. C-reactive protein laboratory tests are commonly used in rheumatoid arthritis; however, there are well-recognised limitations. Although C-reactive protein can be useful to monitor patients, many patients will have C-reactive protein results within normal ranges [26], with the reference range 0.1 to 8.2 mg/L for the assay used in this study [27]. In general, laboratory diagnostic tests should not be considered a gold standard for diagnosis and management of rheumatoid arthritis [28].
Oxidative stress
Plasma malondialdehyde (MDA) was used as a measure of oxidative stress based on the detection of the MDA–thiobarbituric acid adduct by HPLC. The MDA analysis was performed using a modification of the method employed by Li et al. [29] and previously used in our laboratory [23].
Antioxidant capacity
Total antioxidant capacity was measured by microplate assay using a commercial total antioxidant capacity kit (Total Antioxidant Power, Oxford Biomedical Research, Rochester Hills, MI, USA) according to manufacturer’s instruction. The assay is based on reduction of Cu++ to Cu+ by antioxidants in the sample, which selectively binds to a chromogenic reagent with absorption read at 490 nm. Samples were measured in duplicate.
Glutathione peroxidase by ELISA
Plasma GSH-Px was measured by a commercial ELISA kit (Bioxytech® Plasma GSH-Px Enzyme Immunoassay™; Oxis Research, Portland, OR, USA) according to manufacturer’s instructions with the absorbance read using a microplate reader (Model 680 Microplate Reader; Bio-Rad Laboratories Inc., Sydney, Australia). Samples were diluted 1:200 with sample buffer and analysed in duplicate. Diluted samples outside the calibration range of 4.7–300 ng/mL were reanalysed with appropriate dilution.
Assay performance
For C-reactive protein, typical assay performance was a lower limit of quantification (LLoQ) of 5.0 mg/L based on a relative standard deviation (RSD) = 20 % and RSD less than 5 % over the assay range [27]. The oxidative stress assay (plasma MDA) demonstrated acceptable performance with a linear calibration curve (r 2 = 0.991) over the range 0.1 to 5.0 μmol/L, an intra-assay precision RSD of 1.0 % and accuracy of +14 % (n = 4 at the 1.0 μmol/L level) and a LLoQ of 0.1 μmol/L. Within batch antioxidant capacity, assay precision measured by copper reducing equivalents was less than 5 % RSD. The plasma GSH-Px ELISA batch assay precision (%RSD) was 3.6 %.
Statistical analysis
Comparisons between patients with rheumatoid arthritis and healthy controls for basic demographics, plasma antioxidative capacity, selenium, oxidative stress and GSH-Px levels by ELISA were made using two-tailed unpaired Student’s t test. With previous reported levels (mean ± SD) of plasma GSH-Px in healthy adults of 13.8 ± 7.3 μg/mL [23], with two-sided alpha = 0.05 and beta = 0.20, based on a sample size of 30 in each group, a difference of 5.2 μg/mL could be detected.
Linear regression between GSH-Px levels measured by ELISA and oxidative stress (plasma MDA) was investigated. Furthermore, in rheumatoid arthritis patients, relationships between severity measures (HAQ-DI and C-reactive proteins) and GSH-Px by ELISA were investigated, as well as the relationship between C-reactive protein and oxidative stress (plasma MDA) by linear regression. Results with p < 0.05 were considered statistically significant. Analyses were performed with JMP software for Macintosh version 6 (SAS Institute Inc, Cary, NC, USA).
Results
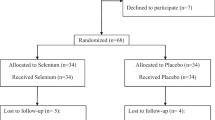
A total of 74 subjects were recruited in the study consisting of 35 rheumatoid arthritis patients and 39 controls. Basic demographics are shown in Table 1. There were no differences in age, weight, height and body mass index between cases and controls for both males and females.
GSH-Px levels, oxidative stress and antioxidant capacity
There were no differences between rheumatoid patients and controls for oxidative stress or antioxidant capacity; however, GSH-Px levels were markedly elevated in rheumatoid cases compared to controls (p < 0.01) as shown in Table 2 (mean ± SD; 85.9 ± 147.7 versus 17.3 ± 13.0 μg/mL, respectively). In controls, levels ranged from 3.3 to 80.1 μg/mL; however, in rheumatoid patients, GSH-Px levels ranged from 10.2 to 714 μg/mL with six patients above 100 μg/mL.
There were no differences between males and females except for antioxidant capacity where male rheumatoid patients had higher mean (±SD) capacity than controls (1,467 ± 467 versus 1,094 ± 486, respectively, p < 0.05). There were no relationships between GSH-Px levels and either antioxidant capacity (r 2 = 0.000, p = 0.93) or oxidative stress (r 2 = 0.002, p = 0.75) for rheumatoid arthritis cases or controls.
GSH-Px levels and rheumatoid arthritis severity
Mean (±SD) C-reactive protein was 7.3 ± 9.7 mg/L and mean (±SD) HAQ-DI score was 1.77 ± 0.73 as shown in Table 2. There were no relationships between GSH-Px levels and severity with either the HAQ-DI (r 2 = 0.019, p = 0.45) or C-reactive protein measures (r 2 = 0.003, p = 0.76). Likewise, there was no relationship between oxidative stress and C-reactive protein (r 2 = 0.011, p = 0.56).
Discussion
Surprisingly, the role of GSH-Px in rheumatoid arthritis (RA) is still not clear after several decades of research into selenoproteins. It is evident from our current work that plasma GSH-Px may play a role in the pathogenesis of rheumatoid arthritis given the elevated levels and clearly warrants further investigation. When considering previous research, it is firstly important to note the difference between GSH-Px activity and GSH-Px concentration measured by ELISA which appears to include GSH-Px-associated cross-reactive proteins. Methods based on ELISA rely on polyclonal antibodies binding to a GSH-Px epitope which may potentially be preserved in various states of GSH-Px synthesis and degradation and be affected by disease state. Multiple proteins detected using 1D and 2D-PAGE which appear to vary between GSH-Px status support this argument [22]. The ELISA approach has the advantage of measuring GSH-Px and associated cross-reactive proteins indicative of turnover under oxidative stress, which may not be observed by measuring GSH-Px activity as this may be under homeostatic regulation. However, this non-specific cross-reactivity could also be disadvantageous with many different unknown determinants of levels and GSH-Px synthesis and degradation proteins [22]. Sustained GSH-Px upregulation under conditions of acute oxidative stress such as RA could lead to GSH-Px activity remaining relatively static, whereas increased turnover of GSH-Px would be reflected by increased levels by ELISA. Relatively constant markers of oxidative stress and oxidative capacity in our current study support this argument of homeostatic regulation.
Similar effects have been shown in antioxidant status under extreme endurance stress in athletes that support this argument. Exercise increases oxidative stress and is associated with changes in antioxidant profiles [30]; however, GSH-Px activity and selenium measured in runners before and after a marathon have been shown to remain relatively unchanged [31]. Over time, it would be reasonable to hypothesise that the upregulation of GSH-Px and demand for selenium would lower total selenium levels. In a small investigation by Tarp et al. [20], patients with RA were found to have lower levels of GSH-Px activity which was corrected with selenium supplementation. Serum selenium (of which GSH-Px makes up approximately 20 %) [5, 6] was found to be significantly lower in patients with active RA over longer periods [32] suggesting some form of depletion, and most compelling, this finding was repeated in a later investigation in which selenium was decreased during periods of high disease activity [33]. Again, these findings are consistent with an increased turnover of GSH-Px during oxidative stress, as found in our current study where GSH-Px and associated cross-reactive proteins were increased. Furthermore, a compensatory GSH-Px mechanism and selenium demand could partially explain previous apparent conflicting results concerning GSH-Px activity and the therapeutic role of selenium in RA. A limitation of the current study is the lack of disease activity score, inflammatory markers, autoantibody status and erosive status, and a larger selenium supplementation intervention study incorporating these measures is now planned.
In conclusion, GSH-Px measured by ELISA has advantages over GSH-Px activity, particularly if homeostatic control of GSH-Px occurs. Using ELISA, patients with rheumatoid arthritis demonstrated increased GSH-Px concentrations which strongly suggest an important role for GSH-Px in disease pathogenesis. At this point, the beneficial effects of selenium supplementation in RA still remain unclear, but our finding of increased GSH-Px levels in RA clearly indicates that more comprehensive investigations to elucidate the role of selenium and the fate of GSH-Px in acute oxidative stress diseases such as RA are warranted.
References
Rahman I, Biswas SK, Kode A (2006) Oxidant and antioxidant balance in the airways and airway diseases. Eur J Pharmacol 533(1–3):222–239
Raes M, Michiels C, Remacle J (1987) Comparative study of the enzymatic defense systems against oxygen-derived free radicals: the key role of glutathione peroxidase. Free Radic Biol Med 3(1):3–7
Maddipati KR, Marnett LJ (1987) Characterization of the major hydroperoxide-reducing activity of human plasma. Purification and properties of a selenium-dependent glutathione peroxidase. J Biol Chem 262(36):17398–17403
Takahashi K, Avissar N, Whitin J, Cohen H (1987) Purification and characterization of human plasma glutathione peroxidase: a selenoglycoprotein distinct from the known cellular enzyme. Arch Biochem Biophys 256(2):677–686
Reyes LH, Marchante-Gayon JM, Alonso JIG, Sanz-Medel A (2003) Quantitative speciation of selenium in human serum by affinity chromatography coupled to post-column isotope dilution analysis ICP-MS. J Anal At Spectrom 18(10):1210–1216
Deagen JT, Butler JA, Zachara BA, Whanger PD (1993) Determination of the distribution of selenium between glutathione peroxidase, selenoprotein P, and albumin in plasma. Anal Biochem 208(1):176–181
Brown KM, Arthur JR (2001) Selenium, selenoproteins and human health: a review. Public Health Nutr 4(2B):593–599
Henrotin YE, Bruckner P, Pujol JP (2003) The role of reactive oxygen species in homeostasis and degradation of cartilage. Osteoarthr Cartil 11(10):747–755
Del Carlo M Jr, Loeser RF (2002) Nitric oxide-mediated chondrocyte cell death requires the generation of additional reactive oxygen species. Arthritis Rheum 46(2):394–403
Tiku ML, Gupta S, Deshmukh DR (1999) Aggrecan degradation in chondrocytes is mediated by reactive oxygen species and protected by antioxidants. Free Radic Res 30(5):395–405
Jovanovic DV, Mineau F, Notoya K, Reboul P, Martel-Pelletier J, Pelletier JP (2002) Nitric oxide induced cell death in human osteoarthritic synoviocytes is mediated by tyrosine kinase activation and hydrogen peroxide and/or superoxide formation. J Rheumatol 29(10):2165–2175
Tiku ML, Shah R, Allison GT (2000) Evidence linking chondrocyte lipid peroxidation to cartilage matrix protein degradation. Possible role in cartilage aging and the pathogenesis of osteoarthritis. J Biol Chem 275(26):20069–20076
Suetens C, Moreno-Reyes R, Chasseur C et al (2001) Epidemiological support for a multifactorial aetiology of Kashin–Beck disease in Tibet. Int Orthop 25(3):180–187
Yang C, Wolf E, Roser K, Delling G, Muller PK (1993) Selenium deficiency and fulvic acid supplementation induces fibrosis of cartilage and disturbs subchondral ossification in knee joints of mice: an animal model study of Kashin–Beck disease. Virchows Arch A Pathol Anat Histopathol 423(6):483–491
Sasaki S, Iwata H, Ishiguro N, Habuchi O, Miura T (1994) Low-selenium diet, bone, and articular cartilage in rats. Nutrition 10(6):538–543
Darlington LG, Stone TW (2001) Antioxidants and fatty acids in the amelioration of rheumatoid arthritis and related disorders. Br J Nutr 85(3):251–269
Aaseth J, Munthe E, Forre O, Steinnes E (1978) Trace elements in serum and urine of patients with rheumatoid arthritis. Scand J Rheumatol 7(4):237–240
Knekt P, Heliovaara M, Aho K, Alfthan G, Marniemi J, Aromaa A (2000) Serum selenium, serum alpha-tocopherol, and the risk of rheumatoid arthritis. Epidemiology 11(4):402–405
Peretz A, Siderova V, Neve J (2001) Selenium supplementation in rheumatoid arthritis investigated in a double blind, placebo-controlled trial. Scand J Rheumatol 30(4):208–212
Tarp U, Hansen JC, Overvad K, Thorling EB, Tarp BD, Graudal H (1987) Glutathione peroxidase activity in patients with rheumatoid arthritis and in normal subjects: effects of long-term selenium supplementation. Arthritis Rheum 30(10):1162–1166
Canter PH, Wider B, Ernst E (2007) The antioxidant vitamins A, C, E and selenium in the treatment of arthritis: a systematic review of randomized clinical trials. Rheumatology (Oxford) 46(8):1223–1233
Jacobson GA, Narkowicz C, Tong YC, Peterson GM (2006) Plasma glutathione peroxidase by ELISA and relationship to selenium level. Clin Chim Acta 369(1):100–103
Jacobson GA, Yee KC, Ng CH (2007) Elevated plasma glutathione peroxidase concentration in acute severe asthma: comparison with plasma glutathione peroxidase activity, selenium and malondialdehyde. Scand J Clin Lab Invest 67(4):423–430
Fries JF, Spitz P, Kraines RG, Holman HR (1980) Measurement of patient outcome in arthritis. Arthritis Rheum 23(2):137–145
Cole JC, Motivala SJ, Khanna D, Lee JY, Paulus HE, Irwin MR (2005) Validation of single-factor structure and scoring protocol for the Health Assessment Questionnaire-Disability Index. Arthritis Rheum 53(4):536–542
Sokka T, Pincus T (2009) Erythrocyte sedimentation rate, C-reactive protein, or rheumatoid factor are normal at presentation in 35%–45% of patients with rheumatoid arthritis seen between 1980 and 2004: analyses from Finland and the United States. J Rheumatol 36(7):1387–1390
Anonymous. C-Reactive protein. Ref 8G65-21, Dec 2008. ARCHITECT c Systems. Abbott Diagnostics, Abbott Park, IL, USA
Pincus T, Sokka T (2009) Laboratory tests to assess patients with rheumatoid arthritis: advantages and limitations. Rheum Dis Clin N Am 35(4):731–734, vi–vii
Li K, Shang X, Chen Y (2004) High-performance liquid chromatographic detection of lipid peroxidation in human seminal plasma and its application to male infertility. Clin Chim Acta 346(2):199–203
Finaud J, Lac G, Filaire E (2006) Oxidative stress: relationship with exercise and training. Sports Med 36(4):327–358
Rokitzki L, Logemann E, Sagredos AN, Murphy M, Wetzel-Roth W, Keul J (1994) Lipid peroxidation and antioxidative vitamins under extreme endurance stress. Acta Physiol Scand 151(2):149–158
Tarp U, Overvad K, Hansen JC, Thorling EB (1985) Low selenium level in severe rheumatoid arthritis. Scand J Rheumatol 14(2):97–101
Tarp U, Graudal H, Overvad K, Thorling EB, Hansen JC (1989) Selenium in rheumatoid arthritis. A historical prospective approach. J Trace Elem Electrolyte Health Dis 3(2):93–95
Acknowledgments
The authors wish to thank Catrina Boon for assistance with the provision of stored samples. This work was supported by the School of Pharmacy as part of a student project. TASOAC was funded by NHMRC and Arthritis Australia.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jacobson, G.A., Ives, S.J., Narkowicz, C. et al. Plasma glutathione peroxidase (GSH-Px) concentration is elevated in rheumatoid arthritis: a case–control study. Clin Rheumatol 31, 1543–1547 (2012). https://doi.org/10.1007/s10067-012-2046-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-012-2046-9