Abstract
Familial Hypertrophic Cardiomyopathy (FHC) is an autosomal dominant disorder affecting the cardiac muscle and exhibits varied clinical symptoms because of genetic heterogeneity. Several disease causing genes have been identified and most code for sarcomere proteins. In the current study, we have carried out clinical and molecular analysis of FHC patients from India. FHC was detected using echocardiography and by analysis of clinical symptoms and family history. Disease causing mutations in the β-cardiac myosin heavy chain (MYH7) and Myosin binding protein C3 (MYBPC3) genes were identified using Polymerase Chain Reaction-Deoxyribose Nucleic Acid (PCR-DNA) sequencing. Of the 55 patient samples screened, mutations were detected in only nineteen in the two genes; MYBPC3 mutations were identified in 12 patients while MYH7 mutations were identified in five, two patients exhibited double heterozygosity. All four MYH7 mutations were missense mutations, whereas only 3/9 MYPBC3 mutations were missense mutations. Four novel mutations in MYBPC3 viz. c.456delC, c.2128G>A (p.E710K), c.3641G>A (p.W1214X), and c.3656T>C (p.L1219P) and one in MYH7 viz. c.965C>T (p.S322F) were identified. A majority of missense mutations affected conserved amino acid residues and were predicted to alter the structure of the corresponding mutant proteins. The study has revealed a greater frequency of occurrence of MYBPC3 mutations when compared to MYH7 mutations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Familial Hypertrophic Cardiomyopathy (FHC) is an autosomal dominant disorder affecting the cardiac sarcomere and is characterized by myocardial hypertrophy and myocyte disarray. FHC is estimated to affect one in every 500 individuals [1] and more importantly appears to be the most common cause of sudden cardiac death in otherwise healthy young individuals [2]. An important feature of FHC is its extensive clinical heterogeneity ranging from death within the first three decades of life to almost complete absence of significant clinical symptoms [3]. At least thirteen disease causing genes for FHC have been identified to date [4, 5]; nearly all coding for sarcomere proteins. This genetic heterogeneity has been proposed to be the main cause for the underlying clinical heterogeneity. The β-cardiac myosin heavy chain (MYH7) and Myosin binding protein C3 (MYBPC3) genes are estimated to account for about 60–70% of all FHC cases [6]. MYH7 was the first (and perhaps the most common) FHC gene to be identified, with more than 500 mutations reported till date. Mutations in MYH7 and in the gene coding for Troponin T2 (TnnT2; the third major FHC gene) appear to often result in severe symptoms including death at a young age [7, 8]. MYBPC3 mutations, however, usually result in delayed onset of symptoms [9]. In addition, the presence of more than one mutation in the same (compound heterozygosity) or different (double heterozygosity) genes has been documented in a significant proportion of FHC patients [10]. The insertion/deletion (I/D) polymorphism of the gene coding for the angiotensin-1 converting enzyme (ace) has often been linked to severe hypertrophy among FHC patients [11], though other studies have also revealed no significant association [12]. Given the wide allelic heterogeneity and rarity of recurrent mutations, it is important to determine the mutation spectrum in any given population to facilitate studies on genotype–phenotype correlation. We earlier commenced analysis of disease causing mutations in Indian FHC patients [13, 14]. In the current study, we have analyzed 55 FHC patients from India and the results indicate that mutations in MYH7 and MYBPC3 may not be as frequent as reported in other populations.
Materials and methods
Patients and samples
Eighty patients, all from the State of Andhra Pradesh in India, were included in the study. Fifty-five presented at one of the two collaborating hospitals viz. the Usha Mullapudi Cardiac Centre, Hyderabad and Care hospital, Hyderabad. Remaining 25 patients were from remote areas and presented at associated clinics of the collaborating hospitals. The study was approved by the ethics committees of the respective hospitals as per the Helsinki declaration of 1975. FHC diagnosis was based mainly on echocardiography, ECG, and family history as reported earlier [14]. One hundred age and gender matched normal individuals were recruited from the local population for the study. Blood samples were collected from each patient, family members, and normal asymptomatic individuals following informed consent. Unfortunately, samples collected for 25 patients (from remote areas) were insufficient for complete genetic analysis of the two genes.
Genetic analysis
We performed mutation screening in 55 patient samples, though ace polymorphism analysis was completed for all 80 samples. Screening for mutations in MYH7 and MYBPC3 genes was performed as described earlier using Polymerase Chain Reaction-Deoxyribose Nucleic Acid (PCR-DNA) sequencing [14]. The sequence of primers for both genes and corresponding annealing temperatures for PCR are given in Table S1. All mutations were validated by bi-directional DNA sequencing and each novel mutation was confirmed to be absent in at least 100 normal individuals. Analysis of the ace I/D polymorphism was carried out as described earlier [13, 14], on all 80 patient samples.
Sequence and structure analysis
Multiple sequence alignments (MSAs) for several orthologues of the human MYBPC3 and MYH7 proteins (Figs. S1 and S2, respectively), identified by PSI-BLAST searches against the non-redundant database, were obtained by using ClustalW (http://www.ebi.ac.uk/clustalw). The MSAs were used for calculating the position-specific Gribskov score using the Prophecy program available as part of the EMBOSS package [15]. X-ray or NMR structures for the human MYH7 are not yet available. Since the human MYH7 (N-terminal amino acids 14–842) shows significant sequence identity (63%) with Scallop myosin S1, whose crystal structure with bound ADP is available (PDB ID: 1QVI), we modeled the human MYH7 with bound ADP by employing comparative modeling procedures using the scallop myosin structure as the template. Sequence alignment of human MYH7 and scallop myosin was carried out using ClustalW. A comparative model was built using Modeller 9v5 [16] (http://salilab.org/modeller); the model with the best PROCHECK [17] G-score (overall G-score = −0.05) and VERIFY-3D [18] profile was subjected to energy minimization using the GROMACS [19] program package (http://www.gromacs.org) adopting the GROMOS96 43a1 force field parameters and steepest descent method.
Human MYBPC3 comprises of seven Immunoglobulin (Ig)-like (C1–C5, C8, and C10) and three Fibronectin type III (C6, C7, and C9) globular domains [20] but its three dimensional structure (either NMR or X-ray) is not yet available. However, NMR/X-ray structures are available for some individual domains. Since all missense and nonsense mutations identified in this study mapped to the C5 or C10 domains (except one which was a truncation mutation and mapped to the C9 domain), we used the available NMR structure of the C5 domain and a homology model of the C10 domain for structural analysis of the mutations. The C10 domain homology model was built using the Ig domain of Neuroplastin (PDB ID: 2wv3) as the template, identified using FUGUE server (http://tardis.nibio.go.jp/fugue/prfsearch.html) and homology modeling was carried out by Modeller 9v5. The model so obtained was validated using PROCHECK (Overall G-score = −0.14) and Verify-3D.
Results
Eighty patients were diagnosed with FHC in the two hospitals during 2006–2008 and included 63 male and 17 female patients. The low proportion of female patients could be a reflection of socio-economic factors and may not necessarily be a reflection of gender-specific difference in incidence rates. The IVS diameter among patients ranged from 1.3 to 2.7 cm (mean = 1.97 cm). Since MYH7 and MYBPC3 genes have been reported to be the two most common genes causing FHC [6, 7], we proceeded to screen the two genes in 55 FHC patients. We screened the coding region and splice junctions of exons 3–23 of MYH7 since these code for the globular head and neck region of the protein that harbor majority of mutations [21]; while the complete coding region and all splice junctions of the MYBPC3 gene were screened. The MYH7 exon 6 was excluded since it is only 28 bp long and no mutations have been discovered in this exon. Disease-causing mutations were identified in either of the two genes in only nineteen patients (35%) out of which two each harbored double heterozygous and compound heterozygous mutations, respectively. Excluding the patients that harbored compound/double heterozygous mutations, mean age of patients harboring MYBCPC3 mutations (41.7 years) was lower than those harboring MYH7 mutations (47.4 years). The details of mutations and corresponding clinical features for each of the nineteen patients are given in Table 1. Electropherograms for all novel mutations and novel single nucleotide polymorphisms (SNPs) are shown in Fig. 1 and known mutations are shown in Figs. S3A and S3B.
Novel mutations and SNPs detected in MYBPC3 and MYH7 among Indian FHC patients. a c.456delC; b c.2128G>A (p.E710K); c c.3641G>A (p.W1214X); d c.3656T>C (p.L1219P); e c.1790+7G>A (IVS17+7G>A) (SNP); f c.4052delA (SNP), all from MYBPC3, and g c.965C>T (p.S322F) from MYH7. For each, electropherogram showing the mutation is on the left and the one showing the normal sequence is on the right. Each mutant nucleotide is indicated by an arrow; in a and e, the deleted base is indicated in the normal sequence. The MYBPC3 electropherograms for the c.456delC, c.3656T>C, and c.4052delA mutations were obtained from cloned PCR products harboring the heterozygous mutations
MYBPC3 mutations
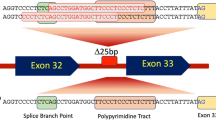
In the current study, MYBPC3 exhibited a higher mutation frequency than MYH7; 12 patients harbored MYBPC3 mutations while only five harbored MYH7 mutations (Table 1). Two patients exhibited double heterozygosity harboring a mutation each in MYH7 and MYBPC3 genes (Table 1). A total of nine MYBPC3 mutations were identified, including four novel mutations viz. c.456delC, c.2128G>A (p.E710K), c.3641G>A (p.W1214X), and c.3656T>C (p.L1219P) (Fig. 1; Table 1). Three mutations viz. c.456delC, c.3656T>C, and c.3628-24_48del25 were confirmed by cloning the corresponding PCR products in the PCR2.1 Topo vector (Invitrogen, USA). The youngest patient in our study was a 3-year old male child who harbored the MYBPC3 c.3372C>A (p.C1124X) mutation; the maternal grandmother of the proband suffered sudden cardiac death. This mutation has been reported earlier [22], but clinical symptoms were not described. Interestingly, the mutation was also detected in the mother and an elder sibling of the proband but both were asymptomatic, though all three harbored the ace I/D genotype (data not shown). The MYBPC3 c.3628-24_48del25 mutation, a common genetic lesion associated with FHC in the Indian population [23], was detected in five patients. Among these, one exhibited compound heterozygosity harboring the additional novel MYBPC3 c.3656T>C mutation (Table 1). A second patient exhibited compound heterozygosity harboring two novel MYBPC3 mutations namely c.2128G>A and c.456delC (Table 1). We identified two novel SNPs in MYBPC3 viz. c.1790+7G>A (IVS17+7G>A) (detected in two patients and in three of 100 normal samples screened; Fig. 1) and c.4052delA, located 227 nucleotides downstream of the stop codon in the 3′ UTR (detected in three patients and in five of 94 normal samples screened; Fig. 1).
MYH7 mutations
MYH7 mutations were detected in only seven patients out of whom two exhibited double heterozygosity (Table 1). Only one novel MYH7 mutation was identified viz. c.965C>T (p.S322F) (Fig. 1; Table 1). Both off springs of the proband (a son aged 21 years and a daughter aged 18 years) harbored the p.S322F mutation but symptoms were absent (data not shown), perhaps indicating late onset. The p.M659I was reported earlier but clinical symptoms were not described [7]. The p.R787H mutation in patient 16 and 17 (Table 1) was reported by us previously [14] and are included in this report, since two additional patients belonging to independent families (patient no. 18 and 19 in Table 1) were detected with the same mutation. Family members of patient 18 and 19 consented for genetic analysis. However, we did not detect any additional member harboring the p.R787H mutation in the respective families (out of 16 members for patient 18 and 26 members for patient 19) indicating the possibility of a de novo origin in these two patients (data not shown).
Status of angiotensin-1 converting enzyme gene I/D polymorphism
The ace gene has been suggested to be an important candidate modifier gene for FHC, based on several earlier studies [24]. We determined the distribution of the two ace alleles in the local population of Andhra Pradesh. Among 91 normal samples (age and gender distribution was comparable to that in patients), 31 harbored the I/I genotype (34%), 51 the I/D genotype (56%), and 9 the D/D genotype (10%). Among 80 symptomatic patient samples screened, 33 harbored the I/I genotype (41%), 35 the I/D genotype (44%), and 12 the D/D genotype (15%). Therefore, the D allele frequency in symptomatic patients (0.37) was not significantly different from that in normals (0.38). The status of ace polymorphism in each of the 19 patients in whom mutation was identified is shown in Table 1.
Sequence and structure analysis
In order to understand the mechanism underlying the pathogenic consequences of missense mutations in the MYH7 and MYBPC3 proteins, sequence and structure analyses of the mutant MYH7 and MYBPC3 proteins were carried out.
MYBPC3 mutations
The MYBPC3 missense mutations detected in this study localize to highly conserved regions (Fig. S1) reflected in the high Gribskov scores for the wild-type residues (Table 2). Each mutant residue, however, exhibited comparatively lower scores (Table 2) indicating non-preference at the respective positions. In addition, we evaluated the effect of each missense and nonsense mutation on the protein by using a recently developed web-server called Hansa (hansa.cdfd.org.in:8080; Acharya and Nagarajaram, communicated). Hansa hosts a recently developed support vector machine based tool for classification of missense mutations into “Disease” and “Neutral” categories. Hansa extracts a set of features associated with missense mutations which include position-specific information, local protein structure information, and intrinsic amino acid properties to classify the missense mutations. Benchmark studies have shown that Hansa outperforms other widely used methods (Acharya and Nagarajaram, communicated). All mutations were predicted as “Disease” (Table 2). MYBPC3 comprises of seven Ig-like (C1–C5, C8, and C10) and three fibronectin type III domains (C6, C7, and C9) [20]. Yeast two-hybrid studies have revealed that domains C5 and C8 as well as C7 and C10 form interacting pairs facilitating trimerization of MYBPC3 protein molecules. Based on this, a model has been suggested wherein three MYBPC3 protein molecules bind serially to form a collar-like structure around the myosin thick filament such that the domains from adjacent MYBPC3 molecules take part in the inter-domain interactions [25]. From this model, it has become clear that the C1124X and W1214X mutant proteins would be devoid of the C10 domain, and therefore may abolish inter-domain interactions thereby compromising myosin binding. The L1219 residue is predicted to reside on the surface of the C10 domain, is exposed, and is likely to participate in C7–C10 interaction. The mutation to Proline at this position is expected to bring about a conformational change at the C7–C10 interface, and hence may not be conducive for inter-domain interactions. Residues E710 and G758 map to the C5 domain whose NMR structure is available [PDB ID: 1GXE; chain A]. E710 is in the conformationally flexible region of the C5 domain and may perhaps be involved in inter-domain interaction with the C10 domain of another MYBPC3 molecule by means of a stabilizing salt-bridge or hydrogen bond interaction. These interactions will be precluded by the mutation to Lysine. The G758 residue occupies the i+3 position of the β turn in one of the β-hairpins in C5 domain. Replacement with Aspartic Acid is expected to destabilize the whole β sheet thereby affecting the intermolecular packing.
MYH7 mutations
The MSAs of human MYH7 with myosin from other species revealed extensive sequence conservation of each amino acid residue exhibiting mutation (Fig. S2) reflected by the corresponding Gribskov scores (Table 2). The Gribskov scores for the mutant amino acid residues were significantly lower (Table 2) indicating that the mutations were not favored at their respective positions. In addition, barring the E710K mutation, all missense mutations were predicted as “Disease” by the Hansa server. The impact of each mutation on protein structure was deduced using a homology model of MYH7 which was built as described in the “Materials and methods” section. MYH7 exhibits actin-dependent ATPase activity and therefore possesses an ADP/ATP binding site characterized by the presence of the Walker motif. MYH7 S322 is located in a loop covering the ADP/ATP binding site such that the S322 side chain hovers around the binding site, and is within 6 Å from the ADP/ATP indicating that S322 may be a part of the ADP/ATP binding region (Fig. 2a). Our model strongly suggests that the S322 polar side chain (i.e., the OH− group) may interact with ADP/ATP and from this perspective the mutated residue (F) becomes unsuitable at this position as it precludes the above said interaction. The other two mutated residues viz. M659 and R663 are located in the actin binding region and are part of the actin–myosin interface (Fig. 2b). It is likely that the two mutations may result in conformational change at the actin binding region, and hence affect actin binding.
a Structure analysis of the MYH7 p.S322F mutation. The nucleotide binding region (NBR) with bound ADP (shown as ball and stick in the centre) is highlighted in the model derived as described in the “Materials and methods” section. The S322 residue (shown as ball and stick at the top) is part of a loop which lies above the NBR. The NBR comprises of I113, Y114, N125-Y130, Y133, I153, G177-V185, N186, R189, E227, N231, D238, N237, N239, S240, S241, S321, D460, I461, G463, and C671 which lie within a distance of 5 Å from ADP. b Structure analysis of the MYH7 p.M659I and p.R663H mutations. Figure shows part of the predicted structure of the MYH7 globular head depicting a part of the actin binding region. The two residues M659 and R663, shown in ball and stick representation, are part of the actin binding region
Discussion
This is perhaps the first analysis of mutation frequency of the two most common genes causing FHC viz. MYH7 and MYBPC3 among Indian patients. A previous study by Tanjore et al. [26] evaluated 95 patient samples but screened only a few selected MYBPC3 exons. Another study included 69 FHC patients but was restricted to genotype–phenotype correlation of only six MYH7 patient mutations [27]. A third study was conducted to determine mutations causing FHC and dilated cardiomyopathy [28] using SSCP, and therefore mutation detection frequency was very low. In addition, the recurrent 25 bp MYBPC3 deletion has earlier been reported from India [23, 29]. A few other studies (including from our own laboratory) were either restricted to very few patients or to a few specific mutations.
In this study, our main objective was to determine whether MYH7 and MYBPC3 were important FHC genes among Indian patients. Surprisingly, mutations in either of the two genes were detected in only 35% of the patients screened indicating perhaps the importance of other disease-causing genes. A recent study from Italy also revealed similar results [30]. Of note, frequency of MYBPC3 mutations was significantly higher than MYH7 among Indian patients (even if the common MYBPC3 c.3628-24_48del25 mutation was excluded from the comparison). In all, we detected nine mutations in MYBPC3 and only four in MYH7 among the nineteen patients (Table 1). Although we did not screen the rod region of MYH7 gene in the current study, only a few mutations are expected to occur in this region, if any. In addition, mutations in the rod region are more likely to cause dilated cardiomyopathy [31]. A recent study from France [32] and an earlier study from eastern Finland [33] also revealed a higher frequency of MYBPC3 mutations compared to MYH7. It would be important to extend this study to a larger sample size and to include patients from other ethnicities within the Indian population to confirm the observation. We are also aware that this study is specific to symptomatic patients, and therefore excludes patients exhibiting sudden cardiac death as well as those that are asymptomatic/pre-symptomatic; the former are usually caused by mutations in MYH7 or TnnT2. Recurrent mutations have been suggested to be rare in FHC; however, out of thirteen mutations identified in this study, five were detected in more than one patient belonging to independent families. The MYBPC3 c.3628-24_48del25 mutation has been reported to occur at a high frequency in the Indian population [23]. It was also suggested that the mutation, in heterozygous form, resulted in incomplete penetrance and low expressivity [29]. In the current study, this mutation was detected in a heterozygous form in five out of 55 patients screened (9%) and all exhibited clinical symptoms (Table 1); one of the five patients also harbored an additional novel MYBPC3 p.L1219P mutation, thereby exhibiting compound heterozygosity. However, we cannot rule out the possibility of presence of mutation in other candidate FHC genes in rest of the four patients. We screened one hundred normal asymptomatic individuals and detected the c.3628-24_48del25 mutation at a frequency of 6%; the p.L1219P mutation was, however not detected.
Five novel mutations were identified in the study; four in MYBPC3 and one in MYH7 (Table 1). For each, absence in at least one hundred normal individuals (200 alleles) was confirmed. The MYBPC3 c.456delC mutation generates a premature termination codon (PTC) located 33 nucleotides upstream of the subsequent exon–exon junction, and therefore is not expected to trigger nonsense mediated decay (NMD) [34]. The resultant truncated protein is, however, expected to be devoid of a major portion of the protein, and therefore will be inactive. The W1214X mutation would result in a truncated protein devoid of the C10 domain which will interfere with trimerization and myosin binding. Among the other two novel MYBPC3 mutations, the p.L1219P mutation is predicted to be a “disease” mutation by the Hansa server; the amino acid substitution results in a drastic reduction in the Gribskov score; and the mutation is expected to affect trimerization of the protein (Table 2). The p.E710K is not predicted to be a “disease” mutation although there is a significant reduction in the Gribskov score for the substituted amino acid (Table 2) and the mutant protein may also be compromised for trimerization. The novel MYH7 mutation p.S322F also results in drastic reduction in Gribskov score for the mutant residue (Table 2) and the mutant protein is expected to be defective in binding ATP/ADP. Taken together, these data provide sufficient evidence in support of the five novel mutations, although it is difficult to associate a novel mutation with FHC without carrying out functional studies, given the existence of several disease causing genes.
All four MYH7 mutations detected in this study were missense mutations. Majority of MYH7 mutations causing hypertrophic cardiomyopathy have been suggested to manifest their effect through a “poison polypeptide” phenomenon [34], thus resulting in a dominant mode of inheritance [23]. In contrast, since most heterozygous MYBPC3 mutations are predicted to trigger NMD leading to reduced mRNA levels, the associated milder symptoms are perhaps because of haploinsufficiency [35]. Of the nine MYBPC3 mutations detected in this study, three occur at consensus splice sequences and are therefore, expected to affect splicing (c.821+1G>A, c.2905+1G>A, and c.3628-24_48del25); three result in a truncated protein (p.W1214X, p.C1124X, and c.456delC); and three are missense mutations (p.G758D, p.E710K, and p.L1219P) which appear to affect key residues in the Ig-like or fibronectin domains and are expected to compromise inter-molecular interactions. Each of the three MYBPC3 truncation mutations result in PTCs located more than 50 nucleotides upstream of the respective subsequent exon–exon junctions and therefore, the respective mutated transcripts may be degraded through NMD [34]. The three mutations affecting splicing can also be predicted to result in generation of PTC because of a change in reading frame as is the case with most splice mutations. Therefore, six out of nine MYBPC3 mutations are expected to cause haploinsufficiency because of loss of transcript through NMD. In addition, we analyzed 417 FHC mutations from the Cardiogenomics database (http://www.cardiogenomics.med.harvard.edu) and from published literature; among 207 MYH7 mutations, 199 were missense mutations (96%), while for MYBPC3 only 87 out of 210 (42%) were missense mutations. Therefore, 58% of MYBPC3 mutations may not result in a “poison polypeptide” providing a possible explanation for the milder symptoms usually associated with this gene. In our study, however, the median age of patients harboring MYBPC3 mutations was lower than those harboring MYH7 mutations; however, no definite conclusions can be drawn given the small numbers analyzed.
The absence of clinical symptoms in family members of the proband (the youngest patient in our study) who harbored the MYBPC3 p.C1124X mutation and also shared the identical I/D ace genotype, indicates a possible role of other modifying genes. The youngest FHC patient reported to date appears to be a 2 years old who harbored an MYH7 mutation [6]. The MYBPC3 p.G758D mutation detected in two patients (Table 1) was reported earlier from the Chinese population; however, details of clinical symptoms were not reported [36].
The novel MYH7 p.S322F mutation is likely to affect ADP/ATP binding, whereas the p.M659I and p.R663H mutations may affect actin–myosin interaction. The p.R787H mutation was detected in four patients including two from our previous study [13]; however, we could not detect a founder effect for this mutation (data not shown). The MYBPC3 missense mutations appear to cause perturbations in the Ig-like domains and are expected to destabilize inter-molecular MYBPC3 interactions thereby compromising binding to the Myosin heavy chain.
Out of 19 patients in whom mutations were identified four patients harbored two mutations each; two exhibited compound heterozygosity, while the other two exhibited double heterozygosity (Table 1), thus yielding a double mutation frequency of about 20%, similar to previous estimates [37]. Given the significant proportion of patients harboring more than one mutation, it may be important to completely screen several FHC genes in each patient, as suggested earlier [4]. Interestingly, the four patients harboring two mutations did not appear to exhibit more severe symptoms as compared to patients harboring a single mutation (Table 1), contrary to previous reports [38].
The present study did not reveal a significant association between the ace D/D genotype and extent of hypertrophy in the patients, similar to our previous results [13, 14], nor was there a significant difference in the D allele frequency in patients and normals. Previous reports have yielded inconsistent association between the D allele frequency and symptomatic FHC patients with varying results for different populations [11, 12]. An earlier study of 118 FHC patients from the northern part of India [39] revealed a significant association of the D allele with patients as compared to controls. Of note, the authors used only one set of primers for genotyping which might increase chances of mistyping of ID genotype as DD [40]. It is also possible that the different ethnicities of patients in the two studies may be the cause for the observed differences in the association.
In conclusion, our analysis of 55 FHC patients has revealed a lower proportion of mutation in the MYH7/MYBPC3 genes than what is reported for other populations. It may therefore be important to screen additional sarcomere coding genes to determine their role in FHC among Indian patients. Sequence and structure analysis of MYH7 missense mutations has revealed that they probably affect actin or nucleotide binding, whereas MYBPC3 mutations either result in the loss of protein expression or may affect protein trimerization ability which in turn may inhibit myosin binding. Our results and analysis of published MYBPC3 mutations also indicate that the milder phenotype usually associated with several MYBPC3 mutations could result from a lack of the dominant “poison polypeptide” phenomenon because of the loss of the mutated gene transcript through NMD.
References
Maron BJ (2002) Hypertrophic cardiomyopathy: a systematic review. JAMA 287:1308–1320
Maron BJ, Epstein SE, Roberts WC (1986) Causes of sudden death in competitive athletes. J Am Coll Cardiol 7:204–214
Alcalai R, Seidman JG, Seidman CE (2008) Genetic basis of hypertrophic cardiomyopathy: from bench to the clinics. J Cardiovasc Electrophysiol 19:104–110
Tsoutsman T, Bagnall RD, Semsarian C (2008) Impact of multiple gene mutations in determining the severity of cardiomyopathy and heart failure. Clin Exp Pharmacol Physiol 35:1349–1357
Morimoto S (2008) Sarcomeric proteins and inherited cardiomyopathies. Cardiovasc Res 77:659–666
Xu Q, Dewey S, Nguyen S, Gomes AV (2010) Malignant and benign mutations in familial cardiomyopathies: insights into mutations linked to complex cardiovascular phenotypes. J Mol Cell Cardiol 48:899–909
Richard P, Charron P, Carrier L, Ledeuil C, Cheav T, Pichereau C, Benaiche A, Isnard R, Dubourg O, Burban M, Gueffet JP, Millaire A, Desnos M, Schwartz K, Hainque B, Komajda M (2003) Hypertrophic cardiomyopathy: distribution of disease genes, spectrum of mutations, and implications for a molecular diagnosis strategy. Circulation 107:2227–2232
Varnava AM, Elliott PM, Baboonian C, Davison F, Davies MJ, McKenna WJ (2001) Hypertrophic cardiomyopathy: histopathological features of sudden death in cardiac troponin T disease. Circulation 104:1380–1384
Niimura H, Bachinski LL, Sangwatanaroj S, Watkins H, Chudley AE, McKenna W, Kristinsson A, Roberts R, Sole M, Maron BJ, Seidman JG, Seidman CE (1998) Mutations in the gene for cardiac myosin-binding protein C and late-onset familial hypertrophic cardiomyopathy. N Engl J Med 338:1248–1257
Ingles J, Doolan A, Chiu C, Seidman J, Seidman C, Semsarian C (2005) Compound and double mutations in patients with hypertrophic cardiomyopathy: implications for genetic testing and counselling. J Med Genet 42:e59
Doolan G, Nguyen L, Chung J, Ingles J, Semsarian C (2004) Progression of left ventricular hypertrophy and the angiotensin-converting enzyme gene polymorphism in hypertrophic cardiomyopathy. Int J Cardiol 96:157–163
Yamada Y, Ichihara S, Fujimura T, Yokota M (1997) Lack of association of polymorphisms of the angiotensin converting enzyme and angiotensinogen genes with nonfamilial hypertrophic or dilated cardiomyopathy. Am J Hypertens 10:921–928
Bashyam MD, Savithri GR, Gopikrishna M, Narasimhan C (2007) A p.R870H mutation in the beta-cardiac myosin heavy chain 7 gene causes familial hypertrophic cardiomyopathy in several members of an Indian family. Can J Cardiol 23:788–790
Purushotham G, Madhumohan K, Anwaruddin M, Nagarajaram H, Hariram V, Narasimhan C, Bashyam MD (2010) The MYH7 p.R787H mutation causes hypertrophic cardiomyopathy in two unrelated families. Exp Clin Cardiol 15:e1–e4
Rice P, Longden I, Bleasby A (2000) EMBOSS: the European molecular biology open software suite. Trends Genet 16:276–277
Sali A, Blundell TL (1993) Comparative protein modelling by satisfaction of spatial restraints. J Mol Biol 234:779–815
Laskowski RA, Moss DS, Thornton JM (1993) Main-chain bond lengths and bond angles in protein structures. J Mol Biol 231:1049–1067
Luthy R, Bowie JU, Eisenberg D (1992) Assessment of protein models with three-dimensional profiles. Nature 356:83–85
Van Der Spoel D, Lindahl E, Hess B, Groenhof G, Mark AE, Berendsen HJ (2005) GROMACS: fast, flexible, and free. J Comput Chem 26:1701–1718
Rybakova IN, Greaser ML, Moss RL (2011) Myosin binding protein C interaction with actin: characterization and mapping of the binding site. J Biol Chem 286:2008–2016
Blair E, Redwood C, de Jesus Oliveira M, Moolman-Smook JC, Brink P, Corfield VA, Ostman-Smith I, Watkins H (2002) Mutations of the light meromyosin domain of the beta-myosin heavy chain rod in hypertrophic cardiomyopathy. Circ Res 90:263–269
Van Driest SL, Vasile VC, Ommen SR, Will ML, Tajik AJ, Gersh BJ, Ackerman MJ (2004) Myosin binding protein C mutations and compound heterozygosity in hypertrophic cardiomyopathy. J Am Coll Cardiol 44:1903–1910
Dhandapany PS, Sadayappan S, Xue Y, Powell GT, Rani DS, Nallari P, Rai TS, Khullar M, Soares P, Bahl A, Tharkan JM, Vaideeswar P, Rathinavel A, Narasimhan C, Ayapati DR, Ayub Q, Mehdi SQ, Oppenheimer S, Richards MB, Price AL, Patterson N, Reich D, Singh L, Tyler-Smith C, Thangaraj K (2009) A common MYBPC3 (cardiac myosin binding protein C) variant associated with cardiomyopathies in South Asia. Nat Genet 41:187–191
Funada A, Konno T, Fujino N, Muramoto A, Hayashi K, Tsubokawa T, Sakata K, Kawashiri MA, Takeda Y, Ino H, Yamagishi M (2010) Impact of renin-angiotensin system polymorphisms on development of systolic dysfunction in hypertrophic cardiomyopathy. Evidence from a study of genotyped patients. Circ J 74:2674–2680
Moolman-Smook J, Flashman E, de Lange W, Li Z, Corfield V, Redwood C, Watkins H (2002) Identification of novel interactions between domains of myosin binding protein-C that are modulated by hypertrophic cardiomyopathy missense mutations. Circ Res 91:704–711
Tanjore RR, Rangaraju A, Kerkar PG, Calambur N, Nallari P (2008) MYBPC3 gene variations in hypertrophic cardiomyopathy patients in India. Can J Cardiol 24:127–130
Rai TS, Ahmad S, Bahl A, Ahuja M, Ahluwalia TS, Singh B, Talwar KK, Khullar M (2009) Genotype phenotype correlations of cardiac beta-myosin heavy chain mutations in Indian patients with hypertrophic and dilated cardiomyopathy. Mol Cell Biochem 321:189–196
Tanjore R, Rangaraju A, Vadapalli S, Remersu S, Narsimhan C, Nallari P (2010) Genetic variations of beta-MYH7 in hypertrophic cardiomyopathy and dilated cardiomyopathy. Indian J Hum Genet 16:67–71
Waldmuller S, Sakthivel S, Saadi AV, Selignow C, Rakesh PG, Golubenko M, Joseph PK, Padmakumar R, Richard P, Schwartz K, Tharakan JM, Rajamanickam C, Vosberg HP (2003) Novel deletions in MYH7 and MYBPC3 identified in Indian families with familial hypertrophic cardiomyopathy. J Mol Cell Cardiol 35:623–636
Roncarati R, Latronico MV, Musumeci B, Aurino S, Torella A, Bang ML, Jotti GS, Puca AA, Volpe M, Nigro V, Autore C, Condorelli G (2011) Unexpectedly low mutation rates in beta-myosin heavy chain and cardiac myosin binding protein genes in italian patients with hypertrophic cardiomyopathy. J Cell Physiol (EPub ahead of print)
Walsh R, Rutland C, Thomas R, Loughna S (2010) Cardiomyopathy: a systematic review of disease-causing mutations in myosin heavy chain 7 and their phenotypic manifestations. Cardiology 115:49–60
Millat G, Bouvagnet P, Chevalier P, Dauphin C, Jouk PS, Da Costa A, Prieur F, Bresson JL, Faivre L, Eicher JC, Chassaing N, Crehalet H, Porcher R, Rodriguez-Lafrasse C, Rousson R (2010) Prevalence and spectrum of mutations in a cohort of 192 unrelated patients with hypertrophic cardiomyopathy. Eur J Med Genet 53:261–267
Jaaskelainen P, Kuusisto J, Miettinen R, Karkkainen P, Karkkainen S, Heikkinen S, Peltola P, Pihlajamaki J, Vauhkonen I, Laakso M (2002) Mutations in the cardiac myosin-binding protein C gene are the predominant cause of familial hypertrophic cardiomyopathy in eastern Finland. J Mol Med 80:412–422
Bashyam MD (2009) Nonsense-mediated decay: linking a basic cellular process to human disease. Expert Rev Mol Diagn 9:299–303
Marston S, Copeland O, Jacques A, Livesey K, Tsang V, McKenna WJ, Jalilzadeh S, Carballo S, Redwood C, Watkins H (2009) Evidence from human myectomy samples that MYBPC3 mutations cause hypertrophic cardiomyopathy through haploinsufficiency. Circ Res 105:219–222
Song L, Zou Y, Wang J, Wang Z, Zhen Y, Lou K, Zhang Q, Wang X, Wang H, Li J, Hui R (2005) Mutations profile in Chinese patients with hypertrophic cardiomyopathy. Clin Chim Acta 351:209–216
Andersen PS, Havndrup O, Hougs L, Sorensen KM, Jensen M, Larsen LA, Hedley P, Thomsen AR, Moolman-Smook J, Christiansen M, Bundgaard H (2009) Diagnostic yield, interpretation, and clinical utility of mutation screening of sarcomere encoding genes in Danish hypertrophic cardiomyopathy patients and relatives. Hum Mutat 30:363–370
Chien KR (2003) Genotype, phenotype: upstairs, downstairs in the family of cardiomyopathies. J Clin Invest 111:175–178
Rai TS, Dhandapany PS, Ahluwalia TS, Bhardwaj M, Bahl A, Talwar KK, Nair K, Rathinavel A, Khullar M (2008) ACE I/D polymorphism in Indian patients with hypertrophic cardiomyopathy and dilated cardiomyopathy. Mol Cell Biochem 311:67–72
Shanmugam V, Sell KW, Saha BK (1993) Mistyping ACE heterozygotes. PCR Methods Appl 3:120–121
Acknowledgments
We are thankful to the patients, their family members and the control subjects for their co-operation in this study. We are thankful to Mr. Chelasani Venkat Reddy for help in making Fig. 2a, b. We are also thankful to Mr. A. S. Raju for critical reading of the manuscript. The study was supported by a grant from the Department of Biotechnology, Government of India (BT/PR6646/MED/12/257/2005) to MDB, and a core grant from the Department of Biotechnology, Government of India to the Centre for DNA Fingerprinting and Diagnostics.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
11010_2011_1077_MOESM1_ESM.doc
Figure S1. Blocks of multiple sequence alignments (MSAs) of human MYBPC3 with orthologues from other species. The MSAs were performed using ClustalW as described in the “Materials and methods” section and only those blocks of MSAs are shown where mutations were detected. The status of residues E710 and G758, C1124, W1214, and L1219 are shown. The sequences are: gi|148342489, Homo sapiens; gi|114326339, Canis lupus familiaris; gi|194217890, Equus caballus; gi|115495853, Bos taurus; gi|297688793, Pongo abelii; gi|297267981, Macaca mulatta; gi|291384958, Oryctolagus cuniculus; gi|134031947, Mus musculus; gi|157824043, Rattus norvegicus; gi|148233421, Xenopus laevis; gi|163915017, Xenopus (Silurana) tropicalis; gi|172072588, Danio rerio; gi|6166593, MYPC3_CHICK (DOC 36 kb)
11010_2011_1077_MOESM2_ESM.doc
Figure S2. Blocks of multiple sequence alignments (MSAs) of human MYH7 with the corresponding myosin chains from other species. The MSAs were performed using ClustalW as described in the “Materials and methods” section and only those blocks of the MSAs are shown that correspond to the regions of interest. The status of residues S322, M659, and R663 are shown. The sequences are: gi|115496169, Homo sapiens; gi|41386711, Bos taurus; gi|125987844, MYH7_PIG; gi|126352320, Equus caballus; gi|297694763, Pongo abelii; gi|296214577, Callithrix jacchus; gi|291403583, Oryctolagus cuniculus; gi|165973990, Canis lupus; gi|3041708, Mesocricetus auratus; gi|18859641, Mus musculus; gi|149063941, Rattus norvegicus; gi|126277437, Monodelphis domestica; gi|281342028, Ailuropoda melanoleuca; gi|297297517, Macaca mulatta; gi|11276954, Coturnix coturnix; gi|50838836, Gallus gallus; gi|148229072, Xenopus laevis; gi|87116414, Cyprinus carpio; gi|189536977, Danio rerio; gi|47208995, Tetraodon nigroviridis; gi|294489339, Oryzias latipes; gi|38347761, Lethenteron japonicum; gi|224074801, Taeniopygia guttata; gi|114669064, Pan troglodytes; gi|55742224, Xenopus (Silurana); gi|171702770, Coryphaenoides acrolepis; gi|171702772, Coryphaenoides cinereus; gi|171702768, Coryphaenoides armatus; gi|171702766, Coryphaenoides yaquinae; gi|134122720, Saurida undosquamis; gi|134122722, Saurida wanieso; gi|9971579, Pennahia argentata; gi|218546789, Sander vitreus; gi|21623523, Oncorhynchus keta; gi|41350446, Siniperca chuatsi; gi|129563832, Siniperca knerii; gi|7209643, Seriola dumerili; gi|15384839, Paracirrhites forsteri; gi|226434435, Takifugu rubripes; gi|160332463, Hypophthalmichthys molitrix; gi|12657354, Notothenia coriiceps (DOC 36 kb)
11010_2011_1077_MOESM3_ESM.tif
Figure S3A. Electropherograms showing known mutations detected in MYBPC3 among Indian FHC patients. A, c.821+1G>A (IVS7+1G>A); B, c.2273G>A (p.G758D); C, c.2905+1G>A (IVS26+1G>A); D, c.3372C>A (p.C1124X); and E, c.3628-24_48del25 (IVS31-24del25). For each, electropherogram showing the mutation is on the left side and the one showing the normal sequence is on the right side. Each mutation is indicated by an arrow; in A, the deleted base is indicated in the normal sequence. The electropherogram for c.3628-24_48del25 was obtained from cloned PCR product. In E, the Bar above the electropherogram for the normal sequence, indicates the 25 nucleotides that are deleted in the patient sample. (TIFF 182 kb)
11010_2011_1077_MOESM4_ESM.tif
Figure S3B. Electropherograms showing known mutations detected in MYH7 among Indian FHC patients. A, c.1977G>A (p.M659I), B, c.1988G>A (p.R663H) and C, c.2360G>A (p.R787H). For each, Electropherogram showing the mutation is on the left side and the one showing the normal sequence is on the right side. Each mutation is indicated by an arrow. (TIFF 150 kb)
Rights and permissions
About this article
Cite this article
Bashyam, M.D., Purushotham, G., Chaudhary, A.K. et al. A low prevalence of MYH7/MYBPC3 mutations among Familial Hypertrophic Cardiomyopathy patients in India. Mol Cell Biochem 360, 373–382 (2012). https://doi.org/10.1007/s11010-011-1077-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-011-1077-x