Abstract
The role of endoplasmic reticulum (ER) stress in kidney diseases is not well elucidated. Fifty patients with primary glomerular diseases (PGD): minimal change disease (MCD), focal segmental glomerulosclerosis (FSGS), membranous glomerulonephritis (MGN), membranoproliferative glomerulonephritis (MPGN), and crescentic glomerulonephritis, n = 10 (each group) were enrolled. MCD, FSGS, and MGN patients were sub-grouped as nonproliferative glomerulonephritis (NPGN) and MPGN, RPGN as proliferative glomerulonephritis (PGN). Glucose regulated proteins (GRP-78), growth arrest and DNA damage inducible proteins (GADD-153), and Bcl-2 protein expression was analyzed by Western blotting, immunofluorescence and immunohistochemistry in the kidney biopsy. Up regulation of GADD-153, GRP-78, with more pronounced expression in PGN vs. NPGN (P < 0.05) and down regulation of Bcl-2 proteins was observed in the GN (PGD excluding MCD) as compared to MCD (P < 0.05). Our results suggest that renal injury in PGD is associated with ER stress and ER stress may be involved in the rapid progression of PGN to renal failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoplasmic reticulum (ER) stress is the term given to an imbalance between the cellular demand for ER function and ER capacity [1]. ER stress can be triggered by various stimuli, such as oxidative stress, hyperhomocysteinemia (Hhcy), disturbance in the Ca2+ homeostasis, and increase in synthesis of client proteins [1–3]. Cells respond to ER stress by activation of the unfolded protein response (UPR) pathway [3]. The UPR involves transient attenuation of new protein synthesis, degradation of misfolded proteins, onset of apoptosis and expression of a variety of ER stress proteins such as glucose-regulated proteins (GRPs) [2]. Under normal conditions, ER stress proteins complex with defective proteins and target them for degradation [2, 3]. Induction of the UPR allows cells to recover from ER stress and is protective to additional insults. However, if the stress is prolonged, or the adaptive response fails, apoptotic cell death ensues, which involves the induction of genes like GADD153, GADD-45 (Growth arrest and DNA damage inducible genes) [4, 5]. GADD-153, also known as CHOP, is a leucine zipper transcription factor that is present at low levels under normal conditions but is robustly expressed in response to stress [5]. Elevated GADD153 expression has been shown to down regulate expression of the anti-apoptotic protein Bcl-2, which leads to enhanced sensitization of the cells to ER stress and apoptosis [4].
ER stress has been shown to be closely associated with several diseases such as neuronal cell injury [6], Alzheimer’s disease [7], Parkinson’s disease [8]; however, its pathophysiological role in kidney disease remains elusive. Glomerular diseases are developed by various causes, but little is known about involvement of ER stress in glomerular injury. However, recent investigations suggest roles of ER stress in some types of glomerular disorders, especially proteinuric diseases caused by injury of podocytes [9–13]. Bek et al. using immunohistochemical staining recently reported up regulation of CHOP in podocytes of proteinuric human kidneys (membranous nephropathy, focal segmental glomerulosclerosis (FSGS), and minimal change nephropathy) as well as kidneys of rats with puromycin nephrosis, a model of minimal change nephropathy [7]. Cybulsky et al. (2002) reported that complement-induced podocyte injury was associated with up regulation of GPR78 (bip) and GRP94 both in vitro and in vivo in proteinuric rats with passive Heymann nephritis indicating that ER stress may be involved in the pathogenesis of membranous nephropathy [14]. Using an in vitro model of ischemia-reperfusion, Cybulsky et al. reported that podocytes subjected to ischemia-reperfusion exhibit phosphorylation of PERK and eIF2 indicating an anti-apoptotic role of the PERK-eIF2 branch of UPR in ischemic injury of podocytes [15]. An increased expression of GRP-78 in rat proximal tubular cells in response to cadmium exposure has been observed by Liu et al. [16], which suggest that ER stress plays an important role in protection against nephrotoxic insults.
Since primary glomerular diseases (PGD) are known to be accompanied by increased homocysteine levels (hHcy) [17, 18], oxidative stress [19, 20], exposure to nephrotoxicants [21], and heavy proteinuria [21]; factors which are known to induce ER stress, we have hypothesized that these glomerular diseases may be accompanied by increased ER stress in the renal cells which may contribute significantly to their pathophysiology and propensity to develop into renal failure. For this, we examined the comparative expression of ER stress biomarkers (GRP-78, GADD-153, and Bcl-2) in proliferative and nonproliferative PGD to evaluate the potential role of ER stress in the pathophysiology of these diseases.
Materials and methods
The study was carried out in the Department of Experimental Medicine and Biotechnology in collaboration with the Department of Nephrology and Department of Pathology of the PGIMER, Chandigarh. Fifty patients with PGD: minimal change disease (MCD); n = 10, FSGS; n = 10, membranous glomerulonephritis (MGN); n = 10, membranoproliferative glomerulonephritis (MPGN); n = 10, and crescentic glomerulonephritis; (n = 10) were enrolled in the study. Only patients with histologically confirmed diagnosis of PGD as per light, immunofluorescence and electron microscopic reports were included. Patients with secondary glomerulonephritis, or those on vitamin supplementation or with any previous history of steroids intake or immunosuppressant were excluded from the study. The demographic profile and the biochemical profile of the study subjects are given in Table 1. The patients with MCD were taken as controls and were compared with GN (PGD patients excluding MCD). The patients with MCD, FSGS, and MGN were sub-grouped as nonproliferative glomerulonephritis (NPGN; n = 30) and patients with MPGN and crescentic glomerulonephritis (RPGN) as proliferative glomerulonephritis (PGN; n = 20). Informed consents were obtained from all the subjects included in the study. The Indian Council of Medical Research (ICMR) approved the study protocol and the ethical clearance was obtained from the Institute ethics committee.
Sample collection
The ER stress specific protein expression profiling was done in the kidney biopsy of the patients with different PGD. Fine needle tissue aspirate (FNAC sample) was taken. The biopsy specimens were snap frozen in liquid nitrogen, followed by immediate storage at −80°C until processing. GRP-78 expression was analyzed by Western blotting and immunofluorescence (IF). Analysis of GADD-153 and Bcl-2 levels and their localization were measured by Western blotting and immunohistochemistry (IHC).
Immunohistochemical analysis
A total of 5-μm thick paraformaldehyde fixed paraffin sections of kidney biopsy were used in the study. The tissue sections of breast carcinoma and follicular lymphoma acted as positive control for GADD-153 and Bcl-2 immunostaining, respectively; biopsy sample incubated without primary antibody was used as negative control. After deparaffinization, rehydration and blocking of the endogenous peroxidase activity (3% H2O2 + methanol) for 20 min, the slides were subjected to microwave antigen retrieval with three cycles of wet heat at 98°C for 5 min each under 150 W. This was followed by incubation with primary rabbit polyclonal antibody against GADD-153 (1:20) and mouse monoclonal antibody against Bcl-2 (1:50) (Santa Cruz Biotechnology Inc., CA, USA) overnight at 4°C and ready to use biotinylated universal secondary antibody [ABC staining system, Novastatin Universal detection kit (Novocastra)] as per the manufacturers protocol. The reaction products were visualized with 3-3′-Diaminobenzidine tetra hydrochloride (DAB) (Sigma Chemical Co, St. Louis, MO) and H2O2 followed by mild counterstaining with haematoxylin.
Evaluation of the expression of GADD-153 in the kidney biopsies of the patients was done as follows: kidney biopsy sections were screened for GADD-153 expression in the tubules, glomerulus, and inflammatory cells. The numbers of GADD-153 positive cells were counted under a light microscope at 40× magnification and were expressed as the average value at each time point based on the examination of 50 fields. The GADD-153 expression was graded as null (0) in absence of any positivity, mild (0.5) denoted 25–50% positivity, moderate (0.75) as 50–75% positivity and strong (1) denoted 75–100% positivity.
Indirect immunofluorescence assay
Immunofluorescence for GRP-78 was done by incubating cryostat processed kidney sections with rabbit polyclonal anti-GRP-78 antibody (1:20; Santa Cruz Biotechnology Inc., CA, USA) at 37°C for 45 min in a humified chamber followed by incubation with FITC-labeled anti-rabbit antibody (1:50, Sigma Chemical Co, St. Louis, MO) at 37°C for 45 min. Sections of breast carcinoma and kidney biopsy sections without primary antibody were run in parallel as positive and negative controls, respectively. The immunofluorescence signals from glomeruli and the tubules were evaluated on Nikon Optophot-2 fluorescent microscope connected to a Nikon UFA-II photomultiplier and camera under high power (i.e., 30×) from three representative glomeruli and tubules from at least 20 fields and averaged. The entire kidney biopsy was viewed and positivity was graded as described, taking into consideration the percentage of tubular, glomerular, or interstitial inflammatory cells showing positivity. The number of cells showing positive immunostaining was recorded. The IF score of 0 was given on absence of any positivity in the cytoplasm as well as the nucleus, IF score 1 denoted focal positivity (1–10%), IF score 2 denoted mild (10–25%) positivity, IF score 3 (25–50%), 4 (50–75%) denoted moderate positivity, and IF score 5 corresponded to strong (75–100%) positivity levels.
In order to minimize observer bias, the scoring was performed in a blinded fashion without knowledge of the disease group from which the tissue originated. The mean score for each group was then calculated.
Polyacrylamide gel electrophoresis and Western blot analysis
Western blotting was done for the tissue biopsies of all the patients enrolled in the study. The kidney biopsy tissue of each patient was lysed in a lysis buffer containing 20 mM Tris–HCl pH 7.4, 150 mM NaCl, 2 mM phenylmethylsulfonyl fluoride (PMSF), 1% V/V Triton-X-100, 10% glycerol, 1 μg/ml leupeptin using sonication for 20 min on ice. The lysates were centrifuged at 10,000 rpm/20 min. Supernatants were boiled in 1× sample buffer (25 mM Tris/HCl (pH 6.8), 2% SDS, 10% glycerol, 5% β-mercapto-ethanol, and 0.01% bromophenol blue) for 5 min. A total of 25 μg of protein lysate [as estimated by bicinchonic acid (BCA) method; BCA estimation kit; Sigma Chemical Co, St. Louis, MO] was separated by 12.5% SDS-PAGE followed by electrotransfer to polyvinylidene difluoride (PVDF) membrane (0.45 μm, Immobilon P; Millipore Eschborn, Germany) in the blotting buffer (100 mM Tris/glycine pH 8.3) containing 20% methanol. The membranes were blocked with 5% (w/v) skim milk powder in phosphate buffer saline (PBS) overnight at 4°C. The strips were incubated with the primary antibodies (rabbit polyclonal anti-GADD-153; 1:300, mouse monoclonal anti-Bcl-2; 1:200 and rabbit polyclonal anti-GRP-78 antibody; 1:300-Santa Cruz Biotechnology Inc., CA, USA, rabbit anti-actin polyclonal antibody, 1:500 as control for GADD-153 and GRP-78 proteins and mouse-anti-actin polyclonal antibody, 1:500 as control for Bcl-2 protein; Sigma chemical Co., St. Louis, MO) in 2.5% PBS-skim milk for 2 h at 37°C. Binding to primary antibodies was visualized by incubation with horse radish peroxidase (HRP) conjugated secondary anti-rabbit IgG for GRP-78, GADD-153, β-actin, and anti-mouse antibody for Bcl-2 and β-actin (Sigma chemical Co., St. Louis, MO) for 1 h at 37°C. The membrane was placed in 0.05% 3,3′-diaminobenzidine tetra hydrochloride (DAB) (Sigma chemical Co., St. Louis, MO) in PBS containing H2O2 (1 μl/ml) for the required time.
Quantization of the immunoblots was performed by densitometry. Blots were scanned, specific bands of interest were selected and the peak density of the bands was measured using gel documentation software of biorad-gel documentation system (Bio-Rad laboratories, USA) and normalized by the band intensity of actin. The densitometric measurements were averaged to get the semi-quantitative protein expression profile.
Statistical analysis
The data was statistically analyzed and expressed as mean ± standard deviation (SD) of the mean. ANOVA and Tukey’s post-hoc tests were carried out to analyze the data between GN patients and MCD patients and between PGN and NPGN groups. Pearson’s coefficient of correlation was calculated to look at the possible correlation of the ER stress markers among themselves and with serum creatinine, GFR, 24 h urinary proteins excretion and serum proteins. Analysis of co-variance (ANCOVA) was performed to compare the parameters of ER stress after adjustment for creatinine. All the statistical analysis was performed using the SPSS software (V10).
Results
GRP-78 expression
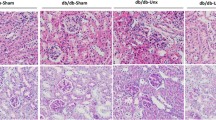
Western blot analysis showed that GRP-78 expression was significantly increased in the kidney biopsies of patients with PGD (GN: PGN + NPGN excluding MCD) as compared to those with MCD (P < 0.05) (Figs. 1, 2). Further, the patients in the PGN group had significantly increased GRP-78 protein expression as compared to those in the NPGN group (P < 0.05) (Figs. 1, 2). The GRP-78 levels in GN and PGN remained significantly elevated after adjustment for creatinine levels with ANCOVA (P < 0.05). Immunofluorescence analysis detected increased GRP-78 levels in the tubules and glomeruli with variable focal granular positivity (Fig. 3). The inflammatory cells showed little positivity (Fig. 3).
Western blot analyses of ER stress proteins in the patients with different PGD (PGN, NPGN). Western blot was done for each patient enrolled in the study. Each band in the figure represents the protein expression profile of a single representative patient belonging to different PGD (MCD, PGN, and NPGN). The average densitometric expression of GRP-78 and GADD-153 was significantly higher and Bcl-2 significantly lower in the patients with PGD as compared to MCD (P < 0.05). The patients with PGN had significantly increased expression of GRP-78 and GADD-153 as compared to those with NPGN. β-actin acted as internal control. A total of 25 μg of sample was loaded in each well as estimated by BCA method
Differential expression of ER stress proteins in (MCD, PGN and NPGN, GN) by Western blot analysis a GRP-78, b GADD-153, and c Bcl-2. The expression of GRP-78 and GADD-153 was significantly higher and Bcl-2 significantly lower in the patients with GN as compared to MCD (P < 0.05). The patients with PGN had significantly increased expression of GRP-78 and GADD-153 as compared to those with NPGN. Each bar represents mean ± SD of mean, * P < 0.05 (GN vs. MCD) and # P < 0.05 (PGN vs. NPGN). MCD minimal change disease, PGN proliferative glomerulonephritis, NPGN nonproliferative glomerulonephritis, GN primary glomerular disease patients including PGN + NPGN but excluding MCD
GADD-153 expression
GADD-153 expression was significantly increased in the GN group as observed by both by Western blot analysis and immunohistochemical analysis as compared to MCD group (Figs. 2, 3). IHC showed significantly increased staining in the tubules and the glomeruli (Fig. 4). GADD-153 expression was significantly greater in the PGN group as compared to the NPGN group (Fig. 4) (P < 0.05). The GADD-153 levels in GN and PGN remained significantly elevated after adjustment for creatinine levels with ANCOVA (P < 0.05).
Bcl-2
Bcl-2 protein expression was found to be mainly localized in the cytoplasm of the tubules (Fig. 4). A significantly decreased expression of Bcl-2 was observed in GN as compared to MCD (P < 0.05) (Figs. 1, 2, 4). Bcl-2 expression was not significantly different in between PGN and NPGN groups (P > 0.05) (Figs. 1, 2, 4). The Bcl-2 levels showed negative correlation with GADD-153 levels in GN patients (r = −0.38, P < 0.05).
Discussion
Accumulating evidence suggests the role of ER stress and UPR in a wide range of renal pathophysiologies [13]. Recent investigations have indicated the involvement of ER stress in some type of glomerular diseases, especially proteinuric diseases caused by podocye injury [9–13]. However, currently, the information is limited regarding the role of ER stress and UPR in PGD. Further, the status of ER stress in PGD with differential predisposition to renal failure has not been studied. In the present study, we examined if the quantum of ER stress, measured as tissue expression of ER stress markers: GRP-78, GADD-153, and Bcl-2, was associated with progression of PGD to ESRD.
We observed increased renal expression of two ER stress proteins (GRP-78 and GADD-153) in FSGS, MGN, MPGN, and crescentic GN as compared to MCD, indicating the presence of ER stress in the kidneys of these patients. Previous studies in proteinuric rats, have reported that renal tubules exposed to high albumin concentrations exhibit ER stress, resulting in tubular injury [22]. We too found increased expression of GRP-78 and GADD-153 proteins in the renal tubules from GN which could be due to proteinuria observed in these diseases. Thus, increased protein load appear to contribute to ER stress in GN.
Since PGD patients had significantly higher creatinine levels, indicative of renal insufficiency, which could also result in ER stress, therefore, we carried out ANCOVA to eliminate the effect of serum creatinine levels on status of ER stress. We observed that even after adjusting the ER stress parameters for serum creatinine, these parameters remained significantly altered indicating that the ER stress observed in PGD is not a consequence of renal insufficiency, rather, it reflects a pathomechanism leading to glomerular injury in these diseases.
hHcy has been reported to cause progression of podocyte injury and glomerulosclerosis in the rat models [23, 24]. It has been recently suggested that Hcy induced glomerular injury might be mediated through ER stress pathway [13]. Further, ER stress has been shown to be involved in down-stream of oxidative stress through generation and accumulation of oxidatively modified, abnormal proteins [25–27]. Hence, increased plasma Hcy levels and oxidative stress observed in the present study could be involved in inducing ER stress in renal cells in the GN. We also observed a positive correlation between plasma Hcy and renal GRP-78 (r = 0.28, P < 0.05) expression in PGD patients, further suggesting that increased Hcy levels were associated with elevated expression of GRP-78 in PGD.
We found significantly lower expression of Bcl-2 in renal biopsies from PGD patients. Similar results have been reported in the patients with IgA nephropathy where Bcl-2 was found to be down-regulated in advanced and end stage renal disease [28]. Bcl-2 expression showed negative correlation with GADD-153 expression (P < 0.05) in present study. McCullough et al. (2001) reported that GADD-153 could sensitize cells to apoptosis through down-regulation of Bcl-2 [4] suggesting that GADD-153 may modulate Bcl-2 activity and apoptosis. We did not find any significant difference in Bcl-2 expression between PGN and NPGN groups. This is in consistence with the observations by Marone et al. (2002) who also found no significant difference in Bcl-2 expression between proliferative and NPGN [29].
Since PGD constitute a heterogeneous group of diseases which show marked variability for progression to renal failure; diseases with rapid proliferation of the parietal epithelial cells and infiltrating monocytes like crescentic glomerulonephritis are often associated with renal failure; whereas, patients with MCD inherently do not progress to the end stage renal disease (ESRD) [30]. On stratification of patients into proliferative and nonproliferative groups, we observed that ER stress was more pronounced in proliferative as compared to nonproliferative group. Our results confirm earlier observations of an increased GADD-153 expression in the acute tubular necrosis (ATN) as compared to nonproliferative MGN [22]. It has been proposed that disturbances in the normal functions of the ER lead to cell stress response, which is initially aimed at compensating for damage, but can eventually trigger cell death if ER dysfunction is severe or prolonged [3]. For example, accumulation of misfolded proteins in neurodegenerative diseases has been shown to lead to an ER stress response rendering neurons more susceptible to cell death [31]. ER stress has been also implicated in renal cell death following exposure to reactive chemical toxicants [16, 23]. We proposed that enhanced ER stress in proliferative glomerulonephritis may render renal cells more susceptible to cell death.
To conclude, the present study indicates that increased ER stress may be an important mechanism of glomerular injury in PGD. A significantly more pronounced ER stress in proliferative glomerulonephritis suggests that it may contribute to increased glomerulosclerosis. Further investigations are warranted to examine how ER stress and UPR contribute to renal pathophysiologies in PGD.
References
Ron D (2001) Hyperhomocysteinemia and function of the endoplasmic reticulum. J Clin Investig 107:1221–1222. doi:10.1172/JCI13092
Liu H, Bowes RC, Water B et al (1997) Endoplasmic reticulum chaperones GRP78 and calreticulin prevent oxidative stress, Ca2+ disturbances and cell death in renal epithelial cells. J Biol Chem 272:21751–21759. doi:10.1074/jbc.272.35.21751
Yoshida H (2007) ER stress and diseases. FEBS J 274:630–658. doi:10.1111/j.1742-4658.2007.05639.x
McCullough KD, Martindale JL, Klotz LO et al (2001) Gadd153 sensitizes cells to endoplasmic reticulum stress by down-regulating bcl-2 and perturbing the cellular redox state. Mol Cell Biol 21:1249–1259. doi:10.1128/MCB.21.4.1249-1259.2001
Leckstrom HJ, Xanthopoulos KG (1998) Biological role of the CCAAT/enhancer-binding protein family of transcription factors. J Biol Chem 273:28545–28548. doi:10.1074/jbc.273.44.28545
Paschen W, Frandsen A (2001) Endoplasmic reticulum dysfunction—a common denominator for cell injury in acute and degenerative diseases of the brain. J Neurochem 79:719–725. doi:10.1046/j.1471-4159.2001.00623.x
Katayama T, Imaizumi K, Sato N et al (1999) Presenilin-1 mutations downregulate the signaling pathway of the unfolded-protein response. Nat Cell Biol 1:479–485. doi:10.1038/70265
Imai Y, Soda M, Inoue H et al (2001) An unfolded putative transmembrane polypeptide, which can lead to endoplasmic reticulum stress, is a substrate of Parkin. Cell 105:891–902. doi:10.1016/S0092-8674(01)00407-X
Bek MF, Bayer M, Müller B et al (2006) Expression and function of C/EBP homology protein (GADD153) in podocytes. Am J Pathol 168:20–32. doi:10.2353/ajpath.2006.040774
Cybulsky AV, Takano T, Papillon J et al (2005) Role of the endoplasmic reticulum unfolded protein response in glomerular epithelial cell injury. J Biol Chem 280:24396–24403. doi:10.1074/jbc.M500729200
Kitamura M (2008) Endoplasmic reticulum stress in the kidney. Clin Exp Nephrol 12:317–325. doi:10.1007/s10157-008-0060-7
Liu L, Doné SC, Khoshnoodi J et al (2001) Defective nephrin trafficking caused by missense mutations in the NPHS1 gene: insight into the mechanisms of congenital nephrotic syndrome. Hum Mol Genet 10:2637–2644. doi:10.1093/hmg/10.23.2637
Kitamura M (2008) Endoplasmic reticulum stress and unfolded protein response in renal pathophysiology: Janus faces. Am J Physiol Renal Physiol 295:F323–F334. doi:10.1152/ajprenal.00050.2008
Cybulsky AV, Takano T, Papillon J et al (2002) Complement C5b-9 membrane attack complex increases expression of endoplasmic reticulum stress proteins in glomerular epithelial cells. J Biol Chem 277:41342–41351. doi:10.1074/jbc.M204694200
Socha L, Silva D, Lesage S et al (2003) The role of endoplasmic reticulum stress in nonimmune diabetes: NOD.k iHEL, a novel model of beta cell death. Ann N Y Acad Sci 1005:178–183. doi:10.1196/annals.1288.022
Liu F, Inageda K, Nishitai G et al (2006) Matsuoka M: cadmium induces the expression of Grp 78, an endoplasmic reticulum molecular chaperone, in LLC-PK1 renal epithelial cells. Environ Health Perspect 114:859–864
Arnadottir M, Hultberg B, Berg AL (2001) Plasma total homocysteine concentration in nephrotic patients with idiopathic membranous nephropathy. Nephrol Dial Transplant 16:45–47. doi:10.1093/ndt/16.1.45
Herrmann W, Schorr H, Geisel J et al (2001) Homocysteine, cystathionine, methylmalonic acid and B-vitamins in patients with renal disease. Clin Chem Lab Med 39:739–746. doi:10.1515/CCLM.2001.123
Wojcicka G, Beltowski J (2001) Oxidative stress in glomerulonephritis. Postepy Hig Med Dosw 55:855–869
Yokouchi M, Hiramatsu N, Hayakawa K et al (2008) Involvement of selective reactive oxygen species upstream of proapoptotic branches of unfolded protein response. J Biol Chem 283:4252–4260. doi:10.1074/jbc.M705951200
Túri S, Németh I, Torkos A et al (1997) Oxidative stress and antioxidant defense mechanism in glomerular disease. Free Radic Biol Med 22:161–168. doi:10.1016/S0891-5849(96)00284-5
Ohse T, Inagi R, Tanaka T et al (2006) Albumin induces endoplasmic reticulum stress and apoptosis in renal proximal tubular cells. Kidney Int 70:1447–1455. doi:10.1038/sj.ki.5001704
Muruganandan S, Cribb AE (2006) Calpain-induced endoplasmic reticulum stress and cell death following cytotoxic damage to renal cells. Toxicol Sci 94:118–128. doi:10.1093/toxsci/kfl084
Yi F, dos Santos EA, Xia M et al (2007) Podocyte injury and glomerulosclerosis in hyperhomocysteinemic rats. Am J Nephrol 27:262–268. doi:10.1159/000101471
Porubsky S, Schmid H, Bonrouhi M et al (2004) Influence of native and hypochlorite modified low density lipoprotein on gene expression in human proximal tubular epithelium. Am J Pathol 164:2175–2187
Yokouchi M, Hiramatsu N, Hayakawa K et al (2008) Involvement of selective reactive oxygen species upstream of proapoptotic branches of unfolded protein response. J Biol Chem 283:4252–4260. doi:10.1074/jbc.M705951200
Markan S, Kohli HS, Sud K et al (2008) Oxidative stress in primary glomerular diseases: a comparative study. Mol Cell Biochem 311:105–110. doi:10.1007/s11010-008-9701-0
Qiu LQ, Sinniah R, Hsu SI-H (2004) Downregulation of Bcl-2 by podocytes is associated with progressive glomerular injury and clinical indices of poor renal prognosis in human IgA nephropathy. J Am Soc Nephrol 15:79–90. doi:10.1097/01.ASN.0000104573.54132.2E
Marone M, Bonanno G, Rutella S et al (2002) Survival and cell cycle control in early hematopoiesis: role of bcl-2, and the cyclin dependent kinase inhibitors p27 and p21. Leuk Lymphoma 43:51–57. doi:10.1080/10428190210195
Noel LH, Gubler MC (2003) Histological classification of chronic glomerular diseases. Rev Prat 53:2005–2012
Terro F, Czech C, Esclaire F et al (2002) Neurons overexpressing mutant presenilin-1 are more sensitive to apoptosis induced by endoplasmic reticulum-golgi stress. J Neurosci Res 69:530–539. doi:10.1002/jnr.10312
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Markan, S., Kohli, H.S., Joshi, K. et al. Up regulation of the GRP-78 and GADD-153 and down regulation of Bcl-2 proteins in primary glomerular diseases: a possible involvement of the ER stress pathway in glomerulonephritis. Mol Cell Biochem 324, 131–138 (2009). https://doi.org/10.1007/s11010-008-9991-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-008-9991-2