Abstract
Objectives To explore ethnic differences in gestational weight gain (GWG). Methods This was a population-based cohort study conducted in primary care child health clinics in Groruddalen, Oslo, Norway. Participants were healthy pregnant women (n = 632) categorised to six ethnic groups (43 % were Western European women, the reference group). Body weight was measured at 15 and 28 weeks’ gestation on average. Data on pre-pregnancy weight and total GWG until delivery were self-reported. The main method of analysis was linear regression adjusting for age, weeks’ gestation, pre-pregnancy body mass index, education and severe nausea. Results No ethnic differences were observed in GWG by 15 weeks’ gestation. By 28 weeks’ gestation, Eastern European women had gained 2.71 kg (95 % confidence interval, CI 1.10–4.33) and Middle Eastern women 1.32 kg (95 % CI 0.14–2.50) more weight on average than the Western European women in the fully adjusted model. Among Eastern European women, the total adjusted GWG was 3.47 kg (95 % CI 1.33–5.61) above the reference group. Other ethnic groups (South Asian, East Asian and African) did not differ from the reference group. When including non-smokers (n = 522) only, observed between-group differences increased and Middle Eastern women gained more weight than the reference group by all time points. Conclusions Eastern European and Middle Eastern women had higher GWG on average than Western European women, especially among the non-smokers. Although prevention of excessive GWG is important for all pregnant women, these ethnic groups might need special attention during pregnancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
What is already known?
High and low gestational weight gain (GWG) increase risk for adverse maternal and fetal outcomes. Ethnic differences in GWG might contribute to ethnic differences observed in some adverse outcomes. The previous evidence on ethnic differences in GWG mainly comes from the USA or Canada.
What this study adds?
This is the first study focusing on GWG in ethnic minorities in Europe. Eastern European and Middle Eastern women had higher GWG on average than Western European women. Although prevention of excessive GWG is important for all pregnant women, these ethnic groups might need special attention.
Introduction
The prevalence of type 2 diabetes and cardiovascular diseases are higher among several ethnic minorities such as Turkish, Moroccan, Sri Lankan, Pakistani, Iranese or Vietnamese than among the majority populations in North-Western Europe [14, 31, 33]. Although obesity rates are higher in middle aged women from several ethnic minority groups [14], prepregnancy BMI seems to be higher in women with origin from Middle East and Africa, and lower in Asian women [16]. During pregnancy, ethnic minorities often have an increased risk of adverse outcomes (e.g. gestational diabetes mellitus, low birth weight, preterm delivery or perinatal mortality) in many parts of the world [1, 8], although the differences between ethnic minorities and the majority population are smaller in countries with a strong policy facilitating integration, for example in Norway [1].
High gestational weight gain (GWG) is strongly associated with weight retention and later overweight in the mother [11, 23, 24] and the offspring [7, 19], and with adverse pregnancy outcomes such as caesarean section and high birth weight infants [11, 24]. High GWG, especially in early pregnancy, also increases the risk of gestational diabetes mellitus [4, 30]. On the other hand, low GWG increases the risk for low-birth-weight babies [29]. The US Institute of Medicine (IOM) has published body mass index (BMI) specific recommendations on GWG based on the evidence available [13].
If there were ethnic differences in GWG, they could potentially contribute to ethnic differences observed in some adverse maternal and fetal outcomes [1, 8]. The previous evidence related to ethnic differences in GWG is mainly based on studies conducted in the USA [2, 6, 12, 20, 26] or Canada [18]. These studies found some ethnic differences in the mean GWG while results related to proportions of women with inadequate or excessive GWG were more inconsistent. However, these results are not directly applicable to Europe as the ethnic composition of the population and the contexts differ between these continents. In our previous study, postpartum weight retention was higher among women from South Asia, Middle East and Africa as compared to the Western European women [34]. This suggests that these ethnic groups might have had higher GWG than the reference group.
More information is needed on GWG across ethnic subgroups in European populations. This information will help us to identify ethnic groups vulnerable to high or low GWG and further to plan interventions to optimise GWG and thereby improve the health of both the mother and the offspring in multi-ethnic populations. The aim of this study was to examine whether there are ethnic differences in mean GWG by 15 and 28 weeks’ gestation and by delivery in a population-based cohort of pregnant women in Oslo, Norway. We describe patterns of GWG by ethnicity, but do not explore predictors of GWG or associations between GWG and maternal or fetal outcomes.
Materials and Methods
Study Design and Population
The study methods have been described in detail elsewhere [15]. The prospective cohort study was conducted among pregnant women attending primary care child health clinics for antenatal care in Groruddalen, in Eastern Oslo, Norway. The original aim was to explore predictors of gestational diabetes mellitus and fetal growth in a multi-ethnic population. Groruddalen covers both affluent and more deprived residential areas and a high proportion of the population belongs to minority ethnic groups. In this area, at least 75–85 % of pregnant women attend the child health clinics for antenatal care.
Pregnant women were eligible for the study if they were (1) living in one of three city districts in Groruddalen, (2) planning to give birth at one of the two study hospitals, (3) at ≤20 weeks’ gestation, (4) not having pre-pregnancy diabetes or other diseases requiring intensive hospital follow-up during pregnancy, (5) not already recruited to the same study during a previous pregnancy lasting ≥22 weeks, (6) able to communicate in Norwegian or any of the eight languages to which all the information materials and questionnaires were translated (Arabic, English, Sorani, Somali, Tamile, Turkish, Urdu and Vietnamese), and (7) able to give informed written consent. The participants were recruited at 15 week’s gestation on average between May 2008 and May 2010. The Regional Ethics Committee and the Norwegian Data inspectorate have approved the study protocol. All participants signed a written informed consent.
Data Collection
Certified study midwives were specially trained to collect the study data by interviewing the participants, to fill in the questionnaires and to perform anthropometric measurements at inclusion (15 weeks’ gestation on average) and at 28 weeks’ gestation on average [15]. Professional interpreters translated the discussions when a participant was not fluent in Norwegian.
Anthropometric Variables
Body height was measured to the nearest 0.1 cm using a fixed stadiometer and pre-pregnancy weight was self-reported at 15 weeks’ gestation on average. Pre-pregnancy BMI was calculated as pre-pregnancy weight divided by squared height and categorised according to the IOM’s categories [13]. Body weight and fat mass were measured in light clothing without shoes using a Tanita-weight BC-418 MA (Tanita, Tokyo, Japan) at 15 and 28 weeks’ gestation. The Tanita BC-418 MA it gives comparable results to the older version Tanita TBF 410, which has been validated in pregnancy [32].
The Outcome Variables
The main outcomes were mean GWG by 15 and 28 weeks’ gestation and the mean total GWG from pre-pregnancy until delivery. GWG by 15 and 28 weeks’ gestation was calculated based on self-reported pre-pregnancy weight and measured body weights at 15 and 28 weeks’ gestation, respectively. Information on total GWG was self-reported at a visit at 14 weeks postpartum. Data on weeks’ gestation at delivery and infant’s birth weight were obtained from the hospital birth records. The secondary outcomes were fat gain between 15 and 28 weeks’ gestation (based on the measured fat mass at both time points) and the total GWG categorised according to the IOM’s recommendations (inadequate, appropriate or excessive) [13].
Ethnicity and the Background Variables
Data on ethnic origin and all the background variables were collected through a questionnaire at inclusion (15 weeks’ gestation). Ethnic origin, the main exposure variable of the present study, was defined by the participant’s own country of birth or mother’s if she was born outside of Europe or North America [15]. Ethnicity was categorised as follows: Western Europe (including North America), Eastern Europe, Middle East (including North Africa and Central Asia), Africa (except for North Africa), South Asia and East Asia. The reference group was the Western European women consisting of women born in Norway (93.6 %), Sweden or Denmark (3.2 %) or other Western European countries (3.2 %, including 3 white women from North America).
Age was collected as a continuous variable and parity was categorised to nulliparous or parous. Concerning women who were not born in Norway, data on duration of residence in Norway was categorised to 0–1 years (recent immigrants) or ≥2 years. Educational level was categorised as <10 years, 10–12 years and university or college. Pre-pregnancy smoking pattern was reported and the response categories were “not smoking”, “occasionally” and “daily”. They were further categorised as (1) non-smokers, (2) smokers before but not during pregnancy, and (3) smokers before and during pregnancy, since smoking cessation during pregnancy has been associated with higher GWG, while continuing smoking during pregnancy has been related to similar GWG as in the non-smokers [27, 28].
At 28 weeks’ gestation, smoking pattern was reported with the same response categories as in pre-pregnancy. Pregnancy-induced severe nausea was categorised as ‘yes’ or ‘no’, based on the midwives’ clinical experience and control questions, regarding impact on daily function, duration of symptoms and frequency of vomiting [3]. The data on depressive symptoms were collected using the Edinburgh Postnatal Depression Scale (EPDS) [22] and an EPDS score ≥10 was used as a proxy measure for depression [10].
Statistical Methods
The descriptive statistics are presented as means and standard deviations (SD) or numbers and percentages. The differences between the background variables of the included (n = 632) and the excluded (n = 191) women were tested using the Pearson Chi-square test for categorical variables and independent samples t test for continuous variables. The correlation between self-reported pre-pregnancy weight and measured weight at 15 weeks’ gestation was calculated using the Pearson correlation coefficient. The differences in the crude continuous outcome variables between the ethnic groups were examined by linear regression models with Western European women as the reference category.
Between-group differences in adjusted means of the outcome variables were tested using two different versions of linear regression models with Western European women as the reference group. Model 1 was adjusted for age and weeks’ gestation at the respective time points (both as continuous variables). Model 2 was additionally adjusted for pre-pregnancy BMI (as a continuous variable), education and severe nausea (both as categorical variables). When fat mass gain was the outcome, the time-related covariates included weeks’ gestation at inclusion and the number of weeks between the inclusion visit and the second study visit around 28 weeks’ gestation (both as continuous variables) in each model. The rationale for choosing confounders for the models was that the variables were known to be associated with the outcome variables based on previous knowledge or in the present data and they differed by ethnicity in the present data (Table 1). The chosen covariates were also not supposed to be in the causal chain between ethnicity and the outcome or be components of the outcome variables.
We explored possible interactions for ethnicity and each of the other covariates (except for weeks’ gestation) one by one for each outcome separately, by adding interaction terms to the regression analysis (with Model 2 adjustments). The results of the linear regression models are presented as regression coefficients (β) with 95 % CI, p values and adjusted R2. p values <0.05 were regarded as statistically significant. Regarding the assumptions of linear regression model, the residuals were normally distributed and no autocorrelation (based on Durbin–Watson test), multi-collinearity (based on variance inflation factor) or remarkable outliers were observed.
In sensitivity analyses, the linear regression analyses (Models 1–2) were restricted to the non-smokers to control for possible confounding by smoking status, as it was not possible to adjust for smoking in the models because the numbers of smokers were very low in some ethnic groups. Parity and depression variables were also included in the models in the preliminary analyses. Since they were not statistically significant and did not change the associations between ethnicity and the outcomes in any of the models, these variables were not included in the final models.
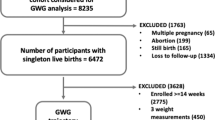
To illustrate GWG in each ethnic group (Fig. 1), analysis of covariance was used to calculate the mean adjusted GWG by each time point and the adjustments were made for age, weeks’ gestation at the respective time point, BMI (all as continuous variables), education and severe nausea (both as categorical variables). The SPSS statistical software package version 20.0 (SPSS Inc., Chicago, IL, USA) was used for the data analyses.
Mean gestational weight gain (kg) by weeks’ gestation in each ethnic group among non-smokers (n = 522), adjusted for age, weeks’ gestation at the respective time point, pre-pregnancy body mass index, education and severe nausea (WE Western European, EA East Asian, EE Eastern European, SA South Asian, ME Middle Eastern, A African)
Results
A total of 823 (74 % of the eligible women) agreed to participate. The participation rate varied by ethnicity (Western European 82 %, Eastern European 75 %, South Asian 73 %, Middle Eastern 65 %, African 64 % and East Asian 63 %). Of the 823 women, 59 % were of ethnic minority origin (i.e. other than Western European). Data on total GWG were available for 632 women, constituting the study sample, after excluding seven women from South or Central America due to the low number.
Descriptive information on the background characteristics of the included women are presented by ethnicity in Table 1. No statistically significant differences were observed between the 632 included and the 191 excluded women for any variables listed in Table 1.
The Primary Outcomes by Ethnicity
The Pearson correlation coefficient for self-reported pre-pregnancy weight and measured weight at 15 weeks’ gestation varied from 0.95 to 0.97 between the ethnic groups. Table 2 shows the crude GWG at three time points. The African women gained more weight on average by 15 weeks’ gestation and the Eastern European women by 28 weeks’ gestation and by delivery compared to the Western European women. Table 3 shows the adjusted coefficients (95 % CI) in Models 1 and 2 for the mean GWG by 15 and 28 gestation and by delivery by ethnicity and the other covariates. In the fully adjusted Model 2, none of the groups differed from the reference group at 15 weeks’ gestation but the Eastern European women had gained 2.7 kg more and the Middle Eastern women 1.3 kg more weight on average than the reference group by 28 weeks’ gestation. The total GWG by delivery was 3.5 kg higher among the Eastern European women than the reference group (Model 2).
Statistically significant overall interactions were found only for ethnicity and severe nausea (p = 0.046) when total GWG was as the outcome. Adding the interaction terms did not essentially change the associations observed between ethnicity and GWG. Since there were no significant interactions in the models for the other outcomes and the numbers of women were low in many subgroups, the data were not stratified by severe nausea.
Although few women were smokers, there were ethnic differences in smoking status (Table 1). As the non-smokers had lower mean crude total GWG (13.2 kg, SD 5.8) than those who smoked before (16.8 kg, SD 6.8) or during pregnancy (15.8 kg, SD 6.8), the linear regression models were restricted to non-smokers to control for confounding by smoking status. When including the non-smokers only (n = 522), the Middle Eastern and the African women had gained more weight by 15 weeks’ gestation and the Middle Eastern and the Eastern European women by 28 weeks’ gestation and by delivery than the reference group, and the coefficients for these groups were larger than in the total sample (not tested statistically) (Table 4). The corresponding ethnic differences in adjusted mean GWG are illustrated by weeks’ gestation for the non-smokers in Fig. 1.
The Secondary Outcomes by Ethnicity
The African women gained less fat and the Eastern European women gained more fat between 15 and 28 weeks’ gestation on average than the Western European women (Table 2). The linear regression model for fat gain showed that the Eastern European women gained 1.4 kg more fat than the reference group in the fully adjusted Model 2 (Table 5). When the analysis was restricted to the non-smokers only, the results regarding fat gain remained similar although the coefficients were now larger as compared to the results observed in the total population (Table 5).
The crude percentages of women with inadequate, appropriate and excessive total GWG are reported in Table 2. Excessive GWG was most common among the Eastern European (54.5 %) and the Middle Eastern (50.0 %) women and the least common among the African women (33.3 %), although the differences between the groups were not statistically significant (p = 0.10).
Discussion
Main Findings
To our knowledge, this is the first European study with a primary aim to examine ethnic differences in mean GWG at several time points during pregnancy. GWG was similar in the ethnic groups in early pregnancy. By 28 weeks’ gestation, the Eastern European women had gained 2.7 kg and the Middle Eastern women 1.3 kg more weight on average than the Western European women in the fully adjusted model. The Eastern European women also had 3.5 kg higher adjusted mean total GWG than the Western European women. When including the non-smokers only, larger differences were discovered between the ethnic groups and the Middle Eastern women had gained more weight on average than the Western European women throughout the pregnancy. In general, no differences were observed in GWG between the other ethnic groups (South Asian, East Asian and African) and the Western European women.
Strengths and Weaknesses
The present study has several strengths. Firstly, this was a population-based cohort study with high participation rates also in minority ethnic groups often excluded in research. The questionnaires were translated into eight different languages. The cohort was representative of the main ethnic groups living in Oslo [15]. We found no significant differences in the background variables between the included and the excluded women. We used measured data on body weight and fat mass at 15 and 28 weeks’ gestation on average. The self-reported pre-pregnancy weight correlated strongly with weight measured at 15 weeks’ gestation (r = 0.95–0.97 in all ethnic groups). The participants reported their pre-pregnancy weight after they had been weighed at 15 weeks’ gestation which may have reduced the likelihood of underestimating their weight. As the validity of measurement of body fat might vary by ethnicity, we used intra-individual change in fat mass as an outcome variable, which reduces the possibility of information bias.
One main weakness is that we relied on self-reported data on total GWG by delivery. We cannot rule out the possibility of differential reporting by ethnic groups. However, the pattern of GWG based on the objectively measured weights from inclusion to 28 weeks’ gestation and the relative position persist to delivery for all ethnic groups, except for the African women. The validity of self-reported data on GWG has been assessed in a US study with a majority of black/African American women [35]. Only half of the participants could be considered as accurate reporters and high pre-pregnancy BMI and inadequate actual GWG were associated with over-reporting while excessive actual GWG was associated with under-reporting of GWG. However, the most relevant question for this study is whether the validity of self-reported data on total GWG differs by ethnicity. To our knowledge, no previous studies have addressed this question. Finally, the numbers of African, East Asian and Eastern European women were small reducing the possibilities to detect statistically significant differences between those groups and the reference group. Additionally, the ethnic groups were relatively broad and therefore heterogenic.
Interpretation
Our results on ethnic differences in fat gain support the main results on GWG. When including the non-smokers only and thereby eliminating confounding by smoking status, the results of Models 1 and 2 were more consistent and the between-group differences were larger in general. The results of the present study might be relevant for other European countries with similar minority ethnic groups. However, factors such as migration history, length of stay, level of integration, socio-economic status and social policy vary by country and ethnic minority group. Therefore caution is needed in generalisation of the results to other countries.
The results of the present study are not directly comparable to findings from the previous US or Canadian studies e.g. due to differences in study populations and ethnic groups included, methods of defining GWG or the confounders the analyses were adjusted for. In the USA, black and Hispanic women have gained less weight on average and have been more likely to gain inadequately and/or less likely to gain excessively weight than white women [2, 6, 12, 20, 26]. The Canadian studies observed very few ethnic differences in GWG [17, 18]. Studies comparing GWG by migrant status have reported mixed findings [5, 17, 18, 26, 27]. In our study, the percentages of women with inadequate or excessive total GWG did not differ statistically significantly between the ethnic groups. This may at least partly be due to the small number of women in some of the groups.
In our cohort, higher increase in adiposity during pregnancy and South Asian ethnicity both independently increased the risk for gestational diabetes [14, 30]. Interestingly, no significant differences were observed in GWG or fat gain between the South Asian and the Western European women in the present study. However, as South Asian people generally have more adiposity for the same BMI and higher risk for obesity-related diseases at lower levels of BMI than white Western people [21], lower BMI cut-offs have been suggested for South Asian people [9]. Therefore lower GWG recommendations might also be needed for South Asian women to reduce their risk for gestational diabetes. Very little research has been done on optimal GWG in different ethnic groups and it is unclear whether the IOM’s recommendations apply equally to all ethnic groups. The IOM’s recommendations have widely been adopted in other Western countries, for example in Norway [11]. The recommended amount of GWG has been associated with better maternal and fetal outcomes also in the Norwegian majority population [11].
In the present cohort women from South Asia, Middle East and Africa had higher postpartum weight retention than Western Europeans [34]. Our hypothesis on higher GWG in these ethnic groups was confirmed only for Middle Eastern women. Therefore it seems that South Asian and African women lose less weight in the early postpartum period, which might be related to different postpartum dietary practices or traditions [25]. To prevent weight-related problems among women in reproductive age, the most relevant time window for interventions may vary by ethnicity.
Conclusions for Practice
In this multi-ethnic cohort of pregnant women in Oslo, the Eastern European women gained more weight on average by 28 weeks’ gestation and by delivery than the Western European women. Among the non-smokers, these between-group differences were larger and the Middle Eastern women also had higher GWG than the Western European women throughout the pregnancy. Although lifestyle counselling and prevention of excessive GWG are important for all pregnant women, these ethnic groups might need special attention during pregnancy.
References
Bollini, P., Pampallona, S., Wanner, P., & Kupelnick, B. (2009). Pregnancy outcome of migrant women and integration policy: A systematic review of the international literature. Social Science and Medicine, 68, 452–461.
Bowers, K., Laughon, S., Kiely, M., Brite, J., Chen, Z., & Zhang, C. (2013). Gestational diabetes, pre-pregnancy obesity and pregnancy weight gain in relation to excess fetal growth: Variations by race/ethnicity. Diabetologia, 56, 1263–1271.
Brekke, I., Berg, J. E., Sletner, L., & Jenum, A. K. (2013). Doctor-certified sickness absence in first and second trimesters of pregnancy among native and immigrant women in Norway. Scandinavian Journal of Public Health, 41, 166–173.
Carreno, C. A., Clifton, R. G., Hauth, J. C., Myatt, L., Roberts, J. M., Spong, C. Y., et al. (2012). Excessive early gestational weight gain and risk of gestational diabetes mellitus in nulliparous women. Obstetrics and Gynecology, 119, 1227.
Chasan-Taber, L., Schmidt, M. D., Pekow, P., Sternfeld, B., Solomon, C. G., & Markenson, G. (2008). Predictors of excessive and inadequate gestational weight gain in Hispanic women. Obesity, 16, 1657–1666.
Fontaine, P. L., Hellerstedt, W. L., Dayman, C. E., Wall, M. M., & Sherwood, N. E. (2012). Evaluating body mass index-specific trimester weight gain recommendations: Differences between black and white women. Journal of Midwifery and Women’s Health, 57, 327–335.
Fraser, A., Tilling, K., Macdonald-Wallis, C., Sattar, N., Brion, M.-J., Benfield, L., et al. (2010). Association of maternal weight gain in pregnancy with offspring obesity and metabolic and vascular traits in childhood. Circulation, 121, 2557–2564.
Gagnon, A. J., McDermott, S., Rigol-Chachamovich, J., Bandyopadhyay, M., Stray-Pedersen, B., Stewart, D., et al. (2011). International migration and gestational diabetes mellitus: A systematic review of the literature and meta-analysis. Paediatric and Perinatal Epidemiology, 25, 575–592.
Gray, L. J., Yates, T., Davies, M. J., Brady, E., Webb, D. R., Sattar, N., et al. (2011). Defining obesity cut-off points for migrant South Asians. PLoS ONE, 6, e26464.
Harris, B., Huckle, P., Thomas, R., Johns, S., & Fung, H. (1989). The use of rating scales to identify post-natal depression. British Journal of Psychiatry, 154, 813–817.
Haugen, M., Brantsaeter, A. L., Winkvist, A., Lissner, L., Alexander, J., Oftedal, B., et al. (2014). Associations of pre-pregnancy body mass index and gestational weight gain with pregnancy outcome and postpartum weight retention: A prospective observational cohort study. BMC Pregnancy and Childbirth, 14, 201.
Headen, I. E., Davis, E. M., Mujahid, M. S., & Abrams, B. (2012). Racial-ethnic differences in pregnancy-related weight. Advances in Nutrition, 3, 83–94.
Institute of Medicine (IOM). (2009). Weight gain during pregnancy: Reexamining the guidelines. Washington, DC: National Academy of Sciences.
Jenum, A. K., Diep, L. M., Holmboe-Ottesen, G., Holme, I. M., Kumar, B. N., & Birkeland, K. I. (2012). Diabetes susceptibility in ethnic minority groups from Turkey, Vietnam, Sri Lanka and Pakistan compared with Norwegians—The association with adiposity is strongest for ethnic minority women. BMC Public Health, 12, 150.
Jenum, A. K., Sletner, L., Voldner, N., Vangen, S., Mørkrid, K., Andersen, L. F., et al. (2010). The STORK Groruddalen research programme: A population-based cohort study of gestational diabetes, physical activity, and obesity in pregnancy in a multiethnic population. Rationale, methods, study population, and participation rates. Scandinavian Journal of Public Health, 38(5 Suppl.), 60–70.
Jenum, A. K., Sommer, C., Sletner, L., Mørkrid, K., Bærug, A., Mosdøl, A. (2013). Adiposity and hyperglycaemia in pregnancy and related health outcomes in European ethnic minorities of Asian and African origin: A review. Food & Nutrition Research, 57, 1–22.
Kowal, C., Kuk, J., & Tamim, H. (2012). Characteristics of weight gain in pregnancy among Canadian women. Maternal and Child Health Journal, 16, 668–676.
Larouche, M., Ponette, V., Correa, J. A., & Krishnamurthy, S. (2010). The effect of recent immigration to Canada on gestational weight gain. Journal of Obstetrics and Gynaecology Canada, 32, 829–836.
Lawlor, D. A., Lichtenstein, P., Fraser, A., & Långström, N. (2011). Does maternal weight gain in pregnancy have long-term effects on offspring adiposity? A sibling study in a prospective cohort of 146,894 men from 136,050 families. American Journal of Clinical Nutrition, 94, 142–148.
Liu, J., Gallagher, A. E., Carta, C. M., Torres, M. E., Moran, R., & Wilcox, S. (2014). Racial differences in gestational weight gain and pregnancy-related hypertension. Annals of Epidemiology, 24, 441–447.
Misra, A., & Khurana, L. (2010). Obesity-related non-communicable diseases: South Asians vs White Caucasians. International Journal of Obesity, 35, 167–187.
Murray, L., & Carothers, A. D. (1990). The validation of the Edinburgh Post-natal Depression Scale on a community sample. British Journal of Psychiatry, 157, 288–290.
Nehring, I., Schmoll, S., Beyerlein, A., Hauner, H., & von Kries, R. (2011). Gestational weight gain and long-term postpartum weight retention: A meta-analysis. American Journal of Clinical Nutrition, 94, 1225–1231.
Nohr, E. A., Vaeth, M., Baker, J. L., Sørensen, T. I., Olsen, J., & Rasmussen, K. M. (2008). Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. American Journal of Clinical Nutrition, 87, 1750–1759.
Onyango, A. W., Nommsen-Rivers, L., Siyam, A., Borghi, E., de Onis, M., Garza, C., et al. (2011). Post-partum weight change patterns in the WHO multicentre growth reference study. Maternal & Child Nutrition, 7, 228–240.
Pawlak, M. T., Alvarez, B. T., Jones, D. M., & Lezotte, D. C. (2015). The effect of race/ethnicity on gestational weight gain. Journal of Immigrant and Minority Health, 17, 325–332.
Restall, A., Taylor, R. S., Thompson, J. M., Flower, D., Dekker, G. A., Kenny, L. C., et al. (2014). Risk factors for excessive gestational weight gain in a healthy, nulliparous cohort. Journal of Obesity, 2014, 148391.
Rode, L., Kjærgaard, H., Damm, P., Ottesen, B., & Hegaard, H. (2013). Effect of smoking cessation on gestational and postpartum weight gain and neonatal birth weight. Obstetrics and Gynecolology, 122, 618–625.
Siega-Riz, A. M., Viswanathan, M., Moos, M.-K., Deierlein, A., Mumford, S., Knaack, J., et al. (2009). A systematic review of outcomes of maternal weight gain according to the Institute of Medicine recommendations: Birthweight, fetal growth, and postpartum weight retention. American Journal of Obstetrics and Gynaecology, 201, 339.e1–339.e14.
Sommer, C., Mørkrid, K., Jenum, A. K., Sletner, L., Mosdol, A., & Birkeland, K. I. (2014). Weight gain, total fat gain and regional fat gain during pregnancy and the association with gestational diabetes: A population-based cohort study. International Journal of Obesity, 38, 76–81.
Tran, A. T., Straand, J., Diep, L. M., Meyer, H. E., Birkeland, K. I., & Jenum, A. K. (2011). Cardiovascular disease by diabetes status in five ethnic minority groups compared to ethnic Norwegians. BMC Public Health, 11, 554.
Ueda, Y., Maruo, M., Nakano, H., Honda, Y., Miyama, T., Nishizawa, M., et al. (2006). Estimation of body fat mass in pregnant women by a new method using bioelectrical impedance analysis with compensation for intrauterine component weight. International Journal of Body Composition Research, 4, 145.
Uitewaal, P. J., Manna, D. R., Bruijnzeels, M. A., Hoes, A. W., & Thomas, S. (2004). Prevalence of type 2 diabetes mellitus, other cardiovascular risk factors, and cardiovascular disease in Turkish and Moroccan immigrants in North West Europe: A systematic review. Preventive Medicine, 39, 1068–1076.
Waage, C. W., Falk, R. S., Sommer, C., Mørkrid, K., Richardsen, K., Bærug, A., et al. (2015). Ethnic differences in postpartum weight retention: A Norwegian cohort study. British Journal of Obstetrics and Gynaecology,. doi:10.1111/1471-0528.13321.
Wright, C. S., Weiner, M., Localio, R., Song, L., Chen, P., & Rubin, D. (2012). Misreport of gestational weight gain (GWG) in birth certificate data. Maternal and Child Health Journal, 16, 197–202.
Acknowledgments
This research was by funded by The Research Council of Norway and the South-Eastern Norway Regional Health Authority, Norwegian Directorate of Health and collaborative partners in The City of Oslo, Stovner, Grorud and Bjerke administrative districts. The pregnant women who participated in this study are gratefully acknowledged. We also thank the study staff at the child health clinics in Stovner, Grorud and Bjerke districts in Oslo and Haavard Skaaland, Oslo University Hospital, for help with the data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kinnunen, T.I., Waage, C.W., Sommer, C. et al. Ethnic Differences in Gestational Weight Gain: A Population-Based Cohort Study in Norway. Matern Child Health J 20, 1485–1496 (2016). https://doi.org/10.1007/s10995-016-1947-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-016-1947-7