Abstract
Objectives Despite potential health risks for women and children, one in five women report alcohol use during pregnancy and a significant proportion of those who quit during pregnancy return to drinking post-delivery. This study seeks to understand the longitudinal patterns of alcohol consumption before, during pregnancy and post-delivery, and the role of maternal characteristics for purposes of informing prevention design. Methods General growth mixture models were used to describe the average developmental patterns of maternal weekly drinking quantity at six time points, from preconception through child entering kindergarten, as well as heterogeneity in these patterns among 9100 mothers from the Early Childhood Longitudinal Study representing the 2001 US national birth cohort. Results Four distinct classes of mothers were defined by their longitudinal alcohol consumption patterns: Low Probability Drinkers (50.3 %), Escalating Risk Drinkers (12.0 %), Escalating Low Risk Drinkers (27.4 %), and Early Parenting Quitters (10.2 %). Heterogeneous covariate associations were observed. For example, mothers who gave birth after age 36 were twice as likely to be Escalating Risk Drinkers and Escalating Low Risk Drinkers (vs Low Probability Drinkers), but not more likely to be Early Parenting Quitters, when compared to mothers who gave birth between the ages of 26 and 35. Conclusions for practice There is significant heterogeneity in maternal longitudinal alcohol use patterns during the perinatal period. Baseline maternal characteristics and behavior associated with these heterogeneous patterns provide valuable tools to identify potential risky drinkers during this critical time period and may be synthesized to tailor pre- and postnatal clinical counseling protocols.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
Alcohol use during pregnancy is a leading cause of poor infant outcomes. Postpartum alcohol consumption potentially poses risk to women’s own health and may contribute to a deficient child-rearing environment. Past research has solely focused on either pregnancy or postpartum use with only a single point-in-time measure within one year post-delivery.
This study investigated the longitudinal patterns of weekly quantity of maternal drinking using data from a large national representative sample, covering the entire perinatal period, from pre-conception to five to six years after childbirth. The investigation of how maternal characteristics and behaviors at baseline predict these patterns contributes to early identification and tailored clinical interventions for perinatal and early parenting women at risk of problematic alcohol use.
Introduction
Alcohol use during pregnancy (AUDP) is a leading cause of still birth, spontaneous abortion, preterm delivery, and various child neurobehavioral problems [1]. Despite a significant dose-response relationship [2], even low-level AUDP can be detrimental to a child’s neurocognitive development [3]. Such risks have inspired a growing body of epidemiological research to examine patterns of use and risk factors for maternal prenatal alcohol consumption [4], and have guided the development of effective prevention programs, such as the Family–Nurse Partnership [5], as well as the implementation of state and federal legislations, such as Title V (Maternal and Child Health Services) of the Social Security Block Grants [6].
Despite the signficant decline in drinking during pregnancy (from 58 to 19 % in the first trimester, further to 6 % in the third trimester), 37–52 % new mothers resume alcohol consumption within a year post-delivery [7–9]. In addition to the well-documented harmful effects of risky drinking (defined as consuming 4 + drinks per occasion or 7 + drinks per week) on mothers’ own health [10], exposure to alcohol through breast milk can also pose significant risks to a child’s well-being [11]. In addition, excessive alcohol consumption postnatal, often accompanied by maternal distraction, neglect, unpredictable behavior, and other mental health issues, contributes to a deficient child rearing environment [12]. While it is recognized that risky maternal drinking can be identified during pediatric visits [13], prevention efforts implemented immediately after delivery have been found to be of limited effectiveness [14] or to have only short-term benefits [15]. Compared to data on mothers’ prenatal alcohol consumption, there are limited epidemiological data on alcohol use during the postpartum and early parenting periods to guide intervention efforts.
There are inherent challenges to understanding maternal drinking around the time of childbirth reflecting each woman’s unique contextual milieu. On one hand, pregnancy and childbirth mark an important transition in women’s lives characterized by psychosocial, economic and logistical changes [16], which may facilitate reduced alcohol consumption through changing norms, expectations, and responsibilities [17, 18]. On the other hand, increased responsibilities associated with caring for a young child may create stressful challenges, undermining the parenthood’s potential protective effect on drinking [19]. Both intra- and interindividual developments inform a longitudinal process that may be expressed as a maternal perinatal drinking pattern. However, to date, studies of maternal drinking behavior have examined prenatal [20–23] and postnatal [7, 24–27] drinking separately, with most postpartum studies measuring it at a single point in time within 1 year post-delivery.
This study is the first to systematically investigate the longitudinal patterns of weekly maternal drinking quantity using data from a large nationally representative sample, covering the entire perinatal period from pre-conception until five to 6 years after childbirth. We hypothesized that mothers in this sample tend to follow several distinct trajectories of alcohol drinking during perinatal period, e.g., a low drinking trajectory, a persistent and high drinking trajectory, and a moderate drinking trajectory. To contribute to the research on early identification of at-risk mothers, we further investigate how maternal characteristics and behaviors measured at baseline predict these patterns. We hypothesized that several of these characteristics may be related to the likelihood of following each trajectory. For example, older women and those with higher income may be less likely to follow a low drinking trajectory compared to their younger and less wealthy peers.
Methods
Sample
Data are drawn from the Early Childhood Longitudinal Study (ECLS-B) conducted by the US Department of Education-National Center for Education Statistics (NCES). ECLS-B is a prospective longitudinal data set with a nationally representative sample of 10,700 children from the 2001 US birth cohort followed from birth through kindergarten. This study employs survey data collected from adult biological mothers interviewed when a child was 9 months old (baseline survey), and then followed up when the child was 2 years old (2003–2004), 4 years old (2005–2006, preschool), and again 5 or 6 years old (2006–2007, kindergarten). Detailed information, including sampling design and survey instruments are available elsewhere [28, 29].
Mothers were asked at each of the four interviews whether they drank any alcohol. Information regarding third trimester AUDP was retrospectively collected at the baseline interview, circumventing the potential underreporting of antenatal reports during pregnancy [30–32]. In addition, mothers were asked at baseline to report their alcohol consumption 3 months prior to conception, resulting in a total of 6 time points for alcohol consumption measures. We excluded mothers with missing alcohol consumption data at all six time points (1 % of the sample). The remaining missing data on drinking measures (about 60 % had valid information on all six drinking measures and another 20 % missed only one drinking measure) were accounted for by using the widely accepted full information maximum likelihood (FIML) estimation method [33, 34]. We further excluded cases with missing data on any of the exogenous variables (about 10 % of the sample) resulting in an analytical sample of 9100 (sample size rounded to the nearest 50 in compliance with the ECLS-B confidentiality rules [29]). Table 1 presents sample characteristics. Complex sampling design was accounted for by computing robust standard errors using a sandwich estimator [35], and results were weighted to represent the 2001 birth cohort.
Measures
Longitudinal Measures of Maternal Perinatal Drinking
For women who reported current alcohol use, quantity of use was assessed in preset categories of the number of drinks consumed in an average week (less than 1, 1–3, 4–6, 7–13, 14–19, and 20 or more drinks). Following Brown et al. [36] using the same dataset, we collapsed the original measures into a four-level variable (no alcohol, <1 drink per week, 1–3 drinks per week, and 4 + drinks per week) to maintain an ordinal scale while managing the low response frequencies in the higher use categories that pose problems for model estimation (Across all measurement occasions, 0.1–7.1 % of mothers drank 4 + drinks and <0.1 % drank 7 + drinks per week.). Self-reported measures of alcohol use are considered reliable and valid, with contextual limitations [37].
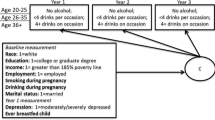
Exogenous Variables
The following information was collected at baseline: maternal age (18–25, 26–35, and 36+), education (<high school, high school degree, some college, college/graduate school); race/ethnicity (white, black, Hispanic, other); postpartum depression measured with a modified 12-item version of the Center for Epidemiologic Studies Depression Scale (CES-D) [38] and recoded into severe/moderate depression and low/no depression per Paulson et al. [39]; mother’s marital status (married/cohabitating, other); household income-poverty (<poverty line, 100–130 % of poverty line, 130–185 % of poverty line, ≥185 % of poverty line); and employment status (full-time, part-time, not employed). Additional covariates include duration of breast-feeding (never, breastfed ≤ 6 months, breastfed > 6 months per Ogbuanu et al. [40]), as well as a binary current maternal smoking measure at baseline.
Analytic Plan
The multilevel nature of the data, i.e., measurement occasions nested within individuals, requires methods to arrive at unbiased point estimates and standard errors. While several methods are available to analyze such data, only General Growth Mixture Models (GGMM) [41] allow for inspecting inter-individual differences in intra-individual change. GGMM uses a categorical latent class variable in combination with continuous latent growth factors (see Fig. 1) to explore population heterogeneity in the change process of the outcome of interest, i.e., whether the study population consists of two or more discrete classes of individuals with varying growth trajectories [41, 42].
The modeling sequence followed the guidelines for growth models with ordered categorical outcomes [42, 43]. The specification of the latent growth model with categorical outcomes uses a latent response variable formulation [43] which assumes that a continuous latent response variable y* underlies the observed response y with different thresholds delineating response categories. Growth factors (e.g. intercept and slope) are estimated representing the relationship between time and y*. However, instead of residual variances for each growth indicator as is the case for conventional growth models, thresholds for each growth indicator are estimated [43].
The origin of time was set at the baseline interview in order to support the association of baseline covariates with subsequent drinking measures [44]. In order to test the overall functional form of the sample, we first estimated a series of growth models with fixed or random growth factors including intercept, linear and quadratic slopes. Model comparison and selection was based on theoretical reasoning and model fit [43] utilizing the Pearson model Chi-squared goodness-of-fit test, relative goodness-of-fit based on the likelihood ratio test (LRT) for nested models, and response pattern goodness-of-fit based on standardized residuals. A model with a random intercept and a random slope best described the development of maternal alcohol use during the study period.
Based on this functional form, heterogeneity in the longitudinal development of maternal drinking was explored by estimating models with increasing numbers of classes. Deciding on the number of longitudinal latent classes is based on substantive evaluation of the classes as well as fit statistics for non-nested models, such as the Bayesian Information Criterion (BIC) and the Lo-Mendell-Rubin likelihood ratio test (LMR-LRT; a significant p value indicates that the model with K-1 number of classes can be rejected in favor of the model with K number of classes) [45]. Entropy (ranges from 0 to 1 and indicates a better classification of individuals as values approach 1), was obtained as a measure of classification quality, [46].
Upon finalizing class enumeration, we re-estimated the preferred GGMM model and simultaneously regressed the latent classes on exogenous variables via multinomial logistic regression equations [47]. All covariates were included simultaneously in a multivariate model, and the odds ratio for each covariate, adjusting for the effects of other covariates, is reported. Five hundred random start values were used to reach a global, rather than local, maximum [48]. All analyses were conducted using Mplus version 7.11 [49].
Results
Observed and Estimated Patterns of Drinking
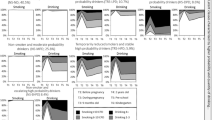
Over half of the women (60.5 %) did not drink any alcohol pre-conception (Table 1). Among those who drank, most drank 1-3 drinks and only 6.9 % drank 4 + drinks per week. The majority (96.7 %) did not consume alcohol during their last trimester of pregnancy. The prevalence of drinking <1 drinks and that of drinking 1–3 drinks weekly re-approached (though never fully returned to) preconception levels by the 9-month interview and remained relatively stable thereafter, while the proportion of women drinking 4 + drinks per week increased gradually to a level slightly higher than preconception. The estimated proportions from the selected functional form closely resembled the observed pattern, indicating good fit.
Heterogeneity in the Drinking Patterns
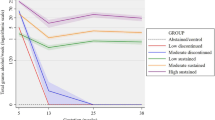
A four-class model (LL = −34,513.0 (16), BIC = 69,171.83) was selected (Table 2). Mothers in this sample were likely to fall into one of four alcohol consumption patterns (Fig. 2). Half of mothers (Low Probability Drinkers) were characterized by a very low and stable probability (<0.1) of any drinking. Nearly all mothers reduced or quit alcohol consumption by the third trimester of pregnancy. An Escalating Risk Drinkers group (12 % of the sample) exhibits a high and significantly increasing probability of drinking at different levels. With the exception of having a lower probability during pregnancy (0.3), mothers in this class had a 0.9 probability of drinking any alcohol (including < 1, 1–3 and 4 + drinks per week) throughout the study period. Mothers in this profile had a probability as high as 0.4 to drink 4 + drinks per week by the time their child entered kindergarten. One-third (27.4 %) of the recent mothers exhibited a low risk pattern of significantly escalating drinking (the Escalating Low Risk Drinkers) during the early parenting years. One in ten (10.2 %) mothers (the Early Parenting Quitters) who consumed at a level similar to the Escalating Risk Drinkers prior to pregnancy resumed consumption briefly postpartum but then exhibited a significantly decreasing trend, essentially having quit drinking when their child entered kindergarten.
Covariate Effects
Table 3 presents the effect of covariates on the log odds of being in one of the three drinking classes using Low Probability Drinkers (LPD) class as the reference group. Adjusted odds ratios (AOR) and significance level are presented, with an AOR >1 indicating increasing log odds of being assigned to a given class compared to the LPD class [50]. When compared to their peers who gave birth between ages 26 and 35, mothers younger than 25 were half as likely (AOR = 0.53) and those who gave birth when older than 36 were twice as likely (AOR = 2.18) to be in the Escalating Risk Drinkers class (vs the LPD class). Age did not significantly influence profile membership for the other two drinking classes. Non-white mothers were less likely (AORs range from 0.26 to 0.57) and mothers with higher level of education were more likely (AORs range from 1.99 to 4.52) to be in either the Escalating Risk Drinkers class or the Escalating Low Risk Drinkers class versus the LPD class, when compared respectively to mothers of white race and those with less than high school education. No significant relationship was detected for race or education between the probabilities of being classified as an Early Parenting Quitter versus the LPD class.
When compared to those who earned an income below the poverty line, reporting a household income higher than 185 % of the poverty line significantly increased the probability of being in each of the three drinking classes (AORs range from 2.16 to 3.96) versus the LPD class, with the strongest effect being observed for the Escalating Risk Drinkers, Married or cohabitating mothers were less likely to be in one of the drinking classes (AOR ranges from 0.56 to 0.63) versus the LPD class, compared to their single or divorced peers. While both part-time (AOR = 1.43) and full-time (AOR = 1.48) employment increased the likelihood of being in the Escalating Low Risk Drinker profile, only part-time employment increased the likelihood of being assigned to the Escalating Risk Drinkers class (AOR = 1.76), versus the LPD class.
Smoking postpartum increased the likelihood of being in each of the three drinking classes versus the LPD class with varying magnitude (AORs range from 2.08 to 4.31). Postpartum depression had a significant impact on being classified as an Early Parenting Quitter (AOR = 1.82) versus the LPD class, while the impact of depression on the other two drinking classes was not statistically significant. Breastfeeding fewer than 6 months increased the probability of being an Escalating Risk Drinker (AOR = 1.68) or an Escalating Low Risk Drinkers (AOR = 1.42) versus the LPD class, while breastfeeding longer than 6 months did not have any significant effect on patterns of maternal drinking.
Discussion
Despite the growing body of literature on maternal alcohol consumption during pregnancy, this study is the first effort to investigate perinatal alcohol use as a longitudinal developmental process from preconception through the close-knit early parenting years. The simultaneous examination of inter-individual variation in intra-individual change is crucial to the identification of what, whom and when to target for prevention interventions aiming to reduce the harmful effect of maternal drinking on maternal and child health. While the literature has consistently reported on the general trend of maternal drinking resuming postpartum, results from this GGMM analysis indicate a great degree of heterogeneity in these longitudinal patterns. Specifically, from preconception until the child enters kindergarten, mothers in our sample were likely to fall into one of four alcohol consumption patterns characterized by different baseline levels of alcohol consumption and changes over time.
While the Escalating Risk Drinking class does not necessarily signal risky drinking as judged by federal standards for women (i.e. 7 + per, per the National Institute on Alcohol Abuse and Alcoholism), the consistent tendency of drinking 4 + drinks per week (with the potential for occasional binge drinking) during this critical period of time is concerning. About one-third of the women in this group continued drinking during pregnancy. According to CDC and the US Surgeon General, no amount of alcohol consumption has been proven safe during pregnancy [51, 52]. Further, excessive postnatal alcohol consumption may pose risks to children [12].
Consistent with other research regarding risk factors for maternal drinking [7, 9, 26, 53, 54], white race, older age, greater income, higher education, being single, and part-time employment are associated with following the Escalating Risk Drinking pattern. Although depressive symptoms are commonly associated with AUDP [21, 53, 55], evidence regarding the association between postpartum depression and longitudinal patterns of alcohol consumption tend to be mixed. Consistent with a study of risky drinking [9], in the present study, postpartum depression did not differentiate escalating drinking patterns from Low Probability Drinkers, whereas other research has found correlations between postpartum alcohol use and depression [56]. However, past studies measured postpartum alcohol use at a single time point and thus were not designed to differentiate the effect of depression on distinct longitudinal patterns of maternal alcohol use.
The finding that smoking postpartum increased the likelihood of mothers following one of the three drinking trajectories (vs the LPD trajectory), is consistent with past studies associating smoking with the risk of drinking [4, 55, 57]. This finding emphasizes the value of guidance for clinical screening of maternal smoking behavior throughout the early parenting years (i.e. in pediatric settings as well as maternal clinical visits) to address alcohol use as well.
The positive association of breastfeeding for <6 months with Escalating Risk and Escalating Low Risk drinking is consistent with studies finding that increased postpartum drinking is associated with breastfeeding for shorter time periods [11]. New mothers may be inclined to make healthier choices through the breastfeeding period out of concern for their child’s health [58]. Postnatal maternal health care and pediatric visits may support women maintaining reduced alcohol consumption for longer by encouraging breastfeeding for at least 6 months, thus reducing the risks to child development associated with maternal drinking [59, 60].
Limitations include: First, the baseline measurement of depression reported an average of 9 months post-delivery does not include any detail about constancy or intensity. Second, although personal characteristics correlated with drinking frequency may vary [20], this study is limited to measures of weekly drinking quantity. Research incorporating longitudinal measures of both quantity and frequency will further elucidate women’s drinking patterns in this critical period of their reproductive lives. Last, while 4 + drinks per week does not necessarily signal risky alcohol consumption outside of pregnancy, there are multiple reasons to attend to such drinking pattern during this period of their lives. Despite the biological risks associated with any drinking during breastfeeding, 4 + drinks per week may also signal for some women the potential of binge drinking which poses threats to women’s health and child wellbeing.
It is concerning that despite a decline in drinking prevalence rates among pregnant women from the 1980s through the early 2000s [61, 62], this rate has stabilized in the past decade [63]. The prevalence of alcohol consumption among recent mothers within a year postpartum also remains high [63]. The potential risks that excessive maternal drinking cast on maternal and newborn health during this critical period of time call for prevention and intervention effort outside of the commonly targeted 9-month pregnancy period.
Though literature suggests some evidence for effectiveness of several interventions (e.g. motivational interviewing, brief interventions, cognitive behavioral therapy, and health education) on drinking abstinence during pregnancy [64], a review of postpartum home visits did not find any evidence of effectiveness in reducing alcohol misuse [14]. Thus, expanding prevention of AUDP and maternal alcohol misuse during early parenting years may require redesigning the approach and expanding the target population to women of reproductive age. Although most women (87 %) who report consuming alcohol before they realized they were pregnant report abstaining completely by the time of their first prenatal visit [55], as many as one-third of women of reproductive age may be classified as risky drinkers [65]. An experiment targeting women of reproductive age with two 15-min scripted sessions resulted not only in significant reductions in past week drinking and binge drinking episodes, but also showed positive impact for participants who got pregnant within the 48-month follow up period [66]. In addition, existing and new prevention strategies should take this research into account to tackle postpartum and early parenthood alcohol consumption whether through enhancing social support systems or promoting healthy stress management associated with increased responsibilities of caring for a young child. Findings of different patterns of maternal perinatal drinking associated with maternal characteristics provide potentially valuable tools for family physicians, pediatricians and nurse practitioners to identify those at risk for problem drinking during this critical time period and to better tailor interventions to individual needs.
References
Meyer-Leu, Y., et al. (2011). Association of moderate alcohol use and binge drinking during pregnancy with neonatal health. Alcoholism, Clinical and Experimental Research, 35, 1669–1677.
Sood, B., et al. (2001). Prenatal alcohol exposure and childhood behavior at age 6 to 7 years: I. Dose-response effect. Pediatrics, 108(2), e34.
Streissguth, A. P., et al. (1999). The long-term neurocognitive consequences of prenatal alcohol exposure: A 14-year study. Psychological Science, 10(3), 186–190.
Ethen, M., et al. (2009). Alcohol consumption by women before and during pregnancy. Maternal and Child Health Journal, 13, 274–285.
Olds, D. L., et al. (2002). Home visiting by paraprofessionals and by nurses: A randomized, controlled trial. Pediatrics, 110, 486–496.
United States of America, Legislative Base: Maternal and Child Health Services Block Grant; Title V of the Social Security Act: Compilation of Maternal and Child Health Legislation 1912–1996. 1996.
Laborde, N., & Mair, C. (2012). Alcohol use patterns among postpartum women. Maternal and Child Health Journal, 16, 1810–1819.
Substance Abuse and Mental Health Services Administration. (2009). Substance use among women during pregnancy and following childbirth, in the NSDUH Report. Substance abuse and mental health services administration. Rockville, MD: Office of Applied Studies.
Jagodzinski, T., & Fleming, M. F. (2007). Correlates of postpartum alcohol use. Wisconsin Medical Journal, 106, 319–325.
Fan, A. Z., et al. (2008). Patterns of alcohol consumption and the metabolic syndrome. Journal of Clinical Endocrinology and Metabolism, 93, 3833–3838.
Little, R. E., Lambert, M. D., & Worthington-Roberts, B. (1990). Drinking and smoking at 3 months postpartum by lactation history. Paediatric and Perinatal Epidemiology, 4, 290–302.
Jester, J. M., et al. (2000). The influence of maternal drinking and drug use on the quality of the home environment of school-aged children. Alcoholism, Clinical and Experimental Research, 24(8), 1187–1197.
Jonas, D. E., et al. (2012). Behavioral counseling after screening for alcohol misuse in primary care: A systematic review and meta-analysis for the us preventive services task force. Annals of Internal Medicine, 157, 645–654.
Turnbull, C., & Osborn, D. A. (2012). Home visits during pregnancy and after birth for women with an alcohol or drug problem. Cochrane Database of Systematic Reviews, (1).
Fleming, M. F., et al. (2008). The healthy moms study: The efficacy of brief alcohol intervention in postpartum women. Alcoholism-Clinical and Experimental Research, 32, 1600–1606.
Rutter, M. (1996). Transitions and turning points in developmental psychopathology: As applied to the age span between childhood and mid-adulthood. International Journal of Behavioral Development, 19, 603–626.
Staff, J., et al. (2014). Family transitions and changes in drinking from adolescence through mid-life. Addiction, 109(2), 227–236.
Fergusson, D. M., Boden, J. M., & Horwood, L. J. (2012). Transition to parenthood and substance use disorders: findings from a 30-year longitudinal study. Drug and Alcohol Dependence, 125(3), 295–300.
Wolfe, J. D. (2009). Age at first birth and alcohol use. Journal of Health and Social Behavior, 50, 395–409.
Haynes, G., Dunnagan, T., & Christopher, S. (2003). Determinants of alcohol use in pregnant women at risk for alcohol consumption. Neurotoxicology and Teratology, 25(6), 659.
Meschke, L. L., et al. (2008). Correlates of prenatal alcohol use. Maternal and Child Health Journal, 12, 442–451.
Duncan, E. M., Forbes-McKay, K. E., & Henderson, S. E. (2012). Alcohol use during pregnancy: An application of the theory of planned behavior. Journal of Applied Social Psychology, 42, 1887–1903.
Skagerstrom, J., Chang, G., & Nilsen, P. (2011). Predictors of drinking during pregnancy: A systematic review. Journal of Womens Health, 20(6), 901–913.
Jagodzinski, T., & Fleming, M. F. (2007). Postpartum and alcohol-related factors associated with the relapse of risky drinking. Journal of studies on Alcohol and Drugs, 68, 879–885.
McLeod, D., et al. (2002). Factors influencing alcohol consumption during pregnancy and after giving birth. New Zealand Medical Journal, 115(1157), U29.
Parackal, S., Ferguson, E., & Harraway, J. (2007). Alcohol and tobacco consumption among 6–24-months post-partum New Zealand women. Maternal and Child Nutrition, 3(1), 40–51.
Liu, W., Mumford, E. A., & Petras, H. (2015). Maternal patterns of postpartum alcohol consumption by age: A longitudinal analysis of adult urban mothers. Prevention Science, 16(3), 353–363.
Najarian, M. (2010). Early childhood longitudinal study, birth cohort (ECLS-B), preschool-kindergarten 2007 psychometric report. Washington, DC: National Center for Education Statistics, Institute of Education Sciences, US Department of Education.
National Center for Education Statistics. Early Childhood Longitudinal Program. http://nces.ed.gov/ecls/birthdatainformation.asp. Accessed 8 June 2012.
Alvik, A., et al. (2006). Alcohol consumption before and during pregnancy comparing concurrent and retrospective reports. Alcoholism-Clinical and Experimental Research, 30, 510–515.
May, P. A., et al. (2009). Prevalence and epidemiologic characteristics of FASD from various research methods with an emphasis on recent in-school studies. Developmental Disabilities Research Reviews, 15(3), 176–192.
Hannigan, J. H., et al. (2010). A 14-year retrospective maternal report of alcohol consumption in pregnancy predicts pregnancy and teen outcomes. Alcohol, 44(7–8), 583–594.
Arbuckle, J. L. (1996). Full information estimation in the presence of incomplete data. In G. A. Marcoulides & R. E. Schumacker (Eds.), Advanced Structural Equation Modeling: Issues and Techniques (pp. 243–277). Mahwah, NJ: Erlbaum.
Schafer, J. L., & Graham, J. W. (2002). Missing data: Our view of the state of the art. Psychological Methods, 7(2), 147–177.
White, H. (1980). A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica: Journal of the Econometric Society, 48, 817–838.
Brown, C. W., Olson, H. C., & Croninger, R. G. (2010). Maternal alcohol consumption during pregnancy and infant social, mental, and motor development. Journal of Early Intervention, 32(2), 110–126.
Del Boca, F. K., & Darkes, J. (2003). The validity of self-reports of alcohol consumption: State of the science and challenges for research. Addiction, 98, 1–12.
Radloff, L. S. (1977). The CES-D scale. Applied Psychological Measurement, 1(3), 385–401.
Paulson, J. F., Keefe, H. A., & Leiferman, J. A. (2009). Early parental depression and child language development. Journal of Child Psychology and Psychiatry, 50(3), 254–262.
Ogbuanu, C., et al. (2011). The effect of maternity leave length and time of return to work on breastfeeding. Pediatrics, 127(6), E1414–E1427.
Muthen, B. (2004). Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In D. Kaplan (Ed.), The SAGE Handbook of Quantitative Methodology for the Social Sciences (pp. 345–368). Newbury Park, CA: Sage Publications.
Petras, H., & Masyn, K. (2010). General growth mixture analysis with antecedents and consequences of change. In A. R. Piquero & D. Weisburd (Eds.), Handbook of Quantitative Criminology (pp. 69–100). New York, NY: Springer.
Masyn, K., Petras, H., & Liu, W. (2013). Growth curve models and the study of change with categorical indicators. In D. W. Gerben Bruinsma (Ed.), Encyclopedia of Criminology and Criminal Justice. New York, NY: Springer.
Biesanz, J. C., et al. (2004). The role of coding time in estimating and interpreting growth curve models. Psychological Methods, 9(1), 30–52.
Lo, Y. T., Mendell, N. R., & Rubin, D. B. (2001). Testing the number of components in a normal mixture. Biometrika, 88, 767–778.
Ramaswamy, V., et al. (1993). An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Science, 12(1), 103–124.
Long, J. S., & Cheng, S. (2004). Regression models for categorical outcomes. In M. Hardy & A. Bryman (Eds.), Handbook of data analysis (pp. 259–284). Thousand Oaks, CA: Sage Publications Ltd.
Hipp, J. R., & Bauer, D. J. (2006). Local solutions in the estimation of growth mixture models. Psychological Methods, 11(1), 36–53.
Muthén, L. K. & Muthén, B. O. (1998-2012). Mplus User’s Guide (7th ed.). Los Angeles, CA: Muthén & Muthén.
Long, J. S. (1997). Regression models for categorical and limited dependent variables (Vol. 7). Thousand Oaks, California: Sage Publications, Incorporated.
Health, U.D.O. and H. Services. (2005). US surgeon general releases advisory on alcohol use in pregnancy. Washington, DC: US Department of Health and Human Services.
Centers for Disease Control and Prevention, Alcohol use and binge drinking among women of childbearing age—US, 2006–2010, in MMWR Morb Mortal Wkly Rep. 2012. pp. 534–538.
Meschke, L. L., Holl, J., & Messelt, S. (2013). Older not wiser: Risk of prenatal alcohol use by maternal age. Maternal and Child Health Journal, 17, 147–155.
Chiodo, L. M., et al. (2010). The impact of maternal age on the effects of prenatal alcohol exposure on attention. Alcoholism, Clinical and Experimental Research, 34, 1813–1821.
Harrison, P. A. S., & Abbey, C. (2009). Alcohol and drug use before and during pregnancy: An examination of use patterns and predictors of cessation. Maternal and Child Health Journal, 13(3), 386–394.
Bowen, A., et al. (2012). Patterns of depression and treatment in pregnant and postpartum women. Canadian Journal of Psychiatry, 57(3), 161–167.
Gladstone, J., et al. (1997). Characteristics of pregnant women who engage in binge alcohol consumption. Canadian Medical Association Journal, 156(6), 789–794.
Edvardsson, K., et al. (2011). Giving offspring a healthy start: Parents’ experiences of health promotion and lifestyle change during pregnancy and early parenthood. BMC Public Health, 11, 936.
Haastrup, M. B., Pottegård, A., & Damkier, P. (2013). Alcohol and breastfeeding. Basic and Clinical Pharmacology and Toxicologa, 114(2), 168–173.
Golding, J., et al., (2013). A review of environmental contributions to Childhood motor skills. Journal of Child Neurology.
Bobo, J. K., Klepinger, D. H., & Dong, F. B. (2006). Changes in the prevalence of alcohol use during pregnancy among recent and at-risk drinkers in the NLSY cohort. J Womens Health (Larchmt), 15(9), 1061–1070.
Grant, T. M., et al. (2009). Alcohol use before and during pregnancy in western Washington, 1989–2004: Implications for the prevention of fetal alcohol spectrum disorders. American Journal of Obstetrics and Gynecology, 200(3), 278.e1–278.e8.
Substance Abuse and Mental Health Services Administration. (2008). Alcohol use among pregnant women and recent mothers, 2002–2007, in The NSDUH Report. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies.
Gilinsky, A., Swanson, V., & Power, K. (2011). Interventions delivered during antenatal care to reduce alcohol consumption during pregnancy: A systematic review. Addiction Research & Theory, 19(3), 235–250.
Nayak, M. B., & Kaskutas, L. A. (2004). Risky drinking and alcohol use patterns in a national sample of women of childbearing age. Addiction, 99(11), 1393–1402.
Manwell, L. B., et al. (2000). Treatment of problem alcohol use in women of childbearing age: Results of a brief intervention trial. Alcoholism, Clinical and Experimental Research, 24(10), 1517–1524.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, W., Mumford, E.A. & Petras, H. Maternal Alcohol Consumption During the Perinatal and Early Parenting Period: A Longitudinal Analysis. Matern Child Health J 20, 376–385 (2016). https://doi.org/10.1007/s10995-015-1836-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1836-5