Abstract
To review e-health interventions for maternal and child health (MCH) and to explore their influence on MCH practices in sub-Sahara Africa (SSA). Keyword searches were used to retrieve articles from four databases and the websites of organisations involved in e-health projects for MCH in SSA. A total of 18relevant articles were retrieved using inclusion and exclusion criteria. The researchers reveal the prevalence of the application of mobile phones for MCH care and the influence of the use of information and communication technology (ICT) for delivering MCH information and services to target populations. There is a need to move the application of ICT for MCH care from pilot initiatives to interventions involving all stakeholders on a sub-regional scale. These interventions should also adopt an integrated approach that takes care of the information needs at every stage along the continuum of care. It is anticipated that the study would be useful in the evolution and implementation of future ICT-based programmes for MCH in the region.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Maternal and child death rates in Africa are unprecedentedly high. An estimate presented by the Africa Progress Panel in 2010 showed that approximately 50 % of all maternal deaths across the globe occurred in Africa, which had only 15 % of the world’s population [1]. According to a WHO Fact Sheet, approximately 75 % of these deaths could have been averted if the victims were informed about practices that would aid the prevention of pregnancy and birth complications [2]. Despite the emotional devastation that families in the region are experiencing as a result of maternal and child deaths and their effects on human capital development, governments’ efforts aimed at addressing this health burden have continuously fallen short of local and global expectations [1, 3].
ICT applications in health care, popularly referred to as e-health or sometimes m-health (the use of mobile technology for healthcare), is being widely embraced because of its innovation, cost effectiveness, and ability to deliver health information and services to remote locations [4–7].
The prospects of rapidly reducing high maternal and child mortalities prevalent in Africa are soaring because of the various innovations and progress made in the field of information communication technology [8]. This opens windows of opportunities for accelerating this progress towards reducing maternal and child deaths [9–11]. This is evident in some African countries where ICT was used to deliver maternal and child health (MCH) information and services. In the Iganga District of Eastern Uganda, a radio communication system was used by Traditional Birth Attendants (TBAs) to partner with the public health facilities to deliver health care to pregnant women [12]. Likewise, in Egypt, the use of mobile phones has helped to reduce the response time for obstetric emergencies [13]. In the Dangme West District of Ghana, mobile phones were used to contact health workers and health facilities in emergencies [14]. Similarly, in Nigeria, the safe-motherhood programme, also known as Abiye, in Ondo State and the Midwifery Service Scheme are notable examples of the use of ICTs by health workers to reduce maternal mortality in Nigeria [15, 16].
Noordam et al. [17] and the review of m-health programmes for mothers and newborns by Tamrat and Kachnowski [10] indicate the need for robust studies on the impact of mobile phones in improving the quality of m-health interventions. Oyeyemi [18] notes that, in spite of the soaring popularity of e-health and the potential for the use of ICTs for health care, studies providing documentation on best practices, challenges, lessons learnt and outcomes are rare, especially in Africa. As such, there is a need for studies to focus more attention on the efficacy and effectiveness of ICTs or cell phones for m-health interventions aimed at promoting MCH.
Therefore, this paper provides a succinct overview of ICT interventions in sub-Sahara Africa (SSA) for MCH. Its focus is to document the applications of ICT for MCH care, including the lessons learnt, challenges and outcomes.
Methodology
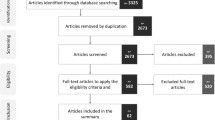
The articles considered for this review focused on ICT interventions in SSA aimed at improving the health of pregnant women and children under the age of five. The Internet keyword search via PubMed, Popline, Global Health, and Google Scholar identified potential peer-reviewed publications. Reference lists were also scrutinised to identify other papers that were promising for review. The Internet search was carried out in March and April 2013 by the researchers and research assistants using keywords combinations, such as maternal, ICT, mobile, technology, child health, health, e-health, m-health, reproductive health, newborn, pregnancy, neonatal, internet, antenatal and prenatal. In addition, programme documents or presentations, reports and guidelines were also identified by searching the websites of organisations and agencies (mhealthalliance, mhealthinfo, and e-health, Nigeria, Millennium Village Project, Text4Change and USAID) engaged in ICT interventions for MCH [10, 17]. The literature search was limited to peer-reviewed articles, programme reports and presentations published from 2002 to 2013. These processes yielded a total of 35 promising articles.
Based on the inclusion criteria (See Table 1), the 35 promising articles were pruned to 18 articles. The articles considered for the study were those that had abstracts that contained information about the use of ICT for communicating information (health tips, patient diagnosis, referral, and patient data) for MCH care before conception, during pregnancy, at birth and during the postpartum period, with evidence of an impact in the SSA region between 2002 and 2013. Studies excluded from this review were those focusing on e-health programmes for MCH implemented outside the sub-Saharan Africa region. In addition, articles on e-health projects for MCH that lacked evidence of outcomes or an impact on MCH in SSA were also excluded from the study (See Fig. 1 in the flow diagram of the literature search).
Results
The articles included in this review consisted of 8 reports and 5 qualitative and 5 quantitative studies (see Table 2). Over 80 % of the projects reviewed adopted the use of mobile phone technologies for delivering MCH information and services. The remaining 11 %, the OpenMRS and Mailafiya project in Nigeria, were implemented using computers.
The articles selected for the study were reviewed with the intention to document lessons learnt, challenges and outcomes. The analysis was also carried out to explore the effect of ICT-based interventions on access to health information, patient diagnosis, utilisation of health facilities and MCH practices. These themes were evolved using cues from previous studies as well as gaps identified in the literature [10, 19].
Improved Access to Health Information
Most of the articles reviewed focused on the use of mobile phones for providing health information, with the exception of the OpenMRS and Mailafiya projects in Nigeria. In the OpenMRS project, computer systems were used to provide information on antenatal visits, labour, child health, immunisation and family planning in northern Nigerian (Kaduna State), which was used to support decision-making by health workers. The Mailafiya project also used Intel-powered notebooks to collect patients’ data, including pictures. Other interventions adopted the use of mobile phones to gather data or disseminate MCH information and services [20–35]. See Table 2 for an overview of these projects.
The MCH information disseminated using mobile phones included:
-
Personalised health messages supporting timely and appropriate care-seeking and health practices by mothers.
-
Practical information for health workers to support patient management and the provision of quality care (Chipatala Chapa Foni project, Malawi).
-
Confidential and accurate information on family planning (LigneVerte, the Republic of Congo).
-
Group messaging and alerts on child nutrition and appointment reminders for ANC visits (Rapid SMS in Rwanda, Malawi, and Kenya).
-
Information on nutrition screening, measles vaccination and child registration to support health workers’ decision-making processes (Every Child Counts MVP, Kenya)
-
The provision of time-specific information or reminders each week in a local dialect (voice or text) for specific treatments, such as tetanus vaccination or prenatal care.
-
Information on foetal development, good health practices, breast-feeding and counselling on challenges during pregnancy.
-
Nutritional information for pregnancy: See Box 1 for an example of a message delivered to a pregnant woman in the 5th and 13th weeks of pregnancy (MOTECH, Ghana).
Box 1 An example of a message disseminated to debunk superstitious belief and to encourage healthy feeding during pregnancy -
The ‘RemindMi’ application was used to remind patients of appointments via short message service (SMS) to ensure that they received key childhood interventions (Programme Mwana).
These information services increased women’s awareness of health issues and encouraged them to use available health resources, which guided them and helped them to stay healthy throughout pregnancy and also for caring for their children. Apart from increasing women’s awareness about health issues surrounding pregnancy and child birth, phone consultations also equipped women with knowledge for making informed decisions about their health and that of their children. As a result, mothers were able to manage health issues before getting medical help. This is evident in the Chipatala Chapa Foni project in Malawi where an increase in the home-based management of common health conditions in women and children was observed. For example, more families used mosquito nets to protect children and pregnant women from malaria. The project was able to help in bridging the gap in health service delivery. This is because women in rural areas, who otherwise would have been unreached, were able to interact remotely with the health system without having to travel long distance before getting access to healthcare. The results from the project evaluation showed that 98 % of them were satisfied with the health tips received and 77 % reported being very satisfied. However, the researchers did not report any change in outcome measures such as the mortality ratios in the project area [24, 31].
Likewise, the LigneVerte project in Congo provided information on family planning using a call centre. From 2005 to 2008, the project received approximately 80,000 calls, out of which over 80 % were from men. As a result, the authors exercised concern over the effectiveness of the intervention because more calls came from men. This may be an indication that the programme did not reach the most important target group (women) [22]. Another pilot project in rural Mozambique also used mobile phones for disseminating information. Women in the intervention group of the experimental study were exposed to the use of mobile phones for disseminating MCH information and were compared to the control group. The results from the pilot study showed that the percentage of mothers who knew at least 2 danger signs in pregnancy was significantly higher in the control group (68 %, OR 0.4, p value = 0.009) than in the intervention group (51.6 %). The proportion of mothers who knew danger signs in the postpartum period was fairly low in both groups, but that of the intervention group (11.8 %, OR 0.4, p value = 0.05) was significantly higher than that of the control group (5.3 %). The author reported that selection bias could be responsible for the differences between the groups [29].
The Influence of ICT Use on Maternal and Child Health Practices
The use of ICT for information dissemination, as discussed in the papers reviewed, has influenced the MCH practices of health workers and patients. Musoke [12] notes that a significant effect of ICT use for MCH in Uganda was a change in the health-seeking behaviour of mothers and reproductive outcomes; as health workers were able to communicate easily, referrals and the reputation of health workers improved. This led to an increase in the number of women seeking quality health care. Cooper [30], in a study evaluating the impact of the Chipatala Chapa Foni project (CCPF) in Malawi (involving women, their partners and health workers), reported that there was an improvement in the MCH practices of the mothers. These included practices such as the exclusive breast-feeding of infants and improvement in the nutritional practices of pregnant women. The use of mobile phones for sending appointment reminders and information on vaccination, as observed in the MOTECH, Chipatala Chapa Foni and Every Child Count projects, encouraged attendance for those who might otherwise have missed antenatal and postnatal visits. This consequently increased the number of facility deliveries [20, 23–25].
Furthermore, the first stage of delay (the delay in deciding to seek care by pregnant women) and the third stage of delay (the delay in receiving care at the health facility) are reduced with m-health interventions. For example, in the Abiye project in Ondo State, Nigeria allowed women and health rangers equipped with tricycle ambulances to make free calls using Abiye phones at no cost. This enabled all of the stakeholders involved in the intervention to communicate easily to facilitate referrals in emergencies. This countered the third and first phases of delay in receiving health care encountered by pregnant women [15, 18]. It also led to a reduction in the mortality ratio by 30 % in the intervention area. Challenges, such as an increase in the workload of health workers, inadequate training on the use of equipment and limitations in the structure of mobile applications to track the most at-risk patients and mortality rates could have affected health outcomes, as indicated by the data gathered from the projects.
Likewise, in South Africa, mobile phones were used to send text messages on Human Immunodeficiency Virus (HIV) related topics to HIV-positive pregnant women as well as reminders to encourage treatment adherence. The project recorded improved self-esteem among participants, and over 90 % of HIV-positive mothers joined the Cell-life treatment group. However, the authors expressed concerns over the limitation of the local language used for the messages and the timelines of the messages sent, which might have compromised the outcome of the intervention [34].
Patient Diagnosis
The use ICT for MCH care also led to improvements in patient management and quality of care. As found in the Mobile Community-based Surveillance (mCBs) in Nigeria where health workers respond in a timely manner to obstetric emergencies, the system provides a database in which reported events, responses to events and health outcomes are stored. The technologies used for the system are RapidSMS (RSMS), an application using mobile phones, which can send information across the Internet at a fast rate, and Open Data Kit (ODK), open source software for managing mobile data collection solutions. The midwives at the health facilities used the mCBs system for weekly reports of the major events seen by (TBAs). This equipped health workers at the hospital with practical information about the patients for prescriptions and prompt diagnoses [32]. As a result, the project recorded improved health outcomes: there were 74 total live births (87 % of the community) with only two deaths (2.35 % of the community). Staff at the hospital also reported being able to give accurate reports without human errors in addition to the timely generation of detailed analyses of data obtained from the patients. It was, however, mentioned that input errors and an overload of input data were recorded, which might have affected the observed outcomes.
Likewise, the RSMS programme for MCH in Rwanda provided useful information about patients to health workers at the facility. It allowed doctors and midwives to respond promptly to patient needs, especially in emergencies. As a result, delays normally experienced in patient care were eliminated. This also built the capacity and improved the decision-making ability of health workers. [25, 33].
In Project Mwana in Zambia, mobile technology was used to deliver test results for the diagnosis of HIV in infants in real time to rural clinics. It also facilitated communication between clinics and community health workers. Observations from the health facilities involved in the project indicated that the results of the HIV tests were 50 % faster and the number of results arriving at the health facilities increased by 30 %.There was also an indication of improvement by approximately 75 % in the survival rates among HIV-positive infants who started treatment within the first 12 weeks of life. However, no relationship between the faster turnaround time of results and early Anti-Retroviral Therapy (ART) access for exposed infants was established. Additionally, the authors mentioned that it was too early to know the impact of messages sent via mobile phones on treatment adherence or postnatal appointments [28].
An Increase in the Utilisation of Health Facilities
The implementation of ICT-based interventions for MCH stimulated an increase in the utilisation of health facilities. The Abiye project in Nigeria led to an increase in deliveries at health facilities, because of referrals from community health workers. This led to a 30 % reduction in maternal mortality in the project area. However, the author reported that there was no significant difference in the number of recorded cases of the five major causes of maternal death in the two study locations, probably because the project was new. It was also mentioned that issues such as increase workload and low remunerations might have compromised the health outcomes reported in the article. Similarly, in Rwanda, the RSMS intervention also led to an increase in antenatal care (ANC) visits and the utilisation of health facilities because appointment reminders, and alerts on child nutrition, were sent to mothers. In addition, as indicated in the OpenMRS project report in northern Nigeria, an increase in facility utilisation was recorded because patients associated the use of ICTs with advanced clinics; consequently, more clinic visits were recorded. However, the researchers mentioned an initial problem of low IT skills among the health workers, which discouraged the use of computer systems when the project was initiated.
Furthermore, the evaluators of the Chipala Chapa Foni project in Malawi also confirmed an increase in facility utilisation with the use of mobile technologies. As access to health care improved via mobile phones, more women visited the health units for antenatal services and childbirth. In another (Rescuer) project in the Iganga district in Uganda, where walkie-talkies were used for obstetric emergencies, a similar trend was also observed. The increase in health facility utilisation led to a reduction in maternal mortality by 50 % within 3 years in the project area. Moreover, the researchers of the mhealth projects at the Federal Medical Centre, Owerri, Nigeria also established an increase in facility utilisation as well as a reduction in maternal and child deaths with m-health interventions. All of the projects positively impacted facility utilisation, although the scholars expressed concern over issues such as transportation, network problems and the maintenance of the communication systems, which could have affected the effectiveness of the projects [12, 15, 24, 25, 31, 33].
Discussion
A brief overview of the ICT-based MCH interventions in SSA revealed that they could be referred to as pilots because they provide practical examples and learning grounds for making desired and sustained progress on achieving set targets (Millennium Development Goals 4 & 5). They showed the enormous tasks and challenges of actualising the targets and provided real examples of how ICT could be used to overcome the challenges of cost, limited resources, personnel training, access to medical records and responses during emergencies. They demonstrated that through a well-designed MCH awareness-raising and stakeholder education campaign, ICT could be used to reach more people simultaneously, regardless of how remote their locations are. It could also be used to boost the performance of health workers in decision support and for knowledge enhancement, especially during emergencies.
In addition, using mobile technologies for information dissemination can encourage the adoption of safe MCH practices as outlined by the World Health Organisation, which can lead to behavioural changes [34]. This review also revealed the following crucial factors that can reduce the barriers encountered in accessing quality healthcare by pregnant women, which will have significant impacts on the effectiveness of e-health initiatives and the costs of investment as well as on maternal and child mortality:
-
Private/public partnerships involving governments, mobile phone service providers and Not-for-Profit organisations.
-
Political-will and involvement of state and local governments,
-
Mobility for health workers and ambulances to transport pregnant women during emergencies,
-
Training more health personnel to fill existing gaps in the workforce,
-
Awareness, information dissemination,
-
The inadequate IT skills of health workers and
-
Robust and efficient mobile phone-Internet infrastructure, supported by traditional ICT media (See Table 3 for details).
Given the outcomes of the existing e-health projects for MCH in the SSA region, a more holistic approach to maternal health care is needed in the SSA region. This should harmonise the strategies and lessons learnt from these projects and lead to the adoption of an integrated approach to addressing MCH issues. This is based on the gaps identified from the projects reviewed: m-health projects varied and little emphasis was placed on the period before and after conception (prenatal and postnatal). The holistic approach should implement a user-centred strategy targeted at meeting the information needs of mothers and their influencers, and offering timely services along the continuum of care. That is, from prenatal, through antenatal to delivery and childhood [9, 37]. Additionally, there should be a shift away from standalone programmes. This approach to e-health project implementation is not cost-effective because it prevents standardisation and interoperability, which may drive up the cost of e-health initiatives [38]. Instead, governments and stakeholders may collaborate to replicate harmonised and integrated projects covering all of the stages along the continuum of care across the region to fully realise the benefits of ICTs for MCH. This model of involving all of the stakeholders can also help in reducing the cost of investment in e-health initiatives.
For cost effectiveness, funders of e-health initiatives in SSA may adopt a public—private partnership (PPP) model that will provide valuable opportunities to evaluate the effect of public—private alliance on the cost of ICT-based projects. The public sector can subsidise e-health projects by facilitating low-cost e-health services, which can help control the cost of e-health projects for MCH. This model is evident in some of the e-health projects in the region, as reported by some of the articles reviewed. An example is the Abiye (Safe Motherhood) project in Nigeria, an impressive mhealth project for MCH that has been successful because of the strong public—private model adopted for the project.In the case of the Abiye project, while the public sector provided the human resources, the private sector provided the technology infrastructure required for e-health services for MCH [19]. In addition, with the PPP model, the public sector can evolve policy frameworks that will create the right ambience for investment. The public sector can incentivise investment in, as well as the use of, e-health services for MCH to drive down costs to attract more investment. This can promote competition, which may lead to the increased efficiency of service providers as well as a reduction in the cost of e-health services. In addition, sharing the cost of e-health services for MCH with other electronic services (ePayments and mobile health insurance) can also help to maximise returns on investment for e-health services. This is because hardware and software can be shared by electronic systems, especially when the systems are configured using an integrated approach [39, 40].
The benefits of e-health services for MCH can also be used to attract the support needed for effective ICT-based projects for MCH. It could be used to bypass the bottlenecks encountered by advocacy targeted at policy-makers and government officials. This will consequently enlighten and equip them with the information required for formulating policies and improving access to resources (for budgeting and planning; the provision of medication; and meeting the demands of health workers and facilities).
Limitations
Most of the data derived from the articles included in this study were from pilot e-health initiatives for MCH, which mostly adopted a standalone approach that addresses the information needs of pregnant women at one or two stages along the continuum of care. As a result, they may be insufficient for generalisation.
Conclusion
Findings from this study revealed that e-health interventions for MCH can improve access to health information, influence pregnant women to adopt safe MCH practices, encourage prompt patient diagnosis, and increase the utilisation of health facilities. The analysis indicated a positive relationship between the use of ICT by health workers and the adoption of safe MCH practices by mothers and,consequently,a reduction in maternal and child mortalities. Unfortunately, the number of health institutions implementing e-health programmes is insignificant compared to the total number of health facilities in sub-Sahara Africa. Therefore, there is a need to move the application of ICTs in the health sector for MCH from pilot initiatives to interventions involving all of the stakeholders on a sub-regional scale, while taking care of the health and information needs at all stages along the continuum of care, as recommended by the WHO [36]. The need for the harmonisation of programmes and for expanding the use of ICT employing the PPP model is paramount for scaling up MCH interventions in sub-Sahara Africa. It is also important to provide a supportive environment (ICT, finance and policy) to aid the implementation of these interventions. It is anticipated that the challenges, lessons and outcomes from this review of e-health programmes in sub-Saharan Africa would be useful for policy-makers, researchers and designers of future ICT-based programmes to evolve better programmes for MCH.
Acknowledgments
This research was partially funded by a fellowship award provided by the Consortium for Advanced Research Training in Africa (CARTA). CARTA has been funded by the Wellcome Trust (UK) (Grant No: 087547/Z/08/Z), the Department for International Development (DfID) under the Development Partnerships in Higher Education (DelPHE), the Carnegie Corporation of New York (Grant No: B 8606), the Ford Foundation (Grant No: 1100–0399), Google.org (Grant No: 191994) Sida (Grant No: 54100029) and the Bill and Melinda Gates Foundation (Grant No: 51228).
References
Africa Progress Panel. (2010). Maternal Health: Investing in the Lifeline of Health Societies and Economies. Retrieved from http://www.who.int/pmnch/topics/maternal/app_maternal_health_english.pdf.
WHO (2012). WHO fact sheet No. 348. Retrieved April 20, 2013, from http://www.who.int/mediacentre/factsheets/fs348/en/index.html.
Joshi, S. (2012). Reproductive Health and Economic Development: What connections should we focus on? Research Brief, 3. From:http://www.prb.org/pdf12/poppov-economicdevelopment-reproductivehealth-women.pdf.
Idowu, B., Ogunbodede, E., & Idowu, B. (Federal Ministry of Health & 2003.). Information and Communication Technology in Nigeria. Information and Communication Technology in Nigeria: The Health Sector Experience. Journal of Information Technology Impact, 3(2), 69–76.
Ibegwam, A. (Ed.). (2004). Internet communication: E-mail and medical research. Ibadan: Evi-Coleman Publications.
Olatokun, W. M., & Adeboyejo, F. C. (2009). Information and communication technology use by reproductive health workers in Nigeria: state of the art, issues, and challenges. An Interdisciplinary Journal on Humans in ICT Environments, 5(2), 181–207.
Yamuah, L. K. (2005). Towards Healthy Nations with ICT Wealth ICT in the African Health Sector. Retrieved August 2012, from: http://www.keewu.com/IMG/pdf/africanhealth.pdf.
Victoria, V., & Nicogossian (2011). mHealth: Saving lives with mobile technology. Retrieved April 2013, from: http://csimpp.gmu.edu/pdfs/student_papers/2011/Victoria.pdf.
Parmar, V. (2009). Design Framework for developing ICT products and services for rural development. A persuasive health information system for rural India. Retrieved January 2013, from: http://repository.tudelft.nl/assets/uuid:99260bf4-7d83-41f0-92c6-cb65ba7c7700/Vikram__parmar__industrial_design.pdf.
Tamrat, T., & Kachnowski, S. (2012). Special delivery: An analysis of mHealth in Maternal and Newborn health programs and their outcomes around the World. Matern Child Health Journal Vol., 16(5), 1092–1101. doi: 10.1007/s10995-011-0836-3http://www.ncbi.nlm.nih.gov/pubmed/21688111.
Rotheram-Borus, M. J., Tomlinson, M., Swendeman, D., Lee, A., & Jones, E. (2012). Standardized functions for smartphone applications: Examples from Maternal and child health. International Journal of Telemedicine Application, 2012, 973237. doi: 10.1155/2012/973237, http://www.hindawi.com/journals/ijta/2012/973237/.
Musoke, M. G. N. (2002). Simple ICTs reduce Maternal Mortality in rural Uganda: A telemedicine case study. Retrieved July 2013, from http://www.medicusmundi.ch/mms/services/bulletin/bulletin200202/kap04/16musoke.html.
Mechael, P. (2005). Case study from Egypt: mobile phones for mother and child care. Information for development. Retrieved March 2013, from: http://unpan1.un.org/intradoc/groups/public/documents/unpan/unpan037365.pdf.
Mechael, P. (2009). MoTECH: mhealth Ethnography Report (pp. 98): Grameen Foundation. Retrieved March 2013, from : http://www.kiwanja.net/database/document/document_motech_mhealth_ethnography_report.pdf.
Fajembola, T. (2011). Abiye: Safemotherhood :A case of leadership in turning the tide of maternal mortality in Nigeria. Nigerian health journal. Retrieved January 2013, from http://nigerianhealthjournal.com/?p=1526.
Murtala Mai, M. (2010). Information and investment to improve availability of skilled providers in underserved areas in Nigeria. The Nigeria Midwives service scheme. Retrieved June 2013, from: http://countdown2015mnch.org/documents/2010Conference/ppts/Murtala-Mai-Mohammad.pdf.
Noordam, C. A., Kuepper, B. M., Stekwlwnburg, J., & Milen, A. (2011). Improvement of Maternal Health services through the use of mobile phones. Tropical Medicine and International Health Vol.16.
Oyeyemi, S. O. (2012). The use of cell phone for Maternal Health : The Abiye project. Retrieve from http://munin.uit.no/handle/10037/4793.
Kaewkungwal, J.,Singhasivanon, P., Khamsiriwatchara, A., Sawang, S., Meankaew, P.,& Wechsart (2010). Application of smart phone in “Better Border Healthcare Program”: A module for mother and child care.BMC Medical Informatics and Decision Making 2010, 10:69.Retrieved September 2012, from http://www.biomedcentral.com/1472-6947/10/69.
Berg, M., Wairiero, J. & Modi, V. (2009). Every child counts- the use of SMS in Kenya to support the community-based management of acute malnutrition and Malaria in children under five. Kenya: Millenium village project. Retrieved, August 21, 2013, from http://www.childcount.org/reports/ChildCount_Kenya_InitialReport.pdf.
Cole-Ceesay, R., Cherian, M., Sonko, A., Shivute, N., Cham, M., Davis, M., Southall, D. (2010). Strengthening the emergency healthcare system for mothers and children in the Gambia. Reproductive Health, 7(21). doi: 10.1186/1742-4755-7-21.
Corker, J. (2010). “Ligne Verte” Toll-Free Hotline: Using cell phones to increase access to family planning information in the Democratic Republic of Congo. Cases in Public Health Communication and Marketing, IV, www.casesjournal.org.
Grameen Foundation (2011). Mobile technology for community Health in Ghana (pp. 30–85). Retrieved May 2013, from: http://courses.cs.washington.edu/courses/cse490d/12sp/docs/MOTECH.pdf.
Innovations for MNCH. (2012). Bridging women and children to better health care: Maternal, newborn and child health access through mobile technology in Balaka District, Malawi http://innovationsformnch.org/uploads/publications/ICT_for_MNCH_2013_Project_Brief_10.02.13_short.pdf.
Kalach, J. (2011). Saving mothers and newborn lives in the community using RapidSMS technology-experience from Musanze District of Rwanda. Retrieved July 2013, from http://www.mhealthinfo.org/project/saving-mothers-and-newborns-using-rapidsms.
Valliere, F., McAuliffe, E. Palmer, I.,Maggity, E. & Bangura, A. S. (2012). Supporting and strengthening Maternal Neonatal and child health services using mobile phones in Sierra Leone: A research protocol. Harvard Africa Policy Journal. Retrieved March, 2013 http://apj.fas.harvard.edu/supporting-strengthening-maternal-neonatal-and-child-health-services-using-mobile-phones-in-sierra-leone-a-research-protocol/.
Ngabo, F., Nguimfack, J., Nwaigwe, F., Mugeni1, C., Muhoza, D., Wilson, D., Binagwaho, A. (2012). Designing and implementing an innovative SMS-based alert system (RapidSMS-MCH) to monitor pregnancy and reduce maternal and child deaths in Rwanda. Pan African Medical Journal, 13(31).
Partnership Profile. (2012). Project Mwana: Using mobile technology to improve early infant diagnosis of HIV in Zambia. http://www.unicef.org/esaro/5440_Zambia_mobile_apps_for_HIV_prevention.html.
Rema, M. T. (2013). Exploring Mobile Technology to Enhance Birth Outcomes in Rural Mozambique: Pilot Study Results. (B.S), USA: University of Georgia.
Osuagwu, E. C., Ogini, A. N., Nnodum, U., & Agbasonu, V. C. The Effectiveness of mHealth Maternal Services of F.M.C. Owerri in reduction of Maternal Mortality rate in Ngor Okpuala Health centre, L.G.A in Imo State. International Conference on Telemedicine and e-health pp. 26–28. http://www.aajimatics.com/wp-content/uploads/2013/05/REPORT-ON-CONF-OUTCOME_17TH-ISfTeH-7-9-NOV-12.pdf.
Cooper, E. (2013). Evaluating social impact of our work- CCPF Malawi. Retrieved November 2013, from http://villagereach.org/2013/04/19/evaluating-the-social-impact-of-our-work-ccpf-malawi.
eHealth, (2011). Mobile Community Based Surveillance(mCBS).(Eds.) In A. Karlyn, E. Castle, A. Thompson, H. Makanjuola and S. Adaji: The use of cellphones for community-based survellance.
Thompson, A., Castle, E., Lubeck, P., & Makarfi, S. (2010). Experience implementing OpenMRS to support Maternal and Reproductive Health in Northern Nigeria. Retrieved April 2013, from http://ehealthafrica.org/wp-content/uploads/2009/10/OMRS_MedInfo_2009_v1.pdf.
Mobile alliance for Maternal action: www. mobilemamalliance.org/mama-south- Africa.
Society For family health. Society for family health and partners release results of Gombe project: Project is tackling Maternal and Neonatal Health challenges in Gombe State, North East Nigeria.http://www.sfhnigeria.org/projects/maternal-and-child-health-gombe.
WHO. (2007). Standards for maternal and neonatal care. Retrieved July 19, 2013 from http://apps.who.int/iris/bitstream/10665/69735/1/a91272.pdf.
Mehl, G. 2010. ehealth and mHealth for Maternal and child health, best practices and challenges of digital health for rural communities: Potential, trends and challenges, ITU. Geneva: WHO. Retrieved March 2013, from http://www.itu.int/ITU-D/cyb/events/2010/infoses_2010/docs/MEHL%20ITU%2017_9_2010%20presented.pdf.
Gerber, T., Olazabal, V., Brown, K., & Pablos-Mendez, A. (2010). An agenda for action on global e-health. Health Affairs, 29, 233–236.
Schweitzer, J., & Synowiec, C. (2012). The economics of eHealth and mHealth. Journal of Health Communication: International Perspectives, 17(sup1), 73–81.
World Health Organization. (2005). eHealth: Proposed Tools and Services: Report by the Secretariat. Geneva, Switzerland: Author. Retrieved April 2012, from http://apps.who.int/gb/ebwha/pdf_files/EB117/B117_15-en.pdf.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Obasola, O.I., Mabawonku, I. & Lagunju, I. A Review of e-Health Interventions for Maternal and Child Health in Sub-Sahara Africa. Matern Child Health J 19, 1813–1824 (2015). https://doi.org/10.1007/s10995-015-1695-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1695-0